HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. General Characteristics of the Study Group
3.2. HPV Vaccination Level in Poland by Gender
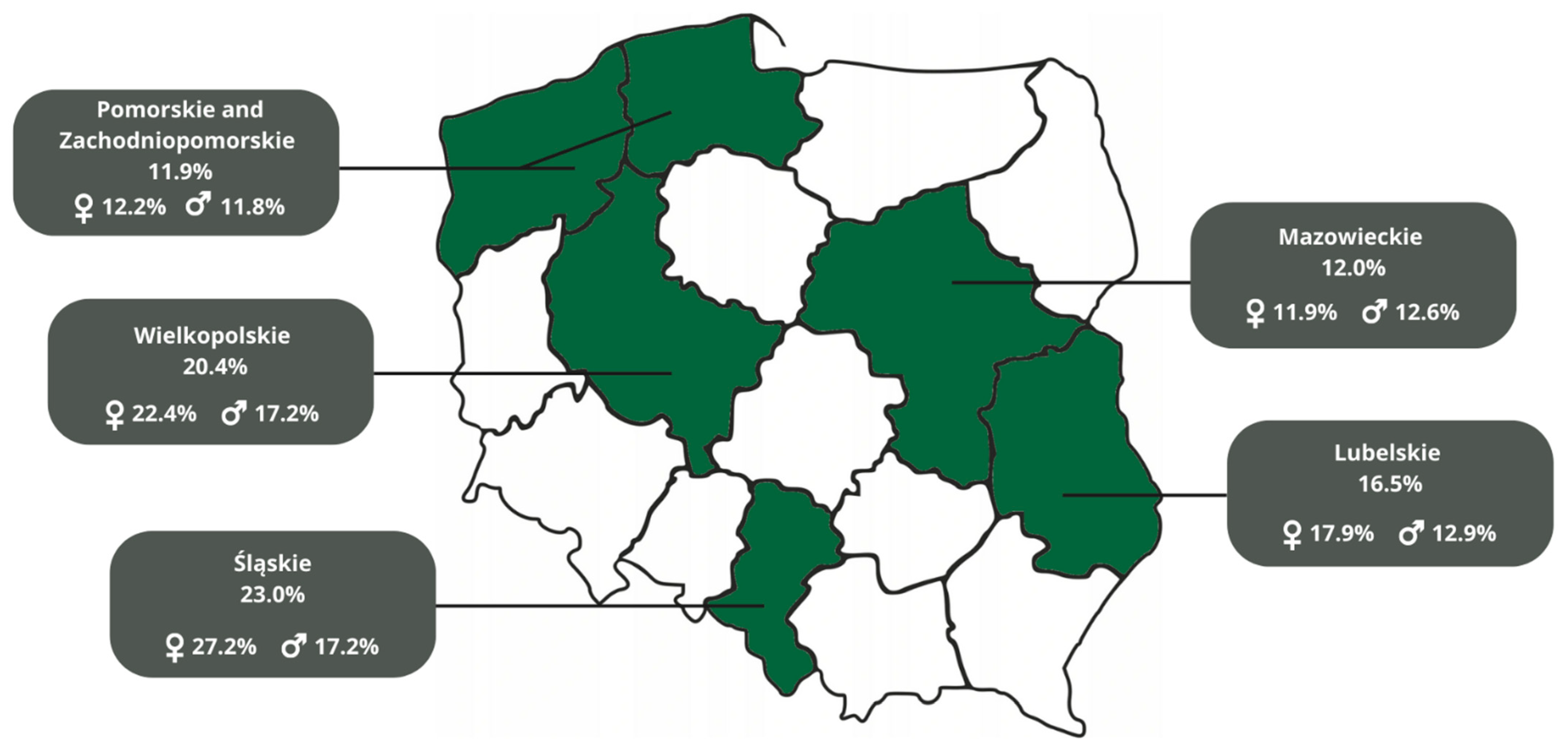
3.3. HPV Vaccination Level in Different Regions of Poland
3.4. HPV Vaccination Level Depending on Sexual Education at Schools
3.5. HPV Vaccination Level by Sexual Debut
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Implications for Policy, Practice and Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Bernard, H.-U.; Burk, R.D.; Chen, Z.; van Doorslaer, K.; zur Hausen, H.; de Villiers, E.-M. Classification of papillomaviruses (PVs) based on 189 PV types and proposal of taxonomic amendments. Virology 2010, 401, 70–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brianti, P.; De Flammineis, E.; Mercuri, S.R. Review of HPV-related diseases and cancers. New Microbiol. 2017, 40, 80–85. [Google Scholar] [PubMed]
- De Sanjosé, S.; Diaz, M.; Castellsagué, X.; Clifford, G.; Bruni, L.; Muñoz, N.; Bosch, F.X. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: A meta-analysis. Lancet Infect. Dis. 2007, 7, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.V. The human papillomavirus replication cycle, and its links to cancer progression: A comprehensive review. Clin. Sci. 2017, 131, 2201–2221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Couto, E.; Sæterdal, I.; Juvet, L.K.; Klemp, M. HPV catch-up vaccination of young women: A systematic review and meta-analysis. BMC Public Health 2014, 14, 867. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moscicki, A.B.; Palefsky, J.M. HPV in men: An update. J. Low. Genit. Tract Dis. 2011, 15, 231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunne, E.F.; Nielson, C.M.; Stone, K.M.; Markowitz, L.E.; Giuliano, A.R. Prevalence of HPV infection among men: A systematic review of the literature. J. Infect. Dis. 2006, 194, 1044–1057. [Google Scholar] [CrossRef] [PubMed]
- Rocha, M.G.D.L.; Faria, F.L.; Gonçalves, L.; Souza, M.D.C.M.; Fernandes, P.A.; Fernandes, A.P. Prevalence of DNA-HPV in male sexual partners of HPV-infected women and concordance of viral types in infected couples. PLoS ONE 2012, 7, e40988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Factsheet about Human Papillomavirus. 2018. Available online: https://www.ecdc.europa.eu/en/human-papillomavirus/factsheet (accessed on 4 July 2022).
- World Health Organization. Comprehensive Cervical Cancer Control: A Guide to Essential Practice, 2nd ed.; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.who.int/iris/handle/10665/144785 (accessed on 15 June 2022).
- Polish Ministry of Health. Cervical Cancer Prevention Programme (Cytology). 2018. Available online: https://www.gov.pl/web/zdrowie/program-profilaktyki-raka-szyjki-macicy-cytologia- (accessed on 24 November 2022).
- PATH. Global HPV Vaccine Introduction Overview. 2022. Available online: Path.org/resources/global-hpv-vaccine-introduction-overview/ (accessed on 20 June 2022).
- Pikala, M.; Burzyńska, M.; Maniecka-Bryła, I. Years of life lost due to cervical Cancer in Poland in 2000 to 2015. Int. J. Environ. Res. Public Health 2019, 16, 1545. [Google Scholar] [CrossRef] [PubMed]
- Nguyen-Huu, N.H.; Thilly, N.; Derrough, T.; Sdona, E.; Claudot, F.; Pulcini, C.; Agrinier, N.; HPV Policy Working Group. Human papillomavirus vaccination coverage, policies, and practical implementation across Europe. Vaccine 2020, 38, 1315–1331. [Google Scholar] [CrossRef] [PubMed]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M.; Ali, H.; Boily, M.C.; Baldo, V.; Brassard, P.; Brotherton, J.M.; Callander, D.; et al. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agency for Health Technology Assessment and Tariffication. Recommendation No. 54/2021 of 18 May 2021 of the President of the Agency for Health Technology Assessment and Tariffication on the Reimbursement of Cervarix, a Vaccine against the Human Papillomavirus [Types 16 and 18] in the Indication: Prophylaxis of Precancerous Lesions of the Genital Organs and Anus (Cervix, Vulva, Vagina and Anus), and Cervical and Anal Cancers Caused by Certain Oncogenic Types of Human Papillomavirus (HPV) in People Aged 9 Years and over. 2021. Available online: https://bipold.aotm.gov.pl/assets/files/zlecenia_mz/2021/041/REK/2021_05_18_BP_rekomendacja_nr_54_2021_REOPTR.pdf (accessed on 20 June 2022).
- Polish Ministry of Health. Information from the Minister of Health on the Inclusion of a Vaccine against the Human Papillomavirus (HPV) in the List of Reimbursed Drugs and Changes in the Vaccination E-Card. 2021. Available online: https://www.gov.pl/web/zdrowie/informacja-ministra-zdrowia-w-sprawie-wlaczenia-do-wykazu-refundowanych-lekow-szczepionki-przeciw-wirusowi-brodawczaka-ludzkiego-hpv-oraz-zmian-w-e-karcie-szczepien (accessed on 4 July 2022).
- Informal Polish Drug Database. Available online: https://www.gdziepolek.pl/ (accessed on 24 November 2022).
- National Institute of Public Health, National Institute of Hygiene—State Research Institute. Towns in Which Municipal Vaccination Programs against HPV Are Implemented. 2021. Available online: https://szczepienia.pzh.gov.pl/faq/gdzie-realizowane-sa-samorzadowe-programy-szczepien-przeciw-hpv/ (accessed on 25 June 2022).
- Polish Ministry of Education, Ośrodek Rozwoju Edukacji. The Core Curriculum for General Education with Commentary. Primary School Family Life Education. Available online: https://www.ore.edu.pl/wp-content/uploads/2017/05/wychowanie-do-zycia-w-rodzinie.-pp-z-komentarzem.-szkola-podstawowa-1.pdf (accessed on 6 July 2022).
- Smolarczyk, K.; Duszewska, A.; Drozd, S.; Majewski, S. Parents’ Knowledge and Attitude towards HPV and HPV Vaccination in Poland. Vaccines 2022, 10, 228. [Google Scholar] [CrossRef] [PubMed]
- Augustynowicz, A.; Bojar, I.; Borowska, M.; Bobinski, K.; Czerw, A. Self-government HPV vaccination programmes in Poland, 2009–2016. Ann. Agric. Environ. Med. 2020, 27, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Ganczak, M.; Owsianka, B.; Korzeń, M. Factors that Predict Parental Willingness to Have Their Children Vaccinated against HPV in a Country with Low HPV Vaccination Coverage. Int. J. Environ. Res. Public Health 2018, 15, 645. [Google Scholar] [CrossRef]
| HPV Vaccination Status * | |
|---|---|
| Vaccinated | 432 (16.0%) |
| Unvaccinated | 602 (22.3%) |
| Do not know | 1571 (58.2%) |
| Age1 | |
| 18 | 2021 (74.8%) |
| 19 | 515 (19.1%) |
| Over 19 | 159 (5.9%) |
| Gender2 | |
| Woman | 1572 (58.2%) |
| Man | 1096 (40.6%) |
| Other | 20 (0.8%) |
| Residence 3 | |
| City over 100,000 | 883 (32.7%) |
| City under 100,000 | 808 (29.9%) |
| Rural area | 991 (36.7%) |
| Region of Poland 4 | |
| Śląskie | 518 (19.2%) |
| Mazowieckie | 737 (27.3%) |
| Wielkopolskie | 653 (24.2%) |
| Lubelskie | 259 (9.6%) |
| Zachodniopomorskie i Pomorskie | 533 (19.7%) |
| Sexual orientation 5 | |
| Heterosexual | 2196 (86.9%) |
| Homosexual | 63 (2.5%) |
| Bi/pansexual | 201 (8.0%) |
| Asexual | 30 (1.2%) |
| Other | 37 (1.5%) |
| Sex education 6 | |
| School offers classes | 1512 (56.0%) |
| School doesn’t offer classes | 1121 (41.5%) |
| Sex education attendance 7 | |
| Attended | 1406 (52.1%) |
| Did not attend | 1236 (45.8%) |
| Sexual debut 8 | |
| Yes | 1382 (51.2%) |
| No | 1269 (47.0%) |
| Vaccinated | Unvaccinated | Do Not Know | p-Value ** | |
|---|---|---|---|---|
| Age | 0.721 | |||
| 18 | 325 (16.6%) | 428 (21.9%) | 1206 (61.6%) | |
| 19 | 77 (15.6%) | 131 (26.6%) | 285 (57.8%) | |
| Over 19 | 20 (19.6%) | 41 (27.7%) | 78 (52.7%) | |
| Gender | 0.106 | |||
| Female | 278 (18.2%) | 358 (23.4%) | 896 (58.5%) | |
| Male | 151 (14.5%) | 236 (22.6%) | 656 (62.9%) | |
| Other | 2 (11.1%) | 4 (22.2%) | 12 (66.7%) | |
| Residence | 0.005 | |||
| City over 100,000 | 169 (19.8%) | 203 (23.8%) | 481 (56.4%) | |
| City under 100,000 | 122 (15.7%) | 191 (24.6%) | 464 (59.7%) | |
| Rural areas | 139 (14.5%) | 205 (21.4%) | 614 (64.1%) | |
| Region of Poland | <0.001 | |||
| Śląskie | 117 (23.0%) | 117 (23.0%) | 275 (54.0%) | |
| Mazowieckie | 85 (12.0%) | 171 (24.2%) | 451 (63.8%) | |
| Wielkopolskie | 128 (20.4%) | 131 (20.9%) | 368 (58.7%) | |
| Lubelskie | 41 (16.5%) | 60 (24.1%) | 148 (59.4%) | |
| Pomorskie i Zachodniopomorskie | 61 (11.9%) | 123 (24.0%) | 329 (64.1%) | |
| Sex education | 0.018 | |||
| School offers classes | 256 (17.4%) | 318 (21.6%) | 897 (61.0%) | |
| School does not offer classes | 162 (15.0%) | 282 (26.2%) | 634 (58.8%) | |
| Sex education attendance | 0.761 | |||
| Attended | 219 (16.0%) | 327 (32.9%) | 821 (60.1%) | |
| Did not attend | 198 (16.6%) | 271 (22.8%) | 722 (60.6%) | |
| Sexual debut | <0.001 | |||
| Have had | 268 (19.8%) | 362 (26.8%) | 721 (52.4%) | |
| Have not had | 163 (13.2%) | 234 (18.9%) | 839 (67.9%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drejza, M.; Rylewicz, K.; Lewandowska, M.; Gross-Tyrkin, K.; Łopiński, G.; Barwińska, J.; Majcherek, E.; Szymuś, K.; Klein, P.; Plagens-Rotman, K.; et al. HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study. Healthcare 2022, 10, 2385. https://doi.org/10.3390/healthcare10122385
Drejza M, Rylewicz K, Lewandowska M, Gross-Tyrkin K, Łopiński G, Barwińska J, Majcherek E, Szymuś K, Klein P, Plagens-Rotman K, et al. HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study. Healthcare. 2022; 10(12):2385. https://doi.org/10.3390/healthcare10122385
Chicago/Turabian StyleDrejza, Michalina, Katarzyna Rylewicz, Maria Lewandowska, Katarzyna Gross-Tyrkin, Grzegorz Łopiński, Joanna Barwińska, Ewa Majcherek, Klaudia Szymuś, Patrycja Klein, Katarzyna Plagens-Rotman, and et al. 2022. "HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study" Healthcare 10, no. 12: 2385. https://doi.org/10.3390/healthcare10122385
APA StyleDrejza, M., Rylewicz, K., Lewandowska, M., Gross-Tyrkin, K., Łopiński, G., Barwińska, J., Majcherek, E., Szymuś, K., Klein, P., Plagens-Rotman, K., Pisarska-Krawczyk, M., Kędzia, W., & Jarząbek-Bielecka, G. (2022). HPV Vaccination among Polish Adolescents—Results from POLKA 18 Study. Healthcare, 10(12), 2385. https://doi.org/10.3390/healthcare10122385








