Abstract
Medical examination plays an essential role in most medical treatment processes, and thus, the quality of service relevant to medical examination has great impact on patient satisfaction. The targeted hospital has long been faced with the problem that patient satisfaction of its medical examination department is below average. An assessment model, integrating 4M1E, ITLV, GRA, DEMATEL and FMEA, was developed in this study to identify the root causes of important service failures across medical examination processes, where (1) a cause-and-effect diagram was enhanced with 4M1E, identifying the list of failure modes relevant to service quality over the medical examination process with the 4M1E analysis framework, (2) FMEA experts were enabled to report their assessment results in their preferred ways by using the ITLV scheme, (3) causes of failure to failure modes with was figured out with DEMATEL, and (4) the evaluation results were improved by integrating GRA. Experimental results obtained by the proposed approach are compared with several benchmarks, and it was observed that (1) the results obtained by the proposed model are more suitable when FMEA experts prefer using different assessment languages versus other approaches; (2) the proposed model can figure out the key root causes according to their impact on overall failure modes.
1. Introduction
Medical examination plays an essential part in the majority of medical treatment processes, and thus, the quality of service relevant to medical examination processes has great impact on patient satisfaction. Shanghai Pulmonary Hospital, a medium-size specialized hospital located in Shanghai, China, has long been faced with the problem that patient satisfaction of its medical examination department is below average, according to patient satisfaction reports of this hospital. Considering that more and more hospitals have regarded patient satisfaction as the most important indicator measuring service quality in recent years [1], it is essential to reveal the key factors resulting in nonsatisfaction of patients and to give valuable suggestions for improving service quality for the targeted medical examination department.
According to the literature, it was observed that there are few research studies on improving the service quality of medical examination, and most studies focus on either specific problems or certain medical examination activities such as the performance of C-arm X-ray machines, service assessments of radiographers’ experiences relevant to patient safety incidents, etc. [1,2,3,4,5]. However, few studies assess the service quality relevant to medical examination from the perspective of the entire process, i.e., from the time the patient makes an appointment for examination to receiving the final examination report.
When the literature review was extended to include studies concerning service quality improvement for organizations other than the medical examination department, it was observed that many hybrid assessment models have been developed to draw on each other’s strengths. For example, Raziei et al. (2018) combined SERVQUAL with group decision making and QFD [6], Serkan and Semih (2019) integrated SERVQUAL and QFD with FMEA [7], and Tuzkaya et al. (2019) combined IVIF and PROMETHEE to overcome service quality problems from the perspectives of patients [8]. The ITLV scheme (2-tuple linguistic variables) has been successfully combined by some researchers, such as Li and He (2021), with assessment models to reduce both the uncertainty of evaluation information and the diversity of evaluation results [9].
Furthermore, it was observed that fuzzy techniques are widely applied in service quality assessment to deal with uncertainties. For instance, Liu et al. (2019) enhanced the performance of a fuzzy multi-attribute decision-making model by using grey relational analysis (GRA) when evaluating hospital service performance [10]. Yucesan and Gul (2020) combined Pythagorean FAHP and Pythagorean fuzzy technique to provide an accurate decision-making process for evaluating hospital service quality [11]. Alkafaji and Al-Shamery (2020) improved a service quality evaluation model by using fuzzy inference that can assess the quality of service in a similar way to the human experts of healthcare [12]. Akram et al. (2022) proposed a decision-making approach retaining the fascinating traits of the conventional VIKOR method in the context of the enrich multidimensional complex Fermatean fuzzy N-soft set [13]. Akram et al. (2022) developed a structure by the fusion of Fermatean fuzzy sets and linguistic term sets to deal with decision-making problems involving qualitative information [14]. Yüksel and Dinçer (2022) utilized hesitant 2-tuple interval-valued Pythagorean fuzzy DEMATEL to enhance the performance of the evaluation model [15].
Among the existing approaches, observed in the literature, developed for service quality improvement, it can be observed that FMEA (failure mode and effect analysis) and its variants have been widely used. A further literature review showed that FMEA and its variants can help prevent possible failure during service delivery in various fields from the perspectives of the entire process. For instance, Najafpour et al. (2017) applied FMEA to improve the efficiency of the blood transfusion process in a teaching general hospital [16]. Sayyadi Tooranloo et al. (2018) utilized FMEA to evaluate knowledge management failure factors in an intuitionistic fuzzy environment [17]. Mete (2019) applied a variant of FMEA to assess occupational risks in a natural gas pipeline construction project [18]. Lo et al. (2020) applied FMEA to identify critical failure modes of individual equipment components or processes to improve the development of plans [19]. Zhou et al. (2021) developed a FMEA-based approach to facilitate risk analysis of product design under uncertainty [20]. Although the traditional FMEA model suffers from several drawbacks when assessing the risk prioritization of potential failure modes, many efforts have been made to enhance the performance of the FMEA model in service quality evaluation so that many enhanced FMEA models can be successfully applied in various field for service quality improvement [21,22,23,24,25,26].
Encouraged by the success of FMEA models, this study aims at developing an advanced FMEA model for improving the service quality of medical examination in the targeted hospital concerning patient satisfaction, from the perspective of the entire medical examination process, where the following approaches have been integrated with FMEA to improve the FMEA assessment results: (1) The cause-and-effect diagram enhanced by 4M1E (man, machine, material, method and environment) structure was applied to systematically identify both the list of potential failure modes (FMs) and that of failure causes (CFs). (2) The ITLV (2-tuple linguistic variables), a multi-grained language scheme, was utilized to improve the collection of assessment opinions from FMEA experts. (3) DEMATEL (decision-making trial and evaluation laboratory) was applied to reveal the relationships between CFs and FMs. (4) The GRA (grey relation analysis) method was adopted to address the loss and uncertainty of decision makers’ judgements.
2. Methodology
2.1. General Procedure of the Proposed Assessment Model
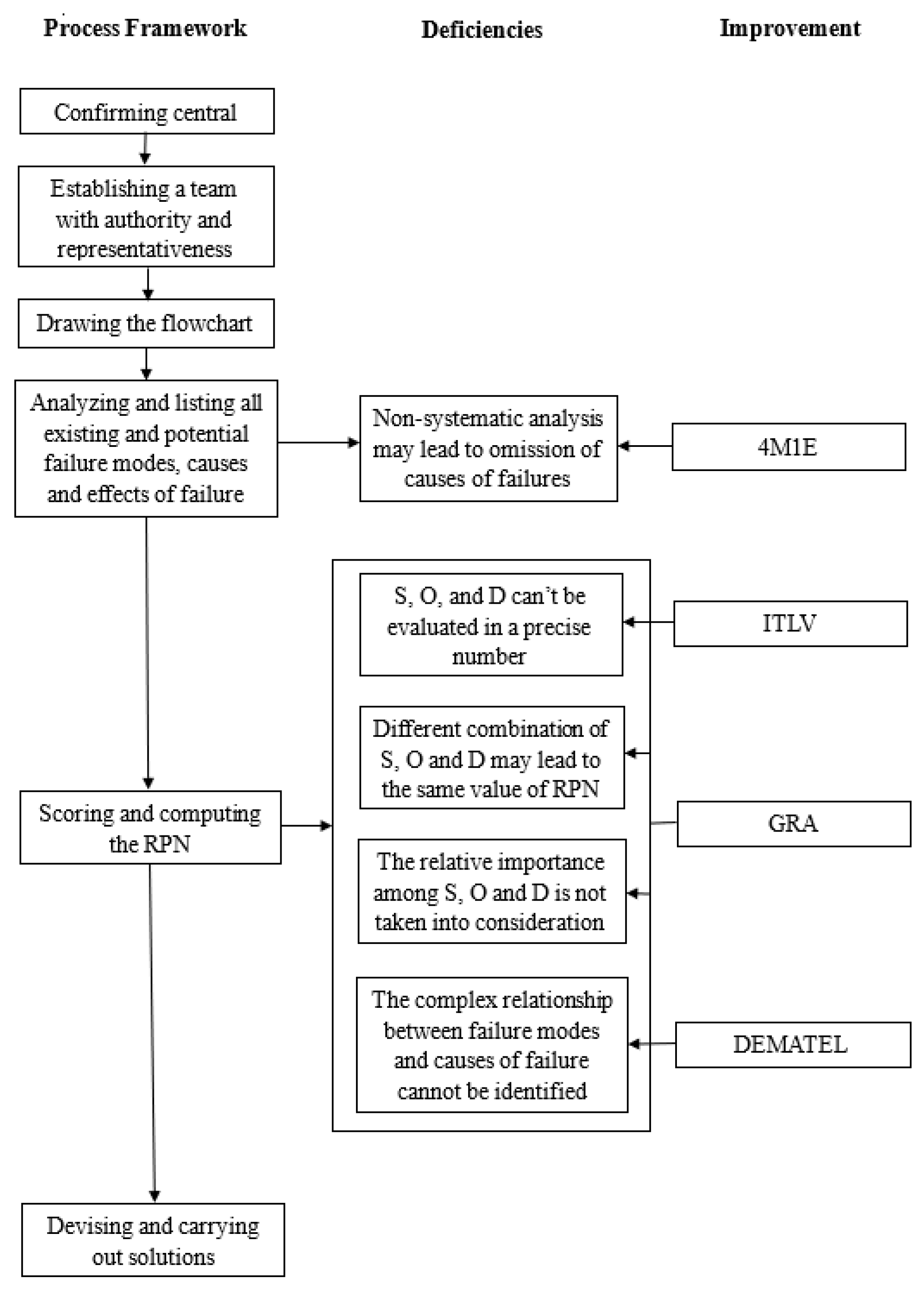
The general procedure of the FMEA model, an advanced service quality assessment model developed in this study, is as follows:
Step 1: Confirming central theme
In this study, the FMEA model is developed to identify potential risks involving the quality of services relevant to the medical examination process in the targeted hospital.
Step 2: Establishing a team with authority and representativeness
Five professionals, including two technicians, two nurses and one report physician, who have been responsible for various job positions across the medical examination process in the targeted hospital over one year, are invited as FMEA experts.
Step 3: Drawing the flowchart
The list of activities involved in the examination process are identified based on full discussions with the invited FMEA experts, and the flowchart of process is confirmed by those FMEA experts as well.
Step 4: Identifying the list of failure modes, failure causes and effects of failure
After full discussions with the expert group, we identify not only the failure modes and their possible effect, but also failure causes with the cause-and-effect diagram enhanced by the 4M1E structure.
Step 5: Scoring and computing the RPN
First, the ITLV (interval 2-tuple linguistic variables) is applied to integrate the evaluation data collected from FMEA experts with multi-grained language.
Then, GRA is used to ranking FMs (failure modes) according to their RPNs.
Afterward, DEMATEL is applied to identify the root causes for each failure mode.
Step 6: Devising and carrying out solutions
Based on the results obtained in Step 5, suggestions are given to improve the service quality across the medical examination process in the targeted hospital.
For better understanding, the contribution of the hybridization mechanism to improve the performance of traditional FMEA is depicted in Figure 1, and details about how each component works are given in the rest of this section.
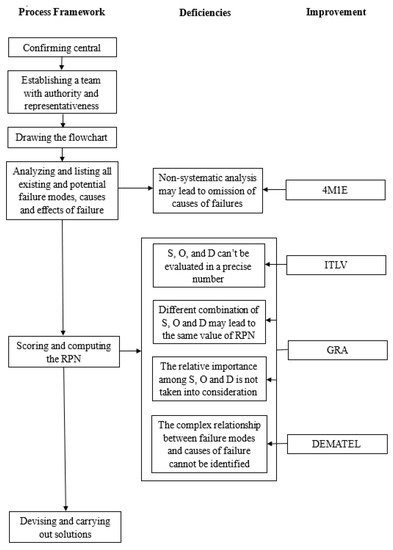
Figure 1.
Comparison between the proposed FMEA and traditional one.
2.2. Linguistic Variables
2.2.1. 2-Tuple Linguistic Variables
2-tuple linguistic variables were firstly identified by Herrera and Martinez based on the concept of symbol translation [1]. In this study, applied is the generalized 2-tuple linguistic variables model raised by Chen and Tai in 2005 based on the concept of 2-tuple linguistic variables to deal with and compare linguistic variables from linguistic evaluation sets with different granularity [27]. Here below are some definitions relevant to 2-tuple linguistic variables.
Definition 1.
Let be a linguistic term set and be a value representing the result of standardization. Then, the generalized translation function used to obtain the 2-tuple linguistic variable equivalent to can be defined as follows [1]:
- (a)
- round means rounding off operation;
- (b)
- means normal multiplication;
- (c)
- is the closet linguistic evaluation to ;
- (d)
- is the value of the symbolic translation depending on g;
- (e)
- is linked with the number of linguistic terms in S. For example, there are 5 linguistic terms in S; then, and
Definition 2.
Let be a linguistic term set and be a 2-tuple. The function that can translate a 2-tuple linguistic variable to its equivalent numerical value , which can be used to compare different multi-granularity linguistic terms, can be defined as follows:
Definition 3.
Let and be two 2-tuples, and define the following rules:
- If , then ;
- If , then
- (1)
- If , then ;
- (2)
- If , then ;
- (3)
- If , then .
In the operation of 2-tuple linguistic variables, function and function ensure no information loss during translation.
Definition 4.
Let be a 2-tuple set and be their associated weights, with , . The 2-tuple weighted average (TWA) is defined as
2.2.2. Interval 2-Tuple Linguistic Variables (ITLV)
Definition 5.
Let be a linguistic term set. An interval 2-tuple linguistic variable is composed of two 2-tuples, denoted by , with and . and represent the linguistic label of the predefined linguistic term set S and symbolic translation.
Interval 2-tuple linguistic variable has the same meaning with (, ) and is derived by the following function:
On the contrary, there always exists function , which can convert into (, ). Function is defined as follows:
when and , the interval 2-tuple linguistic variable can be simplified as a 2-tuple one.
Definition 6.
Let be an interval 2-tuple set, and W = be their associated weights, with , . Then, the interval 2-tuple weighted average (ITWA) is defined as
Definition 7.
Let and be two interval 2-tuples, then the normalized Euclidean distance between and is defined as following:
2.3. Grey Relation Analysis (GRA)
Grey theory was proposed in 1982 and is widely used in situations with multiple input, imperfection and uncertain information, especially in [28]. Grey theory is composed of 6 main research methods, and GRA is one of the most important of them.
Supposing that is a grey relational factor set, represents the reference sequence and , , represents the comparative sequence. and contain n elements, indicated as , , , .
and are the kth elements of reference and comparative sequence, and their grey relation coefficient can be calculated through the following equation:
ξ is the distinguishing coefficient, . is applied.
The grey relational degree between and is indicated by the following equation:
2.4. Decision-Making Trial and Evaluation Laboratory (DEMATEL)
DEMATEL was proposed by the Battelle Memorial Institute of the Geneva Research Center to resolve complex social issues through setting up a matrix to compute the direct and indirect relationships between elements [28].
DEMATEL can be divided into 5 steps as follows.
Step 1: List and define the factors in a complex system, and then, design a form to demonstrate their causal relationship.
Step 2: Establish an initial direct-relation matrix X. Value in the matrix represents the incidence between factors, obtained by pairwise comparisons in terms of influences and directions. is denoted as the degree to which factor i affects factor j.
Step 3: Normalize the initial direct-relation matrix X. The normalized direct-relation matrix (N) can be obtained by the following equation:
Step 4: Calculate the total relation matrix (T).
Step 5: Calculate the sum of every row and column in matrix T. Let be sum of the row and be sum of the column. and contain the direct and indirect relationships among factors.
2.5. GRA-DEMATEL-Based FMEA (GD-FMEA Method)
In this subsection, the GD-FMEA method is combined with the interval 2-tuple linguistic variables, where GRA and DEMATEL will be demonstrated.
Supposing that (a) an expert team is composed of l expert , and is their associated weights, in which , and ; (b), there are m causes of failure with n risk factors . Weights represent the importance of each expert when they evaluate the risk. Every expert can use a different linguistic term set () to evaluate CFs. Let be the linguistic evaluation matrix of the kth expert, where is the linguistic assessment provided by on the assessment of , with respect to . Let be the linguistic weight of risk factor given by to reflect its relative importance in the determination of risk priorities of causes of failure and failure modes. Based on the previously mentioned assumptions, the GD-FMEA method can be divided into the following steps:
Step 1: Establish a team with authority and representativeness, and then, list flowchart, failure modes, causes and effect of failure.
Step 2: Experts use different linguistic term sets to evaluate the risk factors and CFs; then, convert the linguistic decision matrix into an interval 2-tuple linguistic decision matrix , where , and .
Step 3: Aggregate the experts’ opinions to construct a collective interval 2-tuple linguistic decision matrix and obtain the aggregated 2-tuple linguistic weight of each risk factor , where
Step 4: Calculate the weight of risk factors (S, O, D)
Based on the aggregated weights of risk factors , the normalized risk factor weights can be obtained as follows:
Step 5: This step is related to GRA; thus, it can be subdivided into four steps:
- (1)
- Determine the reference sequence
- (2)
- Calculate the distances (differences) between the comparative sequences and the reference one, and establish the distance matrix
- (3)
- Calculate the grey relational coefficientThe grey relational coefficient represents how close is to . The larger the grey relational coefficient is, the closer and are:where , , , the distinguishing coefficient . is applied.
- (4)
- Estimate the grey relational degree
Step 6: Construct the initial relation matrix Y based on the result of Step 5.
Step 7: Normalize matrix Y to obtain the normalized relation matrix H. This step can be subdivided into two steps.
- (1)
- Calculate the sum of every row and column and use Equation (12) to obtain the reciprocal of the maximum of summed columns and rows.
- (2)
- Use Equation (13) to obtain the normalized relation matrix H.
Step 8: Calculate the direct and indirect relative severity matrix T.
Use Equation (14) to obtain the direct and indirect severity matrix T.
Step 9: Calculate the value of (R + C) and (R − C) based on Equation (15) and Equation (16).
(R + C) represents the total relationships between the cause and effect of specific criteria.
(R − C) represents influence, the differences between the cause and effect of specific criteria [29].
3. Case Study
In this section, it will be demonstrated how the GD-FMEA is applied to derive the root causes of failures resulting in poor service quality across the medical examination process in the targeted hospital located in Shanghai, China, and the steps are as follows.
Step 1: Define the list of failure modes (FMs) and corresponding causes of failure (CFs).
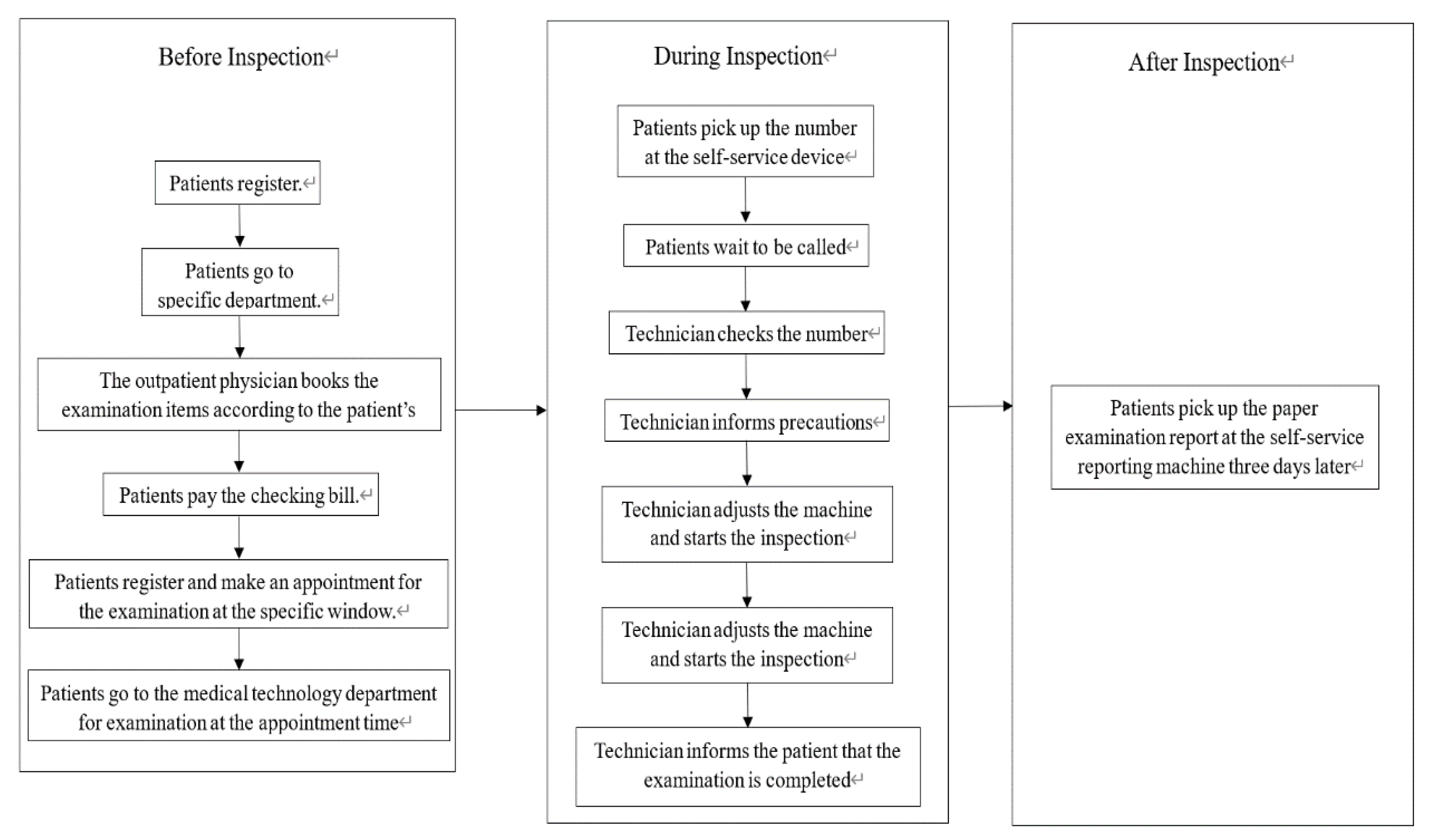
As shown in Figure 2, the process relevant to a medical examination in the targeted hospital consists of three stages, where the pre-inspection process starts from the registration of the patient until the arrival of the patient at the medical technology department at the appointment time; the per-inspection process consists of all the relevant activities carried out during the inspection; and the post-inspection process refers to obtaining the examination report after the inspection.
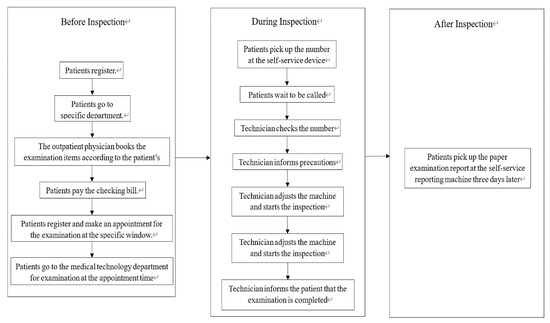
Figure 2.
The flowchart of inspection.
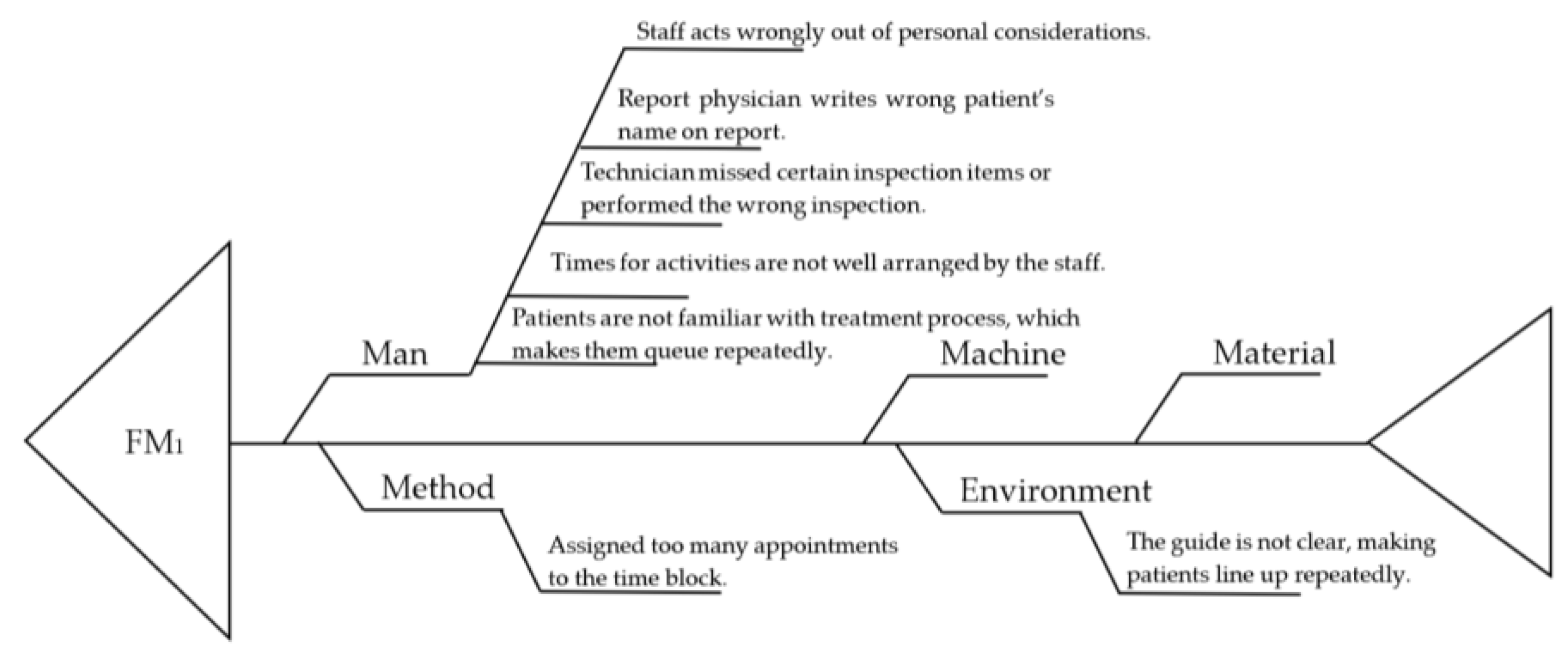
Based on literature review and after full discussion with the FMEA experts, the list of FMs defined in this study is constructed as shown in Table 1, where the corresponding CFs are identified with the cause-and-effect diagram enhanced by the 4M1E mechanism, as shown Figure 3, for FM1, as an example.

Table 1.
List of FMs across the medical examination process in the targeted hospital.
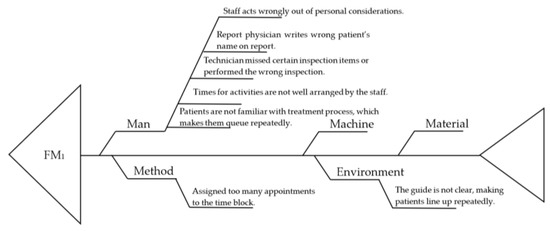
Figure 3.
Cause-and-effect diagram enhanced by 4M1E scheme for identifying root causes of failure relevant to FM1.
Step 2: Collect individual assessment results from FMEA experts.
To ensure the quality of assessment data, the FMEA expert team is composed of five experts, called decision makers (DMs) hereafter, who are senior professionals invited from the medical technology department in the targeted hospital, including two technicians responsible for medical examination operations, two nurses for on-site services at the targeted medical examination department, and one report physician. Considering the job responsibilities of these experts can be regarded as having equally important impact on the satisfaction of the patient partaking in the medical examination; their respective weights are set the same, i.e., 0.2 for each.
Furthermore, when collecting individual assessment data from the FMEA team, three linguistic term sets, whose structures are shown in Table 2, are provided in the questionnaires to enable the experts to fill in the questionnaires using their favorite rating system.

Table 2.
Three linguistic term sets applied in this study (EL: Extremely Low; VL: Very Low; ML: Moderately Low; M: Moderate; MH: Moderately High; H: High; VH: Very High; EH: Extremely High).
According to the questionnaires collected from the FMEA experts, noted as DM1 to DM5, it was observed that DM1 preferred set C, DM4 selected set B, and the other three experts, i.e., DM2, DM3 and DM5, used set A.
As for the collection of experts’ opinions on the importance of risk factors, we applied a five-granularity linguistic term set D = {d0 = very unimportant (VU), d1 = unimportant (U), d2 = medium(M), d3 = important (I), d4 = very important (VI)}.
Since data collected from FMEA experts are multi-linguistic, they are firstly converted uniformly into interval 2-tuple linguistic variables. Table 3, Table 4 and Table 5 show the 2-tuple linguistic variables corresponding to Severity (S), Occurrence (O), Detection (D).

Table 3.
Interval 2-tuple linguistic variables for Severity (S).

Table 4.
Interval 2-tuple linguistic variables for Occurrence (O).

Table 5.
Interval 2-tuple linguistic variables for Detection (D).
Interval 2-tuple linguistic variables for the importance of risk factors are shown in Table 6.

Table 6.
Interval 2-tuple linguistic variables for the importance of risk factors.
Step 3: Construct an aggregated interval 2-tuple linguistic decision matrix.
Use Equation (17) to construct the aggregated interval 2-tuple linguistic decision matrix , and use Equation (18) to obtain the aggregated 2-tuple linguistic weight of each risk factor , as shown in Table 7.

Table 7.
Interval 2-tuple linguistic decision matrix .
Step 4: Normalize the weights of risk factors.
Use Equation (19) to normalize the weights of risk factors, as shown in the last line of Table 7.
Step 5: Set reference sequence.
Use Equation (20) to determine the following reference sequence.
Step 6: Establish distance matrix.
Use Equation (21) to calculate the distances (differences) between the comparative sequences and the reference one, and then, establish the distance matrix , as shown in Table 8.

Table 8.
The distance matrix for pairs of FMs and CFs.
Step 7: Calculate grey relational coefficients.
Determine the grey relational coefficient by using Equation (22), of which the results are shown in Table 9.

Table 9.
The grey relational coefficient for pairs of FMs and CFs.
Step 8: Estimate grey relational degrees.
Determine the grey relational degree by using Equation (23), of which the results are shown in Table 10.

Table 10.
The grey relational degree of FM–CF pairs.
Step 9: Construct initial relation matrix among FMs and CFs.
Use the grey relational degrees obtained in Step 8 to construct the initial relation matrix Y among FMs and CFs, as shown in Table 11.

Table 11.
The initial relation matrix Y.
Step 10: Construct direct and indirect relation matrix among FMs and CFs.
Use Equation (13) and Equation (14) to obtain the direct and indirect relation matrix T among FMs and CFs, as shown in Table 12.

Table 12.
The direct and indirect relation matrix T among FMs and CFs.
Step 11: Calculate the direct and indirect relative relationships.
Use Equation (15) and Equation (16) to calculate R for CFs and C for FMs, as shown in Table 13 and Table 14, respectively.

Table 13.
Values of R for CFs.

Table 14.
Values of C for FMs.
Step 12: Rank the priority of FMs and CFs.
Since the worst case is set as the reference sequence, it is reasonable to conclude that the bigger the value of R, the more significant a CF is, and similarly, the bigger C is, the higher priority FM must have. According to the results shown in Table 13, it can be observed that CF22, CF16, CF4, CF3, and CF5, whose values are close to 1, are considered as significant. With the results shown in Table 14, FM5, FM1 and FM7 are ranked as the top three failures modes resulting in poor service quality at the targeted medical examination department.
Considering that some failure causes may have impact on more than one failure mode, it is also interesting to further analyze the overall impact of causes to those three critical failure modes: FM5, FM1 and FM7. Considering the meanings of R and C, the priority of CFs relevant to these three critical FMs is ranked according to the descending order of (R + C), such that the bigger the value of (R + C) obtained, the higher priority a CF has, and more attention must be paid to improve the activities relevant to this CF. As shown in Table 15, it can be observed that the top five CFs have a firm relationship with the top three FMs and the top two CFs have great impact on FM5 and FM7.

Table 15.
Priority of CFs relevant to the top three FMs.
Furthermore, a comparison among the proposed GD-FMEA, an enhanced VIKOR (CFFS-VIKOR) [13], and a GRA-FMEA (G-FMEA) [21] is conducted to evaluate the performance of GD-FMEA. The results obtained by CFFS-VIKOR contain two parts, where CFFS-VIKOR-A corresponds to the assessment data collected with the five-granularity assessment language (Set A) and CFFS-VIKOR-C corresponds to the nine-granularity assessment language (set C). The results regarding the priorities of FMs and critical FM-related CFs are shown in Table 16 and Table 17, respectively.

Table 16.
Comparison regarding the priorities of FMs.

Table 17.
Comparison regarding the priority of CFs related to FM1, FM4, FM5, FM6 and FM7, which are ranked as the top three by at least one of the compared approaches.
4. Discussions
According to the results shown in Table 13, the FMs whose evaluation results (C) are significantly higher than the others are FM5 (C = 5.409, machines go wrong) and FM1 (C = 3.423, waiting too long in the queue for examination), where the former is related firmly with machine breakdown and the latter reveals the patients’ complaints about long waiting in the queue for examination. As for CFs, it can be observed that CF22 (software system of self-service reporting machine does not work), CF16 (patients do not use the self-service reporting machines according to the regulations), CF4 (report physician writes wrong patient’s name on report), CF3 (technicians missed certain inspection items or performed the wrong inspection) and CF5 (staff acts wrongly out of personal considerations) are ranked as the top five. Furthermore, their evaluation results (R) are quite close to 1, indicating that those causes have great impact on poor quality of relevant services in the targeted services. Further analysis of the relationship between these top FMs and CFs shows that the top two causes of failures (CF22 and CF16) firmly relate with FM5, which indicates that more and more patients derive the inspection report from the self-service reporting machine. Thus, not only the failures of the machine’s operating system but also improper operations of the machine may prevent the patients from successfully obtaining their inspection report, resulting in complaints from patients, and the hospital should not only ensure the normal status of the reporting machines but should also improve on-site assistance service for patients to derive inspection reports from the reporting machines. On the other hand, regarding the analysis of the significant causes related with FM1, i.e., CF3, CF4 and CF5, it can be concluded that all of them are human-related failures, although none of them relate to professionals, such as technicians and report physicians, but rather to nurses responsible for on-site reception and assistance services. Furthermore, it can be concluded that these three CFs are related to a lack of responsibility. Therefore, the suggestion for the targeted hospital is to organize a training program to improve the professionalism and responsibility of the staff, especially the examination technicians and the reporting physicians.
According to the comparison regarding the priority of FMs as shown in Table 16, it can be observed that the results of GD-FMEA and G-FMEA are the same, and the top two FMs identified by these two approaches are the same as the CFFS-VIKOR model. As for the CFFS-VIKOR, we observed that the results are not consistent when different assessment language sets are applied. Furthermore, it can be observed that regarding the results shown in Table 17, the results obtained by GD-FMEA are consistent with those obtained by G-FMEA and CFFS-VIKOR-A for the top four CFs, and the same results can be obtained through G-FMEA for the top six CFs. It is reasonable to conclude that the proposed assessment model is much more stable than the approaches using mono-assessment language set and is consistent with the other assessment approaches.
5. Conclusions
In this study, an assessment model, integrating 4M1E, ITLV, GRA, DEMATEL and FMEA, was developed to identify the root causes of important service failures across medical examination processes in a medium-sized specialty hospital, where (1) the cause-and-effect diagram was enhanced with 4M1E to identify the list of failure modes relevant to service quality over the medical examination process with 4M1E analysis framework, (2) FMEA experts were enabled to report their assessment results in their preferred ways by using ITLV scheme, (3) the causes of failure to failure modes were figured out with DEMATEL, and (4) the evaluation results were improved by integrating GRA. The case study was conducted in the targeted specialized hospital, which has long been faced with the problem that patient satisfaction of its medical examination department is below average. A comparison among the proposed GD-FMEA, CFFS-VIKOR and G-FMEA models was conducted to evaluate the performance of GD-FMEA. According to the comparison, the results obtained by GD-FMEA are consistent with those obtained by G-FMEA and CFFS-VIKOR-A for the top four CFs, and the same results were obtained as G-FMEA for the top six CFs. It is reasonable to conclude that the proposed assessment model was much more stable than approaches using mono-assessment language sets and was consistent with the other assessment approaches. CF22 (software system of self-service reporting machine does not work), CF16 (patients do not use the self-service reporting machines according to the regulations), CF4 (report physician writes wrong patient’s name on report), CF3 (technicians missed certain inspection items or performed the wrong inspection) and CF5 (staff acts wrongly out of personal considerations) were ranked as the top five. Therefore, several suggestions are presented as follows:
- Strengthen the daily maintenance of inspection machines and self-service machines, including software and hardware;
- Train volunteers to operate the self-service machines and assign them to instruct patients at the self-service machines;
- Establish a two-person inspection mechanism for reports to reduce the occurrence of errors.
Author Contributions
Conceptualization, H.F.; methodology, H.F., Y.Z. and S.S.; software, Y.Z. and Y.K.; validation, Y.Z., S.S. and X.X.; formal analysis, H.F., Y.Z. and S.S.; investigation, Y.Z., S.S. and Y.K.; resources, S.S. and X.X.; data curation, Y.Z. and S.S.; writing—original draft preparation, Y.Z.; writing—review and editing, H.F., S.S. and Y.K.; project administration, H.F.; funding acquisition, S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Shanghai Pulmonary Hospital, grant number FKZR2125. And the APC was funded by Shanghai Pulmonary Hospital.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Liu, H.C.; Li, P.; You, J.X.; Chen, Y.Z. A Novel Approach for FMEA: Combination of Interval 2-Tuple Linguistic Variables and Gray Relational Analysis. Qual. Reliab. Eng. Int. 2015, 31, 761–772. [Google Scholar] [CrossRef]
- Bisset, G.S. An honest day’s work: Pay for performance in a pediatric radiology department. Pediatr. Radiol. 2017, 47, 798–802. [Google Scholar] [CrossRef]
- Wallin, A.; Gustafsson, M.; Carlsson, A.A.; Lundén, M. Radiographers’ experience of risks for patient safety incidents in the radiology department. J. Clin. Nurs. 2019, 28, 1125–1134. [Google Scholar] [CrossRef]
- Tellis, R.; Starobinets, O.; Prokle, M.; Raghavan, U.N.; Hall, C.; Chugh, T.; Koker, E.; Chaduvula, S.C.; Wald, C.; Flacke, S. Identifying Areas for Operational Improvement and Growth in IR Workflow Using Workflow Modeling, Simulation, and Optimization Techniques. J. Digit. Imaging 2020, 34, 75–84. [Google Scholar] [CrossRef]
- Alawad, S.; Abujamea, A. Awareness of radiation hazards in patients attending radiology departments. Radiat. Environ. Biophys. 2021, 60, 453–458. [Google Scholar] [CrossRef]
- Raziei, Z.; Torabi, S.A.; Tabrizia, S.; Zahiri, B. A Hybrid GDM-SERVQUAL-QFD Approach for Service Quality Assessment in Hospitals. Eng. Manag. J. 2018, 30, 179–190. [Google Scholar] [CrossRef]
- Altuntas, S.; Kansu, S. An innovative and integrated approach based on SERVQUAL, QFD and FMEA for service quality improvement. Kybernetes 2019, 49, 2419–2453. [Google Scholar] [CrossRef]
- Tuzkaya, G.; Sennatoglu, B.; Kalender, Z.T.; Mutlu, M. Hospital service quality evaluation with IVIF-PROMETHEE and a case study. Socio-Econ. Plan. Sci. 2019, 68, 100705. [Google Scholar] [CrossRef]
- Li, X.B.; He, Z. An integrated approach for evaluating hospital service quality with linguistic preferences. Int. J. Prod. Res. 2021, 59, 1776–1790. [Google Scholar] [CrossRef]
- Liu, A.J.; Guo, X.R.; Liu, T.N.; Zhang, Y.; Tsai, S.-B.; Zhu, Q.; Hsu, C.-F. A GRA-Based Method for Evaluating Medical Service Quality. IEEE Access 2019, 7, 34252–34264. [Google Scholar] [CrossRef]
- Yucesan, M.; Gul, M. Hospital service quality evaluation: An integrated model based on Pythagorean fuzzy AHP and fuzzy TOPSIS. Soft Comput. 2020, 24, 3237–3255. [Google Scholar] [CrossRef]
- Alkafaji, M.K.; Salih, A.E. A Fuzzy Assessment Model for Hospitals Services Quality based on Patient Experience. Karbala Int. J. Mod. Sci. 2020, 6, 10. [Google Scholar] [CrossRef]
- Akram, M.; Muhiuddin, G.; Santos-Garica, G. An enhanced VIKOR method for multi-criteria group decision-making with complex Fermatean fuzzy set. Math. Biosci. Eng. 2022, 19, 7201–7231. [Google Scholar] [CrossRef] [PubMed]
- Akram, M.; Ramzan, N.; Feng, F. Extending COPRAS Method with Linguistic Fermatean Fuzzy Sets and Hamy Mean Operators. J. Math. 2022, 2022, 8239263. [Google Scholar] [CrossRef]
- Yüksel, S.; Dinçer, H. Identifying the Strategic Priorities of Nuclear Energy Investments Using Hesitant 2-tuple Interval-valued Pythagorean Fuzzy DEMATEL. Prog. Nucl. Energy 2022, 145, 104103. [Google Scholar] [CrossRef]
- Najafpour, Z.; Hasoumi, M.; Behzahi, F.; Mohamadi, E.; Jafary, M.; Saeedi, M. Preventing Blood Transfusion Failures: FMEA, an Effective Assessment Method. BMC Health Serv. Res. 2017, 17, 453. [Google Scholar] [CrossRef]
- Tooranloo, H.S.; Ayatollah, A.S.; Alboghobish, S. Evaluating Knowledge Management Failure Factors Using Intuitionistic Fuzzy FMEA Approach. Knowl. Inf. Syst. 2018, 57, 183–205. [Google Scholar] [CrossRef]
- Mete, S. Assessing Occupational Risks in Pipeline Construction Using FMEA-based AHP-MOORA Integrated Approach under Pythagorean Fuzzy Environment. Hum. Ecol. Risk Assess. 2019, 25, 1645–1660. [Google Scholar] [CrossRef]
- Lo, H.W.; Shiue, W.; Liou, J.J.H.; Tzeng, G.-H. A Hybrid MCDM-based FMEA Model for Identification of Critical Failure Modes in Manufacturing. Soft Comput. 2020, 24, 15733–15745. [Google Scholar] [CrossRef]
- Zhou, J.; Liu, Y.; Xiahou, T.F.; Huang, T. A Novel FMEA-Based Approach to Risk Analysis of Product Design Using Extended Choquet Integral. IEEE Trans. Reliab. 2021, 71, 1264–1280. [Google Scholar] [CrossRef]
- Shi, S.X.; Fei, H.Y.; Xu, X.G. Application of a FMEA Method Combining Interval 2-tuple Linguistic Variables and Grey Relational Analysis in Preoperative Medical Service Process. IFAC Pap. OnLine 2019, 52, 1242–1247. [Google Scholar] [CrossRef]
- Liu, S.; Guo, X.J.; Zhang, L.Y. An Improved Assessment Method for FMEA for a Shipboard Integrated Electric Propulsion System Using Fuzzy Logic and DEMATEL Theory. Energies 2019, 12, 3162. [Google Scholar] [CrossRef]
- Li, G.F.; Li, Y.; Chen, C.H.; He, J.-L.; Hou, T.-W.; Chen, J.-H. Advanced FMEA Method Based on Interval 2-tuple Linguistic Variables and TOPSIS. Qual. Eng. 2020, 32, 653–662. [Google Scholar] [CrossRef]
- Mel, H.S.; David, S. Directing Improvements in Primary Care Patient Experience through Analysis of Service Quality. Health Serv. Res. 2018, 53, 4647–4666. [Google Scholar]
- Cheng, C.X.; Qi, Y.M.; Zhang, H. Research on the Value Application of Fishbone Diagram Analysis in the Management and Control of Wound Infection in Operating Room. In Proceedings of the 2018 3rd International Conference on Life Sciences, Medicine and Health, Chongqing, China, 8–11 November 2018. [Google Scholar] [CrossRef]
- Sadeghi, C.; Khan, H.A.; Gudleski, G.; Reynolds, J.L.; Bakhai, S.Y. Multifaceted Strategies to Improve Blood Pressure Control in a Primary Care Clinic: A Quality Improvement Project. Int. J. Cardiol. Hypertens. 2020, 7, 100060. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.T.; Tai, W.S. Measuring the Intellectual Capital Performance Based on 2-Tuple Fuzzy Linguistic Information. 2005. Available online: http://gebrc.nccu.edu.tw/proceedings/APDSI/2005/SessionIndex/DSS%201/DDS-5.pdf (accessed on 1 November 2022).
- Chang, K.H.; Chang, Y.C.; Tsai, I.T. Enhancing FMEA assessment by integrating grey relational analysis and the decision making trial and evaluation laboratory approach. Eng. Fail. Anal. 2013, 31, 211–224. [Google Scholar] [CrossRef]
- Bali, O.; Gumus, S. Multi-terms MADM Procedures with GRA and TOPSIS Based on IFS and IVIFS. Grey Syst. 2014, 4, 164–185. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).