Effects of Exercise in Improving Cardiometabolic Risk Factors in Overweight Children: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources and Search Strategy
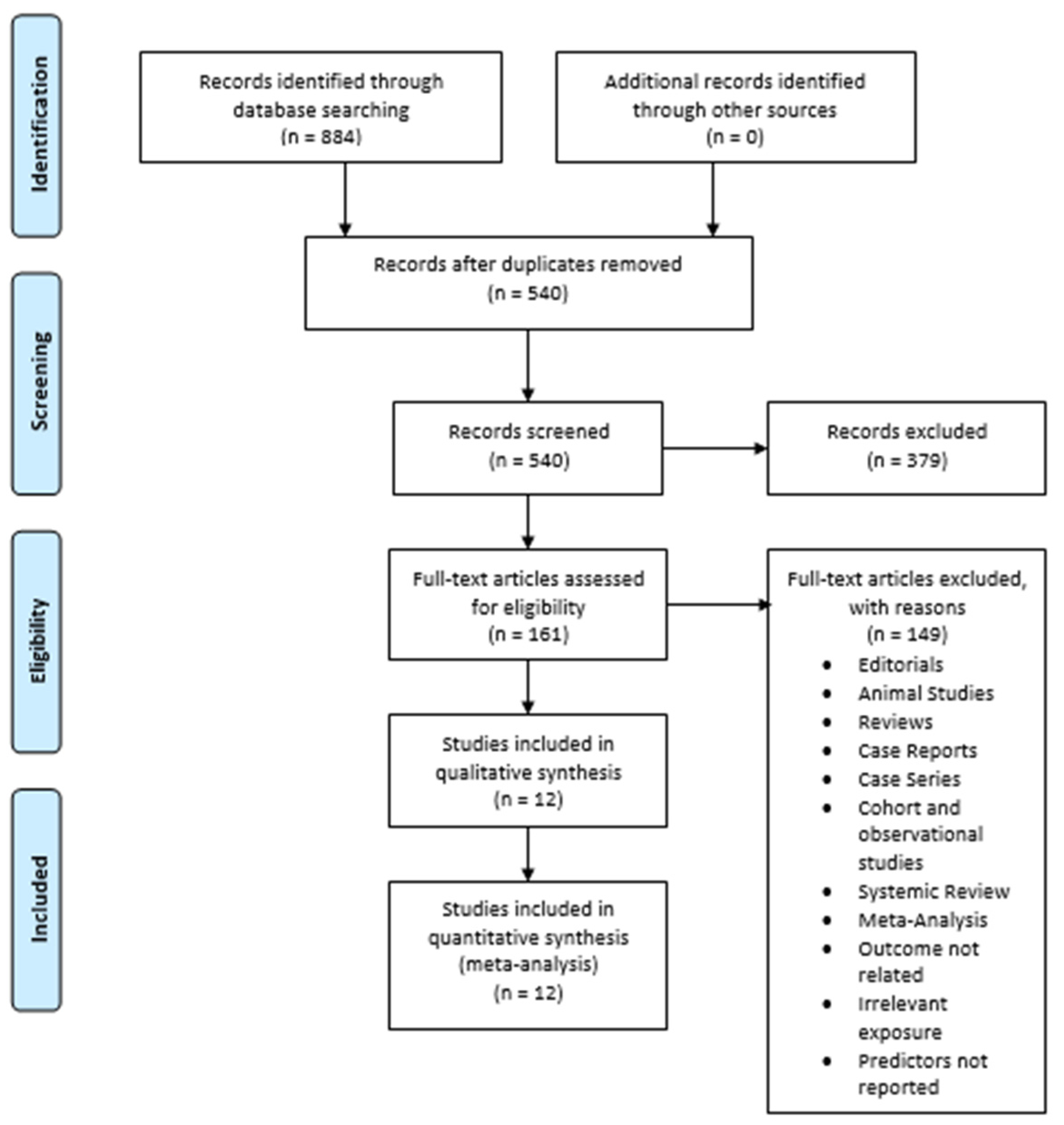
2.2. Study Selection
2.3. Statistical Analysis
2.4. Data Extraction and Quality Assessment of the Studies
3. Results
3.1. Literature Search Results
3.2. Study Characteristics
3.3. Publication Bias Assessment
3.4. Results of the Meta-Analysis
3.4.1. Body Weight
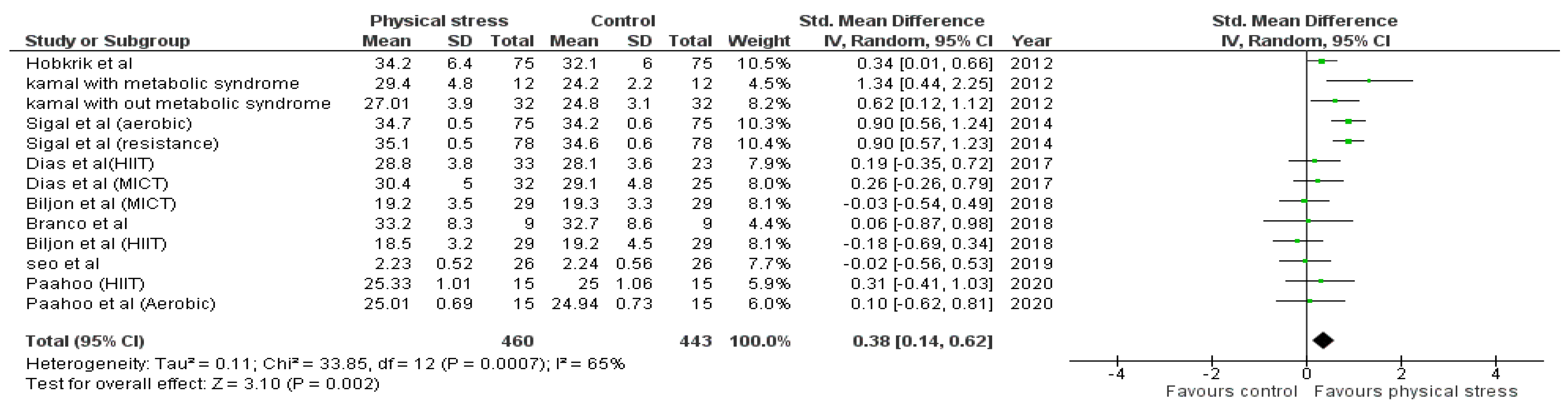
3.4.2. Body Mass Index (BMI)
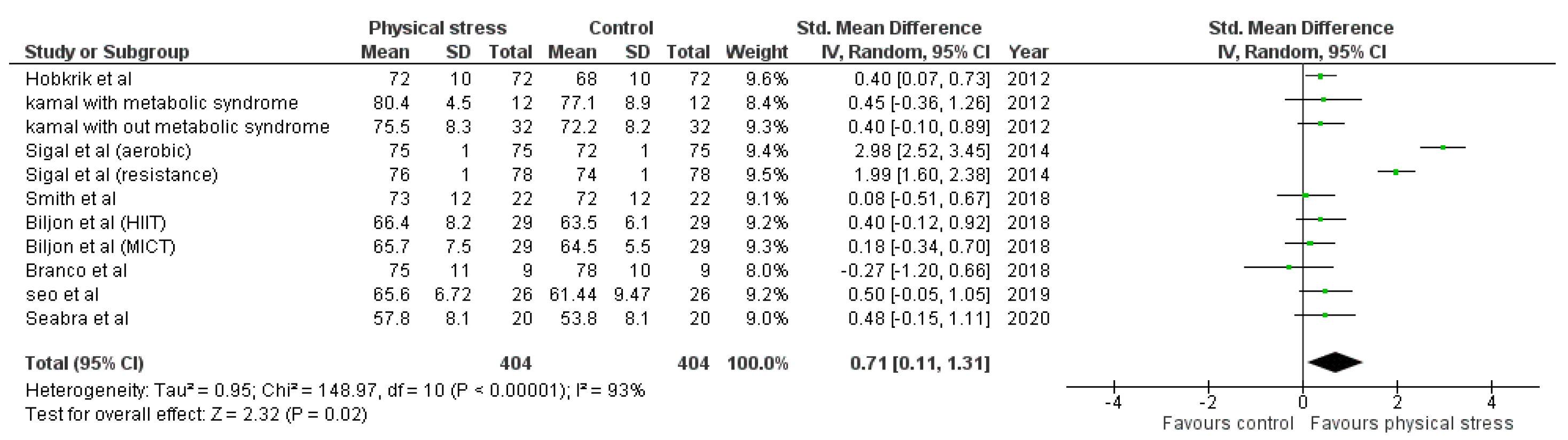
3.4.3. Diastolic Blood Pressure
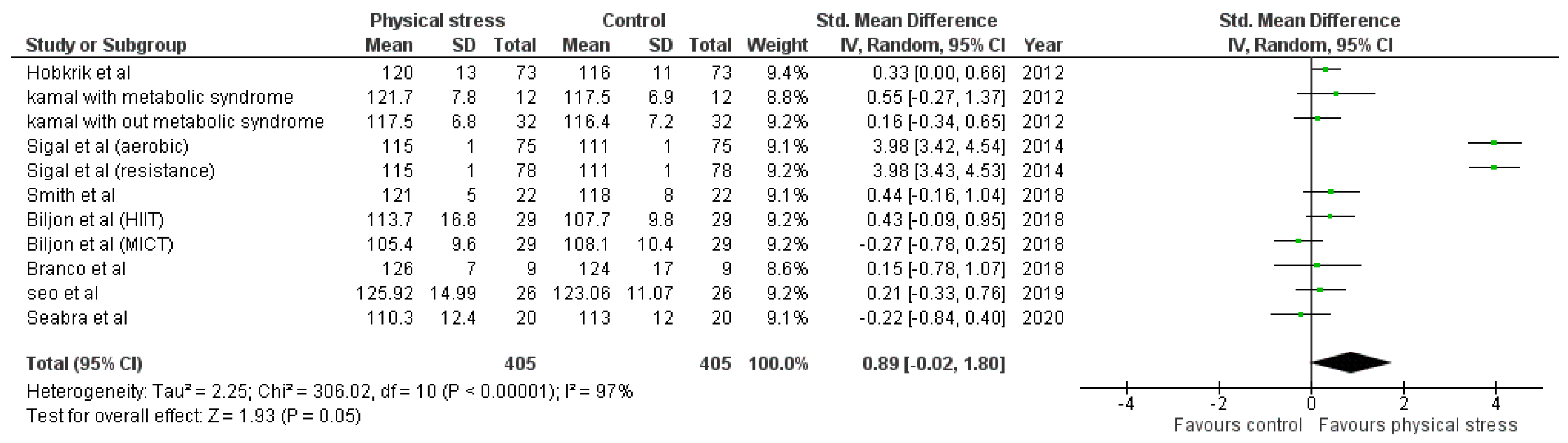
3.4.4. Systolic Blood Pressure
3.4.5. High-Density Lipoprotein (HDL)
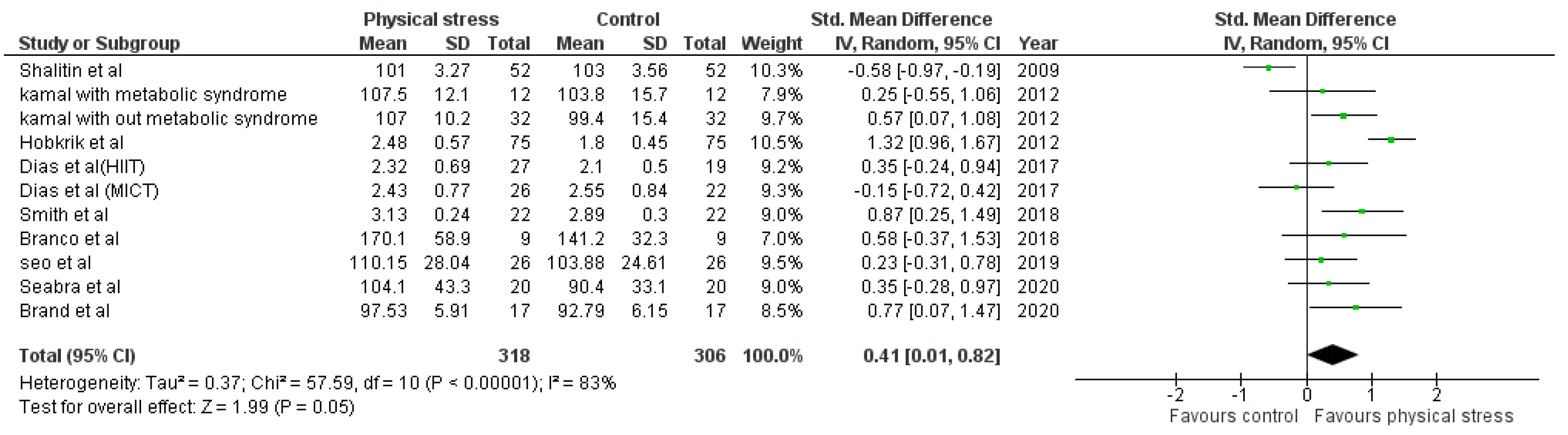
3.4.6. Low-Density Lipoprotein (LDL)
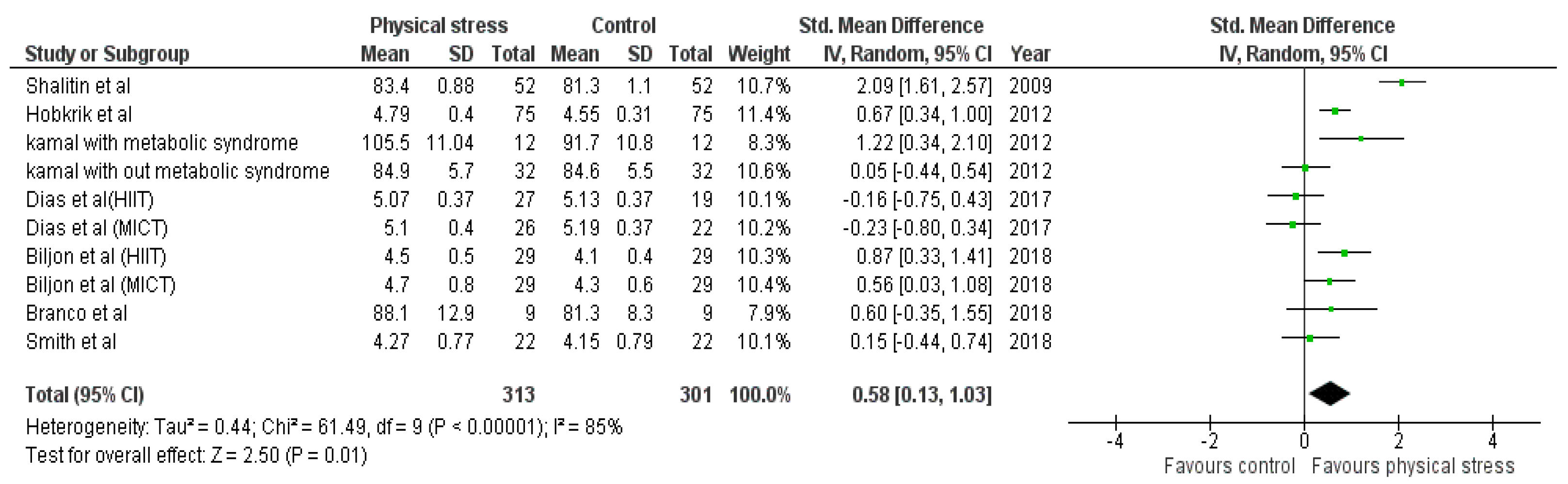
3.4.7. Blood Glucose
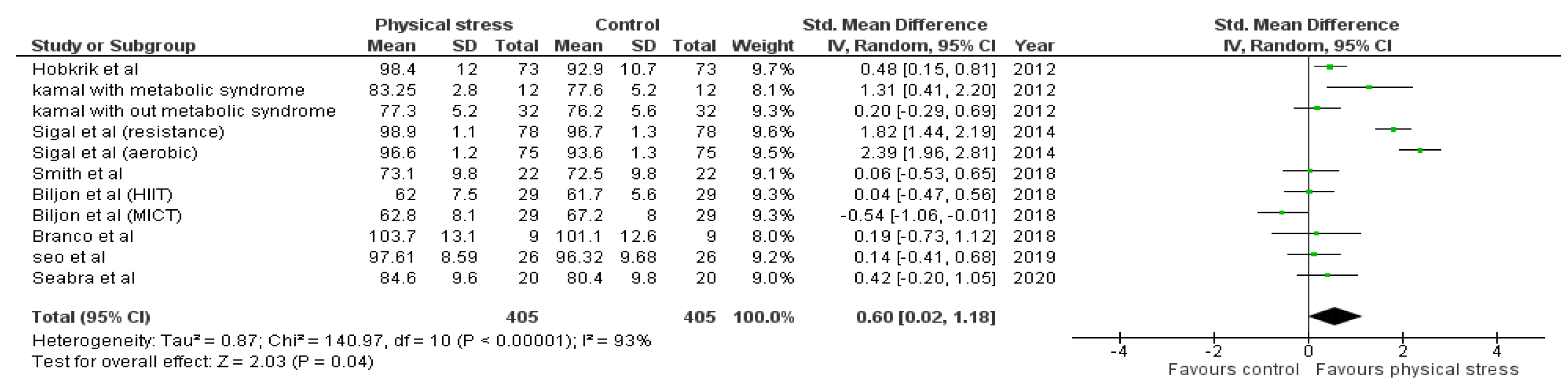
3.4.8. Waist Circumference
3.5. Sensitivity Analysis
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sabin, A.M.; Kao, K.-T.; Juonala, M.; Baur, L.; Wake, M. Viewpoint article: Childhood obesity—Looking back over 50 years to begin to look forward. J. Paediatr. Child Health 2015, 51, 82–86. [Google Scholar] [CrossRef]
- Kelsey, M.M.; Zaepfel, A.; Bjornstad, P.; Nadeau, K. Age-Related Consequences of Childhood Obesity. Gerontology 2014, 60, 222–228. [Google Scholar] [CrossRef]
- Nathan, B.M.; Moran, A. Metabolic complications of obesity in childhood and adolescence: More than just diabetes. Curr. Opin. Endocrinol. Diabetes Obes. 2008, 15, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Weihrauch-Blüher, S.; Wiegand, S. Risk Factors and Implications of Childhood Obesity. Curr. Obes. Rep. 2018, 7, 254–259. [Google Scholar] [CrossRef]
- Bass, R.; Eneli, I. Severe childhood obesity: An under-recognised and growing health problem. Postgrad. Med. J. 2015, 91, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.M. Subcutaneous and visceral adipose tissue: Structural and functional differences. Obes. Rev. 2010, 11, 11–18. [Google Scholar] [CrossRef]
- Abootorabi, M.S.; Ayremlou, P.; Behroozi-Lak, T.; Nourisaeidlou, S. The effect of vitamin D supplementation on insulin resistance, visceral fat and adiponectin in vitamin D deficient women with polycystic ovary syndrome: A randomized placebo-controlled trial. Gynecol. Endocrinol. 2018, 34, 489–494. [Google Scholar] [CrossRef]
- Rosqvist, F.; Iggman, D.; Kullberg, J.; Cedernaes, J.; Johansson, H.-E.; Larsson, A.; Johansson, L.; Ahlström, H.; Arner, P.; Dahlman, I.; et al. Overfeeding Polyunsaturated and Saturated Fat Causes Distinct Effects on Liver and Visceral Fat Accumulation in Humans. Diabetes 2014, 63, 2356–2368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Rourke, R.W. Adipose tissue and the physiologic underpinnings of metabolic disease. Surg. Obes. Relat. Dis. 2018, 14, 1755–1763. [Google Scholar] [CrossRef]
- Goossens, G.H. The Metabolic Phenotype in Obesity: Fat Mass, Body Fat Distribution, and Adipose Tissue Function. Obes. Facts 2017, 10, 207–215. [Google Scholar] [CrossRef]
- Smitka, K.; Marešová, D. Adipose Tissue as an Endocrine Organ: An Update on Pro-inflammatory and Anti-inflammatory Microenvironment. Prague Med Rep. 2015, 116, 87–111. [Google Scholar] [CrossRef] [Green Version]
- Haluzík, M.; Trachta, P.; Haluzíková, D. Hormony tukové tkáne [Adipose tissue hormones]. Vnitřní Lékařství 2010, 56, 1028–1034. [Google Scholar]
- Booth, A.; Magnuson, A.; Fouts, J.; Foster, M.T. Adipose tissue: An endocrine organ playing a role in metabolic regulation. Horm. Mol. Biol. Clin. Investig. 2016, 26, 25–42. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-Y.; Wang, P.; Miao, C.-Y. Adipokines in inflammation, insulin resistance and cardiovascular disease. Clin. Exp. Pharmacol. Physiol. 2011, 38, 888–896. [Google Scholar] [CrossRef]
- Meijer, R.I.; Serne, E.H.; Smulders, Y.M.; Van Hinsbergh, V.W.M.; Yudkin, J.S.; Eringa, E.C. Perivascular Adipose Tissue and Its Role in Type 2 Diabetes and Cardiovascular Disease. Curr. Diabetes Rep. 2011, 11, 211–217. [Google Scholar] [CrossRef] [Green Version]
- Fang, X.; Zuo, J.; Zhou, J.; Cai, J.; Chen, C.; Xiang, E.; Li, H.; Cheng, X.; Chen, P. Childhood obesity leads to adult type 2 diabetes and coronary artery diseases. Medicine 2019, 98, e16825. [Google Scholar] [CrossRef]
- Small, L.; Aplasca, A. Child Obesity and Mental Health. Child Adolesc. Psychiatr. Clin. N. Am. 2016, 25, 269–282. [Google Scholar] [CrossRef] [PubMed]
- Halfon, N.; Larson, K.; Slusser, W. Associations Between Obesity and Comorbid Mental Health, Developmental, and Physical Health Conditions in a Nationally Representative Sample of US Children Aged 10 to 17. Acad. Pediatr. 2013, 13, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Swallen, K.C.; Reither, E.N.; Haas, S.A.; Meier, A.M. Overweight, Obesity, and Health-Related Quality of Life Among Adolescents: The National Longitudinal Study of Adolescent Health. Podiatrics 2005, 115, 340–347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, I.-C.; Frangakis, C.; Wu, A.W. The relationship of excess body weight and health-related quality of life: Evidence from a population study in Taiwan. Int. J. Obes. 2006, 30, 1250–1259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kostovski, M.; Tasic, V.; Laban, N.; Polenakovic, M.; Danilovski, D.; Gucev, Z. Obesity in Childhood and Adolescence, Genetic Factors. Prilozi 2017, 38, 121–133. [Google Scholar] [CrossRef] [Green Version]
- Nielsen, L.A.; Nielsen, T.R.H.; Holm, J.-C. The Impact of Familial Predisposition to Obesity and Cardiovascular Disease on Childhood Obesity. Obes. Facts 2015, 8, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsson, E. Early Childhood Obesity Risk Factors: Socioeconomic Adversity, Family Dysfunction, Offspring Distress, and Junk Food Self-Medication. Curr. Obes. Rep. 2018, 7, 204–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, A.S.; Ge, B.; Petroski, G.; Kruse, R.L.; McElroy, J.A.; Koopman, R.J. Socioeconomic Status and Other Factors Associated with Childhood Obesity. J. Am. Board Fam. Med. 2018, 31, 514–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- An, R. Diet quality and physical activity in relation to childhood obesity. Int. J. Adolesc. Med. Health 2017, 29, 1515. [Google Scholar] [CrossRef] [PubMed]
- Solmi, M.; Ioannidis, J.P.; Carvalho, A.F. Environmental risk factors and interventions for obesity. Eur. J. Clin. Investig. 2019, 49, e13080. [Google Scholar] [CrossRef]
- Weihrauch-Blüher, S.; Schwarz, P.; Klusmann, J.-H. Childhood obesity: Increased risk for cardiometabolic disease and cancer in adulthood. Metabolism 2019, 92, 147–152. [Google Scholar] [CrossRef]
- Catalano, P.M.; Shankar, K. Obesity and pregnancy: Mechanisms of short term and long term adverse consequences for mother and child. BMJ 2017, 356, j1. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, A.; Simmonds, M.C.; Owen, C.; Woolacott, N. Childhood obesity as a predictor of morbidity in adulthood: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 56–67. [Google Scholar] [CrossRef]
- Whitlock, E.P.; Williams, S.B.; Gold, R.; Smith, P.; Shipman, S. Screening and Interventions for Childhood Overweight [In-ternet]. Rockville (MD): Agency for Healthcare Research and Quality (US). Pediatrics 2005, 116, e125–e144. [Google Scholar] [CrossRef] [Green Version]
- Stadler, J.T.; Marsche, G. Obesity-Related Changes in High-Density Lipoprotein Metabolism and Function. Int. J. Mol. Sci. 2020, 21, 8985. [Google Scholar] [CrossRef] [PubMed]
- Gurnani, M.; Birken, C.; Hamilton, J. Childhood Obesity. Pediatr. Clin. N. Am. 2015, 62, 821–840. [Google Scholar] [CrossRef]
- Frank, A. A Multidisciplinary Approach to Obesity Management: The Physician’s Role and Team Care Alternatives. J. Am. Diet. Assoc. 1998, 98, S44–S48. [Google Scholar] [CrossRef]
- Welbourn, R.; on behalf of the Guidance Development Group; Dixon, J.; Barth, J.H.; Finer, N.; Hughes, C.A.; le Roux, C.W.; Wass, J. NICE-Accredited Commissioning Guidance for Weight Assessment and Management Clinics: A Model for a Specialist Multidisciplinary Team Approach for People with Severe Obesity. Obes. Surg. 2016, 26, 649–659. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Després, J.-P. Cardiovascular and Metabolic Heterogeneity of Obesity. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef]
- Rajjo, T.; Almasri, J.; Al Nofal, A.; Farah, W.; Alsawas, M.; Ahmed, A.T.; Mohammed, K.; Kanwar, A.; Asi, N.; Wang, Z.; et al. The Association of Weight Loss and Cardiometabolic Outcomes in Obese Children: Systematic Review and Meta-regression. J. Clin. Endocrinol. Metab. 2016, 101, 4764–4768. [Google Scholar] [CrossRef]
- Skrede, T.; Steene-Johannessen, J.; Anderssen, S.A.; Resaland, G.K.; Ekelund, U. The prospective association between objectively measured sedentary time, moderate-to-vigorous physical activity and cardiometabolic risk factors in youth: A systematic review and meta-analysis. Obes. Rev. 2018, 20, 55–74. [Google Scholar] [CrossRef] [Green Version]
- García-Hermoso, A.; Urbina, A.J.C.; Herrera-Valenzuela, T.; Cristi-Montero, C.; Saavedra, J.M.; Martínez-Vizcaíno, V. Is high-intensity interval training more effective on improving cardiometabolic risk and aerobic capacity than other forms of exercise in overweight and obese youth? A meta-analysis. Obes. Rev. 2016, 17, 531–540. [Google Scholar] [CrossRef]
- Ross, L.M.; Porter, R.R.; Durstine, J.L. High-intensity interval training (HIIT) for patients with chronic diseases. J. Sport Health Sci. 2016, 5, 139–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Astorino, T.A.; Schubert, M.M. Changes in fat oxidation in response to various regimes of high intensity interval training (HIIT). Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 118, 51–63. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [Green Version]
- Cumpston, M.; Li, T.; Page, M.; Chandler, J.; Welch, A.V.; Higgins, J.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef] [Green Version]
- Seo, Y.-G.; Lim, H.; Kim, Y.; Ju, Y.-S.; Lee, H.-J.; Jang, H.B.; Park, S.I.; Park, K.H. The Effect of a Multidisciplinary Lifestyle Intervention on Obesity Status, Body Composition, Physical Fitness, and Cardiometabolic Risk Markers in Children and Adolescents with Obesity. Nutrition 2019, 11, 137. [Google Scholar] [CrossRef] [Green Version]
- Dias, K.A.; Ingul, C.B.; Tjønna, A.E.; Keating, S.E.; Gomersall, S.; Follestad, T.; Hosseini, M.S.; Hollekim-Strand, S.M.; Ro, T.B.; Haram, M.; et al. Effect of High-Intensity Interval Training on Fitness, Fat Mass and Cardiometabolic Biomarkers in Children with Obesity: A Randomised Controlled Trial. Sports Med. 2017, 48, 733–746. [Google Scholar] [CrossRef]
- Hobkirk, J.P.; King, R.F.; Gately, P.; Pemberton, P.; Smith, A.; Barth, J.H.; Carroll, S. Longitudinal Factor Analysis Reveals a Distinct Clustering of Cardiometabolic Improvements During Intensive, Short-Term Dietary and Exercise Intervention in Obese Children and Adolescents. Metab. Syndr. Relat. Disord. 2012, 10, 20–25. [Google Scholar] [CrossRef]
- Paahoo, A.; Tadibi, V.; Behpoor, N. Effect of Two Chronic Exercise Protocols on Pre-Atherosclerotic and Anti-Atherosclerotic Biomarkers Levels in Obese and Overweight Children. Iran. J. Pediatr. 2020, 30, e99760. [Google Scholar] [CrossRef] [Green Version]
- Kamal, N.N.; Ragy, M.M. The effects of exercise on C-reactive protein, insulin, leptin and some cardiometabolic risk factors in Egyptian children with or without metabolic syndrome. Diabetol. Metab. Syndr. 2012, 4, 27. [Google Scholar] [CrossRef] [Green Version]
- Branco, B.H.M.; Carvalho, I.Z.; de Oliveira, H.G.; Fanhani, A.P.; dos Santos, M.C.M.; de Oliveira, L.P.; Boni, S.M.; Nardo, N., Jr. Effects of 2 Types of Resistance Training Models on Obese Adolescents’ Body Composition, Cardiometabolic Risk, and Physical Fitness. J. Strength Cond. Res. 2020, 34, 2672–2682. [Google Scholar] [CrossRef]
- Martin-Smith, R.; Buchan, D.S.; Baker, J.S.; Macdonald, M.J.; Sculthorpe, N.F.; Easton, C.; Knox, A.; Grace, F.M. Sprint Interval Training and the School Curriculum: Benefits Upon Cardiorespiratory Fitness, Physical Activity Profiles, and Cardiometabolic Risk Profiles of Healthy Adolescents. Pediatr. Exerc. Sci. 2019, 31, 296–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seabra, A.; Brito, J.; Figueiredo, P.; Beirão, L.; Seabra, A.; Carvalho, M.J.; Abreu, S.; Vale, S.; Pedretti, A.; Nascimento, H.; et al. School-based soccer practice is an effective strategy to improve cardiovascular and metabolic risk factors in overweight children. Prog. Cardiovasc. Dis. 2020, 63, 807–812. [Google Scholar] [CrossRef] [PubMed]
- Shalitin, S.; Ashkenazi-Hoffnung, L.; Yackobovitch-Gavan, M.; Nagelberg, N.; Karni, Y.; Hershkovitz, E.; Loewenthal, N.; Shtaif, B.; Gat-Yablonski, G.; Phillip, M. Effects of a Twelve-Week Randomized Intervention of Exercise and/or Diet on Weight Loss and Weight Maintenance, and Other Metabolic Parameters in Obese Preadolescent Children. Horm. Res. 2009, 72, 287–301. [Google Scholar] [CrossRef] [PubMed]
- Sigal, R.J.; Alberga, A.S.; Goldfield, G.S.; Prud’Homme, D.; Hadjiyannakis, S.; Gougeon, R.; Phillips, P.; Tulloch, H.; Malcolm, J.; Doucette, S.; et al. Effects of Aerobic Training, Resistance Training, or Both on Percentage Body Fat and Cardiometabolic Risk Markers in Obese Adolescents: The Healthy Eating Aerobic and Resistance Training in Youth Randomized Clinical Trial. JAMA Pediatr. 2014, 168, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Van Biljon, A.; McKune, A.J.; DuBose, K.D.; Kolanisi, U.; Semple, S.J. Do Short-Term Exercise Interventions Improve Cardiometabolic Risk Factors in Children? J. Pediatr. 2018, 203, 325–329. [Google Scholar] [CrossRef]
- Brand, C.; Martins, C.M.D.L.; Lemes, V.B.; Pessoa, M.L.F.; Dias, A.F.; Cadore, E.L.; Mota, J.; Gaya, A.C.A.; Gaya, A.R. Effects and prevalence of responders after a multicomponent intervention on cardiometabolic risk factors in children and adolescents with overweight/obesity: Action for health study. J. Sports Sci. 2020, 38, 682–691. [Google Scholar] [CrossRef]
- Ho, M.; Garnett, S.P.; Baur, L.; Burrows, T.; Stewart, L.; Neve, M.; Collins, C. Effectiveness of Lifestyle Interventions in Child Obesity: Systematic Review with Meta-analysis. Pediatrics 2012, 130, e1647–e1671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batacan, R.B.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef]
- Thivel, D.; Masurier, J.; Baquet, G.; Timmons, B.W.; Pereira, B.; Berthoin, S.; Duclos, M.; Aucouturier, J. High-intensity interval training in overweight and obese children and adolescents: Systematic review and meta-analysis. J. Sports Med. Phys. Fit. 2019, 59, 310–324. [Google Scholar] [CrossRef]
- Pozuelo-Carrascosa, D.P.; Cavero-Redondo, I.; Herraiz-Adillo, Á.; Fernández, A.D.; López, M.S.; Martínez-Vizcaíno, V. School-Based Exercise Programs and Cardiometabolic Risk Factors: A Meta-analysis. Pediatrics 2018, 142, e20181033. [Google Scholar] [CrossRef] [Green Version]
- Díaz, M.; Bassols, J.; López-Bermejo, A.; De Zegher, F.; Ibáñez, L. Metformin treatment to reduce central adiposity after prenatal growth restraint: A placebo-controlled pilot study in prepubertal children. Pediatr. Diabetes 2014, 16, 538–545. [Google Scholar] [CrossRef]
- Bassols, J.; Martínez-Calcerrada, J.-M.; Osiniri, I.; Díaz-Roldán, F.; Xargay-Torrent, S.; Mas-Parés, B.; Dorado-Ceballos, E.; Prats-Puig, A.; Carreras-Badosa, G.; De Zegher, F.; et al. Effects of metformin administration on endocrine-metabolic parameters, visceral adiposity and cardiovascular risk factors in children with obesity and risk markers for metabolic syndrome: A pilot study. PLoS ONE 2019, 14, e0226303. [Google Scholar] [CrossRef]
- Partsalaki, I.; Karvela, A.; Spiliotis, B.E. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2012, 25, 697–704. [Google Scholar] [CrossRef]
- Macknin, M.; Kong, T.; Weier, A.; Worley, S.; Tang, A.S.; Alkhouri, N.; Golubic, M. Plant-Based, No-Added-Fat or American Heart Association Diets: Impact on Cardiovascular Risk in Obese Children with Hypercholesterolemia and Their Parents. J. Pediatr. 2015, 166, 953–959.e3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajakumar, K.; Moore, C.G.; Khalid, A.T.; Vallejo, A.N.; Virji, A.M.; Holick, M.F.; Greenspan, S.L.; Arslanian, S.; Reis, E.S. Effect of vitamin D3 supplementation on vascular and metabolic health of vitamin D–deficient overweight and obese children: A randomized clinical trial. Am. J. Clin. Nutr. 2020, 111, 757–768. [Google Scholar] [CrossRef] [PubMed]
- Specht, I.O.; Rohde, J.F.; Olsen, N.J.; Heitmann, B.L. Duration of exclusive breastfeeding may be related to eating behaviour and dietary intake in obesity prone normal weight young children. PLoS ONE 2018, 13, e0200388. [Google Scholar] [CrossRef] [Green Version]
- Dalrymple, K.V.; Flynn, A.C.; Seed, P.T.; Briley, A.L.; O’Keeffe, M.; Godfrey, K.M.; Poston, L. Associations between dietary patterns, eating behaviours, and body composition and adiposity in 3-year-old children of mothers with obesity. Pediatr. Obes. 2020, 15, e12608. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.E.; Lytle, L.A.; Laska, M.N. Stress, Health Risk Behaviors, and Weight Status among Community College Students. Health Educ. Behav. 2015, 43, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Brady, E.; Bodicoat, D.; Hall, A.; Khunti, K.; Yates, T.; Edwardson, C.; Davies, M. Sleep duration, obesity and insulin resistance in a multi-ethnic UK population at high risk of diabetes. Diabetes Res. Clin. Prac. 2018, 139, 195–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, B.; Gray, A.; Galland, B.; Heath, A.-L.M.; Lawrence, J.; Sayers, R.M.; Cameron, S.; Hanna, M.; Dale, K.; Coppell, K.; et al. Targeting Sleep, Food, and Activity in Infants for Obesity Prevention: An RCT. Pediatrics 2017, 139, e20162037. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stoner, L.; Rowlands, D.; Morrison, A.; Credeur, D.; Hamlin, M.; Gaffney, K.; Lambrick, D.; Matheson, A. Efficacy of Exercise Intervention for Weight Loss in Overweight and Obese Adolescents: Meta-Analysis and Implications. Sports Med. 2016, 46, 1737–1751. [Google Scholar] [CrossRef] [Green Version]
- Tyson, N.; Frank, M. Childhood and adolescent obesity definitions as related to BMI, evaluation and management options. Best Pr. Res. Clin. Obstet. Gynaecol. 2018, 48, 158–164. [Google Scholar] [CrossRef]
- Gutin, I. In BMI we trust: Reframing the body mass index as a measure of health. Soc. Theory Health 2018, 16, 256–271. [Google Scholar] [CrossRef] [PubMed]
- Bosello, O.; Donataccio, M.P.; Cuzzolaro, M. Obesity or obesities? Controversies on the association between body mass index and premature mortality. Eat. Weight. Disord. Stud. Anorexia Bulim. Obes. 2016, 21, 165–174. [Google Scholar] [CrossRef]
- Trinh, A.; Campbell, M.; Ukoumunne, O.C.; Gerner, B.; Wake, M. Physical Activity and 3-Year BMI Change in Overweight and Obese Children. Pediatrics 2013, 131, e470–e477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suceveanu, A.-I.; Mazilu, L.; Katsiki, N.; Parepa, I.; Voinea, F.; Pantea-Stoian, A.; Rizzo, M.; Botea, F.; Herlea, V.; Serban, D.; et al. NLRP3 Inflammasome Biomarker—Could Be the New Tool for Improved Cardiometabolic Syndrome Outcome. Metabolites 2020, 10, 448. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, M.; Hosseini-Fard, R.; Najafi, M. Circulating low density lipoprotein (LDL). Horm. Mol. Biol. Clin. Investig. 2018, 35, 20180024. [Google Scholar] [CrossRef]
- Naito, R.; Miyauchi, K. Coronary Artery Disease and Type 2 Diabetes Mellitus. Int. Heart J. 2017, 58, 475–480. [Google Scholar] [CrossRef] [Green Version]
- Hartley, A.; Haskard, D.; Khamis, R. Oxidized LDL and anti-oxidized LDL antibodies in atherosclerosis—Novel insights and future directions in diagnosis and therapy. Trends Cardiovasc. Med. 2019, 29, 22–26. [Google Scholar] [CrossRef]
- Luo, Y.; Duan, H.; Qian, Y.; Feng, L.; Wu, Z.; Wang, F.; Feng, J.; Yang, D.; Qin, Z.; Yan, X. Macrophagic CD146 promotes foam cell formation and retention during atherosclerosis. Cell Res. 2017, 27, 352–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, L.X.; Que, X.M.; Gao, X.; Wang, T. Childhood obesity and coronary artery disease: A Mendelian randomization study. Front. Genet. 2019, 40, 839–843. [Google Scholar]
- Gomes, F.; Telo, D.F.; Souza, H.P.; Nicolau, J.C.; Halpern, A.; Serrano, C.V., Jr. Obesidade e doença arterial coronariana: Papel da inflamação vascular. Arquivos Brasileiros de Cardiologia 2010, 94, 273–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO); Office of World Health Reporting. The World Health Report: 2002: Reducing Risks, Promoting Healthy Life: Overview; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Berchtold, P.; Jörgens, V.; Kemmer, F.W.; Berger, M. Obesity and hypertension: Cardiovascular response of weight reduction. Hypertension 1982, 4, III50–III55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dascalu, A.M.; Stoian, A.P.; Cherecheanu, A.P.; Serban, D.; Costea, D.O.; Tudosie, M.S.; Stana, D.; Tanasescu, D.; Sabau, A.D.; Gangura, G.A.; et al. Outcomes of Diabetic Retinopathy Post-Bariatric Surgery in Patients with Type 2 Diabetes Mellitus. J. Clin. Med. 2021, 10, 3736. [Google Scholar] [CrossRef] [PubMed]


| Search Engine | Search Strategy |
|---|---|
| Pubmed/Medline | (“exercise”[MeSH Terms] OR “exercise”[All Fields] OR (“physical”[All Fields] AND “exercise”[All Fields]) OR “physical exercise”[All Fields] OR (“workout”[All Fields] OR “workouts”[All Fields]) OR (“physical exertion”[MeSH Terms] OR (“physical”[All Fields] AND “exertion”[All Fields]) OR “physical exertion”[All Fields])) AND (“cardiometabolic”[All Fields] OR “cardiometabolically”[All Fields]) AND (“risk factors”[MeSH Terms] OR (“risk”[All Fields] AND “factors”[All Fields]) OR “risk factors”[All Fields] OR (“causality”[MeSH Terms] OR “causality”[All Fields] OR (“predisposing”[All Fields] AND “factor”[All Fields]) OR “predisposing factor”[All Fields]) OR ((“predict”[All Fields] OR “predictabilities”[All Fields] OR “predictability”[All Fields] OR “predictable”[All Fields] OR “predictably”[All Fields] OR “predicted”[All Fields] OR “predicting”[All Fields] OR “prediction”[All Fields] OR “predictions”[All Fields] OR “predictive”[All Fields] OR “predictively”[All Fields] OR “predictiveness”[All Fields] OR “predictives”[All Fields] OR “predictivities”[All Fields] OR “predictivity”[All Fields] OR “predicts”[All Fields]) AND (“factor”[All Fields] OR “factor s”[All Fields] OR “factors”[All Fields]))) AND (“child”[MeSH Terms] OR “child”[All Fields] OR “children”[All Fields] OR “child s”[All Fields] OR “children s”[All Fields] OR “childrens”[All Fields] OR “childs”[All Fields] OR (“young”[All Fields] OR “youngs”[All Fields]) OR (“adolescences”[All Fields] OR “adolescency”[All Fields] OR “adolescent”[MeSH Terms] OR “adolescent”[All Fields] OR “adolescence”[All Fields] OR “adolescents”[All Fields] OR “adolescent s”[All Fields]) OR (“adolescent”[MeSH Terms] OR “adolescent”[All Fields] OR “youth”[All Fields] OR “youths”[All Fields] OR “youth s”[All Fields]) OR (“adolescent”[MeSH Terms] OR “adolescent”[All Fields] OR “teenage”[All Fields] OR “teenager”[All Fields] OR “teenagers”[All Fields] OR “teenaged”[All Fields] OR “teenager s”[All Fields] OR “teenages”[All Fields])) |
| Cochrane | ((physical exercise OR workout OR physical exertion) AND (cardiometabolic)) AND (risk factors OR predisposing Factor OR predictive factors) AND (children OR young OR adolescent OR youth OR teenagers) |
| Google Scholar | ((physical exercise OR workout OR physical exertion) AND (cardiometabolic)) AND (risk factors OR predisposing Factor OR predictive factors) AND (children OR young OR adolescent OR youth OR teenagers) |
| Authors | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total Score | Methodological Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Seo et al. [43] | Y | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 8 | High |
| Dias et al. [44] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Hobkrik et al. [45] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Paahoo et al. [46] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Kamal et al. [47] | Y | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 | Low |
| Branco et al. [48] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Smith et al. [49] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Seabra et al. [50] | Y | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 4 | Low |
| Shalitin et al. [51] | Y | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | High |
| Author | Country | Total Sample by Gender (n) | Age (Years) (M ± SD) | Groups (n) | Body Fat (%) | Body Mass (kg) | BMI (kg/m2) | Registered Protocol |
|---|---|---|---|---|---|---|---|---|
| Seo et al., 2019 [43] | Korea | 25F | CG = 12.09 ± 2.20 | CG = 44 | CG = 41.26 ± 4.25 | CG = 72.1 ± 19.88 | CG = 29.43 ± 4.81 | Yes |
| EG = 12.8 ± 1.72 | EG = 26 | EG = 41.77 ± 4.23 | EG = 77.4 ± 11.34 | EG = 30.06 ± 3.40 | ||||
| Dias et al. 2017 [44] | Australia | 103F | CG = 11.5 ± 2.4 | CG = 100 | CG = 44.1 ± 6.2 | CG = 31.3 ± 10.6 | CG = 29.5 ± 4.4 | Yes |
| EG = 12.0 ± 2.3 | EG = 99 | EG = 19.5 ± 7.5 | EG = 7.7 ± 3.6 | EG = 17.6 ± 2.1 | ||||
| Hobkrik et al., 2016 [45] | United Kingdom | N/R | N/R | 75 | N/R | 94.2 ± 22.1 | 34. 2 ± 6.4 | N/R |
| Pahoo et al., 2020 [46] | Iran | N/R | CG = 11.20 ± 0.94 | CG = 15 | CG = 27.88 ± 1.06 | CG = 54.20 ± 4.45 | CG = 25.02 ± 1.89 | N/R |
| HIITG = 11.13 ± 0.99 | HIITG = 15 | HIITG = 28.04 ± 1.46 | HIITG = 56.00 ± 4.51 | HIITG = 25.33 ± 1.01 | ||||
| AG = 10.86 ± 1.06 | AG = 15 | AG = 27.87 ± 1.06 | AG = 55.06 ± 3.75 | AG = 25.01 ± 0.69 | ||||
| Kamal et al., 2012 [47] | Egypt | 40F | CG = 10.1 ± 1.21 | CG = 49 | N/R | CG = 62.6 ± 4.1 | CG = 67.1 ± 6.3 | N/R |
| EG without MS = 10.2 ± 1.2 | EG without MS = 32 | EG without MS = 50.2 ± 3.7 | EG without MS = 17.2 ± 2.5 | |||||
| EG with MS = 11.04 ± 1.15 | EG with MS = 12 | EG with MS = 67.1 ± 6.3 | EG with MS = 29.4 ± 4.8 | |||||
| Branco et al., 2016 [48] | Brazil | N/R | FG = 16 ± 1 | FG = 9 | FG = 43.9 ± 4 | FG = 99 ± 20.5 | FG = 34.7 ± 3.8 | Yes |
| WG = 16 ± 1 | WG = 9 | WG = 38.7 ± 9.2 | WG = 97.8 ± 24.2 | WG = 33.2 ± 8.3 | ||||
| Smith et al., 2017 [49] | United Kingdom | 20F | CG = 16.8 ± 0.5 | CG = 30 | N/R | CG = 66.2 ± 13.8 | CG = 21.8 ± 2.1 | N/R |
| EG = 17 ± 0.3 | EG = 22 | EG = 67.1 ± 14.4 | EG = 22.5 ± 2.5 | |||||
| Seabra et al., 2020 [50] | Germany | 40M | CG = 10.1 ± 1.5 | CG = 20 | CG = 35.1 ± 8.3 | CG = 57.6 ± 15.7 | N/R | N/R |
| EG = 10.5 ± 1.5 | EG = 20 | EG = 34.4 ± 6 | EG = 54.5 ± 13.4 | |||||
| Shalitin et al., 2009 [51] | Israel | 81F | EG = 8.21 ± 1.78 | EG = 52 | EG = 41.2 ± 1.36 | EG = 46 ± 1.6 | EG = 25.5 ± 0.52 | N/R |
| D + EG = 8.2 ± 1.56 | D + EG = 55 | D + EG = 41.3 ± 1.3 | D + EG = 46.4 ± 1.51 | D + EG = 25.9 ± 0.51 | ||||
| DG = 8.51 ± 1.52 | DG = 55 | DG = 43.1 ± 1.24 | DG = 47.5 ± 1.52 | DG = 25.5 ± 0.52 | ||||
| Sigal et al., 2014 [52] | Canada | 213F | AG = 15.5 ± 1.4 | AG = 75 | AG = 47.1 ± 1.3 | AG = 97.1 ± 1.8 | AG = 34.7 ± 0.5 | N/R |
| RG = 15.9 ± 1.5 | RG = 78 | RG = 48 ± 1.3 | RG = 100.1 ± 1.7 | RG = 35.1 ± 0.5 | ||||
| CTG = 15.5 ± 1.3 | CTG = 75 | CTG = 48.4 ± 1.3 | CTG = 97.8 ± 1.8 | CTG = 34.7 ± 0.5 | ||||
| CG = 15.6 ± 1.3 | CG = 76 | CG = 46.6 ± 1.3 | CG = 97.9 ± 1.8 | CG = 34.2 ± 0.5 | ||||
| Biljon et al., 2018 [53] | South Africa | 67F | 11.1 ± 0.8 | MICTG = 29 | N/R | MICTG = 41.0 ± 10.6 | MICTG = 19.2 ± 3.5 | N/R |
| HIITG = 29 | HIITG = 41.0 ± 10.6 | HIITG = 18.5 ± 3.2 | ||||||
| MICTG + HIITG = 27 | MICTG + HIITG = 38.7 ± 9.3 | MICTG + HIITG = 18.0 ± 3.8 | ||||||
| CG = 24 | CG = 42.6 ± 9.6 | CG = 20.3 ± 3.7 | ||||||
| Brand et al., 2020 [54] | Brazil | 22F | CG = 8.27 | CG = 18 | CG = 14.13 | CG = 39.29 | CG = 21.88 | Yes |
| EG = 8.17 | EG = 17 | EG = 13.6 | EG = 40.9 | EG = 21.97 |
| Author | Exercise Modality | Exercise (Names) | Frequency (Days/Week) | Intensity | Sets/Exercise (n) | Reps per Set (n) | Rest | Intervention Duration (Weeks) | Session Duration (min) | Eccentric Velocity (s) | Supervised? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Seo et al., 2019 [43] | Cardio training | Aerobic exercise and ICAAN exercise | 3 | moderate-intensity intervention | N/R | N/R | 30–40 s | 16 | 60 | N/R | Yes |
| Dias et al. [44] | Cardio training | treadmill | 3 | High- and Moderate-Intensity Interval Training | N/R | N/R | 3 min | 12 weeks | 36 (High intensity) 44 (Moderate intensity) | N/R | Yes |
| Hobkrik et al. [45] | Cardio training | N/R | N/R | N/R | N/R | N/R | N/A | 4 | N/R | N/R | Yes |
| Pahoo et al. [46] | Cardio training and Flexibility | warm-up and other exercise | 3 | High-Intensity Interval Training and Aerobic Exercise | 3 | N/R | 5 min | 12 | 45 | N/R | Yes |
| Kamal et al. [47] | Cardio training | warm-up, walking–jogging, and relaxation exercises | 3 | N/R | N/R | N/R | N/R | 12 weeks | 30–65 | N/R | Yes |
| Branco et al. [48] | Cardio training and Strength training | warm-up, CP, HS, SP, Leg extension, Triceps pulley, ACM, OAM, Scott curl machine, Aerobics, CRM, Incline row, Leg curl, LCGP, Push-ups, SWS, MBV, GUD, Triceps bench dips, SSU, HLKF, RTRX, TPNR, BTRX, OSSB | 3 | High- and Moderate- Intensity Interval Training | 3 | N/R | 3 min | 12 weeks | 46 | N/R | |
| Smith et al. [49] | Cardio training | “all out” running sprints | 3 | Sprint Interval Training | 5–6 | N/R | 30 s | 4 weeks | 4.5–5.5 | N/R | Yes |
| Seabra et al. [50] | Cardio training | soccer | 2 | N/R | N/R | N/R | 10 min | 6 months | 60–90 | N/R | Yes |
| Shalitin et al. [51] | Cardio training and Strength training | Sports, running games, sit-ups, hand-lifting of small weights, and ball exercise | 3 | Aerobic exercise and resistance training exercises | N/R | N/R | N/R | 12 weeks | 45 (each group) | N/R | Yes |
| Sigal et al. [52] | Cardio training and Strength training | Gymnasiums, weight machines or free weights | 2–4 | aerobic and resistance training | 2–3 | 8–15 | N/R | 6 months | 20–45 | N/R | Yes |
| Biljon et al. [53] | Cardio training | Warm-up and cool-down periods consisting of jogging at a low intensity, followed by static stretching | 3 | High- and Moderate- Intensity Interval Training | N/R | N/R | 5 min | 5 weeks | 23 (High intensity) 33 (Moderate intensity) | N/R | Yes |
| Brand et al. [54] | Multicomponent | Exercise | 2 | N/R | N/R | N/R | N/R | 12 weeks | 60 | N/R | Yes |
| Factors | No. of Studies | Odds Ratio (OR 95% CI) | p-Value | Heterogeneity (I2) |
|---|---|---|---|---|
| (n) | (%) | |||
| Body weight | 7 | 0.11 95% CI −0.05, 0.28 | 0.18 | 27 |
| BMI | 8 | 0.38 95% CI 0.14, 0.62 | 0.002 | 65 |
| Diastolic blood pressure | 8 | 0.71 95% CI 0.11, 1.31 | 0.02 | 93 |
| Systolic blood pressure | 8 | 0.89 95% CI −0.02, 1.80 | 0.05 | 97 |
| High-density lipoprotein | 10 | −0.48 95% CI −1.06, 0.11 | 0.11 | 92 |
| Low-density lipoprotein | 9 | 0.41 95% CI 0.01, 0.82 | 0.05 | 83 |
| Blood glucose | 7 | 0.58 95% CI 0.13, 1.03 | 0.01 | 85 |
| Waist circumference | 8 | 0.60 95% CI 0.02, 1.18 | 0.04 | 93 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Busnatu, S.S.; Serbanoiu, L.I.; Lacraru, A.E.; Andrei, C.L.; Jercalau, C.E.; Stoian, M.; Stoian, A. Effects of Exercise in Improving Cardiometabolic Risk Factors in Overweight Children: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 82. https://doi.org/10.3390/healthcare10010082
Busnatu SS, Serbanoiu LI, Lacraru AE, Andrei CL, Jercalau CE, Stoian M, Stoian A. Effects of Exercise in Improving Cardiometabolic Risk Factors in Overweight Children: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(1):82. https://doi.org/10.3390/healthcare10010082
Chicago/Turabian StyleBusnatu, Stefan Sebastian, Liviu Ionut Serbanoiu, Andreea Elena Lacraru, Catalina Liliana Andrei, Cosmina Elena Jercalau, Marilena Stoian, and Anca Stoian. 2022. "Effects of Exercise in Improving Cardiometabolic Risk Factors in Overweight Children: A Systematic Review and Meta-Analysis" Healthcare 10, no. 1: 82. https://doi.org/10.3390/healthcare10010082







