A Pilot Study on Attentional Focus in Prescribing Physical Exercise in Outpatients with Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Multidisciplinary Rehabilitation Program
2.3. Procedures
2.3.1. Fitness Parameters
2.3.2. Body Composition and Anthropometric Parameters
2.4. Training Intervention
2.5. Statement of Ethics
2.6. Statistical Analysis
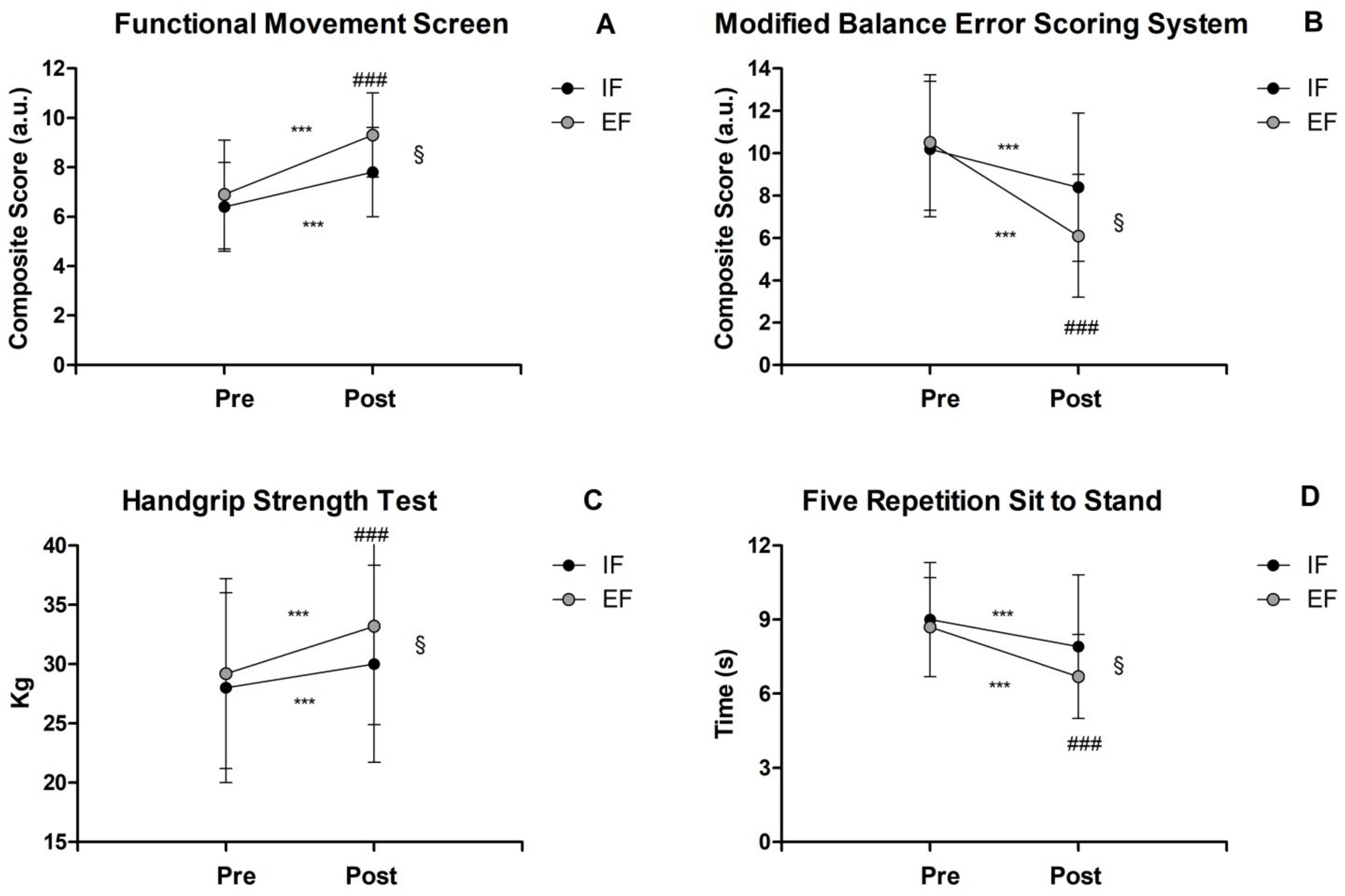
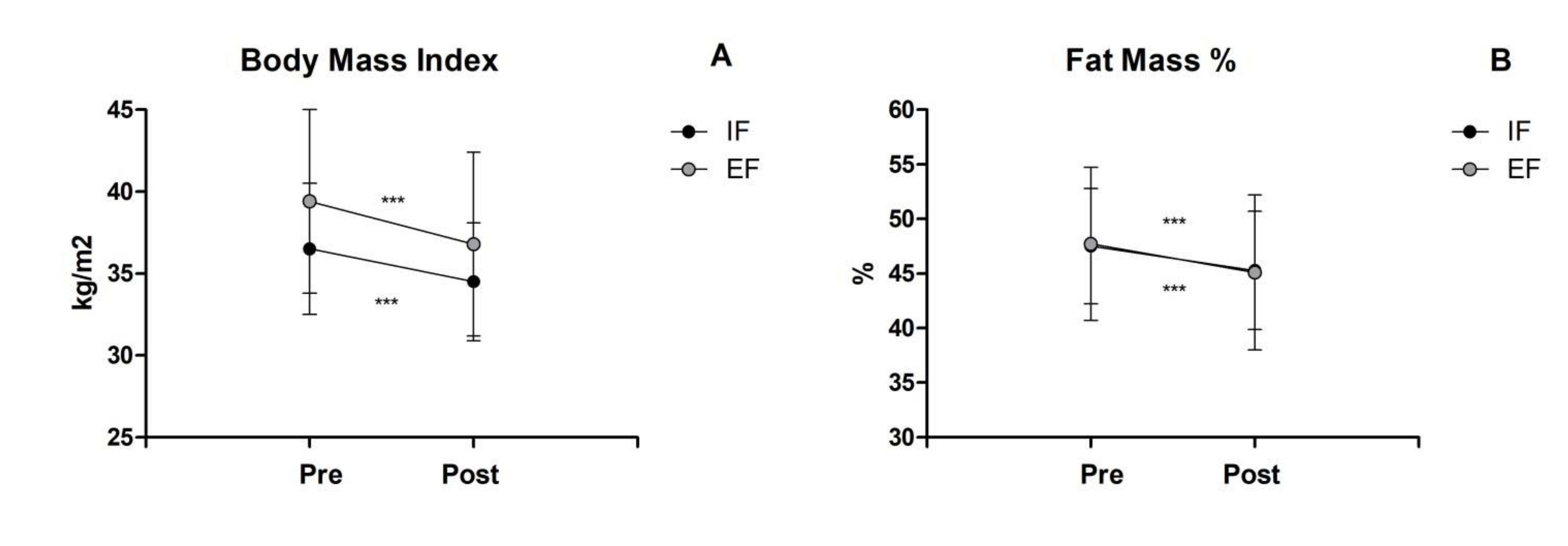
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lin, X.; Zhang, X.; Guo, J.; Roberts, C.K.; McKenzie, S.; Wu, W.C.; Liu, S.; Song, Y. Effects of Exercise Training on Cardiorespiratory Fitness and Biomarkers of Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002014. [Google Scholar] [CrossRef] [PubMed]
- Ratamess, N.A.; Alvar, B.A.; Evetoch, T.E.; Housh, T.J.; Ben Kibler, W.; Kraemer, W.J.; Triplett, N.T. Progression models in resistance training for healthy adults. Med. Sci. Sport. Exerc. 2009, 41, 687–708. [Google Scholar] [CrossRef]
- Benz, A.; Winkelman, N.; Porter, J.; Nimphius, S. Coaching Instructions and Cues for Enhancing Sprint Performance. Strength Cond. J. 2016, 38, 1–11. [Google Scholar] [CrossRef]
- Chua, L.K.; Jimenez-Diaz, J.; Lewthwaite, R.; Kim, T.; Wulf, G. Superiority of external attentional focus for motor performance and learning: Systematic reviews and meta-analyses. Psychol. Bull. 2021, 147, 618–645. [Google Scholar] [CrossRef]
- Wulf, G. Attentional focus and motor learning: A review of 15 years. Int. Rev. Sport Exerc. Psychol. 2013, 6, 77–104. [Google Scholar] [CrossRef]
- Wulf, G.; Shea, C.; Park, J.H. Attention and Motor Performance: Preferences for and Advantages of an External Focus. Res. Q. Exerc. Sport 2001, 72, 335–344. [Google Scholar] [CrossRef]
- Wulf, G.; Mercer, J.; McNevin, N.; Guadagnoli, M.A. Reciprocal Influences of Attentional Focus on Postural and Suprapostural Task Performance. J. Mot. Behav. 2004, 36, 189–199. [Google Scholar] [CrossRef]
- Wulf, G.; Töllner, T.; Shea, C.H. Attentional Focus Effects as a Function of Task Difficulty. Res. Q. Exerc. Sport 2007, 78, 257–264. [Google Scholar] [CrossRef]
- Ashraf, R.; Aghdasi, M.T.; Sayyah, M.; Taghibiglo, N. The Effects of Internal and External Focus of Attention on Children’s Performance in Vertical Jump Task. Int. J. Basic Sci. Appl. Res. 2012, 6, 1–7. [Google Scholar]
- Lohse, K.R.; Sherwood, D. Thinking about muscles: The neuromuscular effects of attentional focus on accuracy and fatigue. Acta Psychol. 2012, 140, 236–245. [Google Scholar] [CrossRef]
- Marchant, D.C.; Greig, M.; Scott, C. Attentional Focusing Instructions Influence Force Production and Muscular Activity during Isokinetic Elbow Flexions. J. Strength Cond. Res. 2009, 23, 2358–2366. [Google Scholar] [CrossRef] [PubMed]
- Lohse, K.R.; Sherwood, D.E.; Healy, A.F. How changing the focus of attention affects performance, kinematics, and electromyography in dart throwing. Hum. Mov. Sci. 2010, 29, 542–555. [Google Scholar] [CrossRef] [PubMed]
- Halperin, I.; Hughes, S.; Panchuk, D.; Abbiss, C.; Chapman, D.W. The Effects of Either a Mirror, Internal or External Focus Instructions on Single and Multi-Joint Tasks. PLoS ONE 2016, 11, e0166799. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, Y.A.; Keller, M.; Ruffieux, J.; Taube, W. Adopting an external focus of attention alters intracortical inhibition within the primary motor cortex. Acta Physiol. 2016, 220, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Wulf, G.; Dufek, J.; Lozano, L.; Pettigrew, C. Increased jump height and reduced EMG activity with an external focus. Hum. Mov. Sci. 2010, 29, 440–448. [Google Scholar] [CrossRef]
- Coratella, G.; Tornatore, G.; Longo, S.; Borrelli, M.; Doria, C.; Esposito, F.; Cè, E. The Effects of Verbal Instructions on Lower Limb Muscles’ Excitation in Back-Squat. Res. Q. Exerc. Sport 2020, 93, 429–435. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Vigotsky, A.; Contreras, B.; Golden, S.; Alto, A.; Larson, R.; Winkelman, N.; Paoli, A. Differential effects of attentional focus strategies during long-term resistance training. Eur. J. Sport Sci. 2018, 18, 705–712. [Google Scholar] [CrossRef]
- Abdollahipour, R.; Land, W.M.; Cereser, A.; Chiviacowsky, S. External relative to internal attentional focus enhances motor performance and learning in visually impaired individuals. Disabil. Rehabil. 2019, 42, 2621–2630. [Google Scholar] [CrossRef]
- Beck, E.N.; Almeida, Q.J. Dopa-Responsive Balance Changes Depend on Use of Internal versus External Attentional Focus in Parkinson Disease. Phys. Ther. 2016, 97, 208–216. [Google Scholar] [CrossRef]
- Landers, M.R.; Hatlevig, R.M.; Davis, A.D.; Richards, A.R.; Rosenlof, L.E. Does attentional focus during balance training in people with Parkinson’s disease affect outcome? A randomised controlled clinical trial. Clin. Rehabil. 2015, 30, 53–63. [Google Scholar] [CrossRef]
- Durham, K.; Sackley, C.; Wright, C.; Wing, A.; Edwards, M.; van Vliet, P. Attentional focus of feedback for improving performance of reach-to-grasp after stroke: A randomised crossover study. Physiotherapy 2013, 100, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Fasoli, S.E.; Trombly, C.A.; Tickle-Degnen, L.; Verfaellie, M.H. Effect of Instructions on Functional Reach in Persons with and without Cerebrovascular Accident. Am. J. Occup. Ther. 2002, 56, 380–390. [Google Scholar] [CrossRef] [PubMed]
- McNevin, N.; Weir, P.; Quinn, T. Effects of Attentional Focus and Age on Suprapostural Task Performance and Postural Control. Res. Q. Exerc. Sport 2013, 84, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Porter, J.M.; Anton, P.M. Directing attention externally improves continuous visuomotor skill performance in older adults who have undergone cancer chemotherapy. J. Am. Geriatr. Soc. 2011, 59, 369–370. [Google Scholar] [CrossRef] [PubMed]
- Pourazar, M.; Mirakhori, F.; Bagherzadeh, F.; Hemayattalab, R. Effects of External and Internal Focus of Attention in Motor Learning of Children with Cerebral Palsy. Int. J. Sport Health Sci. 2017, 11, 361–366. [Google Scholar]
- Shafizadeh, M.; Platt, G.K.; Mohammadi, B. Effects of different focus of attention rehabilitative training on gait performance in Multiple Sclerosis patients. J. Bodyw. Mov. Ther. 2013, 17, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Maktouf, W.; Durand, S.; Boyas, S.; Pouliquen, C.; Beaune, B. Combined effects of aging and obesity on postural control, muscle activity and maximal voluntary force of muscles mobilizing ankle joint. J. Biomech. 2018, 79, 198–206. [Google Scholar] [CrossRef]
- Błaszczyk, J.W.; Cieślińska-Świder, J.; Plewa, M.; Zahorska-Markiewicz, B.; Markiewicz, A. Effects of excessive body weight on postural control. J. Biomech. 2009, 42, 1295–1300. [Google Scholar] [CrossRef]
- Hills, A.P.; Hennig, E.M.; Byrne, N.M.; Steele, J.R. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obes. Rev. 2002, 3, 35–43. [Google Scholar] [CrossRef]
- Baños, R.M.; Escobar, P.; Cebolla, A.; Guixeres, J.; Pitti, J.A.; Lisón, J.F.; Botella, C. Using Virtual Reality to Distract Overweight Children from Bodily Sensations During Exercise. Cyberpsychol. Behav. Soc. Netw. 2016, 19, 115–119. [Google Scholar] [CrossRef]
- Van Abswoude, F.; Nuijen, N.B.; Van Der Kamp, J.; Steenbergen, B. Individual Differences Influencing Immediate Effects of Internal and External Focus Instructions on Children’s Motor Performance. Res. Q. Exerc. Sport 2018, 89, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Cavaggioni, L.; Gilardini, L.; Redaelli, G.; Croci, M.; Capodaglio, P.; Gobbi, M.; Bertoli, S. Effects of a Randomized Home-Based Quality of Movement Protocol on Function, Posture and Strength in Outpatients with Obesity. Healthcare 2021, 9, 1451. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef] [PubMed]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 1. Int. J. Sport. Phys. Ther. 2014, 9, 396–409. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 2. Int. J. Sport. Phys. Ther. 2014, 9, 549–563. [Google Scholar]
- Molina-Garcia, P.; Migueles, J.H.; Cadenas-Sanchez, C.; Esteban-Cornejo, I.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Plaza-Florido, A.; Molina-Molina, A.; Garcia-Delgado, G.; D’Hondt, E.; et al. Fatness and fitness in relation to functional movement quality in overweight and obese children. J. Sport. Sci. 2018, 37, 878–885. [Google Scholar] [CrossRef]
- Iverson, G.L.; Koehle, M.S. Normative data for the modified balance error scoring system in adults. Brain Inj. 2013, 27, 596–599. [Google Scholar] [CrossRef]
- Iverson, G.L.; Koehle, M.S. Normative Data for the Balance Error Scoring System in Adults. Rehabil. Res. Pract. 2013, 2013, 846418. [Google Scholar] [CrossRef]
- Trecroci, A.; Duca, M.; Cavaggioni, L.; Rossi, A.; Scurati, R.; Longo, S.; Merati, G.; Alberti, G.; Formenti, D. Relationship between Cognitive Functions and Sport-Specific Physical Performance in Youth Volleyball Players. Brain Sci. 2021, 11, 227. [Google Scholar] [CrossRef]
- Hamilton, G.F.; McDonald, C.; Chenier, T.C. Measurement of Grip Strength: Validity and Reliability of the Sphygmomanometer and Jamar Grip Dynamometer. J. Orthop. Sport. Phys. Ther. 1992, 16, 215–219. [Google Scholar] [CrossRef]
- Bohannon, R.W. Test-Retest Reliability of the Five-Repetition Sit-to-Stand Test: A Systematic Review of the Literature Involving Adults. J. Strength Cond. Res. 2011, 25, 3205–3207. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Bubela, D.J.; Magasi, S.R.; Wang, Y.C.; Gershon, R.C. Sit-to-stand test: Performance and determinants across the age-span. Isokinet. Exerc. Sci. 2010, 18, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Cavaggioni, L.; Trecroci, A.; Tosin, M.; Iaia, F.M.; Alberti, G. Individualized dry-land intervention program for an elite Paralympic swimmer. J. Sport. Med. Phys. Fit. 2018, 59, 82–86. [Google Scholar] [CrossRef]
- Robertson, R.J.; Goss, F.L.; Rutkowski, J.; Lenz, B.; Dixon, C.; Timmer, J.; Frazee, K.; Dube, J.; Andreacci, J. Concurrent Validation of the OMNI Perceived Exertion Scale for Resistance Exercise. Med. Sci. Sport. Exerc. 2003, 35, 333–341. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S. Application of the TIDieR checklist to improve understanding and replicability of studies in Physical and Rehabilitation Medicine. Eur. J. Phys. Rehabil. Med. 2015, 51, 667–668. [Google Scholar] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013; ISBN 978-1-134-74277-6. [Google Scholar]
- Samsa, G.; Edelman, D.; Rothman, M.L.; Williams, G.R.; Lipscomb, J.; Matchar, D. Determining Clinically Important Differences in Health Status Measures: A General Approach with Illustration to the Health Utilities Index Mark II. Pharmacoeconomics 1999, 15, 141–155. [Google Scholar] [CrossRef] [PubMed]
- Capodaglio, P.; Cimolin, V.; Tacchini, E.; Parisio, C.; Galli, M. Balance Control and Balance Recovery in Obesity. Curr. Obes. Rep. 2012, 1, 166–173. [Google Scholar] [CrossRef]
- Grgic, J.; Mikulic, I.; Mikulic, P. Acute and Long-Term Effects of Attentional Focus Strategies on Muscular Strength: A Meta-Analysis. Sports 2021, 9, 153. [Google Scholar] [CrossRef]
- Halperin, I.; Williams, K.J.; Martin, D.T.; Chapman, D.W. The Effects of Attentional Focusing Instructions on Force Production During the Isometric Midthigh Pull. J. Strength Cond. Res. 2016, 30, 919–923. [Google Scholar] [CrossRef]
- Nadzalan, A.; Lee, J.L.F.; Azzfar, M.S.; Muhammad, N.S.; Chan, E.W.M.; Mohamad, N.I. The Effects of Resistance Training with Different Focus Attention on Muscular Strength: Application to Teaching Methods in Physical Conditioning Class. Age 2019, 8, 5. [Google Scholar]
- Bredin, S.S.; Dickson, D.B.; Warburton, D.E. Effects of varying attentional focus on health-related physical fitness performance. Appl. Physiol. Nutr. Metab. 2013, 38, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, D.J.; Erskine, R.; Morse, C.; Winwood, K.; Onambélé-Pearson, G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology 2015, 17, 467–483. [Google Scholar] [CrossRef] [PubMed]
- Roh, E.; Choi, K.M. Health Consequences of Sarcopenic Obesity: A Narrative Review. Front. Endocrinol. 2020, 11, 332. [Google Scholar] [CrossRef] [PubMed]
- Bilman, E.; Van Kleef, E.; Van Trijp, H. External cues challenging the internal appetite control system—Overview and practical implications. Crit. Rev. Food Sci. Nutr. 2015, 57, 2825–2834. [Google Scholar] [CrossRef] [PubMed]
- Wulf, G.; McNevin, N.; Shea, C.H. The automaticity of complex motor skill learning as a function of attentional focus. Q. J. Exp. Psychol. Sect. A 2001, 54, 1143–1154. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, Y.A.; Keller, M.; Egger, S.; Taube, W. Effects of an external compared to an internal focus of attention on the excitability of fast and slow(er) motor pathways. Sci. Rep. 2021, 11, 17910. [Google Scholar] [CrossRef]
- Gilardini, L.; Cancello, R.; Cavaggioni, L.; Bruno, A.; Novelli, M.; Mambrini, S.P.; Castelnuovo, G.; Bertoli, S. Are People with Obesity Attracted to Multidisciplinary Telemedicine Approach for Weight Management? Nutrients 2022, 14, 1579. [Google Scholar] [CrossRef]
- Formenti, D.; Trecroci, A.; Cavaggioni, L.; Caumo, A.; Alberti, G. Heart rate response to a marathon cross-country skiing race: A case study. Sport Sci. Health 2014, 11, 125–128. [Google Scholar] [CrossRef]
| Name of Exercise | IF Cue | EF Cue |
|---|---|---|
| Yoga Triangle Pose | Keep your feet wider than shoulder-width apart, extend one elbow overhead and bend to the side the spine at the hip joint and then return to the starting position. | Open your legs laterally, push one arm to the sky and then bend to the side the spine like a half-moon and then return to the starting position. |
| Wall Lat stretching | Facing the wall and staying a foot away, flex forward your spine at the hip joint, putting your hands on the wall. | Facing a wall and staying a foot away, lean forward your spine, gently putting your hands on the wall while imagining moving the wall away. |
| In place standing marching | Stand with your feet slightly apart with arms at the side; then, start to step in place, lifting your knees and moving your arms, both flexed at 90° at the elbow. | Stand with your feet slightly apart with arms at the side; then, start to step in place as if you are a puppet; please swing your arms like a pendulum. |
| Goblet Squat with dumbbell | Stand with your feet shoulder-width apart, then go down in a squatting position by bending your hips and knees at 90° flexed. | Stand with your feet shoulder-width apart, then go down with your back by imagining sitting on an invisible stool behind you. |
| Dumbbells curl to press | Flex simultaneously both elbows to the shoulders, rotate your palms outwards and then extend both elbows overhead. | Curl both arms simultaneously like a hook and then push them gently to the sky by imagining putting a suitcase on a shelf. |
| In place forward lunges | Start with feet hip-width apart, then take a big step forward with one leg by flexing your knees at 90° until the thigh is parallel to the floor and the shin is vertical. | Start with feet hip-width apart, then take a big step forward with one leg and bend both knees as if you are picking up two suitcases from the ground. |
| Wall push-up with torso rotation | Place both hands on the wall at shoulder height, slightly wider than your shoulders; then, take a step backward with both feet. From here flex both elbows approaching the sternum toward the wall. Finally, push yourself away from the wall, reaching the starting position, and begin to externally rotate the torso. | Place both hands on the wall at shoulder height, then take a step backward with both feet. From here, bend your arms, lowering the upper-body toward the wall. Finally, push yourself away from the wall as if you want to push someone away and begin to rotate your body outward as if you are screwing in a light bulb. |
| One-Arm overhead dumbbell extension from staggered stance | Hold a dumbbell in one hand behind your head, with your elbow flexed and pointed toward the ceiling. Then, extend your elbow overhead until the arm is straight with the dumbbell directly above you. | Hold a dumbbell in one hand behind your head, with your arm bent. Then, gently extend your arm to the sky by imagining hammering a nail. |
| Characteristics | IF, n = 47 | EF, n = 47 |
|---|---|---|
| Participants’ Age (years) | 54.3 ± 10.1 | 53.9 ± 10.4 |
| Sex (Male/Female) | 8/39 | 9/38 |
| Body Mass Index (kg/m2) | 36.5 ± 4.0 | 37.7 ± 3.9 |
| Fat Mass (%) | 47.5 ± 5.3 | 47.7 ± 4.2 |
| Functional Movement Screen (a.u.) | 6.5 ± 1.9 | 6.9 ± 1.8 |
| Modified Balance Error Scoring System (a.u.) | 10.2 ± 3.3 | 10.5 ± 3.3 |
| Handgrip Strength Test (kg) | 28.0 ± 8.0 | 29.3 ± 9.8 |
| Five-Repetition Sit-to-Stand test (s) | 9.0 ± 3.0 | 8.8 ± 2.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cavaggioni, L.; Gilardini, L.; Redaelli, G.; Croci, M.; Cancello, R.; Capodaglio, P.; Bruno, A.; Bertoli, S. A Pilot Study on Attentional Focus in Prescribing Physical Exercise in Outpatients with Obesity. Healthcare 2022, 10, 2306. https://doi.org/10.3390/healthcare10112306
Cavaggioni L, Gilardini L, Redaelli G, Croci M, Cancello R, Capodaglio P, Bruno A, Bertoli S. A Pilot Study on Attentional Focus in Prescribing Physical Exercise in Outpatients with Obesity. Healthcare. 2022; 10(11):2306. https://doi.org/10.3390/healthcare10112306
Chicago/Turabian StyleCavaggioni, Luca, Luisa Gilardini, Gabriella Redaelli, Marina Croci, Raffaella Cancello, Paolo Capodaglio, Amalia Bruno, and Simona Bertoli. 2022. "A Pilot Study on Attentional Focus in Prescribing Physical Exercise in Outpatients with Obesity" Healthcare 10, no. 11: 2306. https://doi.org/10.3390/healthcare10112306
APA StyleCavaggioni, L., Gilardini, L., Redaelli, G., Croci, M., Cancello, R., Capodaglio, P., Bruno, A., & Bertoli, S. (2022). A Pilot Study on Attentional Focus in Prescribing Physical Exercise in Outpatients with Obesity. Healthcare, 10(11), 2306. https://doi.org/10.3390/healthcare10112306









