Basic Differences and Most Common Findings in Ultrasound Examinations of Musculoskeletal System in Children: A Narrative Literature Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. The Differences in Musculoskeletal US Examination in Children and Adults
3.1.1. The Differences between the Approach to Children and Adults: The Basic Requirements for the Musculoskeletal Ultrasound in Children
- SRI (Speckle Reduction Filter)—software reducing “speckle” noise in the image;
- SCI (Spatial Compounding Imaging), the so-called “cross imaging”;
- Edge Enhance—edge filters allowing to sharpen the boundaries between the tissues;
- THI (Tissue Harmonic Imaging)—harmonic imaging, which uses the second harmonic of the received signal to create an image, increasing the contrast resolution of received images;
- Inversion—harmonic imaging with inverted pulse. In addition to the main ultrasonic wave pulse, an impulse in the opposite phase is generated, which allows “natural” suppression of the reflected signal components related to the noise in the image. A much higher contrast resolution of the received images can be achieved;
- Single-Crystal—technology of probe construction that increases the frequency response, which in practice means it has a much higher sensitivity to a wider frequency range, and allows the probe to be used for both superficial and deep structures.
3.1.2. The Anatomical Causes of Differences in US Examination of the MSK System in Children and Adults
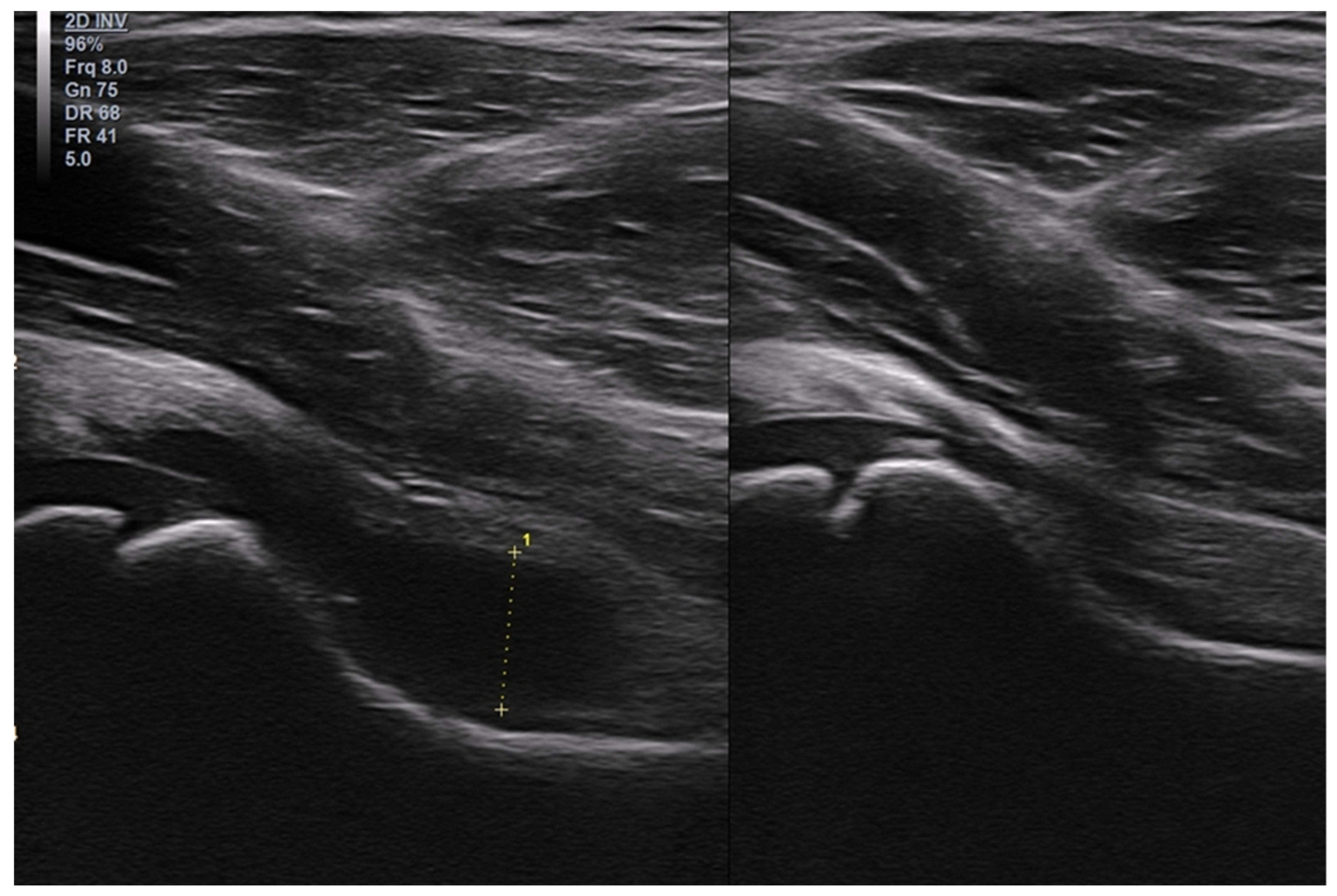
3.2. The Most Common Pathologies Encountered in the US Image in Children
3.2.1. Osteochondritis Dissecans
3.2.2. Osgood–Schlatter Disease
3.2.3. Ligament Injuries
3.2.4. Exfoliation of Growth Plates
3.2.5. Osteochondroma
3.2.6. Exudates and Inflammations Affecting Joints
3.2.7. Baker’s Cysts
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strakowski, J.A.; Visco, C.J. Diagnostic and therapeutic musculoskeletal ultrasound applications of the shoulder. Muscle Nerve 2019, 60, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Roth, J.; Jousse-Joulin, S.; Magni-Manzoni, S.; Rodriguez, A.; Tzaribachev, N.; Iagnocco, A.; Naredo, E.; D’Agostino, M.A.; Collado, P. Outcome Measures in Rheumatology Ultrasound Group Definitions of the Sonographic Features of Joints in Healthy Children. Arthritis Care Res. 2015, 67, 136–142. [Google Scholar] [CrossRef] [Green Version]
- Bleck, J.S.; Gebel, M.; Witt, B.; Schmitt, K.J.; Breitkopf, P.; Westhoff-Bleck, M.; Wagner, S.; Göke, M.; Caselitz, M.; Schneider, A.; et al. Sonography under Daylight Conditions. Ultraschall. Med. 1998, 19, 259–264. [Google Scholar] [CrossRef]
- Maurer, K. Musculoskeletal ultrasound in childhood. Eur. J. Radiol. 2014, 83, 1529–1537. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Harvey, N.; Javaid, K.; Hanson, M.; Dennison, E. Growth and bone development. Nestle Nutr. Workshop Ser. Pediatr. Program 2008, 61, 53–68. [Google Scholar] [CrossRef]
- Crowder, C.; Austin, D. Age ranges of epiphyseal fusion in the distal tibia and fibula of contemporary males and females. J. Forensic Sci. 2005, 50, 1001–1007. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; González-Morán, G.; Garay, E.G.; Moraleda, L. Developmental dysplasia of the hip: Update of management. EFORT Open Rev. 2019, 4, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Knipe, H.; Tatco, V. Ossification Centers of the Hip. Reference Article. Available online: https://radiopaedia.org/articles/24706 (accessed on 29 August 2022).
- Knipe, H.; Hacking, C. Ossification Centers of the Knee. Reference Article. Available online: https://radiopaedia.org/articles/24707 (accessed on 12 June 2022).
- Davies, A.M.; Johnson, K.; Whitehouse, R.W. Imaging of the Hip & Bony Pelvis: Techniques and applications. Med. Radiol. 2006, 7, 93. [Google Scholar]
- Pettersson, H.; Theander, G. Ossification of femoral head in infancy. I. Normal standards. Acta Radiol. 1979, 20, 170–179. [Google Scholar]
- Gaillard, F.; Weerakkody, Y. Elbow Ossification. Reference Article. Available online: https://radiopaedia.org/articles/1263 (accessed on 12 June 2022).
- Knipe, H.; Weerakkody, Y. Ossification Centers of the Pectoral Girdle. Reference Article. Available online: https://radiopaedia.org/articles/24673 (accessed on 12 June 2022).
- Vinagre, G.; Cruz, F.; Alkhelaifi, K.; D’Hooghe, P. Isolated meniscus injuries in skeletally immature children and adolescents: State of the art. J. ISAKOS, 2021; ahead of print. [Google Scholar] [CrossRef]
- Nguyen, J.C.; Lee, K.S.; Thapa, M.M.; Rosas, H.G. US Evaluation of Juvenile Idiopathic Arthritis and Osteoarticular Infection. Radiographics 2017, 37, 1181–1201. [Google Scholar] [CrossRef] [Green Version]
- Karmazyn, B. Ultrasound of pediatric musculoskeletal disease: From head to toe. Semin. Ultrasound CT MR 2011, 32, 142–150. [Google Scholar] [CrossRef]
- Ortiz-Neira, C.L.; Laffan, E.; Daneman, A.; Fong, K.; Roposch, A.; Ohlsson, A.; Jarrin, J.; Wang, C.; Wedge, J.; Doria, A.S. Colour Doppler ultrasound assessment of the normal neonatal hip. Can. Assoc. Radiol. J. 2009, 60, 79–87. [Google Scholar] [CrossRef] [Green Version]
- Grechenig, W.; Mayr, J.M.; Peicha, G.; Hammerl, R.; Schatz, B.; Grechenig, S. Sonoanatomy of the Achilles tendon insertion in children. J. Clin. Ultrasound 2004, 32, 338–343. [Google Scholar] [CrossRef]
- Kessler, J.I.; Nikizad, H.; Shea, K.G.; Jacobs, J.C., Jr.; Bebchuk, J.D.; Weiss, J.M. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am. J. Sports Med. 2014, 42, 320–326. [Google Scholar] [CrossRef]
- Chau, M.M.; Klimstra, M.A.; Wise, K.L.; Ellermann, J.M.; Tóth, F.; Carlson, C.S.; Nelson, B.J.; Tompkins, M.A. Osteochondritis Dissecans: Current Understanding of Epidemiology, Etiology, Management and Outcomes. J. Bone Jt. Surg. Am. 2021, 103, 1132–1151. [Google Scholar] [CrossRef]
- DeLee, J.C.; Drez, D., Jr.; Miller, M.D. DeLee & Drez’s Orthopaedic Sports Medicine Principles and Practice, 2nd ed.; Elsevier Science: Philadelphia, PA, USA, 2003. [Google Scholar]
- Dipaola, J.D.; Nelson, D.W.; Colville, M.R. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991, 7, 101. [Google Scholar] [CrossRef]
- Guhl, J.F. Arthroscopic treatment of osteochondritis dissecans. Clin. Orthop. Relat. Res. 1982, 65–74. [Google Scholar] [CrossRef]
- Albert, C.; Hergenroeder, M.D.; Brian, S.; Harvey, D.O. Osteochondritis Dissecans (OCD): Clinical Manifestations, Evaluation, and Diagnosis; UpToDate: Waltham, MA, USA, 2022. [Google Scholar]
- Nissen, C.W.; Albright, J.C.; Anderson, C.N.; Busch, M.T.; Carlson, C.; Carsen, S.; Chambers, H.G.; Edmonds, E.W.; Ellermann, J.M.; Ellis, H.B., Jr.; et al. Descriptive Epidemiology from the Research in Osteochondritis Dissecans of the Knee (ROCK) Prospective Cohort. Am. J. Sports Med. 2022, 50, 118–127. [Google Scholar] [CrossRef]
- Perumal, V.; Wall, E.; Babekir, N. Juvenile osteochondritis dissecans of the talus. J. Pediatr. Orthop. 2007, 27, 821–825. [Google Scholar] [CrossRef] [PubMed]
- Letts, M.; Davidson, D.; Ahmer, A. Osteochondritis dissecans of the talus in children. J. Pediatr. Orthop. 2003, 23, 617–625. [Google Scholar] [CrossRef]
- Ladenhauf, H.N.; Seitlinger, G.; Green, D.W. Osgood-Schlatter disease: A 2020 update of a common knee conditio in children. Curr. Opin. Pediatr. 2020, 32, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Launay, F. Sports-related overuse injuries in children. Orthop. Traumatol. Surg. Res. 2015, 101, S139–S147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mital, M.A.; Matza, R.A.; Cohen, J. The so-called unresolved Osgood-Schlatter lesion: A concept based on fifteen surgically treated lesions. J. Bone Jt. Surg. Am. 1980, 62, 732–739. [Google Scholar] [CrossRef] [PubMed]
- Ogden, J.A.; Southwick, W.O. Osgood-Schlatter’s disease and tibial tuberosity development. Clin. Orthop. Relat. Res. 1976, 116, 180–189. [Google Scholar]
- Hirano, A.; Fukubayashi, T.; Ishii, T.; Ochiai, N. Magnetic resonance imaging of Osgood-Schlatter disease: The course of the disease. Skeletal. Radiol. 2002, 31, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Gholve, P.A.; Scher, D.M.; Khakharia, S.; Widmann, R.F.; Green, D.W. Osgood Schlatter syndrome. Curr. Opin. Pediatr. 2007, 19, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Kujala, U.M.; Kvist, M.; Heinonen, O. Osgood-Schlatter’s disease in adolescent athletes. Retrospective study of incidence and duration. Am. J. Sports Med. 1985, 13, 236–241. [Google Scholar] [CrossRef]
- Willis, R.B. Sports medicine in the growing child. In Lovell and Winter’s Pediatric Orthopaedics, 6th ed.; Morrissey, R.T., Weinstein, S.L., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; p. 1384. [Google Scholar]
- Cassas, K.J.; Cassettari-Wayhs, A. Childhood and adolescent sports-related overuse injuries. Am. Fam. Physician 2006, 73, 1014–1022. [Google Scholar] [PubMed]
- MacDonald, J.; Rodenberg, R.; Sweeney, E. Acute Knee Injuries in Children and Adolescents: A Review. JAMA Pediatr. 2021, 175, 624–630. [Google Scholar] [CrossRef]
- Gage, B.E.; McIlvain, N.M.; Collins, C.L.; Fields, S.K.; Comstock, R.D. Epidemiology of 6.6 million knee injuries presenting to United States emergency departments from 1999 through 2008. Acad. Emerg. Med. 2012, 19, 378–385. [Google Scholar] [CrossRef]
- Ferry, T.; Bergström, U.; Hedström, E.M.; Lorentzon, R.; Zeisig, E. Epidemiology of acute knee injuries seen at the Emergency Department at Umeå University Hospital, Sweden, during 15 years. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1149–1155. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. 2016 consensus statement of the International Ankle Consortium: Prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1493–1495. [Google Scholar] [CrossRef] [PubMed]
- Gribble, P.A.; Bleakley, C.M.; Caulfield, B.M.; Docherty, C.L.; Fourchet, F.; Fong, D.T.P.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; McKeon, P.O.; et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br. J. Sports Med. 2016, 50, 1496–1505. [Google Scholar] [CrossRef] [Green Version]
- Doherty, C.; Delahunt, E.; Caulfield, B.; Hertel, J.; Ryan, J.; Bleakley, C. The incidence and prevalence of ankle sprain injury: A systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014, 44, 123–140. [Google Scholar] [CrossRef]
- Szczepaniak, J.; Ciszkowska-Łysoń, B.; Śmigielski, R.; Zdanowicz, U. Value of ultrasonography in assessment of recent injury of anterior talofibular ligament in children. J. Ultrason. 2015, 15, 259–266. [Google Scholar] [CrossRef]
- Peck, K.; Herrera-Soto, J. Slipped capital femoral epiphysis: What’s new? Orthop. Clin. N. Am. 2014, 45, 77–86. [Google Scholar] [CrossRef]
- Georgiadis, A.G.; Zaltz, I. Slipped capital femoral epiphysis: How to evaluate with a review and update of treatment. Pediatr. Clin. N. Am. 2014, 61, 1119–1135. [Google Scholar] [CrossRef]
- Belayneh, R.; Fourman, M.S.; Bhogal, S.; Weiss, K.R. Update on Osteosarcoma. Curr. Oncol. Rep. 2021, 23, 71. [Google Scholar] [CrossRef]
- Eaton, B.R.; Schwarz, R.; Vatner, R.; Yeh, B.; Claude, L.; Indelicato, D.J.; Laack, N. Ewing sarcoma. Pediatr. Blood Cancer 2021, 68 (Suppl. 2), e28355. [Google Scholar] [CrossRef]
- Wu, M.; Zheng, E.T.; Anderson, M.E.; Miller, P.E.; Spencer, S.A.; Heyworth, B.E. Surgical Treatment of Solitary Periarticular Osteochondromas About the Knee in Pediatric and Adolescent Patients: Complications and Functional Outcomes. J. Bone Jt. Surg. Am. 2021, 103, 1276–1283. [Google Scholar] [CrossRef]
- Bernd, L.; Niethard, F.U.; Graf, J.; Kaps, H.P. Die Flüchtige Hüftgelenksentzündung (Coxitis fugax) [Transient hip joint inflammation (coxitis fugax)]. Z. Orthop. Ihre Grenzgeb. 1992, 130, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Sudoł-Szopińska, I.; Grochowska, E.; Gietka, P.; Płaza, M.; Pracoń, G.; Saied, F.; Walentowska-Janowicz, M. Imaging of juvenile idiopathic arthritis. Part II: Ultrasonography and MRI. J. Ultrason. 2016, 16, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Sudoł-Szopińska, I.; Płaza, M.; Pracoń, G. Selected issues in diagnostic imaging of spondyloarthritides: Psoriatic arthritis and juvenile spondyloarthritis. Reumatologia 2016, 54, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Windschall, D.; Trauzeddel, R.; Haller, M.; Krumrey-Langkammerer, M.; Nimtz-Talaska, A.; Berendes, R.; Ganser, G.; Nirschl, C.; Schoof, P.; Trauzeddel, R.F.; et al. Pediatric musculoskeletal ultrasound: Age- and sex-related normal B-mode findings of the knee. Rheumatol. Int. 2016, 36, 1569–1577. [Google Scholar] [CrossRef]
- Brunner, E.; Ting, T.; Vega-Fernandez, P. Musculoskeletal ultrasound in children: Current state and future directions. Eur. J. Rheumatol. 2020, 7 (Suppl. S1), S28–S37. [Google Scholar] [CrossRef]
- Alessi, S.; Depaoli, R.; Canepari, M.; Bartolucci, F.; Zacchino, M.; Draghi, F. Baker’s cyst in pediatric patients: Ultrasonographic characteristics. J. Ultrasound 2012, 15, 76–81. [Google Scholar] [CrossRef]



















| Assesed Structure | In Children | In Adults |
|---|---|---|
| Joint space | A possibility of the physiological presence of a small amount of fluid or small synovial folds | A possibility of physiologically moderately increased amount of fluid after physical activity or in the evening |
| Articular cartilage | Relatively thick layer of hyaline cartilage (the non-ossified part of the epiphysis), the possibility of existence of blood vessels in the cartilaginous epiphysis at a young age | A thin layer of articular cartilage, lack of vascularity |
| Growth cartilage | Present. The possibility of the presence of blood vessels in the area of growth cartilage. In adolescents—unevenness at the site of growth plates. | Not present. Unevenness on the bone surface is usually an indication of pathology. |
| Muscle and tendon attachments | Attach to non-ossified hypoechoic bone parts | Attach to calcified bones |
| Assessed Structures | Potential Pathologies |
|---|---|
| Subcutaneous tissue | Edema, postraumatic “hematomas”, discontinuity (Morel–Lavallée lesion)—rare in children, and tumors (lipomas, fibromas, and neurofibromas, such asVon Recklinghausen’s disease) |
| Fascia | Discontinuity, muscle hernias—usually coexisting with post-operative or traumatic scars, and desmoid fibromatosis |
| Muscles | Post-traumatic changes, breaks in continuity, “hematomas”, and tumors (a lesion with the features of a lipoma is benign if it occurs in the subcutaneous tissue; if it is visible within the muscles, at the depth of the fascia, it is likely to be a malignant (e.g., liposarcoma), even if it has well-defined edges and does not show features of hypervascularity) |
| Tendons | Tendon injuries, enthesopathies, enthesitis, tendinopathies, tenosynovitis, tendinitis secondary to tenosynovitis, and stenosing tenosynovitis (most frequent in children is the congenital trigger thumb) |
| Bone surface | Post-traumatic changes, features of fractures, local thickening of the periosteum, increased vascularization of the periosteum, and the presence of periosteal reactions, which may indicate the presence of osteomyelitis or neoplasms |
| Nerves | Pathologies of the peripheral nervous system in children are rare, compression syndromes are practically absent, and tumors, which include rare neuromas and fibrolipomatus hamartoma of median nerve with coexisting macrodactyly (usually digit III) |
| Joint cavity and recesses | Effusions, synovial thickening, synovial hypervascularity, increased echogenicity of the synovial membrane, indicating chronic inflammation or fibrosis, and presence of loose bodies |
| Intra- and extra-articular fat tissue | Assessment of inflammation: increased echogenicity and increased vascularization |
| Hyaline cartilage of epiphyses, subchondral layer | Signs of damage (chondromalacia, erosions, cysts, and scars after injuries) |
| Growth plate area | Assessment in terms of post-traumatic lesions: features of exfoliation, erosions, and neoplasms, commonly found at the border of epiphysis and metaphysis |
| Ligaments | Assessment for post-traumatic changes |
| Bursae | Effusions, synovial thickening, hypervascularity, and loose bodies |
| Structures characteristic of a given joint or area (e.g., labrum in the shoulder or hip joint, menisci in the knee joint, etc.) | Limited diagnostic possibilities. The advantage of an MRI is unquestionable, but it is worth to at least make an initial diagnosis and recommend further examinations. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poboży, T.; Konarski, W.; Piotrowska-Lis, K.; Domańska, J.; Poboży, K.; Kielar, M. Basic Differences and Most Common Findings in Ultrasound Examinations of Musculoskeletal System in Children: A Narrative Literature Review. Healthcare 2022, 10, 2010. https://doi.org/10.3390/healthcare10102010
Poboży T, Konarski W, Piotrowska-Lis K, Domańska J, Poboży K, Kielar M. Basic Differences and Most Common Findings in Ultrasound Examinations of Musculoskeletal System in Children: A Narrative Literature Review. Healthcare. 2022; 10(10):2010. https://doi.org/10.3390/healthcare10102010
Chicago/Turabian StylePoboży, Tomasz, Wojciech Konarski, Karolina Piotrowska-Lis, Julia Domańska, Kamil Poboży, and Maciej Kielar. 2022. "Basic Differences and Most Common Findings in Ultrasound Examinations of Musculoskeletal System in Children: A Narrative Literature Review" Healthcare 10, no. 10: 2010. https://doi.org/10.3390/healthcare10102010
APA StylePoboży, T., Konarski, W., Piotrowska-Lis, K., Domańska, J., Poboży, K., & Kielar, M. (2022). Basic Differences and Most Common Findings in Ultrasound Examinations of Musculoskeletal System in Children: A Narrative Literature Review. Healthcare, 10(10), 2010. https://doi.org/10.3390/healthcare10102010





