Might Dog Walking Reduce the Impact of COPD on Patients’ Life?
Abstract
:1. Introduction
2. Materials and Methods
- CAT [33] an 8-item unidimensional measure of health status impairment in COPD. The score ranges from 0 to 40, with higher scores representing worse health.
- EuroQol-5D (EQ-5D), developed in 1990, is a most widely used generic questionnaire to assess HRQoL [35]. It is applicable to the general population as well as a wide range of health conditions including COPD [36]. It consists of five questions assessing whether subjects were experiencing problems (no, some/moderate, or severe/extreme) in 5 dimensions of health (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). It also includes a vertical visual analogue scale (VAS) asking subjects to rate their overall health on a scale from 0 (the worst imaginable health) to 100 (the best imaginable health).
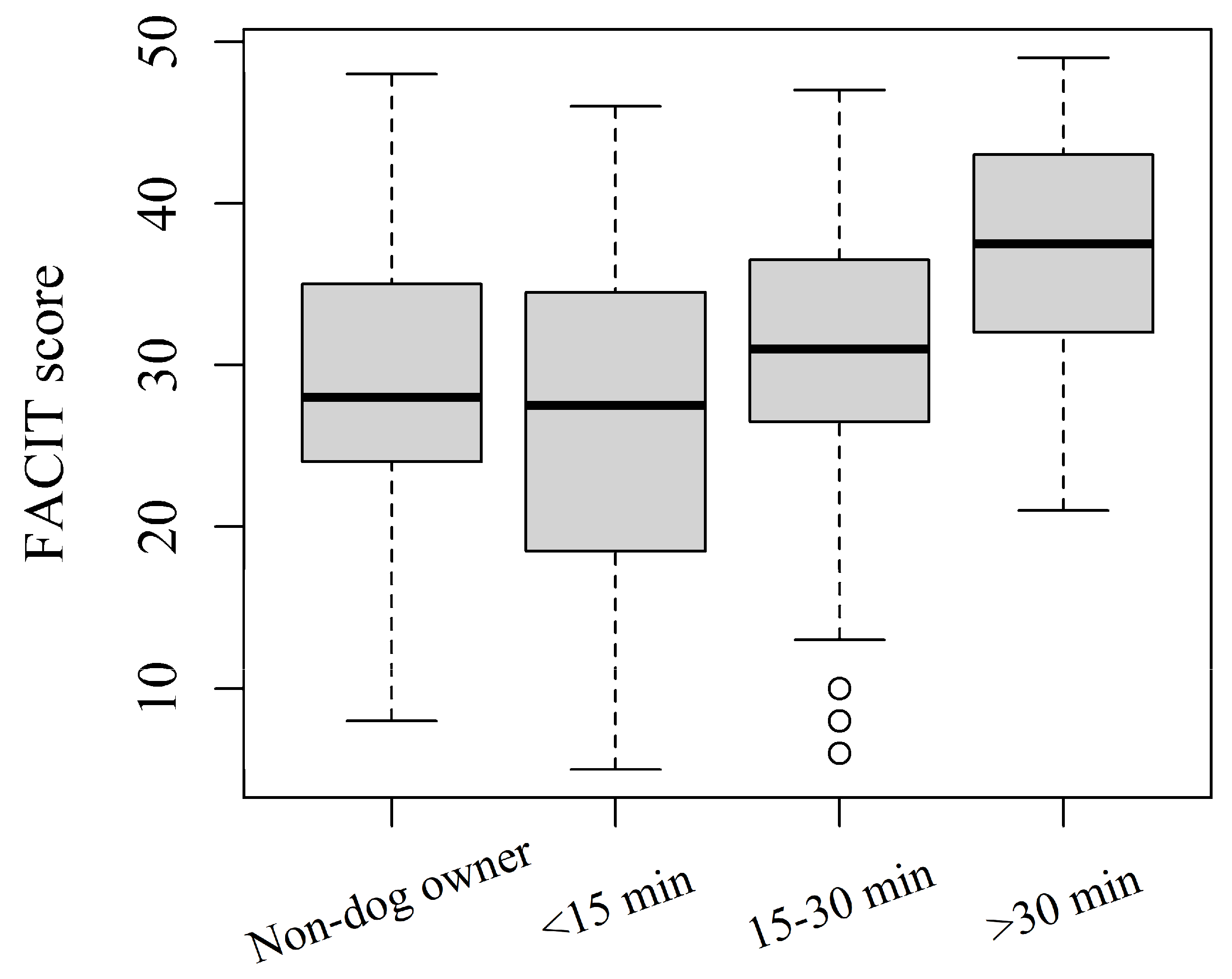
- Functional Assessment of Chronic Illness Therapy Fatigue Scale (FACIT-Fatigue), a 13-item questionnaire to assess fatigue and its impact on daily activities and functioning [37], which has been previously used in COPD [38,39,40]. The total score ranges from 0 to 52, with higher scores indicating less fatigue [41].
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miravitlles, M.; Ribera, A. Understanding the impact of symptoms on the burden of COPD. Respir. Res. 2017, 18, 67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kosteli, M.C.; Heneghan, N.R.; Roskell, C.; Williams, S.E.; Adab, P.; Dickens, A.P.; Enocson, A.; Fitzmaurice, D.A.; Jolly, K.; Jordan, R.; et al. Barriers and enablers of physical activity engagement for patients with COPD in primary care. Int. J. Chronic Obstr. Pulm. Dis. 2017, 12, 1019–1031. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donaire-Gonzalez, D.; Gimeno-Santos, E.; Balcells, E.; Rodríguez, D.A.; Farrero, E.; de Batlle, J.; Benet, M.; Ferrer, A.; Barberà, J.A.; Gea, J.; et al. Physical activity in COPD patients: Patterns and bouts. Eur. Respir. J. 2013, 42, 993–1002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vorrink, S.N.; Kort, H.S.; Troosters, T.; Lammers, J.W. Level of daily physical activity in individuals with COPD compared with healthy controls. Respir. Res. 2011, 12, 33. [Google Scholar] [CrossRef] [Green Version]
- Fermont, J.M.; Fisk, M.; Bolton, C.E.; MacNee, W.; Cockcroft, J.R.; Fuld, J.; Cheriyan, J.; Mohan, D.; Mäki-Petäjä, K.M.; Al-Hadithi, A.B.; et al. Cardiovascular risk prediction using physical performance measures in COPD: Results from a multicentre observational study. BMJ Open 2020, 10, e038360. [Google Scholar] [CrossRef]
- Watz, H.; Pitta, F.; Rochester, C.L.; Garcia-Aymerich, J.; ZuWallack, R.; Troosters, T.; Vaes, A.W.; Puhan, M.A.; Jehn, M.; Polkey, M.I.; et al. An official European Respiratory Society statement on physical activity in COPD. Eur. Respir. J. 2014, 44, 1521–1537. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Aymerich, J.; Lange, P.; Benet, M.; Schnohr, P.; Antó, J.M. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: A population based cohort study. Thorax 2006, 61, 772–778. [Google Scholar] [CrossRef] [Green Version]
- Yohannes, A.M.; Baldwin, R.C.; Connolly, M. Mortality predictors in disabling chronic obstructive pulmonary disease in old age. Age Ageing 2002, 31, 137–140. [Google Scholar] [CrossRef] [Green Version]
- Ramos, M.; Lamotte, M.; Gerlier, L.; Svangren, P.; Miquel-Cases, A.; Haughney, J. Cost-effectiveness of physical activity in the management of COPD patients in the UK. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 227–239. [Google Scholar] [CrossRef] [Green Version]
- Waschki, B.; Kirsten, A.; Holz, O.; Müller, K.C.; Meyer, T.; Watz, H.; Magnussen, H. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: A prospective cohort study. Chest 2011, 140, 331–342. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.T.; Tomata, Y.; Watanabe, T.; Sugawara, Y.; Kakizaki, M.; Tsuji, I. Relationships between changes in time spent walking since middle age and incident functional disability. Prev. Med. 2014, 59, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Rogers, N.T.; Marshall, A.; Roberts, C.H.; Demakakos, P.; Steptoe, A.; Scholes, S. Physical activity and trajectories of frailty among older adults: Evidence from the English Longitudinal Study of Ageing. PLoS ONE 2017, 12, e0170878. [Google Scholar] [CrossRef] [Green Version]
- Teba, P.P.; Esther, M.G.; Raquel, S.G. Association between physical activity and patient-reported outcome measures in patients with lung cancer: A systematic review and meta-analysis. Qual. Life Res. 2022, 31, 1963–1976. [Google Scholar] [CrossRef]
- Sritharan, S.S.; Østergaard, E.B.; Callesen, J.; Elkjaer, M.; Sand, L.; Hilberg, O.; Skaarup, S.H.; Løkke, A. Barriers toward Physical Activity in COPD: A Quantitative Cross-Sectional, Questionnaire-Based Study. J. Chronic Obstr. Pulm. Dis. 2021, 18, 272–280. [Google Scholar] [CrossRef]
- Thorpe, O.; Kumar, S.; Johnston, K. Barriers to and enablers of physical activity in patients with COPD following a hospital admission: A qualitative study. Int. J. Chronic Obstr. Pulm. Dis. 2014, 9, 115–128. [Google Scholar] [CrossRef] [Green Version]
- Sievi, N.A.; Senn, O.; Brack, T.; Brutsche, M.H.; Frey, M.; Irani, S.; Leuppi, J.D.; Thurnheer, R.; Franzen, D.; Kohler, M.; et al. Impact of comorbidities on physical activity in COPD. Respirology 2015, 20, 413–418. [Google Scholar] [CrossRef]
- Carl, J.; Schultz, K.; Janssens, T.; von Leupoldt, A.; Pfeifer, K.; Geidl, W. The “can do, do do” concept in individuals with chronic obstructive pulmonary disease: An exploration of psychological mechanisms. Respir. Res. 2021, 22, 260. [Google Scholar] [CrossRef]
- Lee, S.H.; Kim, K.U.; Lee, H.; Kim, Y.S.; Lee, M.K.; Park, H.K. Factors associated with low-level physical activity in elderly patients with chronic obstructive pulmonary disease. Korean J. Intern. Med. 2018, 33, 130–137. [Google Scholar] [CrossRef]
- Chen, M.L.; Chen, L.S.; Chen, Y.T.; Gardenhire, D.S. The Association of Health-Related Factors with Leisure-Time Physical Activity among Adults with COPD: A Cross-Sectional Analysis. Healthcare 2022, 10, 249. [Google Scholar] [CrossRef] [PubMed]
- Hartman, J.E.; Ten Hacken, N.H.; Boezen, H.M.; De Greef, M.H. Self-efficacy for physical activity and insight into its benefits are modifiable factors associated with physical activity in people with COPD: A mixed-methods study. J. Physiother. 2013, 59, 117–124. [Google Scholar] [CrossRef] [Green Version]
- Holland, A.E.; Cox, N.S.; Houchen-Wolloff, L.; Rochester, C.L.; Garvey, C.; ZuWallack, R.; Nici, L.; Limberg, T.; Lareau, S.C.; Yawn, B.P.; et al. Defining Modern Pulmonary Rehabilitation. An Official American Thoracic Society Workshop Report. Ann. Am. Thorac. Soc. 2021, 18, e12–e29. [Google Scholar] [CrossRef]
- Paixão, C.; Rocha, V.; Brooks, D.; Marques, A. Unsupervised physical activity interventions for people with COPD: A systematic review and meta-analysis. Pulmonology 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Christian, H.E.; Westgarth, C.; Bauman, A.; Richards, E.A.; Rhodes, R.E.; Evenson, K.R.; Mayer, J.A.; Thorpe, R.J., Jr. Dog ownership and physical activity: A review of the evidence. J. Phys. Act. Health 2013, 10, 750–759. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Westgarth, C.; Christley, R.M.; Jewell, C.; German, A.J.; Boddy, L.M.; Christian, H.E. Dog owners are more likely to meet physical activity guidelines than people without a dog: An investigation of the association between dog ownership and physical activity levels in a UK community. Sci. Rep. 2019, 9, 5704. [Google Scholar] [CrossRef] [Green Version]
- Reeves, M.J.; Rafferty, A.P.; Miller, C.E.; Lyon-Callo, S.K. The impact of dog walking on leisure-time physical activity: Results from a population-based survey of Michigan adults. J. Phys. Act. Health 2011, 8, 436–444. [Google Scholar] [CrossRef]
- Riske, J.; Janert, M.; Kahle-Stephan, M.; Nauck, M.A. Owning a Dog as a Determinant of Physical Activity and Metabolic Control in Patients with Type 1 and Type 2 Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2021, 129, 379–384. [Google Scholar] [CrossRef]
- Maugeri, A.; Medina-Inojosa, J.R.; Kunzova, S.; Barchitta, M.; Agodi, A.; Vinciguerra, M.; Lopez-Jimenez, F. Dog Ownership and Cardiovascular Health: Results from the Kardiovize 2030 Project. Mayo Clin. Proc. Innov. Qual. Outcomes 2019, 3, 268–275. [Google Scholar] [CrossRef]
- Forbes, C.C.; Blanchard, C.M.; Mummery, W.K.; Courneya, K.S. Dog ownership and physical activity among breast, prostate, and colorectal cancer survivors. Psychooncology 2017, 26, 2186–2193. [Google Scholar] [CrossRef]
- Kuban, M.; Królikowski, J.; Nowicki, M. Dog ownership status and self-assessed health, life-style and habitual physical activity in chronic hemodialysis patients. Hemodial Int. 2016, 20, 447–452. [Google Scholar] [CrossRef] [PubMed]
- Hancock, J.; Jackson, S.; Johnson, A.B. The Importance of Dog Ownership: Implications for Long-Term Weight Reduction after Gastric Banding. Am. J. Lifestyle Med. 2016, 11, 86–89. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [Green Version]
- Singh, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Criner, G.J.; Frith, P.; Halpin, D.M.G.; Han, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: The GOLD science committee report 2019. Eur. Respir. J. 2019, 53, 1900164. [Google Scholar] [CrossRef] [PubMed]
- Devlin, N.J.; Brooks, R. EQ-5D and the EuroQol group: Past, present and future. Appl. Health Econ. Health Policy 2017, 15, 127–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wacker, M.E.; Jörres, R.A.; Karch, A.; Koch, A.; Heinrich, J.; Karrasch, S.; Schulz, H.; Peters, A.; Gläser, S.; Ewert, R.; et al. Relative impact of COPD and comorbidities on generic health-related quality of life: A pooled analysis of the COSYCONET patient cohort and control subjects from the KORA and SHIP studies. Respir. Res. 2016, 17, 81. [Google Scholar] [CrossRef] [Green Version]
- Yellen, S.B.; Cella, D.F.; Webster, K.; Blendowski, C.; Kaplan, E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J. Pain Symptom. Manag. 1997, 13, 63–74. [Google Scholar] [CrossRef]
- Stridsman, C.; Skär, L.; Hedman, L.; Rönmark, E.; Lindberg, A. Fatigue affects health status and predicts mortality among subjects with COPD: Report from the population based OLIN COPD study. J. Chronic Obstr. Pulm. Dis. 2015, 12, 199–206. [Google Scholar] [CrossRef]
- Stridsman, C.; Svensson, M.; Johansson Strandkvist, V.; Hedman, L.; Backman, H.; Lindberg, A. The COPD Assessment Test (CAT) can screen for fatigue among patients with COPD. Ther. Adv. Respir. Dis. 2018, 12, 1753466618787380. [Google Scholar] [CrossRef] [Green Version]
- Baghai-Ravary, R.; Quint, J.K.; Goldring, J.J.; Hurst, J.R.; Donaldson, G.C.; Wedzicha, J.-A. Determinants and impact of fatigue in patients with chronic obstructive pulmonary disease. Respir. Med. 2009, 103, 216–223. [Google Scholar] [CrossRef]
- Cella, D. Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System; Center on Outcomes, Research and Education (Core), Evanston Northwestern Healthcare and Northwestern University: Evanston, IL, USA, 1997. [Google Scholar]
- Lipovetsky, S.; Nowakowska, E. Modeling with Structurally Missing Data by OLS and Shapley Value Regressions. Int. J. Oper. Quant. Manag. 2013, 19, 169–178. [Google Scholar]
- Soares, J.; Epping, J.N.; Owens, C.J.; Brown, D.R.; Lankford, T.J.; Simoes, E.J.; Caspersen, C.J. Odds of Getting Adequate Physical Activity by Dog Walking. J. Phys. Act. Health 2015, 12, S102–S109. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arbillaga-Etxarri, A.; Gimeno-Santos, E.; Barberan-Garcia, A.; Balcells, E.; Benet, M.; Borrell, E.; Celorrio, N.; Delgado, A.; Jané, C.; Marin, A.; et al. Long-term efficacy and effectiveness of a behavioural and community-based exercise intervention (Urban Training) to increase physical activity in patients with COPD: A randomised controlled trial. Eur. Respir. J. 2018, 52, 1800063. [Google Scholar] [CrossRef] [PubMed]
- Powell, L.; Edwards, K.M.; Bauman, A.; McGreevy, P.; Podberscek, A.; Neilly, B.; Sherrington, C.; Stamatakis, E. Does dog acquisition improve physical activity, sedentary behaviour and biological markers of cardiometabolic health? Results from a three-arm controlled study. BMJ Open Sport Exerc. Med. 2020, 6, e000703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, D.R.; Carroll, D.D.; Workman, L.M.; Carlson, S.A.; Brown, D.W. Physical activity and health-related quality of life: US adults with and without limitations. Qual. Life Res. 2014, 23, 2673–2680. [Google Scholar] [CrossRef] [Green Version]
- Ozdemir, K.; Keser, I.; Sen, I.; Ozgur Tan, M. Investigating the relationships between quality of life, fatigue and leisure time physical activity in prostate cancer patients. J. Back Musculoskelet. Rehabil. 2019, 32, 497–503. [Google Scholar] [CrossRef]
- Cui, Y.; Russel, M.; Davern, M.; Christian, H. Longitudinal evidence of the impact of dog ownership and dog walking on mental health. J. Public Health 2021, 43, e145–e152. [Google Scholar] [CrossRef]
- Waschki, B.; Spruit, M.A.; Watz, H.; Albert, P.S.; Shrikrishna, D.; Groenen, M.; Smith, C.; Man, W.D.; Tal-Singer, R.; Edwards, L.D.; et al. Physical activity monitoring in COPD: Compliance and associations with clinical characteristics in a multicenter study. Respir. Med. 2012, 106, 522–530. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Rio, F.; Rojo, B.; Casitas, R.; Lores, V.; Madero, R.; Romero, D.; Galera, R.; Villasante, C. Prognostic value of the objective measurement of daily physical activity in patients with COPD. Chest 2012, 142, 338–346. [Google Scholar] [CrossRef]
- Pitta, F.; Troosters, T.; Probst, V.S.; Spruit, M.A.; Decramer, M.; Gosselink, R. Physical activity and hospitalization for exacerbation of COPD. Chest 2006, 129, 536–544. [Google Scholar] [CrossRef] [Green Version]
- Barberà, J.A.; Roca, J.; Ferrer, A.; Félez, M.A.; Díaz, O.; Roger, N.; Rodriguez-Roisin, R. Mechanisms of worsening gas exchange during acute exacerbations of chronic obstructive pulmonary disease. Eur. Respir. J. 1997, 10, 1285–1291. [Google Scholar] [CrossRef] [PubMed]
- Maltais, F.; LeBlanc, P.; Simard, C.; Jobin, J.; Bérubé, C.; Bruneau, J.; Carrier, L.; Belleau, R. Skeletal muscle adaptation to endurance training in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1996, 154, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Das, U.N. Anti-inflammatory nature of exercise. Nutrition 2004, 20, 323–326. [Google Scholar] [CrossRef]
- Wright, R.A. Refining the prediction of effort: Brehm’s distinction between potential motivation and motivation intensity. Soc. Personal. Psychol. Compass 2008, 2, 682–701. [Google Scholar] [CrossRef]
- Westgarth, C.; Christley, R.M.; Christian, H.E. How might we increase physical activity through dog walking?: A comprehensive review of dog walking correlates. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, C.; Rhodes, R.E. Sizing up physical activity: The relationships between dog characteristics, dog owners’ motivations, and dog walking. Psychol. Sport Exerc. 2016, 24, 65–71. [Google Scholar] [CrossRef]
- Fletcher, M.J.; Upton, J.; Taylor-Fishwick, J.; Buist, S.A.; Jenkins, C.; Hutton, J.; Barnes, N.; Van Der Molen, T.; Walsh, J.W.; Jones, P.; et al. COPD uncovered: An international survey on the impact of chronic obstructive pulmonary disease [COPD] on a working age population. BMC Public Health 2011, 11, 612. [Google Scholar] [CrossRef] [Green Version]
- Kwon, H.Y.; Kim, E. Factors contributing to quality of life in COPD patients in South Korea. Int. J. Chronic Obstr. Pulm. Dis. 2016, 13, 103–109. [Google Scholar] [CrossRef] [Green Version]
- Esquinas, C.; Ramon, M.A.; Nuñez, A.; Molina, J.; Quintano, J.A.; Roman-Rodríguez, M.; Naberan, K.; Llor, C.; Roncero, C.; Miravitlles, M.; et al. Correlation between disease severity factors and EQ-5D utilities in chronic obstructive pulmonary disease. Qual. Life Res. 2020, 29, 607–617. [Google Scholar] [CrossRef]
| Overall n = 200 | Dog Owners n = 99 | Non-Dog Owners n = 101 | p-Value 1 | |
|---|---|---|---|---|
| Age (years) | 64.35 (9.56) | 62.9 (9.4) | 65.7 (9.6) | 0.038 |
| Gender | 1.000 | |||
| Male | 102 (51) | 50 (51) | 52 (51) | |
| Female | 98 (49) | 49 (49) | 49 (49) | |
| Education ≥8 years | 132 (66) | 69 (70) | 63 (62) | 0.345 |
| Retired | 89 (44) | 42 (42) | 47 (47) | 0.658 |
| Living alone | 31 (16) | 13 (13) | 18 (18) | 0.471 |
| Physical activity frequency | 0.071 | |||
| Never/hardly ever | 63 (32) | 27 (27) | 36 (36) | |
| <1 times/week | 29 (14) | 11 (11) | 18 (18) | |
| 1–2 times/week | 36 (18) | 16 (16) | 20 (20) | |
| 3–4 times/week | 26 (13) | 18 (18) | 8 (8) | |
| Almost every day | 46 (23) | 27 (27) | 19 (19) | |
| Dog-ownership duration | - | |||
| Non-dog owner | 101 (50) | 0 (0) | 101 (100) | |
| 0–2 years | 14 (7) | 14 (14) | 0 (0) | |
| 3–5 years | 34 (17) | 34 (34) | 0 (0) | |
| >5 years | 51 (26) | 51 (52) | 0 (0) | |
| Dog-walking duration | - | |||
| Non-dog owner | 101 (50) | 0 (0) | 101 (100) | |
| <15 min | 40 (20) | 40 (40) | 0 (0) | |
| 15–30 min | 47 (24) | 47 (47) | 0 (0) | |
| >30 min | 12 (6) | 12 (13) | 0 (0) |
| Physical Activity | Never/Hardly Ever (1) | <1 Times/Week (2) | 1–2 Times/Week (3) | 3–4 Times/Week (4) | Almost Every Day (5) | p-Value 1 | Group Separation 2 |
|---|---|---|---|---|---|---|---|
| CAT | 29.32 (5.35) | 23.17 (7.27) | 24.42 (5.13) | 24.15 (5.24) | 23.93 (5.80) | <0.001 | {2543}{1} |
| EQ5D | 0.69 (0.20) | 0.83 (0.13) | 0.81 (0.11) | 0.84 (0.08) | 0.85 (0.07) | <0.001 | {1}{3245} |
| VAS | 53.97 (14.19) | 64.45 (13.68) | 61.42 (13.45) | 62.69 (10.29) | 64.98 (10.50) | <0.001 | {1}{3425} |
| FACIT | 23.27 (8.75) | 32.72 (10.99) | 31.89 (7.89) | 32.54 (9.53) | 31.96 (8.62) | <0.001 | {1}{3542} |
| >1 exacerb. | 35 (56) | 13 (45) | 8 (22) | 5 (19) | 12 (26) | <0.001 | {4352}{21} |
| Dog-ownership | Non-dog owner (1) | 0–2 years (2) | 3–5 years (3) | >5 years (4) | - | p-value 1 | Group separation 2 |
| CAT | 25.16 (6.31) | 24.86 (8.24) | 25.32 (5.35) | 27.00 (5.87) | - | 0.340 | - |
| EQ5D | 0.79 (0.15) | 0.83 (0.16) | 0.78 (0.17) | 0.79 (0.15) | - | 0.735 | - |
| VAS | 60.45 (14.99) | 66.57 (10.19) | 60.47 (9.43) | 58.94 (13.02) | - | 0.316 | - |
| FACIT | 29.03 (9.14) | 32.57 (14.17) | 29.38 (9.87) | 29.25 (10.06) | - | 0.663 | - |
| >1 exacerb. | 41 (41) | 3 (21) | 10 (29) | 19 (37) | - | 0.415 | - |
| Dog-walking | Non-dog owner (1) | <15 min (2) | 15–30 min (3) | >30 min (4) | - | p-value 1 | Group separation 2 |
| CAT | 25.16 (6.31) | 27.52 (6.55) | 25.49 (5.40) | 23.92 (6.47) | - | 0.154 | - |
| EQ5D | 0.79 (0.15) | 0.74 (0.20) | 0.82 (0.11) | 0.88 (0.06) | - | 0.015 | {213}{34} |
| VAS | 60.45 (14.99) | 58.42 (12.71) | 60.77 (10.47) | 66.75 (11.34) | - | 0.313 | - |
| FACIT | 29.03 (9.14) | 26.77 (11.05) | 30.55 (9.82) | 36.67 (8.81) | - | 0.017 | {213}{34} |
| >1 exacerb. | 41 (41) | 15 (38) | 14 (30) | 3 (25) | - | 0.504 | - |
| Unadjusted Models | CAT | EQ5D | VAS | FACIT | ||||
|---|---|---|---|---|---|---|---|---|
| β | p-Value | β | p-Value | β | p-Value | β | p-Value | |
| Intercept | 23.92 (20.41, 27.43) | <0.001 | 0.88 (0.85, 0.91) § | <0.001 | 66.75 (59.12, 74.38) | <0.001 | 36.67 (31.15, 42.18) | <0.001 |
| Dog-walking >30 min (ref.) | - | - | - | - | - | - | - | - |
| Non-dog owner | 1.24 (−2.47, 4.96) | 0.510 | −0.09 (−0.14, −0.05) § | 0.043 | −6.30 (−14.38, 1.77) | 0.125 | −7.64 (−13.47, −1.80) | 0.011 |
| Dog-walking <15 min | 3.61 (−0.39, 7.61) | 0.077 | −0.14 (−0.22, −0.08) § | 0.004 | −8.33 (−17.03, 0.38) | 0.061 | −9.89 (−16.18, −3.60) | 0.002 |
| Dog-walking 15–30 min | 1.57 (−2.36, 5.51) | 0.431 | −0.07 (−0.11, 0.02) § | 0.177 | −5.98 (−14.54, 2.57) | 0.169 | −6.11 (−12.29, 0.07) | 0.053 |
| Adjusted Models | CAT | EQ5D | VAS | FACIT | ||||
| β | p-Value | β | p-Value | β | p-Value | β | p-Value | |
| Intercept | 29.51 (22.16, 36.87) | <0.001 | 0.77 (0.59, 0.97) § | <0.001 | 66.14 (50.44, 81.83) | <0.001 | 14.28 (3.13, 25.43) | 0.012 |
| Dog-walking >30 min (ref.) | - | - | - | - | - | - | - | - |
| Non-dog owner | −0.42 (−3.91, 3.07) | 0.813 | −0.05 (−0.10, 0.01) § | 0.262 | −2.23 (−9.68, 5.21) | 0.555 | −6.00 (−11.29, −0.71) | 0.026 |
| Dog-walking <15 min | 1.60 (−2.16, 5.37) | 0.402 | −0.09 (−0.16, −0.03) § | 0.043 | −3.98 (−12.01, 4.06) | 0.330 | −7.61 (−13.32, −1.90) | 0.009 |
| Dog-walking 15–30 min | 0.77 (−2.86, 4.41) | 0.675 | −0.04 (−0.09, 0.01) § | 0.348 | −3.28 (−11.04, 4.49) | 0.406 | −4.97 (−10.49, 0.54) | 0.077 |
| Age (unit increase) | −0.03 (−0.15, 0.08) | 0.584 | 0.0007 (−0.002, 0.003) § | 0.584 | −0.02 (−0.27, 0.23) | 0.868 | 0.31 (0.13, 0.49) | 0.001 |
| Female gender | 0.88 (−0.75, 2.51) | 0.287 | −0.03 (−0.07, 0.01) § | 0.098 | −6.63 (−10.1, −3.15) | <0.001 | −2.10 (−4.56, 0.37) | 0.095 |
| Education <8 years | 0.14 (−1.74, 2.02) | 0.883 | −0.02 (−0.07, 0.02) § | 0.334 | −1.75 (−5.77, 2.26) | 0.390 | −1.2 (−4.06, 1.65) | 0.406 |
| Retired | 1.08 (−1.09, 3.24) | 0.327 | −0.06 (−0.10, −0.01) § | 0.021 | −5.75 (−10.37, −1.13) | 0.015 | −4.64 (−7.92, −1.36) | 0.006 |
| Living alone | 2.23 (0.03, 4.43) | 0.047 | −0.05 (−0.12, 0.02) § | 0.064 | −1.27 (−5.98, 3.43) | 0.594 | −3.85 (−7.19, −0.51) | 0.024 |
| Physical activity | −4.92 (−6.72, −3.12) | <0.001 | 0.12 (0.07, 0.17) § | <0.001 | 7.31 (3.46, 11.16) | <0.001 | 7.20 (4.47, 9.94) | <0.001 |
| Unadjusted Models | >1 Exacerbations | |
|---|---|---|
| Odds Ratio | p-Value | |
| Dog-walking >30 min (ref.) | - | - |
| Non-dog owner | 2.05 (0.57, 9.66) | 0.303 |
| Dog-walking <15 min | 1.80 (0.45, 9.07) | 0.428 |
| Dog-walking 15–30 min | 1.27 (0.32, 6.38) | 0.744 |
| Adjusted Models | >1 Exacerbations | |
| Odds Ratio | p-Value | |
| Dog-walking >30 min (reference) | - | - |
| Non-dog owner | 1.31 (0.32, 6.81) | 0.725 |
| Dog-walking <15 min | 1.02 (0.22, 5.71) | 0.985 |
| Dog-walking 15–30 min | 0.85 (0.19, 4.63) | 0.839 |
| Age (unit increase) | 0.96 (0.92, 1.01) | 0.123 |
| Female gender | 1.42 (0.75, 2.68) | 0.279 |
| Education <8 years | 0.70 (0.32, 1.47) | 0.347 |
| Retired | 2.63 (1.10, 6.56) | 0.033 |
| Living alone | 0.76 (0.31, 1.78) | 0.541 |
| Regular physical activity § | 0.30 (0.15, 0.57) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baiardini, I.; Fasola, S.; Lorenzi, C.; Colombo, N.; Bruno, M.; La Grutta, S.; Scognamillo, C.; Braido, F. Might Dog Walking Reduce the Impact of COPD on Patients’ Life? Healthcare 2022, 10, 2317. https://doi.org/10.3390/healthcare10112317
Baiardini I, Fasola S, Lorenzi C, Colombo N, Bruno M, La Grutta S, Scognamillo C, Braido F. Might Dog Walking Reduce the Impact of COPD on Patients’ Life? Healthcare. 2022; 10(11):2317. https://doi.org/10.3390/healthcare10112317
Chicago/Turabian StyleBaiardini, Ilaria, Salvatore Fasola, Chiara Lorenzi, Nicole Colombo, Matteo Bruno, Stefania La Grutta, Carla Scognamillo, and Fulvio Braido. 2022. "Might Dog Walking Reduce the Impact of COPD on Patients’ Life?" Healthcare 10, no. 11: 2317. https://doi.org/10.3390/healthcare10112317
APA StyleBaiardini, I., Fasola, S., Lorenzi, C., Colombo, N., Bruno, M., La Grutta, S., Scognamillo, C., & Braido, F. (2022). Might Dog Walking Reduce the Impact of COPD on Patients’ Life? Healthcare, 10(11), 2317. https://doi.org/10.3390/healthcare10112317







