Prospective Observational Study after Eversion Carotid Endarterectomy with Ultrasound-Guided Deep-Intermediate Cervical Plexus Blockade
Abstract
1. Introduction
2. Material and Methods
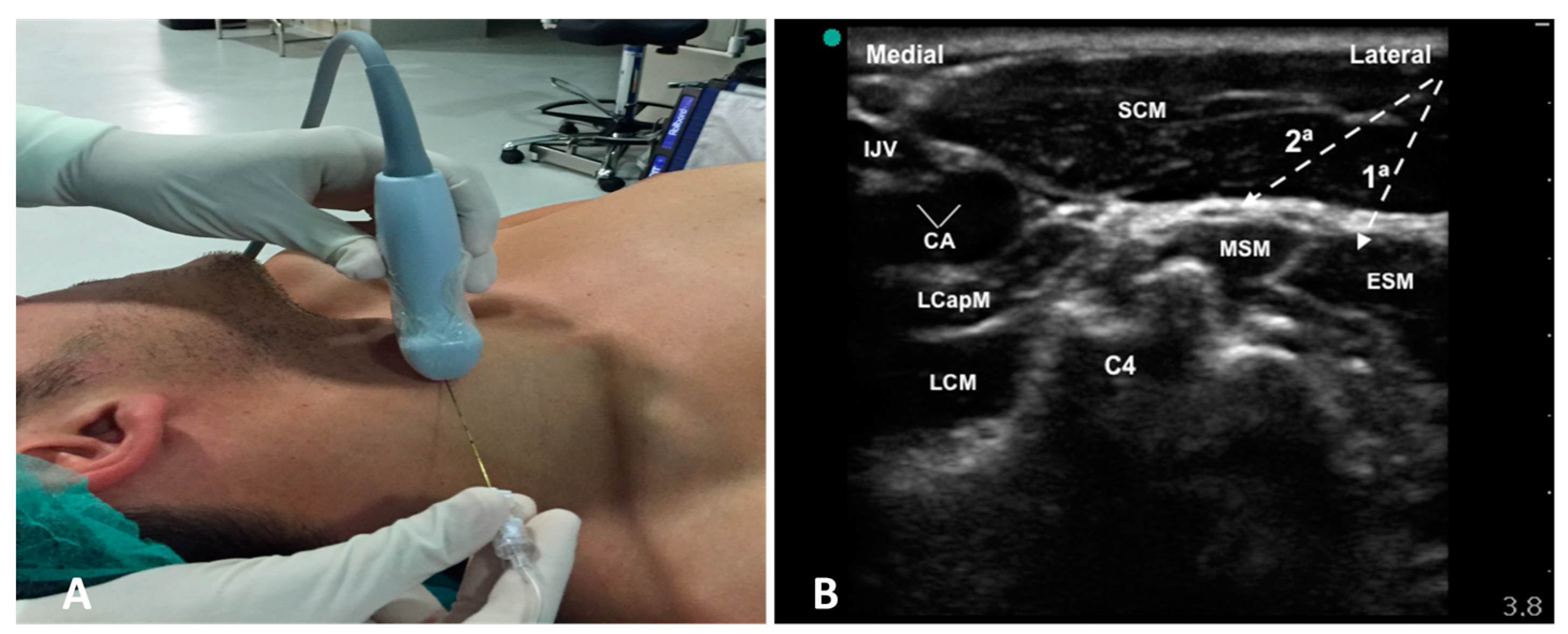
2.1. Anesthetic Technique
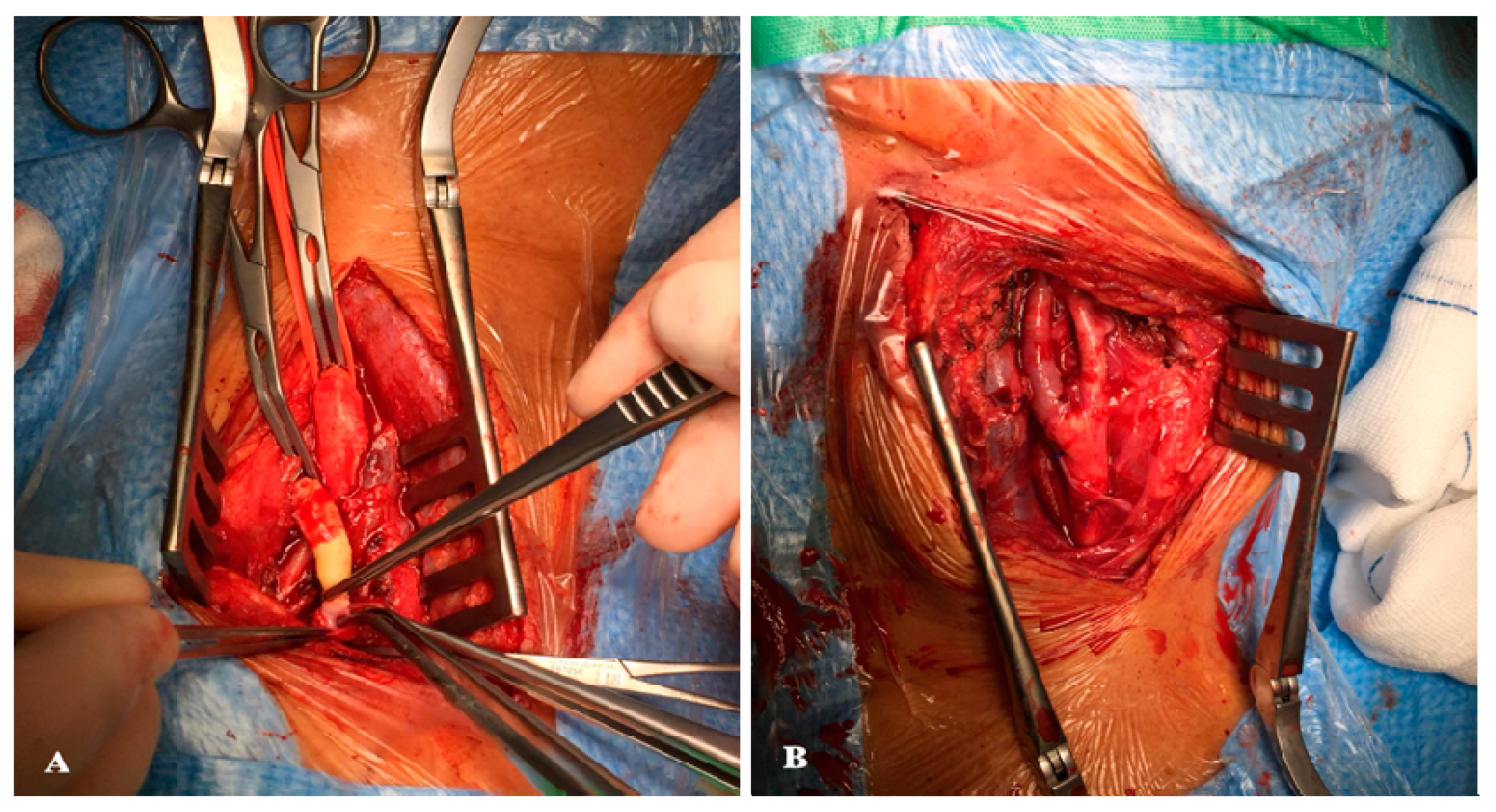
2.2. Surgical Technique
2.3. Statistical Analysis
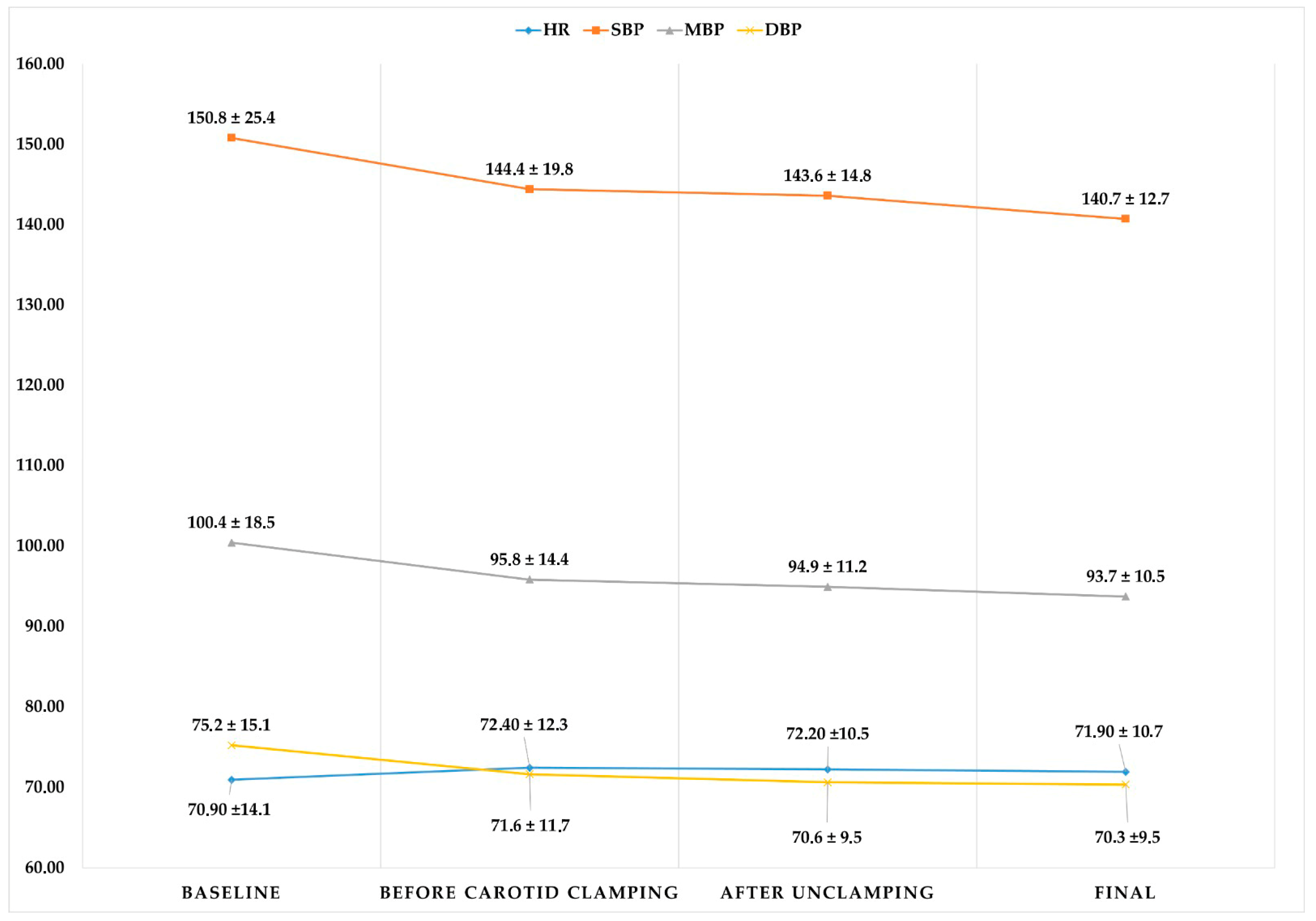
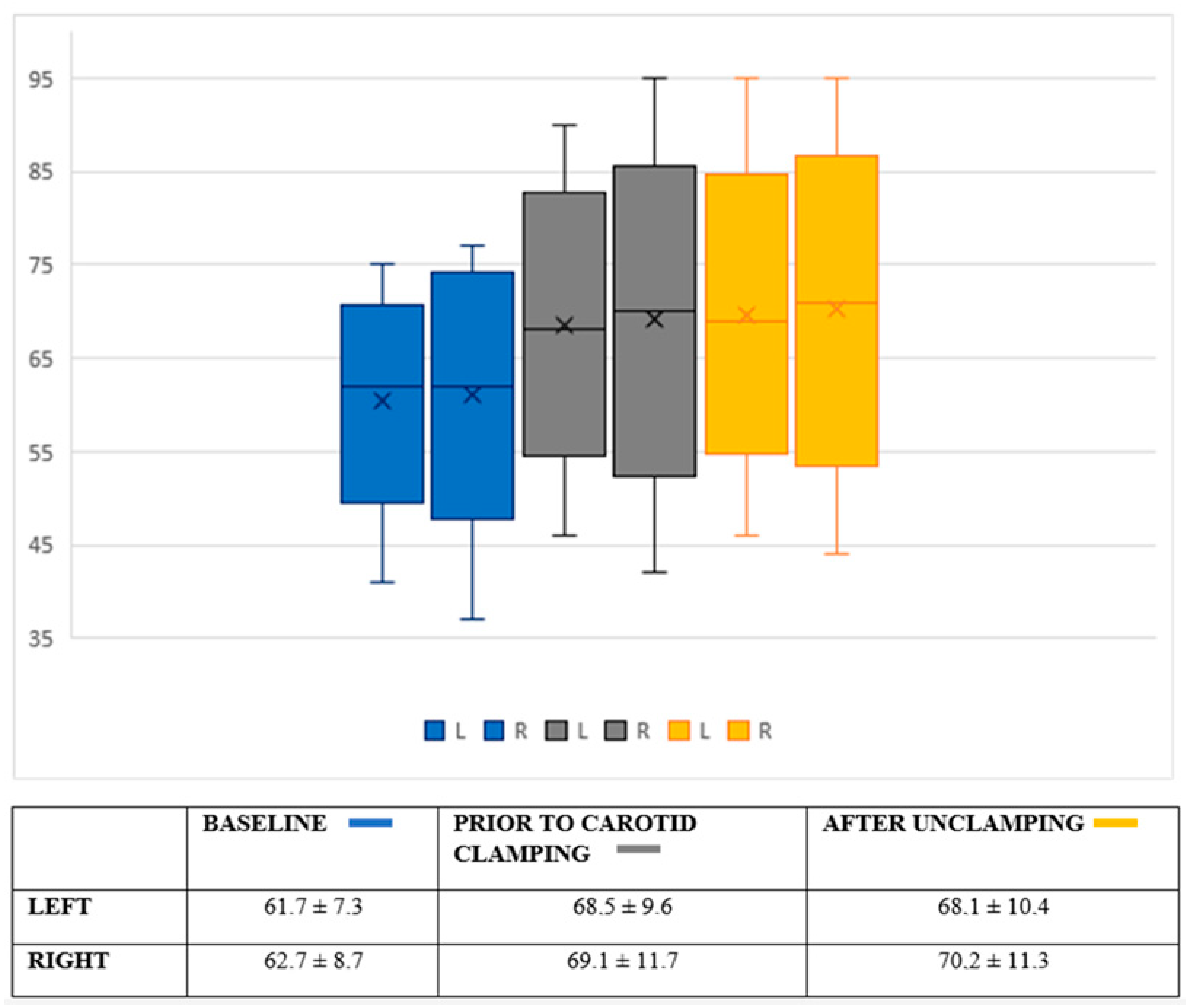
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheng, S.F.; Richards, T.; Gregson, J.; Brown, M.M.; Borst, G.J.; Bonati, L.H. Long term restenosis rate after carotid endarterectomy: Comparison of three surgical techniques and intra-operative shunt use. Eur. J. Vasc. Endovasc. Surg. 2021, 62, 513–521. [Google Scholar] [CrossRef]
- GALA Trial Collaborative Group; Lewis, S.C.; Warlow, C.P.; Bodenham, A.R.; Colam, B.; Rothwell, P.M.; Torgerson, D.; Dellagrammaticas, D.; Horrocks, M.; Liapis, C.; et al. General anaesthesia versus local anaesthesia for carotid surgery (GALA): A multicentre, randomised controlled trial. Lancet 2008, 372, 2132–2142. [Google Scholar] [PubMed]
- Harky, A.; Shi Kai Chan, J.; Ka MIng Kot, T.; Sanli, D.; Rahimli, R.; Belamaric, Z.; Ng, M.; Yu Young Kwan, I.; Bithas, C.; Makar, R.; et al. General anesthesia versus local anesthesia in carotid endarterectomy: A systematic review and meta-analysis. J. Cardiothorac. Vasc. Anesth. 2020, 34, 219–234. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, A.S.; White, R.S.; Tangel, V.; Storch, B.M.; Pryor, K.O. Carotid Revascularization procedures and perioperative outcomes: A multistate analysis, 2007–2014. J. Cardiothorac.Vasc. Anesth. 2019, 33, 1963–1972. [Google Scholar] [CrossRef] [PubMed]
- Leichtle, S.W.; Mouawad, N.J.; Welch, K.; Lampman, R.; Whitehouse, W.M., Jr.; Heidenreich, M. Outcomes of carotid endarterectomy under general and regional anesthesia from the American College of Surgeons’ National Surgical Quality Improvement Program. J. Vasc. Surg. 2012, 56, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Yepes Temiño, M.J.; Lillo Cuevas, M. Anestesia en la endarterectomía carotídea: Revisión. Rev. Esp. Anestesiol. Reanim. 2011, 58, 34–41. [Google Scholar] [CrossRef]
- Sait Kavaklı, A.; Kavrut Öztürk, N.; Umut Ayoğlu, R.; Sağdıç, K.; Çakmak, G.; İnanoğlu, K.; Emmiler, M. Comparison of Combined (Deep and Superficial) and Intermediate Cervical Plexus Block by Use of Ultrasound Guidance for Carotid Endarterectomy. J. Cardiothorac. Vasc. Anesth. 2016, 30, 317–322. [Google Scholar] [CrossRef]
- Chiesa, R.; Melissano, G.; Castellano, R.; Tshomba, Y.; Marone, E.M.; Civilini, E.; Astore, D.; Calliari, F.; Catenaccio, B.; Coppi, G.; et al. Carotid Endarterectomy: Experience in 8743 cases. HSR Proc. Intensive Care Cardiovasc. Anesth. 2009, 1, 33–45. [Google Scholar]
- European Carotid Surgery Trialist Collaborative Group. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: Final results of the MRC European carotid surgery trial (ECST). Lancet 1998, 351, 1379–1387. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Gutnikov, S.A.; Warlow, C.P.; European Carotid Surgery Trialist’s Collaboration. Reanalysis of the final results of the european carotid surgery trial. Stroke 2003, 34, 514–523. [Google Scholar] [CrossRef]
- Narins, C.R.; Illig, K.A. Patient selection for carotid stenting versus ensarterectomy: A systematic review. J. Vasc. Surg. 2006, 44, 661–672. [Google Scholar] [CrossRef] [PubMed]
- Hill, M.D.; Brooks, W.; Mackey, A.; Clark, W.M.; Meschia, J.F.; Morrish, W.F.; Mohr, J.P.; Rhodes, J.D.; Popma, J.J.; Lal, B.K.; et al. Stroke after carotid stenting and endarterectomy in the carotid revascularization endarterectomy versus stenting trial (CREST). Circulation 2012, 126, 3054–3061. [Google Scholar] [CrossRef]
- Howell, S.J. Carotid endarterectomy. Br. J. Anaesth. 2007, 99, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Cañibano, E.; Reina-Gutierrez, T.; Serrano-Hernando, F.J.; Martín-Conejero, A.; Ponce-Cano, A.I.; Vega de Céniga, M.; Aguilar-Lloret, C. Endarterectomía carotídea con anestesia locorregional. Estudio de factores clínicos y arteriográficos de riesgo de isquemia cerebral durante el clampaje carotídeo. Angiología 2004, 56, 133–145. [Google Scholar] [CrossRef]
- Hoefer, J.; Pierer, E.; Rantner, B.; Stadlbauer, K.H.; Fraedrich, G.; Fritz, J.; Kleinsasser, A.; Velik-Salchner, C. Ultrasound-guided regional anesthesia for carotid endarterectomy induces early hemodynamic and stress hormone changes. J. Vasc. Surg. 2015, 62, 57–67. [Google Scholar] [CrossRef]
- Malik, O.S.; Brovman, E.Y.; Urman, R.D. The Use of Regional or Local Anesthesia for Carotid Endarterectomies May Reduce Blood Loss and Pulmonary Complications. J. Cardiothorac. Vasc. Anesth. 2019, 33, 935–942. [Google Scholar] [CrossRef]
- Grieff, A.N.; Dombrovskiy, V.; Beckerman, W.; Ventarola, D.; Truong, H.; Huntress, L.; Rahimi, S. Anesthesia type is associated with decreased cranial nerve injury in carotid endarterectomy. Ann. Vasc. Surg. 2021, 70, 318–325. [Google Scholar] [CrossRef]
- Hye, R.J.; Voeks, J.H.; Malas, M.B.; Tom, M.; Longson, S.; Blackshear, J.L.; Brott, T.G. Anesthetic type and risk of myocardial infarction after carotid endarterectomy in the Carotid Revascularization Endarterectomy versus Stenting Trial (CREST). J. Vasc. Surg. 2016, 64, 3–8. [Google Scholar] [CrossRef]
- Sindjelic, R.P.; Vlajkovic, G.P.; Lucic, M.; Koncar, I.; Kostic, D.; Davidovic, L.B. Incidence of and indications for conversion of cervical plexus block to general anesthesia in patients undergoing carotid surgery: A single center experience. J. Cardiovasc. Surg. 2015, 56, 441–446. [Google Scholar]
- Pandit, J.J.; Satya Krishna, R.; Gration, P. Superficial or deep cervical plexus block for carotid endarterectomy: A systematic review of complications. Br. J. Anaesth. 2007, 99, 159–169. [Google Scholar] [CrossRef]
- Carling, A.; Simmonds, M. Complications from regional anaesthesia for carotid endarterectomy. Br. J. Anaesth. 2000, 84, 797–800. [Google Scholar] [CrossRef] [PubMed]
- Pasin, L.; Nardelli, P.; Landoni, G.; Cornero, G.; Magrin, S.; Tshomba, Y.; Chiesa, R.; Zangrillo, A. Examination of regional anesthesia for carotid endarterectomy. J. Vasc. Surg. 2015, 1, 631–634. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Variables | Sample Size (N = 30) |
|---|---|
| Men | 22 (73.3%) |
| Women | 8 (26.7%) |
| Age (years) | 71.2 ± 8.7 |
| Weight (kg) | 76.5 ± 12.7 |
| Height (cm) | 166.0 ± 9.56 |
| ASA ASA III or superior | 2.9 ± 0.2 28 (93.3%) |
| Comorbidities | |
| Hypertension | 23 (76.7%) |
| Diabetes mellitus | 11 (36.7%) |
| Atrial fibrillation | 8 (26.7%) |
| Ischemic heart disease | 4 (13.3%) |
| Dyslipidemia | 19 (63.3%) |
| Transient ischemic attack | 21 (70%) |
| Stroke | 16 (53.3%) |
| Active smoker | 18 (60%) |
| Hypothyroidism | 2 (6.7%) |
| Sleep apnea syndrome | 1 (3.3%) |
| Chronic renal syndrome | 3 (10%) |
| COPD | 3 (10%) |
| Contralateral stenosis | 11 (36.7%) |
| Baseline | After Anesthesia | Final |
|---|---|---|
| 97.5 (97–98) | 85.6 ± 3.8 | 96.4 ± 1.3 |
| Variable | Sample Size (N = 30) |
|---|---|
| Postoperative pain | |
| 6 h | 0.4 ± 0.9 |
| 12 h | 1.2 ± 0.9 |
| 24 h | 0.47 ± 0.5 |
| Transient residual nerve block | 12 (40%) |
| Hypoglossal nerve block | 9 (30%) |
| Laryngeal nerve block | 7 (23.3%) |
| Facial nerve block | 2 (6.7%) |
| Early complications | 5 (16.7%) |
| Cervical hematoma | 2 (6.7%) |
| Bleeding | 1 (3.3%) |
| Pharyngeal edema | 1 (3.3%) |
| Headache | 1 (3.3%) |
| Major complications in the first 30 days | 1 (3.3%) |
| Length of stay at resuscitation unit (h) | 24 (24–24) |
| Hospital length of stay (h) | 60 (48–78) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vega Colón, M.; López González, J.M.; Jiménez Gómez, B.M.; Pico Veloso, J.; Fernández Mendez, M.; Fernández Suárez, F.E.; del Castro Madrazo, J.A.; Álvarez Marcos, F.; Fajardo Pérez, M.; Lin, J.-A.; et al. Prospective Observational Study after Eversion Carotid Endarterectomy with Ultrasound-Guided Deep-Intermediate Cervical Plexus Blockade. Healthcare 2022, 10, 1986. https://doi.org/10.3390/healthcare10101986
Vega Colón M, López González JM, Jiménez Gómez BM, Pico Veloso J, Fernández Mendez M, Fernández Suárez FE, del Castro Madrazo JA, Álvarez Marcos F, Fajardo Pérez M, Lin J-A, et al. Prospective Observational Study after Eversion Carotid Endarterectomy with Ultrasound-Guided Deep-Intermediate Cervical Plexus Blockade. Healthcare. 2022; 10(10):1986. https://doi.org/10.3390/healthcare10101986
Chicago/Turabian StyleVega Colón, María, José Manuel López González, Bárbara María Jiménez Gómez, Jandro Pico Veloso, Marta Fernández Mendez, Félix Ezequiel Fernández Suárez, José Antonio del Castro Madrazo, Francisco Álvarez Marcos, Mario Fajardo Pérez, Jui-An Lin, and et al. 2022. "Prospective Observational Study after Eversion Carotid Endarterectomy with Ultrasound-Guided Deep-Intermediate Cervical Plexus Blockade" Healthcare 10, no. 10: 1986. https://doi.org/10.3390/healthcare10101986
APA StyleVega Colón, M., López González, J. M., Jiménez Gómez, B. M., Pico Veloso, J., Fernández Mendez, M., Fernández Suárez, F. E., del Castro Madrazo, J. A., Álvarez Marcos, F., Fajardo Pérez, M., Lin, J.-A., Galluccio, F., Hou, J.-D., & Chan, S.-M. (2022). Prospective Observational Study after Eversion Carotid Endarterectomy with Ultrasound-Guided Deep-Intermediate Cervical Plexus Blockade. Healthcare, 10(10), 1986. https://doi.org/10.3390/healthcare10101986








