Association between Sleep Quality and Physical Activity in Physical Education Students in Chile in the Pandemic Context: A Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Setting and Design
2.2. Instruments
2.3. Statistical Analysis
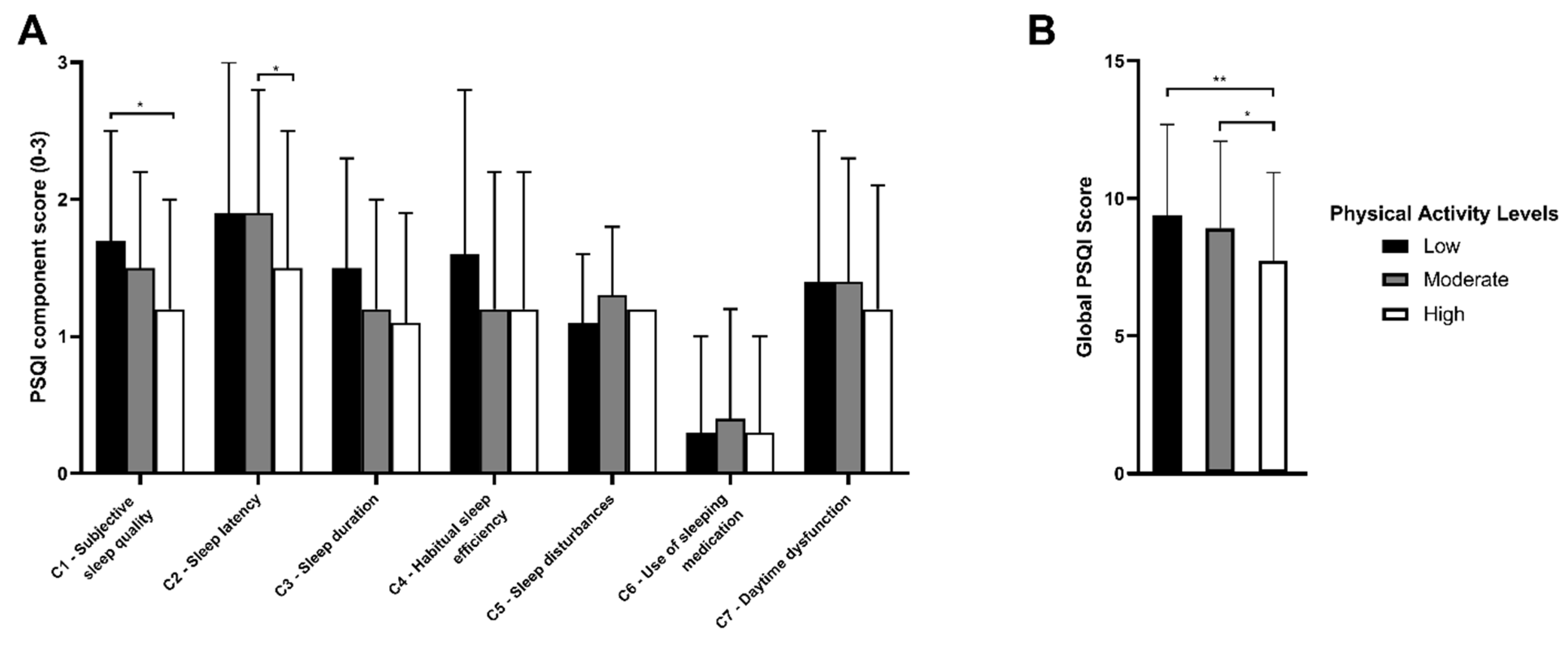
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Almeida, I.M. Proteção da saúde dos trabalhadores da saúde em tempos de COVID-19 e respostas à pandemia. Rev. Bras. Saúde Ocup. 2020, 45, e17. [Google Scholar] [CrossRef]
- Castillo, A.E.; Parra, B.; Tapia, P.; Acevedo, A.; Lagos, J.; Andrade, W.; Arata, L.; Leal, G.; Barra, G.; Tambley, C.; et al. Phylogenetic analysis of the first four SARS-CoV-2 cases in Chile. J. Med. Virol. 2020, 92, 1562–1566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diez, C.S.; Macho, R.M.; López, J.A.; Peña, K.M.; Lüer, M.C.; González, M.C. Early experience with severely burned COVID-19 patients at the National Reference Center for adult major burns in Chile. Burns 2020, 47, 1208–1211. [Google Scholar] [CrossRef]
- WHO. Novel Coronavirus. Situat. Rep. 2020, 205, 1–19. [Google Scholar]
- Chen, P.; Mao, L.; Nassis, G.P.; Harmer, P.; Ainsworth, B.E.; Li, F. Coronavirus disease (COVID-19): The need to maintain regular physical activity while taking precautions. J. Sport Health Sci. 2020, 9, 103–104. [Google Scholar] [CrossRef]
- Hughes, D.; Saw, R.; Perera, N.K.P.; Mooney, M.; Wallett, A.; Cooke, J.; Coatsworth, N.; Broderick, C. The Australian Institute of Sport framework for rebooting sport in a COVID-19 environment. J. Sci. Med. Sport 2020, 23, 639–663. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- Li, Y.; Qin, Q.; Sun, Q.; Sanford, L.D.; Vgontzas, A.N.; Tang, X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 2020, 16, 1417–1418. [Google Scholar] [CrossRef]
- Robbins, R.; Grandner, M.A.; Buxton, O.M.; Hale, L.; Buysse, D.J.; Knutson, K.; Patel, S.; Troxel, W.M.; Youngstedt, S.D.; Czeisler, C.A.; et al. Sleep myths: An expert-led study to identify false beliefs about sleep that impinge upon population sleep health practices. Sleep Health 2019, 5, 409–417. [Google Scholar] [CrossRef]
- Robotham, D. Sleep as a public health concern: Insomnia and mental health. J. Public Ment. Health 2011, 10, 234–237. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Buchanan, J.L. Prevention of Depression in the College Student Population: A Review of the Literature. Arch. Psychiatr. Nurs. 2012, 26, 21–42. [Google Scholar] [CrossRef]
- Majumdar, P.; Biswas, A.; Sahu, S. COVID-19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 2020, 37, 1191–1200. [Google Scholar] [CrossRef]
- Becker, S.P.; Jarrett, M.A.; Luebbe, A.M.; Garner, A.A.; Burns, G.L.; Kofler, M.J. Sleep in a large, multi-university sample of college students: Sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 2018, 4, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Kenney, S.R.; LaBrie, J.W.; Hummer, J.F.; Pham, A.T. Global sleep quality as a moderator of alcohol consumption and consequences in college students. Addict. Behav. 2012, 37, 507–512. [Google Scholar] [CrossRef] [Green Version]
- Orzech, K.M.; Salafsky, D.B.; Hamilton, L.A. The State of Sleep among College Students at a Large Public University. J. Am. Coll. Health 2011, 59, 612–619. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.A.; Najman, J.M.; Mamun, A.A. Exploring ender difference in sleep quality of young adults: Findings from large population study. Clin. Med. Res. 2016, 14, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Mallampalli, M.; Carter, C. Exploring sex and gender differences in sleep health: A society for women health research report. J. Women’s Health 2014, 7, 553–562. [Google Scholar] [CrossRef] [Green Version]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2020, 268, 8–15. [Google Scholar] [CrossRef]
- Podhorecka, M.; Androsiuk-Perkowska, J.; Marta, P.; Magdalena, C.; Dominika, G.; Radosław, P.; Joanna, A.-P.; Alina, J.; Emilia, G.-S.; Remigiusz, S.; et al. Can physical activity influence the quality of sleep among the elderly? J. Educ. Health Sport 2017, 7, 288–305. [Google Scholar]
- Kelley, G.A.; Kelley, K.S. Exercise and sleep: A systematic review of previous meta-analyses. J. Evid. Based Med. 2017, 10, 26–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kredlow, M.A.; Capozzoli, M.C.; Hearon, B.A.; Calkins, A.W.; Otto, M.W. The effects of physical activity on sleep: A meta-analytic review. J. Behav. Med. 2015, 38, 427–449. [Google Scholar] [CrossRef] [PubMed]
- Ghrouz, A.K.; Noohu, M.M.; Dilshad, M.; Spence, D.; BaHammam, A.S.; Pandi-Perumal, S.R. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019, 23, 627–634. [Google Scholar] [CrossRef] [PubMed]
- Badicu, G. Physical activity and sleep quality in students of the Faculty of Physical Education and Sport of Braşov, Romania. Sustainability 2018, 10, 2410. [Google Scholar] [CrossRef] [Green Version]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Chang, S.; Cheng, Y. Relationships between sleep quality, physical fitness and body mass index in college freshmen. J. Sport Phys. Fit. 2015, 55, 1234–1241. [Google Scholar]
- Olivares, C.S.; Lera, M.L.; Bustos, Z.N. Etapas del cambio, beneficios y barreras en actividad física y consumo de frutas y verduras en estudiantes universitarios de Santiago de Chile. Rev. Chil. Nutr. 2008, 35, 25–35. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, F.; Cristi-Montero, C.; Villa-González, E.; Solís-Urra, P.; Chillón, P. Comparación de los niveles de actividad física durante la vida universitaria. Rev. Med. Chile 2018, 146, 442–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luciano, F.; Cenacchi, V.; Vegro, V.; Pavei, G. COVID-19 lockdown: Physical activity, sedentary behaviour and sleep in Italian medicine students. Eur. J. Sport Sci. 2021, 21, 1459–1468. [Google Scholar] [CrossRef]
- Dongol, E.; Shaker, K.; Abbas, A.; Assar, A.; Abdelraoof, M.; Saady, E.; Hassan, A.; Youssef, O.; Essam, M.; Mahmoud, M.; et al. Sleep quality, stress level and COVID-19 in university students; the forgotten dimension. Sleep Sci. 2022, 15, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Bustamante-Ara, N.; Russell, J.; Godoy-Cumillaf, A.; Merellano-Navarro, E.; Uribe, N. Rendimiento académico, actividad física, sueño y género en universitarios durante la pandemia-2020. Cult. Cienc. Deporte 2022, 17, 109–131. [Google Scholar]
- Xu, F.; Adams, S.; Cohen, S.; Earp, J.; Greaney, M. Relationship between Physical Activity, Screen Time, and Sleep Quantity and Quality in US Adolescents Aged 16–19. Int. J. Environ. Res. Public Health 2019, 30, 1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zangiacomi, E.; Mabelle, F.; Zanin, T.; Lucindo, M.; Lucena, T.; Gregorio, A. Atividade física em períodos de distanciamento social devidos à COVID-19: Um estudo transversal. Cienc. Saude Coletiva 2020, 25, 4157–4168. [Google Scholar]
- Silva, D.R.; Werneck, A.O.; Malta, D.C.; Souza-Júnior, P.R.B.; Azevedo, L.O.; Barros, M.B.A.; Szwarcwald, C.L. Incidence of physical inactivity and excessive screen time during the first wave of the COVID-19 pandemic in Brazil: What are the most affected population groups? Ann. Epidemiol. 2021, 62, 30–35. [Google Scholar] [CrossRef]
- Ernstsen, L.; Havnen, A. Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: Does change in physical activity level matter? Sleep Med. 2021, 77, 309–312. [Google Scholar] [CrossRef]
- Nyenhuis, S.M.; Greiwe, J.; Zeiger, J.S.; Nanda, A.; Cooke, A. Exercise and Fitness in the Age of Social Distancing during the COVID-19 Pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 2152–2155. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Molina, D.; Alonso-Cabrera, J.; Nazar, G.; Parra-Rizo, M.A.; Zapata-Lamana, R.; Sanhueza-Campos, C.; Cigarroa, I. Association between the Physical Activity Behavioral Profile and Sedentary Time with Subjective Well-Being and Mental Health in Chilean University Students during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2107. [Google Scholar] [CrossRef] [PubMed]
- Durán, A.S.; Valdés, P.; Godoy, A.; Herrera, V.T. Hábitos alimentarios y condición física en estudiantes de pedagogía en educación física. Rev. Chil. Nutr. 2014, 41, 251–259. [Google Scholar] [CrossRef] [Green Version]
- Valdes-Badilla, P.; Godoy-Cumillaf, A.; Herrera-Valenzuela, T.; Durán-Agüero, S. Comparación en hábitos alimentarios y condición física entre estudiantes de educación física y otras carreras universitarias. Nutr. Hosp. 2015, 32, 829–836. [Google Scholar]
- Bauman, A.; Ainsworth, B.; Sallis, J.; Hagstromer, M.; Craig, C.L.; Bull, F.C.; Pratt, M.; Venugopal, K.; Chau, J.; Sjöström, M.; et al. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am. J. Prev. Med. 2011, 41, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.; Reynolds, C.; Monk, T.; Berman, S.; Kupfer, D. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Medina, C.; Barquera, S.; Janssen, I. Validity and reliability of the international activity questionnaire among adults in Mexico. Rev. Panam. Salud Publica 2013, 34, 21–28. [Google Scholar]
- Jiménez-Genchi, A.; Monteverde-Maldonado, E.; Nenclares, A.; Esquivel-Adasme, G.; Vega-Pacheco, A. Confiabilidad y análisis factorial de la versión en español del índice de calidad de sueño Pittsburgh en pacientes psiquiátricos. Gac. Médica México 2008, 6, 491–496. [Google Scholar]
- Vega, R.; Tomé-Pires, C.; Solé, E.; Racine, M.; Castarlenas, E.; Jensen, M.; Miro, J. The Pittsburgh sleep quality ndex: Validity nd factor structure in young people. Psychol. Assess 2015, 27, e22–e27. [Google Scholar] [CrossRef] [PubMed]
- Hita-Contreras, F.; Martínez-López, E.; Latorre-Román, P.; Garrido, F.; Santos, M.; Martínez-Amat, A. Reliability and validity of the Spanish version of the Pittsburgh sleep quality index (PSQI) in patients with fibromyalgia. Rheumatil. Int. 2014, 34, 929–936. [Google Scholar] [CrossRef]
- Dolezal, B.; Neufeld, E.; Boland, D.; Martin, J.; Cooper, K. Interrelationship between sleep and exercise: A systematic Review. Adv. Prev. Med. 2017, 2017, e1364387. [Google Scholar]
- Ortega, F.B.; Ruiz, J.R.; Espana-Romero, V.; Vicente-Rodriguez, G.; Martínez-Gómez, D.; Manios, Y.; Béghin, L.; Molnar, D.; Widhalm, K.; Moreno, L.A.; et al. The International Fitness Scale (IFIS): Usefulness of self-reported fitness in youth. Int. J. Epidemiol. 2011, 40, 701–711. [Google Scholar] [CrossRef] [Green Version]
- Merellano-Navarro, E.; Collado-Mateo, D.; García-Rubio, J.; Gusi, N.; Olivares, P.R. Validity of the International Fitness Scale “IFIS” in older adults. Exp. Gerontol. 2017, 95, 77–81. [Google Scholar] [CrossRef]
- Serón, P.; Muñoz, S.; Lanas, F. Nivel de actividad física medida a través del cuestionario internacional de actividad física en población chilena. Rev. Med. Chile 2010, 138, 1232–1239. [Google Scholar] [CrossRef]
- Mahfouz, M.S.; Ali, S.A.; Bahari, A.Y.; Ajeebi, R.E.; Sabei, H.J.; Somaily, S.Y.; Madkhali, Y.A.; Hrooby, R.H.; Shook, R.N. Association between sleep quality and physical activity in Saudi Arabian University students. Nat. Sci. Sleep 2020, 12, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Zhai, X.; Ye, M.; Wang, C.; Gu, Q.; Huang, T.; Wang, K.; Chen, Z.; Fan, X. Associations among physical activity and smartphone use with perceived stress and sleep quality of Chinese college students. Ment. Health Phys. Act. 2020, 18, 100323. [Google Scholar] [CrossRef]
- Haripriya, S.; Samuel, S.E.; Megha, M. Correlation between Smartphone Addiction, Sleep Quality and Physical Activity among Young Adults. J. Clin. Diagn. Res. 2019, 13, 5–9. [Google Scholar] [CrossRef]
- Štefan, L.; Sporiš, G.; Krističević, T.; Knjaz, D. Associations between sleep quality and its domains and insufficient physical activity in a large sample of Croatian young adults: A cross-sectional study. BMJ Open 2018, 8, e021902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gangwar, A.; Tiwari, S.; Rawat, A.; Verma, A.; Singh, K.; Kant, S.; Garg, R.K.; Singh, P.K. Circadian Preference, Sleep Quality, and Health-impairing Lifestyles Among Undergraduates of Medical University. Cureus 2018, 10, e2856. [Google Scholar] [CrossRef] [Green Version]
- Fenq, Q.; Zhang, Q.; Du, Y.; Ye, Y.; He, Q. Associations of Physical Activity, Screen Time with Depression, Anxiety and Sleep Quality among Chinese College Freshmen. PLoS ONE 2014, 9, e100914. [Google Scholar] [CrossRef] [Green Version]
- Lipert, A.; Musial, K.; Rasmus, P. Working Mode and Physical Activity as Factors Determining Stress and Sleep Quality during COVID-19 Pandemic Lockdown in Poland. Life 2021, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Papaconstantinou, E.; Quick, V.; Vogel, E.; Coffey, S.; Miller, A.; Zitzelsberger, H. Exploring Relationships of Sleep Duration with Eating and Physical Activity Behaviors among Canadian University Students. Clocks Sleep 2020, 2, 194–207. [Google Scholar] [CrossRef]
- Fawzy, M.; Hamed, S.A. Prevalence of psychological stress, depression and anxiety among medical students in Egypt. Psychiatry Res. 2017, 255, 186–194. [Google Scholar] [CrossRef]
- Gelaye, B.; Lohsoonthorn, V.; Lertmeharit, S.; Pensuksan, W.C.; Sanchez, S.E.; Lemma, S.; Berhane, Y.; Zhu, X.; Vélez, J.C.; Barbosa, C.; et al. Construct Validity and Factor Structure of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale in a Multi-National Study of African, South East Asian and South American College Students. PLoS ONE 2014, 9, e116383. [Google Scholar]
- de la Portilla-Maya, S.; Dussán, C.; Montoya, D.M.; Taborda, J.; Nieto, L.S. Calidad de sueño y somnolencia diurna excesiva en estudiantes universitarios de diferentes dominios. Hacia. Promoción Salud 2019, 24, 84–96. [Google Scholar] [CrossRef]
- Núñez, P.; Perillan, C.; Arguelles, J.; Diaz, E. Comparison of sleep and chronotype between senior and undergraduate university students. Chronobiol. Int. 2019, 36, 1626–1637. [Google Scholar] [CrossRef]
- Baron, K.G.; Duffecy, J.; Reutrakul, S.; Levenson, J.C.; McFarland, M.M.; Lee, S.; Qeadan, F. Behavioral interventions to extend sleep duration: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 60, 101532. [Google Scholar] [CrossRef] [PubMed]
- Benham, G. Stress and sleep in college students prior to and during the COVID-19 pandemic. Stress Health 2021, 3, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Malta, K.S.; Bittencourt, A.T.; Kapp, A.C.; Leite, N. Sleep deprivation and drowsiness of medical residents and medical students. Rev. Col. Bras. Cir. 2016, 43, 438–444. [Google Scholar]
- Pilcher, J.J.; Erikson, D.N.; Yochum, C.A. Fighting the Freshman Fifteen: Sleep, Exercise, and BMI in College Students. Am. J. Health Promot. 2021, 35, 580–583. [Google Scholar] [CrossRef] [PubMed]
- López, F.; Oyanedel, J.C.; Rivera-lópez, G. Calidad del sueño según progresión académica en estudiantes chilenos de Obstetricia. Medisur 2020, 18, 211–222. [Google Scholar]
- Durán-Agüero, S.; Sepulveda, R.; Guerrero-Wyss, M. Sleep disorders and anthropometric measures in Chilean university students. Rev. Española Nutr. Hum. Dietética 2020, 23, 153. [Google Scholar] [CrossRef] [Green Version]
- Oliveira, C.R.; de Oliveira, B.C.; de Ferreira, L.G.F. Qualidade de sono em universitários de uma instituição privada. Rev. Pesqui. Fisioter. 2020, 10, 274. [Google Scholar] [CrossRef]
- Durán, S.; Crovetto, M.; Espinoza, V.; Mena, F.; Oñate, G.; Fernández, M.; Coñuecar, S.; Guerra, Á.; Valladares, M. Caracterización del estado nutricional, hábitos alimentarios y estilos de vida de estudiantes universitarios chilenos: Estudio multicéntrico. Rev. Med. Chile 2017, 145, 1403–1411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colten, H.R.; Altevogt, B.M. Sleep Disorders and Sleep Deprivation; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Fraschetti, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. COVID-19 lockdown and poor sleep quality: Not the whole story. J. Sleep Res. 2021, 30, e13368. [Google Scholar] [CrossRef]
- Holzinger, B.; Mayer, L.; Nierwetberg, F.; Klösch, G. COVID-19 lockdown—Are Austrians finally able to compensate their sleep debt? Sleep Med. 2021, 3, 100032. [Google Scholar] [CrossRef]
- Martínez-de-Quel, Ó.; Suárez-Iglesias, D.; López-Flores, M.; Pérez, C.A. Physical activity, dietary habits and sleep quality before and during COVID-19 lockdown: A longitudinal study. Appetite 2021, 158, 105019. [Google Scholar] [CrossRef]
- Hershner, S.D.; Chervin, R.D. Causes and consequences of sleepiness among college students. Nat. Sci. Sleep 2014, 6, 73–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiang, M.; Zhang, Z.; Kuwahara, K. Impact of COVID-19 pandemic on children and adolescents’ lifestyle behavior larger than expected. Prog. Cardiovasc. Dis. 2020, 63, 531–532. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Larrad, A.; Mañas, A.; Labayen, I.; González-Gross, M.; Espin, A.; Aznar, S.; Serrano-Sánchez, J.A.; Vera-Garcia, F.J.; González-Lamuño, D.; Ara, I.; et al. Impact of COVID-19 confinement on physical activity and sedentary behaviour in Spanish university students: Role of gender. Int. J. Environ. Res. Public Health 2021, 18, 369. [Google Scholar] [CrossRef] [PubMed]
- Celis-Morales, C.; Salas-Bravo, C.; Yáñez, A.; Castillo, M. Inactividad física y sedentarismo. La otra cara de los efectos secundarios de la Pandemia de COVID-19. Rev. Med. Chile 2020, 148, 885–886. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Toledo-Vargas, M.; Miranda-Marquez, S.; Cortinez-O’Ryan, A.; Cristi-Montero, C.; Rodriguez-Rodriguez, F.; Martino-Fuentealba, P.; Okely, A.B.; Del Pozo Cruz, B. Sociodemographic Predictors of Changes in Physical Activity, Screen Time, and Sleep among Toddlers and Preschoolers in Chile during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 18, 176. [Google Scholar] [CrossRef] [PubMed]
- Cortinez-O’Ryan, A.; Moran, M.R.; Rios, A.P.; Anza-Ramirez, C.; Slovic, A.D. Could severe mobility and park use restrictions during the COVID-19 pandemic aggravate health inequalities? Insights and challenges from Latin America. Cad. Saúde Pública 2020, 36, e00185820. [Google Scholar] [CrossRef]
- Droomers, M.; Schrijvers, C.T.M.; Mackenbach, J.P. Educational level and decreases in leisure time physical activity: Predictors from the longitudinal globe study. J. Epidemiol. Community Health 2001, 55, 562–568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srivastav, A.K.; Sharma, N.; Samuel, A.J. Impact of Coronavirus disease-19 (COVID-19) lockdown on physical activity and energy expenditure among physiotherapy professionals and students using web-based open E-survey sent through WhatsApp, Facebook and Instagram messengers: Impact of COVID-19 lock. Clin. Epidemiol. Glob. Health 2021, 9, 78–84. [Google Scholar] [CrossRef]
- Gobierno de Chile. Actualización de la Estrategia Gradual “Paso a Paso nos cuidamos”. 2021. Available online: https://s3.amazonaws.com/gobcl-prod/public_files/Campa%C3%B1as/Corona-Virus/documentos/Estrategia-gradual-v15.pdf (accessed on 1 April 2020).
- Woods, J.A.; Hutchinson, N.T.; Powers, S.K.; Roberts, W.O.; Gomez-Cabrera, M.C.; Radak, Z.; Berkes, I.; Boros, A.; Boldogh, I.; Leeuwenburgh, C.; et al. The COVID-19 pandemic and physical activity. Sports Med. Health Sci. 2020, 2, 55–64. [Google Scholar] [CrossRef]
- García-Tascón, M.; Sahelices-Pinto, C.; Mendaña-Cuervo, C.; Magaz-González, A.M. The Impact of the COVID-19 Confinement on the Habits of PA Practice According to Gender (Male/Female): Spanish Case. Int. J. Environ. Res. Public Health 2020, 17, 6961. [Google Scholar] [CrossRef]
- Chang, S.; Huang, S.; Chen, Y.; Wright, R. The Relationship between Sleep Quality and the Exercise Participation Behavior of College Students in the Central Taiwan Region. Int. J. Sport Exerc. Sci. 2013, 5, 13–18. [Google Scholar]
- Schuch, F.B.; Bulzing, R.A.; Meyer, J.; Vancampfort, D.; Firth, J.; Stubbs, B.; Grabovac, I.; Willeit, P.; Tavares, V.D.O.; Calegaro, V.C.; et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: A cross-sectional survey in Brazil. Psychiatry 2020, 292, 113339. [Google Scholar] [CrossRef]
- Rajkumar, R.P. Sleep, physical activity and mental health during the COVID-19 pandemic: Complexities and opportunities for intervention. Sleep Med. 2021, 77, 307–308. [Google Scholar] [CrossRef]
- Memon, A.R.; Gupta, C.C.; Crowther, M.E.; Ferguson, S.A.; Tuckwell, G.A.; Vincent, G.E. Sleep and physical activity in university students: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 58, 101482. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.K.; Rebellon, J.; Huber, C.; Leonard, A.J.; Henderson, D.; Magal, M. Cardiorespiratory fitness, sleep, and physiological responses to stress in women. Eur. J. Sport Sci. 2020, 20, 1368–1377. [Google Scholar] [CrossRef]

| All Participants n = 280 | Males n = 204 | Females n = 76 | p-Value | |
|---|---|---|---|---|
| Sex | 72.9 | 27.1% | ||
| Age (years) mean ± SD | 21.4 ± 2.3 | 21.4 ± 2.3 | 21.1 ± 2.2 | 0.155 |
| Residence urban, n (%) | 236 (84.3) | 175 (85.8) | 61 (80.3) | 0.26 |
| Academic year, n (%) | ||||
| ≥4th year | 67 (23.9) | 48 (23.5) | 19 (25.0) | 0.24 |
| 3rd year | 57 (20.4) | 44 (21.6) | 13 (17.1) | |
| 2nd year | 60 (21.4) | 38 (18.6) | 22 (28.9) | |
| 1st year | 96 (34.3) | 74 (36.3) | 22 (28.9) | |
| Living with, n (%) | 0.079 | |||
| Both parents | 140 (50.0) | 108 (52.9) | 32 (42.1) | |
| Mother | 98 (35.0) | 71 (34.8) | 27 (35.5) | |
| Friends or other | 42 (15.0) | 25 (12.3) | 17 (22.4) | |
| Habits and Health, n (%) | ||||
| Chronic illness | 23 (8.2) | 11 (5.4) | 12 (15.8) | 0.005 |
| COVID-19 diagnosis | 9 (3.2) | 7 (3.4) | 2 (2.6) | 0.736 |
| Smoker | 38 (13.6) | 22 (10.8) | 16 (21.1) | 0.026 |
| Drinking alcohol | 179 (63.9) | 130 (63.7) | 49 (64.5) | 0.908 |
| Mood | ||||
| Good (without problems) | 100 (32.7) | 79 (35.7) | 21 (24.7) | 0.065 |
| Bad (with mild or severe problems) | 206 (67.3) | 142 (64.3) | 64 (75.3) | |
| Physical Activity Level, IPAQ, n (%) | ||||
| High | 146 (52.1) | 116 (56.9) | 30 (39.5) | 0.026 |
| Moderate | 106 (37.9) | 68 (33.3) | 38 (50.0) | |
| Low | 28 (10.0) | 20 (9.8) | 8 (10.5) | |
| Met guidelines WHO *, n (%) | ||||
| Yes | 252 (90.0) | 184 (90.2) | 68 (89.5) | 0.858 |
| Type of physical activity on pandemic, n (%) | ||||
| General | 138 (49.3) | 102 (50.0) | 36 (47.4) | 0.465 |
| Specific | 124 (44.3) | 87 (42.6) | 37 (48.7) | |
| None | 18 (6.4) | 15 (7.4) | 3 (3.9) | |
| PSQI global score, mean ± DS | 8.4 ± 3.3 | 8.0 ± 3.1 | 9.3 ± 3.4 | 0.039 * |
| Good Sleep Quality, n (%) | 57 (20.4) | 48 (23.5) | 9 (11.8) | 0.031 |
| Poor Sleep Quality, n (%) | 223 (79.6) | 156 (76.5) | 67 (88.2) | |
| Sleep duration, n (%) | ||||
| <7 h | 222 (79.3) | 158 (77.5) | 64 (84.2) | 0.215 |
| >7 h | 58 (20.7) | 46 (22.5) | 12 (15.8) |
| High n (%) | Moderate n (%) | Low n (%) | p-Value | |
|---|---|---|---|---|
| PSQI global score, mean ±SD | 7.7 ± 3.2 | 8.9 ± 3.2 | 9.4 ± 3.3 | 0.003 * |
| Good sleep quality | 38 (26.0) | 16 (15.1) | 3 (10.7) | 0.043 |
| Poor sleep quality | 108 (74.0) | 90 (84.9) | 25 (89.3) | |
| Sleep duration | ||||
| <7 h | 109 (74.7) | 87 (82.1) | 26 (92.9) | 0.062 |
| >7 h | 37 (25.3) | 19 (17.9) | 2 (7.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Merellano-Navarro, E.; Bustamante-Ara, N.; Russell-Guzmán, J.; Lagos-Hernández, R.; Uribe, N.; Godoy-Cumillaf, A. Association between Sleep Quality and Physical Activity in Physical Education Students in Chile in the Pandemic Context: A Cross-Sectional Study. Healthcare 2022, 10, 1930. https://doi.org/10.3390/healthcare10101930
Merellano-Navarro E, Bustamante-Ara N, Russell-Guzmán J, Lagos-Hernández R, Uribe N, Godoy-Cumillaf A. Association between Sleep Quality and Physical Activity in Physical Education Students in Chile in the Pandemic Context: A Cross-Sectional Study. Healthcare. 2022; 10(10):1930. https://doi.org/10.3390/healthcare10101930
Chicago/Turabian StyleMerellano-Navarro, Eugenio, Natalia Bustamante-Ara, Javier Russell-Guzmán, Roberto Lagos-Hernández, Natasha Uribe, and Andrés Godoy-Cumillaf. 2022. "Association between Sleep Quality and Physical Activity in Physical Education Students in Chile in the Pandemic Context: A Cross-Sectional Study" Healthcare 10, no. 10: 1930. https://doi.org/10.3390/healthcare10101930
APA StyleMerellano-Navarro, E., Bustamante-Ara, N., Russell-Guzmán, J., Lagos-Hernández, R., Uribe, N., & Godoy-Cumillaf, A. (2022). Association between Sleep Quality and Physical Activity in Physical Education Students in Chile in the Pandemic Context: A Cross-Sectional Study. Healthcare, 10(10), 1930. https://doi.org/10.3390/healthcare10101930








