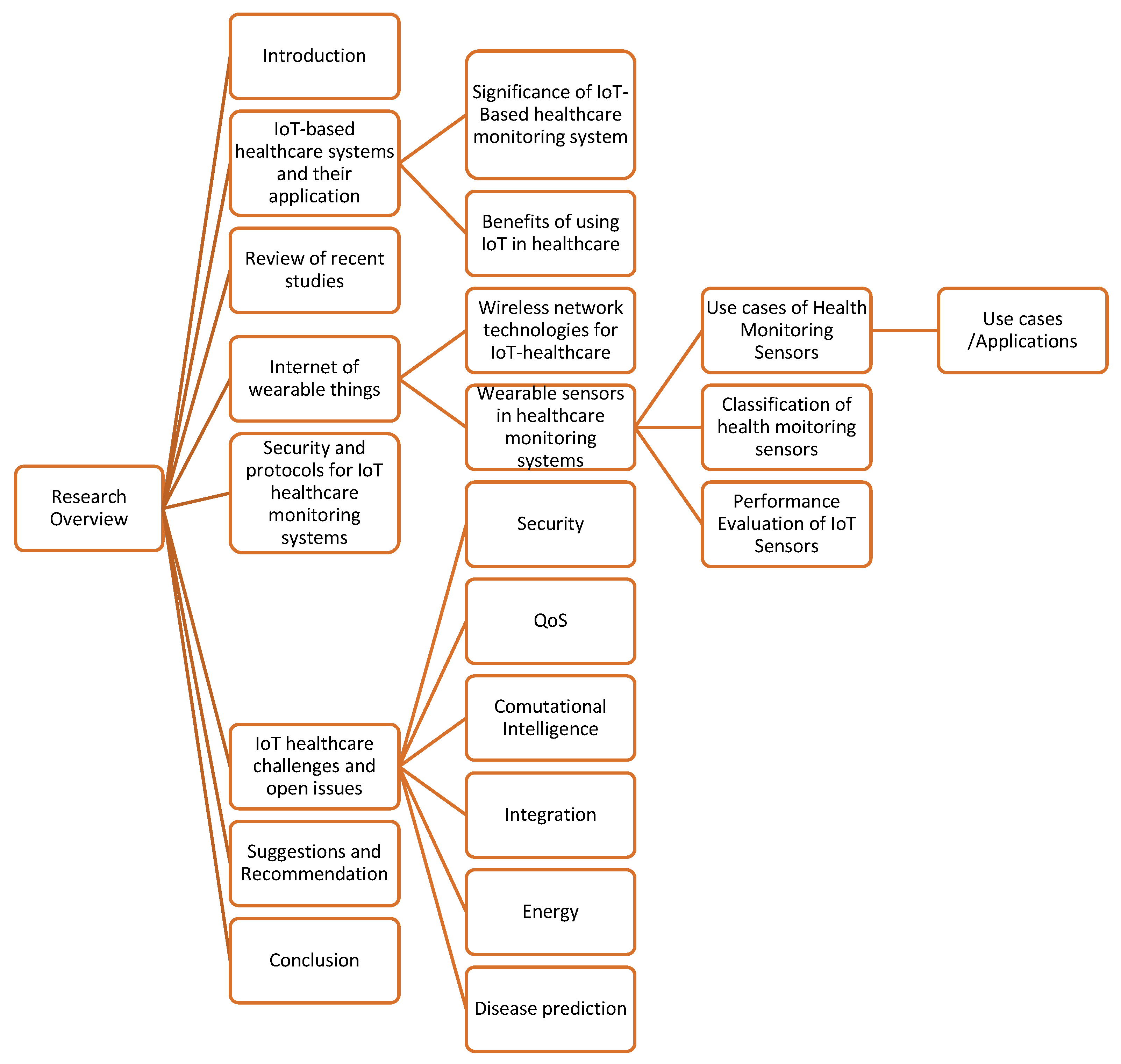
IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review
Abstract
1. Introduction
2. IoT-Based Healthcare Systems and Their Applications
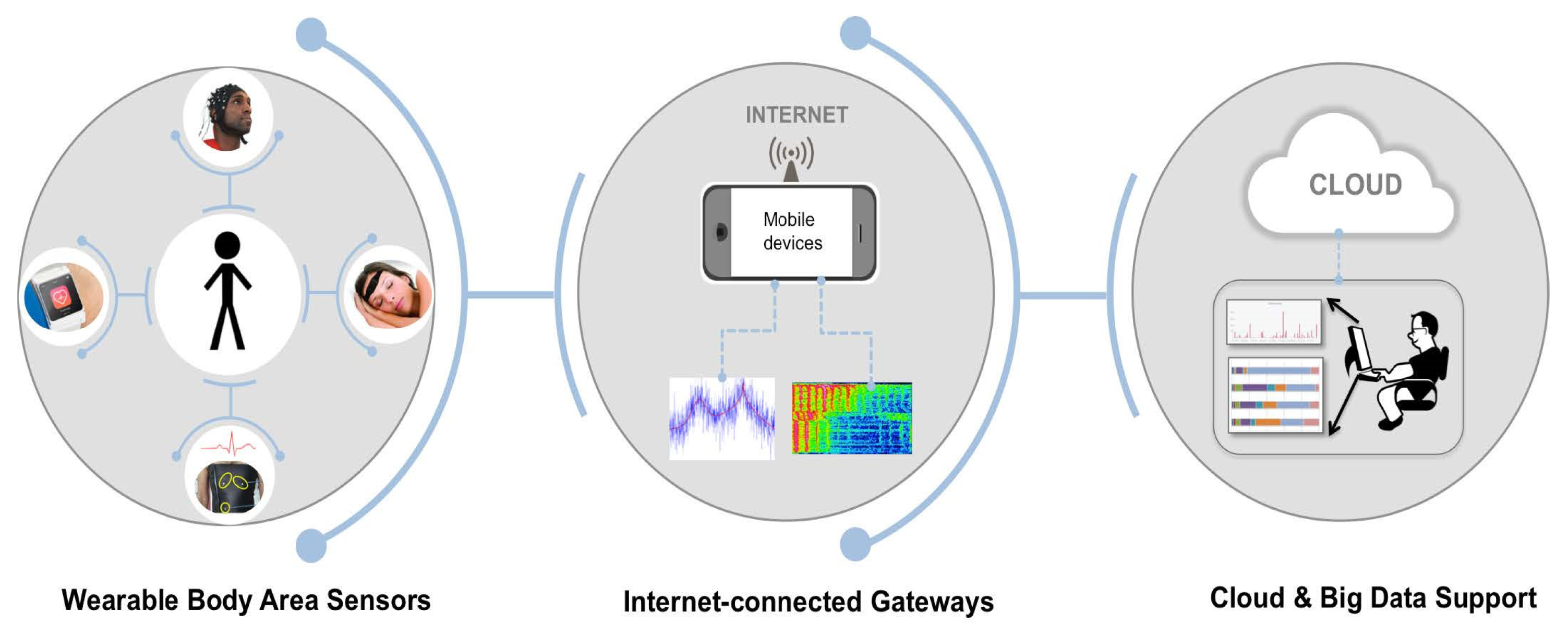
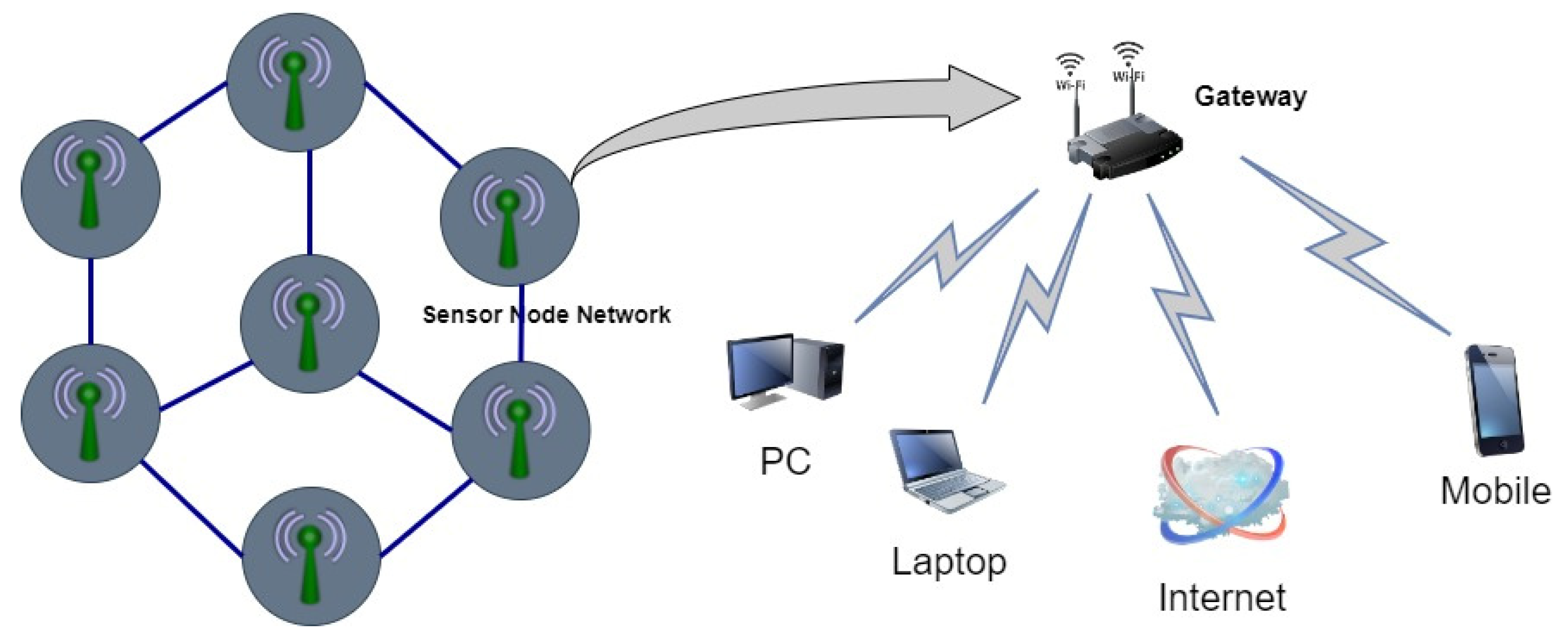
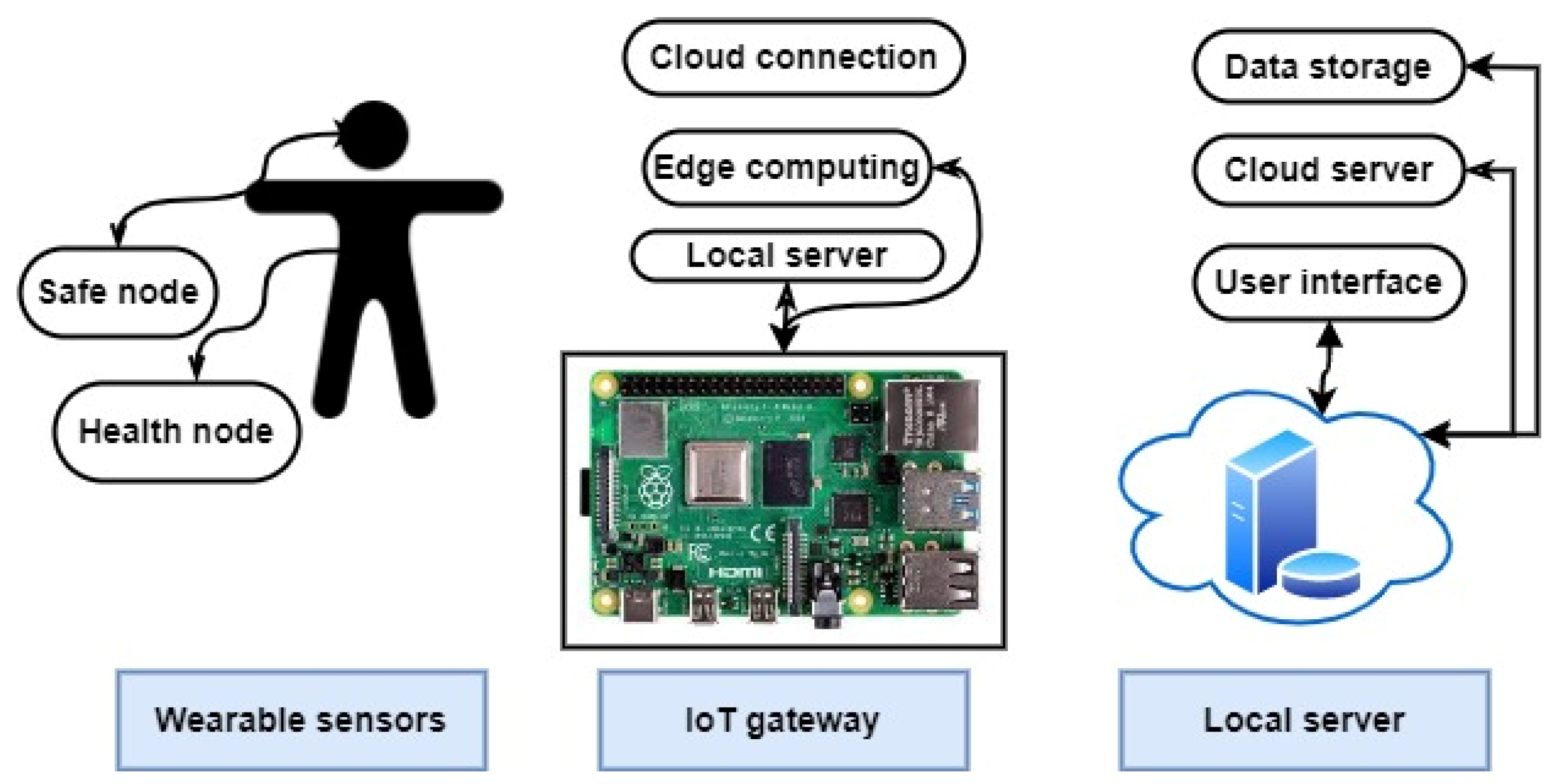
- Remote healthcare: Wireless IoT-driven solutions bring healthcare to patients rather than the patient to healthcare. Data are collected securely through IoT-based sensors, and the data are analyzed by a small algorithm before being shared with health professionals for appropriate recommendations.
- Real-time monitoring: IoT-driven non-invasive-monitoring sensors collect comprehensive psychological information. Gateways and cloud-based analysis manage the storage of data.
- Preventive care: IoT healthcare systems use sensor data, which help with the early detection of emergencies and alerts family members. Machine learning for health-trend tracking and early anomaly detection is achieved through the IoT approach [12].
2.1. The Significance of IoT-Based Healthcare-Monitoring Systems
2.2. Benefits of Using IoT in Healthcare
- Reduced cost of care.
- Human errors are reduced.
- Elimination of the limitations of distance.
- Reduced amounts of paperwork and record keeping.
- Chronic diseases are detected early.
- Improvements in medication management.
- The need for prompt medical care.
- Better treatment outcomes.
3. Review of Recent Related Studies
| Authors with Reference | Aims and Contributions | Methodology | Hardware/Software Technology | Features | Evaluation Metrics | Protocol | Limitations | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gera et al. [6] | A patient health-monitoring system that is built on IoT technology and is connected to the Cloud Talk platform. | Used method known as software development life cycle (SDLC) | LM35, SEN-11574, MAX30102, and BMP 180. | Improves decision-making abilities and streamlines the normal flow of the healthcare system | Temperature, SpO2 level, BP, and pulse rate | IEE 802.11 | Minimal contribution to the administration of medical care for patients | |||||
| Wu, Wu [16] | Developed a small wearable sensor patch that can assess a variety of physiological signals. | Uses a smartphone as the mobile gateway, Raspberry Pi 3 as a fixed gateway, and a BLE module for transmission parameters. | AD8232, PPG, and Si7051 sensors, RFD77101 and Raspberry Pi 3. |
| ECG, HR, BT, and BP. | MQTT | Range and bandwidth limitations. | |||||
| Islam, Rahaman [17] | Proposed a real-time IoT system to monitor patients’ vital signs and the room’s environmental conditions. | Data from sensors are gathered, processed, and uploaded to the cloud using an ESP32. | LM35, Heartbeat Sensor Module, DHT11, MQ-9, MQ-135, and ESP32. | In cases of infectious disease, the system is helpful. | BT and HR, CO, CO2, and humidity. | HTTP |
| |||||
| Al-Sheikh and Ameen [18] | Designed an IoT healthcare-monitoring system that uses a mobile phone. | The system uses Arduino Uno to collect and process sensors’ data, followed by Wi-Fi transmission to the cloud. | Max30102, AD8232, LM35, NodeMCU, and Arduino. |
| HR, SpO2, ECG, and BT | IEEE 802.11 |
| |||||
| Hamim, Paul [19] | Developed a prototype of IoT-based remote health-monitoring system. | The system collects and processes sensor data using Arduino UNO and sends it to the cloud using Raspberry Pi 3. | LM35, HR Sensor Module, GSR sensor, Arduino, and Raspberry Pi 3. |
| HR, BT, and GSR | IEEE 802.11 | System uses two microcontrollers that make it quite big. | |||||
| Swaroop, Chandu [20] | Enhances healthcare delivery by communicating multiplexed data over three modes—BLE, GSM, and Wi-Fi. | Monitoring three parameters and sending data using three modes. | DS18B20, Sunrom BP/ HR monitor, Raspberry Pi 3, BLE adaptor, and USB GSM module. |
| HR, BT, and BP. | MQTT, BLE CSR Mesh | Accuracy depends on the sensors. | |||||
| Gupta, Parikh [21] | Designed a real-time IoT monitoring system to track and evaluate the health of obese adults. Can store the data of multiple patients. | The MCU includes a built-in keyboard, LCD, and all the linked sensors. The keypad gives the user access to the device’s menus and the LCD display. The data are gathered by the ESP8266 and uploaded to the cloud. | MAX30100, LM35, wrist BP and pulse rate monitor, Atmega 328, keypad, LCD, and ESP8266 Wi-Fi Module. |
| BP, BT, pulse rate, and SpO2. | IEEE 802.11 |
| |||||
| Alamsyah, Ikhlayel [22] | Built an IoT-based system to monitor patients’ vital signs. Helps clinicians to make diagnoses. | This system uses Raspberry Pi for processing and communicating with the Internet using Wi-Fi technology. | MCP3008, HRM-2511E, DS18b20, MPX5050DP, and LCD. | Medical staff can access patients’ data through an Android device. | HR, BP, and BT | IEEE 802.11 | Wi-Fi technology is not preferred for long-range application. | |||||
| Sangeethalakshmi et al. [23] | Devised a real-time IoT-based system to track the condition of patients and save lives. | Detects vital parameters and sends them to ESP32 for processing and transferring to the cloud using Wi-Fi module. | LM35, AD8232, MAX30100, BP sensor, and ESP32. |
| Temperature, HR, ECG, BP and SpO2. | Wi-Fi/802.11 | System needs to be evaluated, tested, and reorganized. | |||||
| Sahu, Atulkar [24] | Created an IoT-enabled vital-sign-monitoring system. | Small electrical sensors are fitted to different bodily parts. Body sensor network transmits vital indicators to a controller via wireless or wired means (BSN). | ECG electrodes, pulse Oximeter, NIBP, BT sensors, STM32F103xC, CY8C58LP, and BLE 4.0 module. | System has an Android application and shows high accuracy measurements. | HR, SpO2, temperature, BP, and ECG. | Wi-Fi/802.11 BLE | Not suitable for long-range communication. | |||||
| A. D. Acharya and S. N. Patil [25] |
| The patient’s body has sensors attached. These send body data to the MCU; then, they send the data to the cloud via a Wi-Fi module. | AD8232, LM35, MPX10, Arduino, and Raspberry Pi Module. |
| ECG, temperature, and BP. | IEEE 802.11 | Wi-Fi technology is not preferred for long-range application. | |||||
| Jennifer S. Raj [26] | Innovative Big Data-processing platform for IoT-based healthcare-monitoring system. | Data processing is divided into three stages: collection and aggregation, classification and analysis of collected data, and decision-making. |
| In comparison to the traditional model, it is efficient in the process of handling data and extracting information. | Data management, storage, f-measure, sensitivity, and specificity | Not provided | Data-processing time is not entertained. | |||||
| Kishor and Chakraborty [27] | An approach to medical care that is underpinned by fog computing and makes use of AI and IoT | Three phases are involved. First, data are collected; then, they are pre-processed and computed; and lastly, the results are made visible to doctors or end-users and stored in the cloud. |
| This model assists medical professionals in making accurate and timely diagnoses of the disease. | Heart disease, diabetes, breast cancer, hepatitis, liver disorder, dermatology, surgery data, and thyroid data. | Not provided | Predicts only the common diseases | |||||
| Souri et al. [28] | A student healthcare-monitoring system based on the IoT. | This methodology has three levels: finding the relevant data, collecting the data, and pre-processing the data. |
| Utilizes innovative medical technologies and identifies changes. | Biological and behavioral changes. | Not provided |
| |||||
| Kaur et al. [29] | Enhancing the interaction between patients and medical professionals | Eight datasets on different diseases were used to test the proposed work. | Five machine learning techniques. | Provides automatic recommendations. | Accuracy and area under the curve | Not provided | The performance comparison displayed here only includes accuracy and area under curve (AUC). | |||||
| SoonHyeong et al. [30] | Enhanced reliability and security through the implementation of blockchain technology. | This study used blockchain-based IoT. Several sensors were used to assess ECG data. | Integrated sensor module |
| BP, HR, temperature, weight, and ECG | BLE | Stored data/information can be transferred through smartphone only. | |||||
| Piyush et al. [31] | Offers a mechanism for improving the quality of life of Alzheimer’s patients, and also benefits the people who care for them. | The study utilized IoT-based sensor data to determine various patient body parameters. All these sensors, attached to the MCU, are then transferred to the cloud. | LM35, pulse sensor, Gyroscope MPU6050, Atmega328 microcontroller, and ESP8266. | Dynamic estimation. | BT, BP, striding action, and speed. | IEEE 802.11 | Cannot predict the condition of the patient before the situation becomes worse. | |||||
| Hashim et al. [32] | Developed an IoT-based healthcare-monitoring system with multiple sensors and a smart security system. | Multiple sensors are connected to Arduino, and the collected data are presented on an LCD. The Wi-Fi module transmits data to the cloud. | DHT11, pulse sensor, mlx 90164, Arduino, LCD, and ESP8266 Wi-Fi module. |
| HR, BT, room temperature, and humidity. | IEEE 802.11 | The size of the prototype needs to be reduced and enhanced. | |||||
| Mostafa et al. [33] | Designed an IoT that can monitor patients’ readings continuously; keeps the data on display in front of the patient and on the screen of the doctor’s mobile device. | Three sensors are read by MCU with availability to represent the data locally and remotely. | Max30100, DS18B20, IR sensor, NodeMCU, and LCD. |
| HR, SpO2, and temperature | Wi-Fi/802.11 | The prototype’s size should be minimized. | |||||
| Jenifer et al. [34] | Designed an IoT based on electronic sensors to monitor patient healthcare remotely. | Sensors collect data on various physical factors and upload them to the cloud database over Wi-Fi. | LM35, Arduino Uno, SIM300, GPS shield. | Automatic emergency alert message and location can be sent. | HR, temperature, BP, and SpO2 level | IEEE 802.11 |
| |||||
| Dhruba et al. [35] | Developed a real-time sleep apnea-monitoring system based on the IoT. | Takes readings of sensors and measures several sleep indices, and alerts users via a mobile application when anything unusual occurs. | Max 30102, pulse sensor, GSR sensor, AD8232 and sound sensor, Arduino Uno, and Bluetooth module. |
| GSR, ECG, HR, sound, and SpO2. | BLE | During sleep, the worn device can be detached and feel uncomfortable to the patient. | |||||
| Tiwari et al. [37] | Designed a system for remote monitoring of healthcare based on IoT. | Performs ongoing observation of a patient’s vital signs and detects the presence of abnormalities. | LM35, MAX30100, AD8232 and IR sensors, NodeMCU, and Arduino IDE. | Simple to operate and affordable due to its high level of cost effectiveness. | HR, temperature, and ECG. | MQTT, HTTP IEEE 802.11 |
| |||||
| Vaneeta et al. [38] | Conceived and built an intelligent health-monitoring system based on the IoT. | Consists of three primary steps: data collection, data processing, data storage, and the display of patients’ parameters locally and remotely. | MLX90614 and MAX30100 sensors, BP serial port, LCD, and Raspberry Pi. | This system will send an alert to the attending doctor or physician if there have been any deviations from the normal values of the patient’s health. | BP, HR, SpO2, and temperature. | IEEE 802.11 | Need to increase the security of patients’ data and decrease the data-transfer delay. | |||||
| Khan et al. [39] | Established a mechanism for measuring multiple health indicators quickly. | Sensors capture information on various physical factors and upload them to the cloud using the Bluetooth module. | LM35, MAX30100, Arduino UNO, Bluetooth module, and LCD. | Data can be monitored using mobile app. | BT, HR, and SpO2. | BLE | The size of prototype needs to be enhanced. | |||||
- The IoT has the potential to be integrated with a wide variety of devices, which is not possible with most of the systems that are currently in use.
- There is the possibility that the data that are stored will not be protected.
- Complex systems have many disconnects between the various people, stages, and procedures.
- An investigation into the circumstances surrounding an accident will typically reveal the existence of several gaps, but gaps themselves are rarely the cause of accidents.
- The ability to understand and reinforce the normal ability of practitioners in order to bridge gaps contributes to an increase in overall safety.
- The conventional viewpoint, which maintains that systems ought to be shielded from the unreliable influence of humans, is challenged by this point of view.
- We have a limited understanding of how professionals pinpoint newly formed gaps and devise solutions to close them when systems undergo transformation.
4. Internet of Wearable Things
4.1. Wireless Network Technologies for IoT Healthcare
4.2. Wearable Sensors in Healthcare-Monitoring Systems
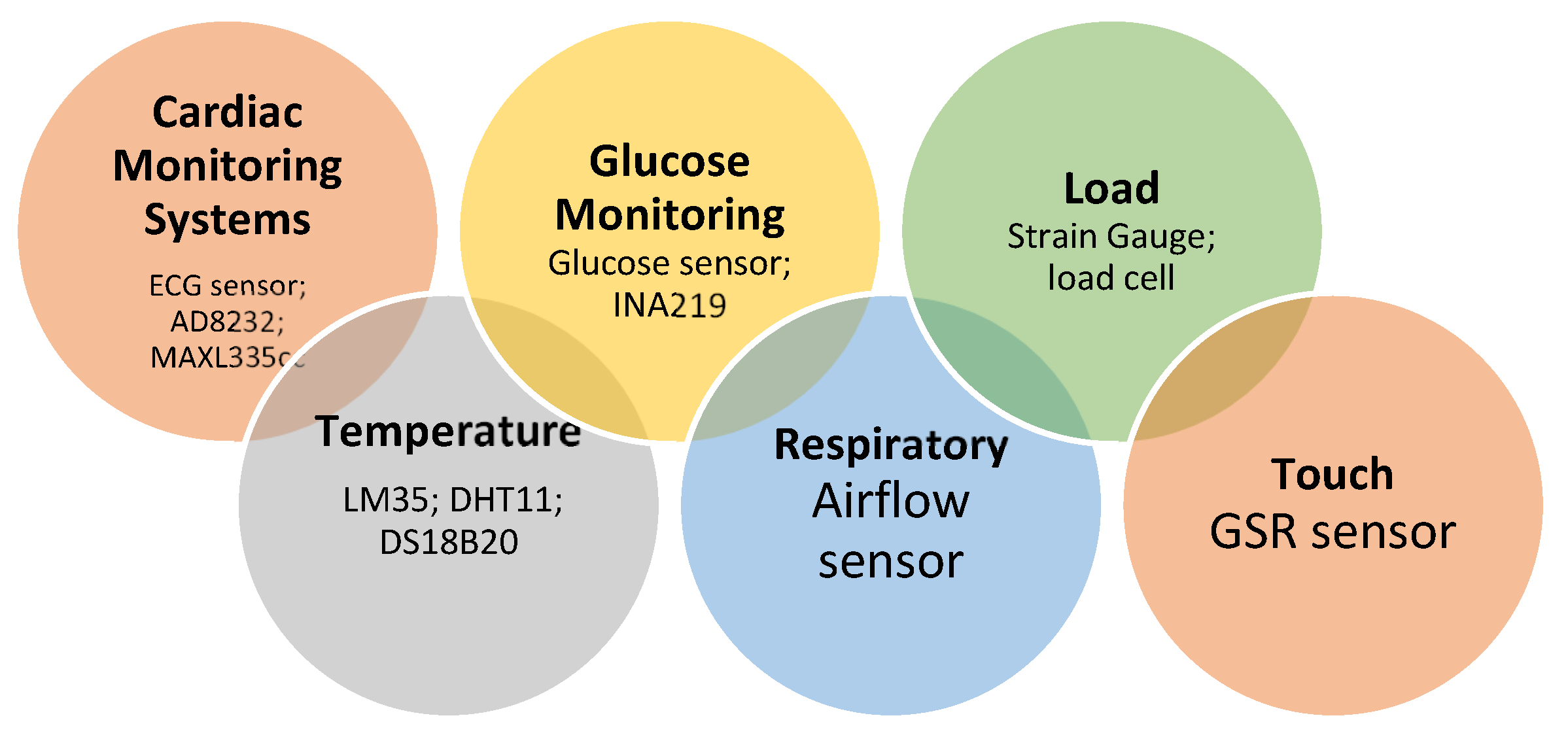
4.2.1. Use Cases of Health-Monitoring Sensors
Use Cases/Applications
- Heart-rate detection/Cardiac monitoring systems/Stroke
- 2.
- Body-temperature measuring
- 3.
- Activity recognition
- 4.
- Blood-glucose monitoring and hemoglobin concentration
- 5.
- Respiration-rate detection and monitoring
- 6.
- Sleep monitoring
- 7.
- Alzheimer’s disease monitoring and Anemia detection
- 8.
- Molecular diagnostics and Clinical diagnosis
- 9.
- Blood-oxygen-saturation detection
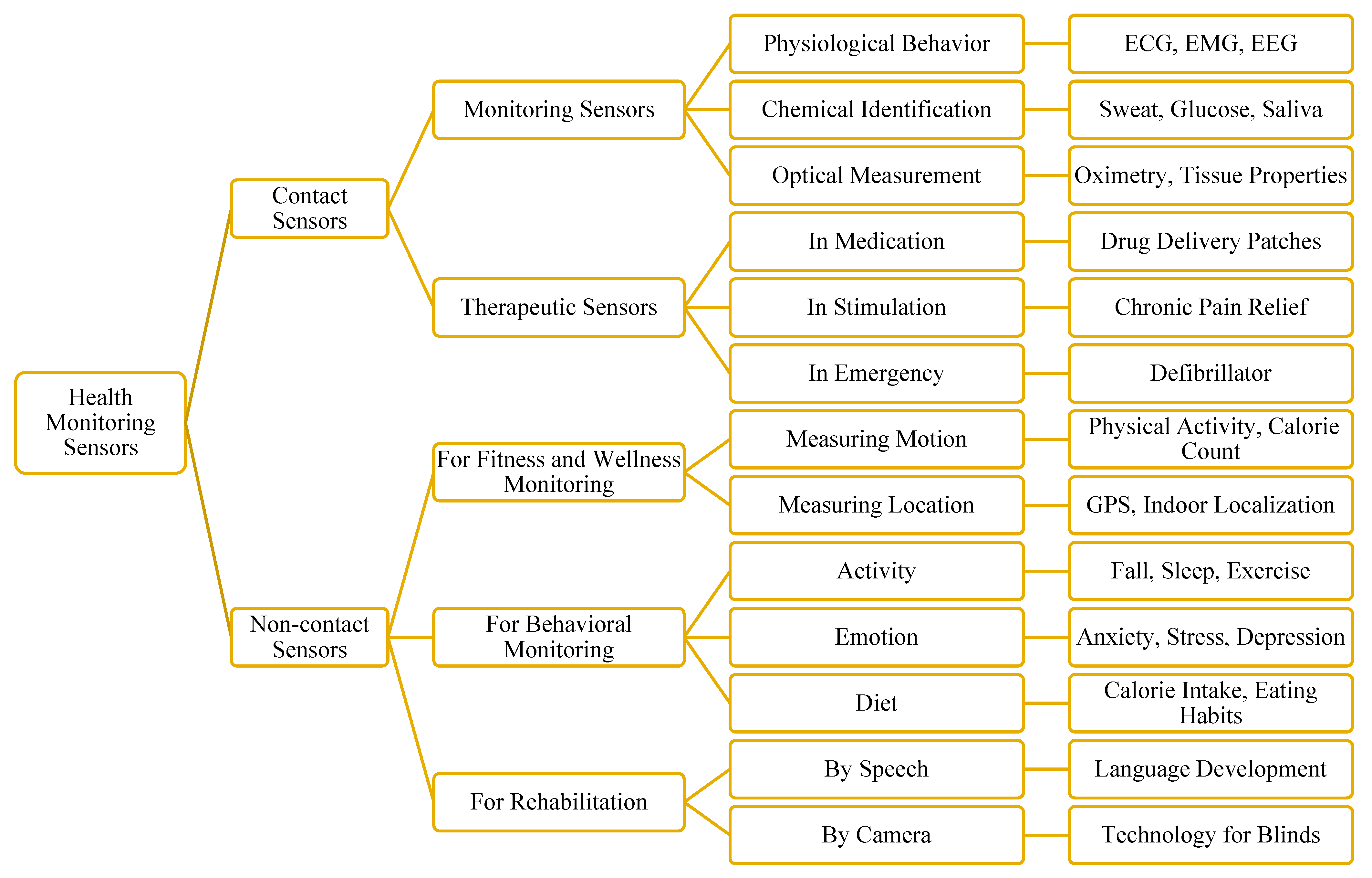
4.2.2. Classification of Health-Monitoring Sensors
- Monitoring vital signs in hospitals.
- Aging in place and in motion.
- Assistance with motor and sensory impairments.
- Large-scale medical and behavioral research in the field.
4.2.3. Performance Evaluation of IoT Sensors
5. Security and Protocols for IoT Healthcare-Monitoring Systems
6. IoT Healthcare Challenges and Open Issues
6.1. Security-Based: Security and Privacy
6.2. QoS-Based: Performance, Fuctional Stability and Reliability, and Cost
6.3. Computational Intelligence-Based
6.4. Integration-Based
6.5. Energy-Based
6.6. Disease-Prediction-Based
7. Suggestions and Recommendations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Farhan, L.; Hameed, R.S.; Ahmed, A.S.; Fadel, A.H.; Gheth, W.; Alzubaidi, L.; Fadhel, M.A.; Al-Amidie, M. Energy Efficiency for Green Internet of Things (IoT) Networks: A Survey. Network 2021, 1, 279–314. [Google Scholar] [CrossRef]
- Alekya, R.; Boddeti, N.D.; Monica, K.S.; Prabha, R.; Venkatesh, V. IoT based smart healthcare monitoring systems: A literature review. Eur. J. Mol. Clin. Med. 2021, 7, 2020. [Google Scholar]
- Naveen; Sharma, R.K.; Nair, A.R. IoT-based Secure Healthcare Monitoring System. In Proceedings of the 2019 IEEE International Conference on Electrical, Computer and Communication Technologies (ICECCT), Coimbatore, India, 20–22 February 2019; pp. 1–6. [Google Scholar]
- Rathi, V.K.; Rajput, N.K.; Mishra, S.; Grover, B.A.; Tiwari, P.; Jaiswal, A.K.; Hossain, M.S. An edge AI-enabled IoT healthcare monitoring system for smart cities. Comput. Electr. Eng. 2021, 96, 107524. [Google Scholar] [CrossRef]
- Alshamrani, M. IoT and artificial intelligence implementations for remote healthcare monitoring systems: A survey. J. King Saud Univ. Comput. Inf. Sci. 2022, 34, 4687–4701. [Google Scholar] [CrossRef]
- Gera, S.; Mridul, M.; Sharma, S. IoT based Automated Health Care Monitoring System for Smart City. In Proceedings of the 2021 5th International Conference on Computing Methodologies and Communication (ICCMC), Erode, India, 8–10 April 2021; pp. 364–368. [Google Scholar]
- Bhatia, H.; Panda, S.N.; Nagpal, D. Internet of Things and its Applications in Healthcare—A Survey. In Proceedings of the 2020 8th International Conference on Reliability, Infocom Technologies and Optimization (Trends and Future Directions) (ICRITO), Noida, India, 4–5 June 2020; pp. 305–310. [Google Scholar]
- Jain, U.; Gumber, A.; Ajitha, D.; Rajini, G.; Subramanian, B. A Review on a Secure IoT-Based Healthcare System. In Proceedings of the Advances in Automation, Signal Processing, Instrumentation, and Control: Select Proceedings of i-CASIC, India, 27–28 February 2020; pp. 3005–3016. [Google Scholar]
- Kumar, R.; Rajasekaran, M.P. An IoT based patient monitoring system using raspberry Pi. In Proceedings of the 2016 International Conference on Computing Technologies and Intelligent Data Engineering (ICCTIDE’16), Kovilpatti, India, 7–9 January 2016; pp. 1–4. [Google Scholar]
- Meliá, S.; Nasabeh, S.; Luján-Mora, S.; Cachero, C. MoSIoT: Modeling and Simulating IoT Healthcare-Monitoring Systems for People with Disabilities. Int. J. Environ. Res. Public Health 2021, 18, 6357. [Google Scholar] [CrossRef]
- Philip, N.Y.; Rodrigues, J.J.P.C.; Wang, H.; Fong, S.J.; Chen, J. Internet of Things for In-Home Health Monitoring Systems: Current Advances, Challenges and Future Directions. IEEE J. Sel. Areas Commun. 2021, 39, 300–310. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Gupta, S.N.; Gupta, M.; Tiwari, P. IoT based Healthware and Healthcare Monitoring System in India. In Proceedings of the 2021 International Conference on Advance Computing and Innovative Technologies in Engineering (ICACITE), Greater Noida, India, 4–5 March 2021; pp. 406–408. [Google Scholar]
- Patel, W.D.; Patel, C.; Valderrama, C. IoMT based Efficient Vital Signs Monitoring System for Elderly Healthcare Using Neural Network. Int. J. Res. 2019, VIII, 239. [Google Scholar]
- Li, C.; Hu, X.; Zhang, L. The IoT-based heart disease monitoring system for pervasive healthcare service. Procedia Comput. Sci. 2017, 112, 2328–2334. [Google Scholar] [CrossRef]
- Cao, H.-R.; Zhan, C. A Novel Emergency Healthcare System for Elderly Community in Outdoor Environment. Wirel. Commun. Mob. Comput. 2018, 2018, 7841026. [Google Scholar] [CrossRef]
- Wu, T.; Wu, F.; Qiu, C.; Redouté, J.M.; Yuce, M.R. A Rigid-Flex Wearable Health Monitoring Sensor Patch for IoT-Connected Healthcare Applications. IEEE Internet Things J. 2020, 7, 6932–6945. [Google Scholar] [CrossRef]
- Islam, M.M.; Rahaman, A.; Islam, M.R. Development of smart healthcare monitoring system in IoT environment. SN Comput. Sci. 2020, 1, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Al-Sheikh, M.A.; Ameen, I.A. Design of mobile healthcare monitoring system using IoT technology and cloud computing. In Proceedings of the IOP Conference Series: Materials Science and Engineering, Baghdad, Iraq, 15 April 2020; p. 012113. [Google Scholar]
- Hamim, M.; Paul, S.; Hoque, S.I.; Rahman, M.N.; Baqee, I. IoT Based Remote Health Monitoring System for Patients and Elderly People. In Proceedings of the 2019 International Conference on Robotics, Electrical and Signal Processing Techniques (ICREST), Dhaka, Bangladesh, 10–12 January 2019; pp. 533–538. [Google Scholar]
- Swaroop, K.N.; Chandu, K.; Gorrepotu, R.; Deb, S. A health monitoring system for vital signs using IoT. Internet Things 2019, 5, 116–129. [Google Scholar] [CrossRef]
- Gupta, D.; Parikh, A.; Swarnalatha, R. Integrated healthcare monitoring device for obese adults using internet of things (IoT). Int. J. Electr. Comput. Eng. 2020, 10, 1239–1247. [Google Scholar] [CrossRef]
- Alamsyah, M.S.; Ikhlayel, M.; Setijadi, E. Internet of things–based vital sign monitoring system. Int. J. Electr. Comput. Eng. 2020, 10, 5891–5898. [Google Scholar] [CrossRef]
- Manoj, A.S.; Hussain, M.A.; Teja, P.S. Patient health monitoring system using IoT. Mater. Today Proc. 2021, 2214–7853. Available online: https://reader.elsevier.com/reader/sd/pii/S2214785321045545?token=8754B71C6BCB0D29EE25147CAB93A0B1F81C57B14222BA15DC7F113D8FCF4283FA11801D93C5D41DE78990D489B38BE3&originRegion=eu-west-1&originCreation=20221008165401 (accessed on 5 October 2022). [CrossRef]
- Sahu, M.L.; Atulkar, M.; Ahirwal, M.K.; Ahamad, A. Vital Sign Monitoring System for Healthcare Through IoT Based Personal Service Application. Wirel. Pers. Commun. 2021, 122, 129–156. [Google Scholar] [CrossRef]
- Acharya, A.D.; Patil, S.N. IoT based Health Care Monitoring Kit. In Proceedings of the 2020 Fourth International Conference on Computing Methodologies and Communication (ICCMC), Erode, India, 11–13 March 2020; pp. 363–368. [Google Scholar]
- Raj, J.S. A novel information processing in IoT based real time health care monitoring system. J. Electron. 2020, 2, 188–196. [Google Scholar]
- Kishor, A.; Chakraborty, C. Artificial Intelligence and Internet of Things Based Healthcare 4.0 Monitoring System. Wirel. Pers. Commun. 2021, 1–17. Available online: https://link.springer.com/content/pdf/10.1007/s11277-021-08708-5.pdf (accessed on 5 October 2022). [CrossRef]
- Souri, A.; Ghafour, M.Y.; Ahmed, A.M.; Safara, F.; Yamini, A.; Hoseyninezhad, M. A new machine learning-based healthcare monitoring model for student’s condition diagnosis in Internet of Things environment. Soft Comput. 2020, 24, 17111–17121. [Google Scholar] [CrossRef]
- Kaur, P.; Kumar, R.; Kumar, M. A healthcare monitoring system using random forest and internet of things (IoT). Multimed. Tools Appl. 2019, 78, 19905–19916. [Google Scholar] [CrossRef]
- Jeong, S.; Shen, J.-H.; Ahn, B. A Study on Smart Healthcare Monitoring Using IoT Based on Blockchain. Wirel. Commun. Mob. Comput. 2021, 2021, 9932091. [Google Scholar] [CrossRef]
- Yadav, P.; Kumar, P.; Kishan, P.; Raj, P.; raj, U. Development of Pervasive IoT Based Healthcare Monitoring System for Alzheimer Patients. J. Phys. Conf. Ser. 2021, 2007, 012035. [Google Scholar] [CrossRef]
- Hashim, H.; Salihudin, S.F.B.; Saad, P.S.M. Development of IoT Based Healthcare Monitoring System. In Proceedings of the 2022 IEEE International Conference in Power Engineering Application (ICPEA), Selangor, Malaysia, 7–8 March 2022; pp. 1–5. [Google Scholar]
- Mostafa, S.M.G.; Zaki, M.; Islam, M.M.; Alam, M.S.; Ullah, M.A. Design and Implementation of an IoT-Based Healthcare Monitoring System. In Proceedings of the 2022 International Conference on Innovations in Science, Engineering and Technology (ICISET), Chittagong, Bangladesh, 26–27 February 2022; pp. 362–366. [Google Scholar]
- Jenifer, M.; Rinesh, S.; Thamaraiselvi, K. Internet of Things (IOT) based Patient health care Monitoring System using electronic gadget. In Proceedings of the 2022 6th International Conference on Intelligent Computing and Control Systems (ICICCS), Madurai, India, 25–27 May 2022; pp. 487–490. [Google Scholar]
- Dhruba, A.R.; Alam, K.N.; Khan, M.S.; Bourouis, S.; Khan, M.M. Development of an IoT-Based Sleep Apnea Monitoring System for Healthcare Applications. Comput. Math. Methods Med. 2021, 2021, 7152576. [Google Scholar] [CrossRef]
- Kshirsagar, P.; Pote, A.; Paliwal, K.K.; Hendre, V.; Chippalkatti, P.; Dhabekar, N. A Review on IOT Based Health Care Monitoring System. In Proceedings of the ICCCE 2019, Pune, India, February 2019; Springer: Singapore, 2019; pp. 95–100. [Google Scholar]
- Tiwari, A.; Parate, N.; Khamari, M.; Jaiswal, A.; Joshi, P.; Jadhav, P. IOT Based Health Care Monitoring and Facilitation. In Proceedings of the 2022 10th International Conference on Emerging Trends in Engineering and Technology—Signal and Information Processing (ICETET-SIP-22), Nagpur, India, 29–30 April 2022; pp. 1–6. [Google Scholar]
- Bhardwaj, V.; Joshi, R.; Gaur, A.M. IoT-Based Smart Health Monitoring System for COVID-19. SN Comput. Sci. 2022, 3, 137. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.M.; Alanazi, T.M.; Albraikan, A.A.; Almalki, F.A. IoT-Based Health Monitoring System Development and Analysis. Secur. Commun. Netw. 2022, 2022, 9639195. [Google Scholar] [CrossRef]
- Rahman, M.; Mehedi Shamrat, F.; Kashem, M.A.; Akter, M.; Chakraborty, S.; Ahmed, M.; Mustary, S. Internet of things based electrocardiogram monitoring system using machine learning algorithm. Int. J. Electr. Comput. Eng. 2022, 12, 3739–3751. [Google Scholar]
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A survey of wearable devices and challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620. [Google Scholar] [CrossRef]
- Hiremath, S.; Yang, G.; Mankodiya, K. Wearable Internet of Things: Concept, architectural components and promises for person-centered healthcare. In Proceedings of the 2014 4th International Conference on Wireless Mobile Communication and Healthcare—Transforming Healthcare Through Innovations in Mobile and Wireless Technologies (MOBIHEALTH), Athens, Greece, 3–5 November 2014; pp. 304–307. [Google Scholar]
- Misran, N.; Islam, M.S.; Beng, G.K.; Amin, N.; Islam, M.T. IoT Based Health Monitoring System with LoRa Communication Technology. In Proceedings of the 2019 International Conference on Electrical Engineering and Informatics (ICEEI), Bandung, Indonesia, 9–10 July 2019; pp. 514–517. [Google Scholar]
- Dias, R.M.; Marques, G.; Bhoi, A.K. Internet of Things for Enhanced Food Safety and Quality Assurance: A Literature Review. Adv. Electron. Commun. Comput. 2021, 709, 653–663. [Google Scholar]
- Almuhaya, M.A.; Jabbar, W.A.; Sulaiman, N.; Abdulmalek, S. A survey on Lorawan technology: Recent trends, opportunities, simulation tools and future directions. Electronics 2022, 11, 164. [Google Scholar] [CrossRef]
- Desai, M.R.; Toravi, S. A Smart Sensor Interface for Smart Homes and Heart Beat Monitoring using WSN in IoT Environment. In Proceedings of the 2017 International Conference on Current Trends in Computer, Electrical, Electronics and Communication (CTCEEC), Mysore, India, 8–9 September 2017; pp. 74–77. [Google Scholar]
- Malapane, T.J. A Cyber-Physical System for Smart Healthcare; University of Johannesburg: Johannesburg, South Africa, 2020. [Google Scholar]
- Vedaei, S.S.; Fotovvat, A.; Mohebbian, M.R.; Rahman, G.M.E.; Wahid, K.A.; Babyn, P.; Marateb, H.R.; Mansourian, M.; Sami, R. COVID-SAFE: An IoT-Based System for Automated Health Monitoring and Surveillance in Post-Pandemic Life. IEEE Access 2020, 8, 188538–188551. [Google Scholar] [CrossRef]
- Wu, F.; Wu, T.; Yuce, M.R. Design and Implementation of a Wearable Sensor Network System for IoT-Connected Safety and Health Applications. In Proceedings of the 2019 IEEE 5th World Forum on Internet of Things (WF-IoT), Limerick, Ireland, 15–18 April 2019; pp. 87–90. [Google Scholar]
- Wan, J.; AAH Al-awlaqi, M.; Li, M.; O’Grady, M.; Gu, X.; Wang, J.; Cao, N. Wearable IoT enabled real-time health monitoring system. EURASIP J. Wirel. Commun. Netw. 2018, 2018, 298. [Google Scholar] [CrossRef]
- Mamdiwar, S.D.; Shakruwala, Z.; Chadha, U.; Srinivasan, K.; Chang, C.-Y. Recent advances on IoT-assisted wearable sensor systems for healthcare monitoring. Biosensors 2021, 11, 372. [Google Scholar] [CrossRef]
- Pal, A.; Visvanathan, A.; Choudhury, A.D.; Sinha, A. Improved heart rate detection using smart phone. In Proceedings of the 29th Annual ACM Symposium on Applied Computing, Gyeongju, Korea, 24–28 March 2014; pp. 8–13. [Google Scholar]
- Gogate, U.; Bakal, J. Healthcare monitoring system based on wireless sensor network for cardiac patients. Biomed. Pharmacol. J. 2018, 11, 1681. [Google Scholar] [CrossRef]
- Arun, U.; Natarajan, S.; Rajanna, R.R. A novel IoT cloud-based real-time cardiac monitoring approach using NI myRIO-1900 for telemedicine applications. In Proceedings of the 2018 3rd International Conference on Circuits, Control, Communication and Computing (I4C), Bangalore, India, 3–5 October 2018; pp. 1–4. [Google Scholar]
- Pal, A.; Sinha, A.; Dutta Choudhury, A.; Chattopadyay, T.; Visvanathan, A. A robust heart rate detection using smart-phone video. In Proceedings of the 3rd ACM MobiHoc Workshop on Pervasive Wireless Healthcare, Bangalore, India, 29 July 2013; pp. 43–48. [Google Scholar]
- Gaoan, G.; Zhenmin, Z. Heart rate measurement via smart phone acceleration sensor. In Proceedings of the 2014 International Conference on Smart Computing, Hong Kong, China, 3–5 November 2014; pp. 295–300. [Google Scholar]
- Saha, R.; Biswas, S.; Sarmah, S.; Karmakar, S.; Das, P. A Working Prototype Using DS18B20 Temperature Sensor and Arduino for Health Monitoring. SN Comput. Sci. 2021, 2, 1–21. [Google Scholar]
- Adeniyi, E.A.; Ogundokun, R.O.; Awotunde, J.B. IoMT-based wearable body sensors network healthcare monitoring system. In IoT in Healthcare and Ambient Assisted Living; Springer: Berlin/Heidelberg, Germany, 2021; pp. 103–121. [Google Scholar]
- Fan, Z.; Zhou, Y.; Zhai, H.; Wang, Q.; He, H. A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy. Biosensors 2022, 12, 781. [Google Scholar] [CrossRef]
- Charlton, P.H.; Birrenkott, D.A.; Bonnici, T.; Pimentel, M.A.; Johnson, A.E.; Alastruey, J.; Tarassenko, L.; Watkinson, P.J.; Beale, R.; Clifton, D.A. Breathing rate estimation from the electrocardiogram and photoplethysmogram: A review. IEEE Rev. Biomed. Eng. 2017, 11, 2–20. [Google Scholar] [CrossRef]
- Karlen, W.; Garde, A.; Myers, D.; Scheffer, C.; Ansermino, J.M.; Dumont, G.A. Estimation of respiratory rate from photoplethysmographic imaging videos compared to pulse oximetry. IEEE J. Biomed. Health Inform. 2015, 19, 1331–1338. [Google Scholar] [CrossRef]
- Haghi, M.; Neubert, S.; Geissler, A.; Fleischer, H.; Stoll, N.; Stoll, R.; Thurow, K. A flexible and pervasive IoT-based healthcare platform for physiological and environmental parameters monitoring. IEEE Internet Things J. 2020, 7, 5628–5647. [Google Scholar] [CrossRef]
- Pirani, E.Z.; Bulakiwala, F.; Kagalwala, M.; Kalolwala, M.; Raina, S. Android based assistive toolkit for alzheimer. Procedia Comput. Sci. 2016, 79, 143–151. [Google Scholar] [CrossRef]
- Batsis, J.A.; Boateng, G.G.; Seo, L.M.; Petersen, C.L.; Fortuna, K.L.; Wechsler, E.V.; Peterson, R.J.; Cook, S.B.; Pidgeon, D.; Dokko, R.S. Development and usability assessment of a connected resistance exercise band application for strength-monitoring. World Acad. Sci. Eng. Technol. 2019, 13, 340. [Google Scholar]
- Wang, R.; Aung, M.S.; Abdullah, S.; Brian, R.; Campbell, A.T.; Choudhury, T.; Hauser, M.; Kane, J.; Merrill, M.; Scherer, E.A. CrossCheck: Toward passive sensing and detection of mental health changes in people with schizophrenia. In Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Heidelberg, Germany, 12–16 September 2016; pp. 886–897. [Google Scholar]
- Ghatpande, N.S.; Apte, P.P.; Joshi, B.N.; Naik, S.S.; Bodas, D.; Sande, V.; Uttarwar, P.; Kulkarni, P.P. Development of a novel smartphone-based application for accurate and sensitive on-field hemoglobin measurement. RSC Adv. 2016, 6, 104067–104072. [Google Scholar] [CrossRef]
- Li, P.; Lee, G.-H.; Kim, S.Y.; Kwon, S.Y.; Kim, H.-R.; Park, S. From diagnosis to treatment: Recent advances in patient-friendly biosensors and implantable devices. ACS Nano 2021, 15, 1960–2004. [Google Scholar] [CrossRef]
- Song, J.; Pandian, V.; Mauk, M.G.; Bau, H.H.; Cherry, S.; Tisi, L.C.; Liu, C. Smartphone-based mobile detection platform for molecular diagnostics and spatiotemporal disease mapping. Anal. Chem. 2018, 90, 4823–4831. [Google Scholar] [CrossRef]
- Hussain, S.; Chen, X.; Wang, C.; Hao, Y.; Tian, X.; He, Y.; Li, J.; Shahid, M.; Iyer, P.K.; Gao, R. Aggregation and Binding-Directed FRET Modulation of Conjugated Polymer Materials for Selective and Point-of-Care Monitoring of Serum Albumins. Anal. Chem. 2022, 94, 10685–10694. [Google Scholar] [CrossRef]
- Muthuraj, B.; Hussain, S.; Iyer, P.K. A rapid and sensitive detection of ferritin at a nanomolar level and disruption of amyloid β fibrils using fluorescent conjugated polymer. Polym. Chem. 2013, 4, 5096–5107. [Google Scholar] [CrossRef]
- Lu, W.; Bai, W.; Zhang, H.; Xu, C.; Chiarelli, A.M.; Vázquez-Guardado, A.; Xie, Z.; Shen, H.; Nandoliya, K.; Zhao, H. Wireless, implantable catheter-type oximeter designed for cardiac oxygen saturation. Sci. Adv. 2021, 7, eabe0579. [Google Scholar] [CrossRef]
- Muratyan, A.; Cheung, W.; Dibbo, S.V.; Vhaduri, S. Opportunistic multi-modal user authentication for health-tracking IoT wearables. In Proceedings of the The Fifth International Conference on Safety and Security with IoT, Da Nang, Vietnam, 25 April 2021; pp. 1–18. [Google Scholar]
- Fang, D.; Hu, J.; Wei, X.; Shao, H.; Luo, Y. A smart phone healthcare monitoring system for oxygen saturation and heart rate. In Proceedings of the 2014 International Conference on Cyber-Enabled Distributed Computing and Knowledge Discovery, Shanghai, China, 13–15 October 2014; pp. 245–247. [Google Scholar]
- Nemcova, A.; Jordanova, I.; Varecka, M.; Smisek, R.; Marsanova, L.; Smital, L.; Vitek, M. Monitoring of heart rate, blood oxygen saturation, and blood pressure using a smartphone. Biomed. Signal Process. Control 2020, 59, 101928. [Google Scholar] [CrossRef]
- Singh, P. Internet of things based health monitoring system: Opportunities and challenges. Int. J. Adv. Res. Comput. Sci. 2018, 9, 224–228. [Google Scholar] [CrossRef]
- Ko, J.; Lu, C.; Srivastava, M.B.; Stankovic, J.A.; Terzis, A.; Welsh, M. Wireless sensor networks for healthcare. Proc. IEEE 2010, 98, 1947–1960. [Google Scholar] [CrossRef]
- Rashmi, I.; Sahana, M.; Sangeetha, R.; Shruthi, K. IOT based Patient Health Monitoring System to Remote Doctors using Embedded Technology. Int. J. Eng. Res. Technol. 2020, 8, 230–233. [Google Scholar]
- Prakash, B.; Nagesh, M.; Mukunda, D.; Gowda, C. Arm Based Health Care Monitoring Services Using Wireless Network. Int. Res. J. Mod. Eng. Technol. Sci. 2020, 2. Available online: https://www.researchgate.net/profile/Mukunda-D-S/publication/341607121_ARM_BASED_HEALTH_CARE_MONITORING_SERVICES_USING_WIRELESS_NETWORK/links/5eca2d6792851c11a884f973/ARM-BASED-HEALTH-CARE-MONITORING-SERVICES-USING-WIRELESS-NETWORK.pdf (accessed on 5 October 2022).
- Misbahuddin, S.; Al-Ahdal, A.R.; Malik, M.A. Low-Cost MPI Cluster Based Distributed in-Ward Patients Monitoring System. In Proceedings of the 2018 IEEE/ACS 15th International Conference on Computer Systems and Applications (AICCSA), Aqaba, Jordan, 28 October–1 November 2018; pp. 1–6. [Google Scholar]
- Patil, H.; Manohare, S.; Magdum, S.; Gore, M.S. Smart Healthcare Monitoring and Patient Report Generation System Using IOT. Int. J. Res. Appl. Sci. Eng. Technol. 2020, 8. Available online: https://www.academia.edu/43408033/Smart_Healthcare_Monitoring_and_Patient_Report_Generation_System_using_IOT (accessed on 5 October 2022). [CrossRef]
- Mhatre, P.; Shaikh, A.; Khanvilkar, S. Non Invasive E-Health Care Monitoring System Using IOT. Int. J. Innov. Res. Technol. 2020, 6, 307–311. [Google Scholar]
- Zaman, F.; Lee, S.; Rahim, M.K.; Khan, S. Smart Antennas and Intelligent Sensors Based Systems: Enabling Technologies and Applications; Hindawi: London, UK, 2019; Volume 2019. [Google Scholar]
- El Zouka, H.A.; Hosni, M.M. Secure IoT communications for smart healthcare monitoring system. Internet Things 2021, 13, 100036. [Google Scholar] [CrossRef]
- Gholamhosseini, L.; Sadoughi, F.; Ahmadi, H.; Safaei, A. Health internet of things: Strengths, weakness, opportunity, and threats. In Proceedings of the 2019 5th International Conference on Web Research (ICWR), Tehran, Iran, 24–25 April 2019; pp. 287–296. [Google Scholar]
- Safavi, S.; Meer, A.M.; Melanie, E.K.J.; Shukur, Z. Cyber vulnerabilities on smart healthcare, review and solutions. In Proceedings of the 2018 Cyber Resilience Conference (CRC), Putrajaya, Malaysia, 13–15 November 2018; pp. 1–5. [Google Scholar]
- Pacheco, J.; Ibarra, D.; Vijay, A.; Hariri, S. IoT security framework for smart water system. In Proceedings of the 2017 IEEE/ACS 14th International Conference on Computer Systems and Applications (AICCSA), Hammamet, Tunisia, 30 October 2017–3 November 2017; pp. 1285–1292. [Google Scholar]
- Nasiri, S.; Sadoughi, F.; Tadayon, M.H.; Dehnad, A. Security requirements of internet of things-based healthcare system: A survey study. Acta Inform. Med. 2019, 27, 253. [Google Scholar] [CrossRef]
- Islam, M.; Nooruddin, S.; Karray, F.; Muhammad, G. Internet of Things Device Capabilities, Architectures, Protocols, and Smart Applications in Healthcare Domain: A Review. arXiv 2022, arXiv:2204.05921. [Google Scholar]
- Silva, J.d.C.; Rodrigues, J.J.; Al-Muhtadi, J.; Rabêlo, R.A.; Furtado, V. Management platforms and protocols for internet of things: A survey. Sensors 2019, 19, 676. [Google Scholar] [CrossRef]
- Kanakaris, V.; Papakostas, G.A. Internet of things protocols—A survey. Int. J. Humanit. Technol. 2020, 1, 101–117. [Google Scholar] [CrossRef]
- Bhuiyan, M.N.; Rahman, M.M.; Billah, M.M.; Saha, D. Internet of Things (IoT): A review of its enabling technologies in healthcare applications, standards protocols, security and market opportunities. IEEE Internet Things J. 2021, 8, 10474–10498. [Google Scholar] [CrossRef]
- El-Rashidy, N.; El-Sappagh, S.; Islam, S.M.R.; M. El-Bakry, H.; Abdelrazek, S. Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics 2021, 11, 607. [Google Scholar] [CrossRef]
- Abdelmaboud, A.; Ahmed, A.I.A.; Abaker, M.; Eisa, T.A.E.; Albasheer, H.; Ghorashi, S.A.; Karim, F.K. Blockchain for IoT Applications: Taxonomy, Platforms, Recent Advances, Challenges and Future Research Directions. Electronics 2022, 11, 630. [Google Scholar] [CrossRef]
- Ali, Z.H.; Ali, H.A. Towards sustainable smart IoT applications architectural elements and design: Opportunities, challenges, and open directions. J. Supercomput. 2021, 77, 5668–5725. [Google Scholar] [CrossRef]
- Qadri, Y.A.; Nauman, A.; Zikria, Y.B.; Vasilakos, A.V.; Kim, S.W. The future of healthcare internet of things: A survey of emerging technologies. IEEE Commun. Surv. Tutor. 2020, 22, 1121–1167. [Google Scholar] [CrossRef]
- Goyal, S.; Sharma, N.; Bhushan, B.; Shankar, A.; Sagayam, M. Iot enabled technology in secured healthcare: Applications, challenges and future directions. In Cognitive Internet of Medical Things for Smart Healthcare; Springer: Berlin/Heidelberg, Germany, 2021; pp. 25–48. [Google Scholar]
- Ullah, A.; Azeem, M.; Ashraf, H.; Alaboudi, A.A.; Humayun, M.; Jhanjhi, N. Secure healthcare data aggregation and transmission in IoT—A survey. IEEE Access 2021, 9, 16849–16865. [Google Scholar] [CrossRef]
- Selvaraj, S.; Sundaravaradhan, S. Challenges and opportunities in IoT healthcare systems: A systematic review. SN Appl. Sci. 2020, 2, 1–8. [Google Scholar] [CrossRef]
- Aghdam, Z.N.; Rahmani, A.M.; Hosseinzadeh, M. The role of the Internet of Things in healthcare: Future trends and challenges. Comput. Methods Programs Biomed. 2021, 199, 105903. [Google Scholar] [CrossRef]
- Raykar, S.S.; Shet, V.N. Design of healthcare system using IoT enabled application. Mater. Today Proc. 2020, 23, 62–67. [Google Scholar] [CrossRef]
- Birje, M.N.; Hanji, S.S. Internet of things based distributed healthcare systems: A review. J. Data Inf. Manag. 2020, 2, 149–165. [Google Scholar] [CrossRef]
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 2020, 140, 100523. [Google Scholar] [CrossRef]
- Majedi, N.; Naeem, M.; Anpalagan, A. Telecommunication integration in e-healthcare: Technologies, applications and challenges. Trans. Emerg. Telecommun. Technol. 2016, 27, 775–789. [Google Scholar] [CrossRef]
- Kim, S.; Kim, S. User preference for an IoT healthcare application for lifestyle disease management. Telecommun. Policy 2018, 42, 304–314. [Google Scholar] [CrossRef]
- Javaid, M.; Khan, I.H. Internet of Things (IoT) enabled healthcare helps to take the challenges of COVID-19 Pandemic. J. Oral Biol. Craniofacial Res. 2021, 11, 209–214. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.M.; Bairagi, A.K.; Khan, M.A.-M.; Kee, S.-H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. https://doi.org/10.3390/healthcare10101993
Abdulmalek S, Nasir A, Jabbar WA, Almuhaya MAM, Bairagi AK, Khan MA-M, Kee S-H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare. 2022; 10(10):1993. https://doi.org/10.3390/healthcare10101993
Chicago/Turabian StyleAbdulmalek, Suliman, Abdul Nasir, Waheb A. Jabbar, Mukarram A. M. Almuhaya, Anupam Kumar Bairagi, Md. Al-Masrur Khan, and Seong-Hoon Kee. 2022. "IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review" Healthcare 10, no. 10: 1993. https://doi.org/10.3390/healthcare10101993
APA StyleAbdulmalek, S., Nasir, A., Jabbar, W. A., Almuhaya, M. A. M., Bairagi, A. K., Khan, M. A.-M., & Kee, S.-H. (2022). IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare, 10(10), 1993. https://doi.org/10.3390/healthcare10101993









