Responses of Bilevel Ventilators to Unintentional Leak: A Bench Study
Abstract
:1. Introduction
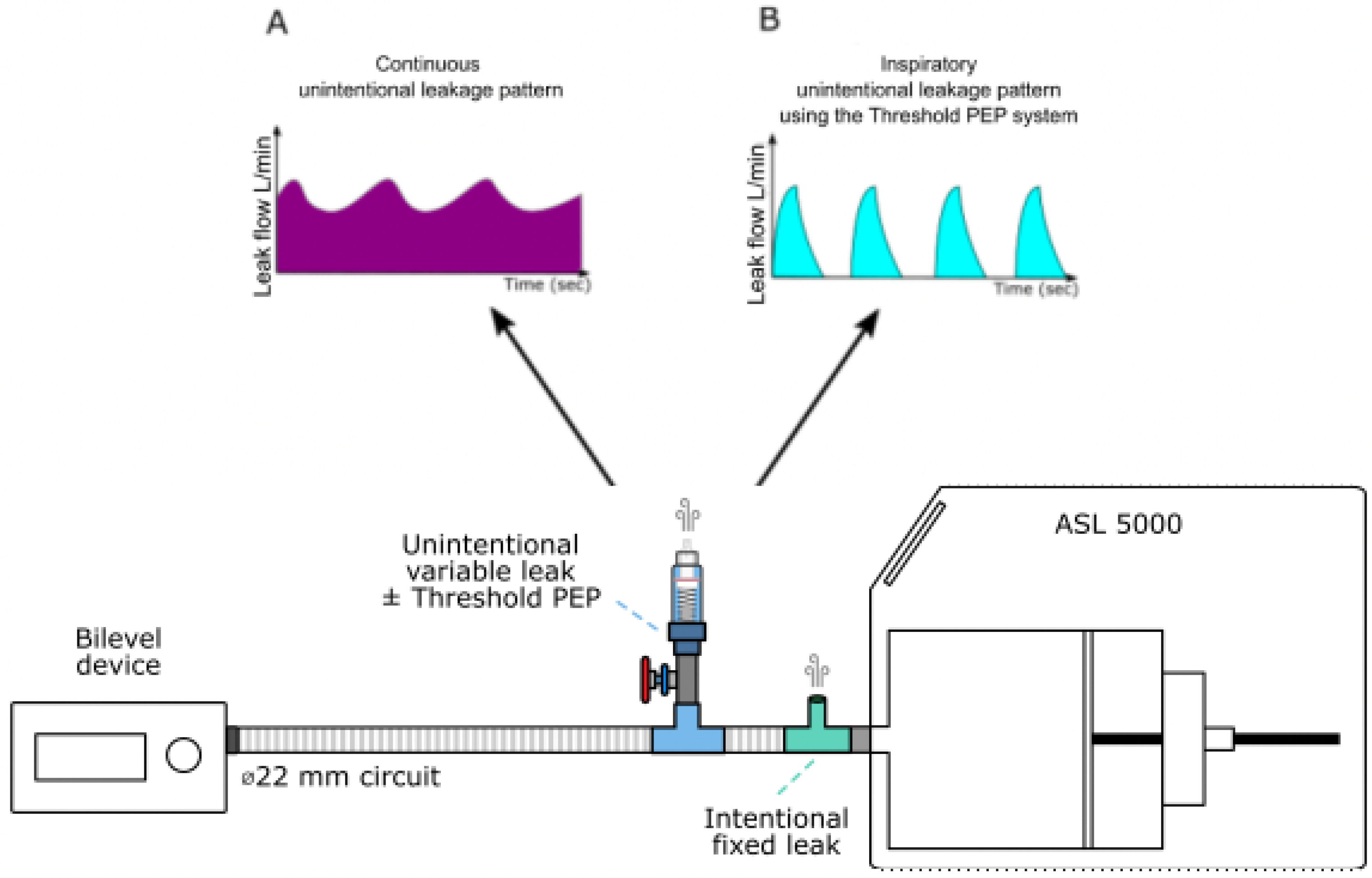
2. Materials and Methods
2.1. Simulated Airway Obstruction
2.2. Intentional and Unintentional Leaks
2.3. Ventilator Settings
2.4. Ventilator Performance and Synchrony Indicators
- (1)
- Triggering delay (or Time to trigger) in ms, by measuring the time lag between the onset of the simulated effort and the onset of the pressure support;
- (2)
- Work of breathing (or WOB) in J/s, computed as the integral of the product of the muscular pressure and the flow during the inspiratory phase and reported to the tidal volume;
- (3)
- Pressure rise time in ms, defined as the time required to reach the set pressure during the inspiratory phase;
- (4)
- Delivered inspiratory pressure in cmH2O, defined as the peak pressure reached during the inspiratory pressurization phase;
- (5)
- Tidal volume in ml, defined as the difference between the maximal volume delivered within the current cycle to the mechanical lung and its residual volume;
- (6)
- Cycling delay in ms, by measuring the time lag between the expiratory pressure release and the end of the patient’s neural inspiration.
- Ineffective efforts (IE) characterized by an inspiratory effort not assisted by the ventilator. It can be identified as a drop of airway pressure associated with an increase or decrease of airflow (if occurring during expiratory or inspiratory phase, respectively).
- Auto-triggering (Auto), characterized by the presence of mechanical cycles unrelated to the patient’s spontaneous breathing.
2.5. Experimental Protocol
2.6. Statistical Analysis
3. Results
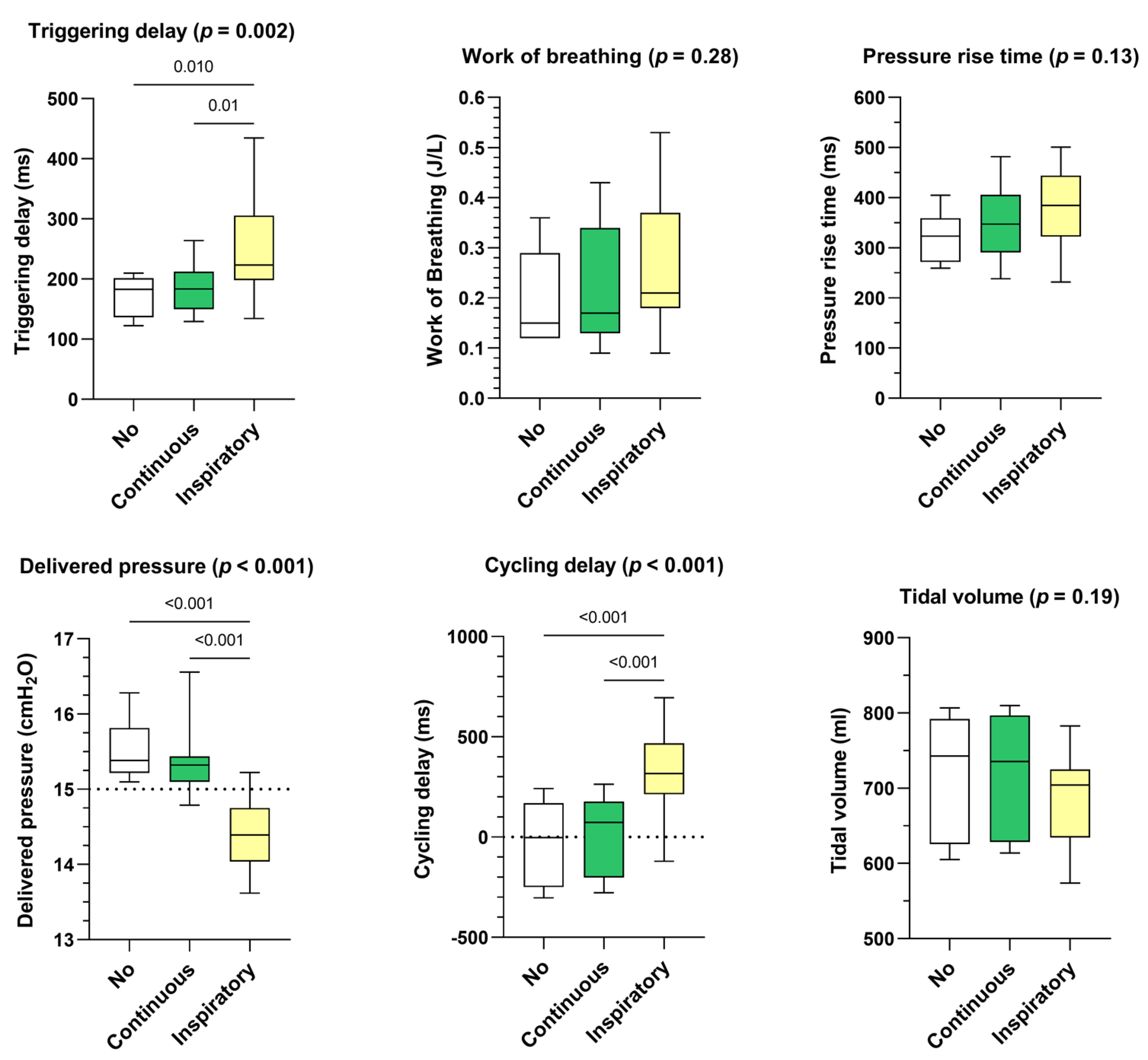
- Influence of leakage rate
- Influence of leak pattern
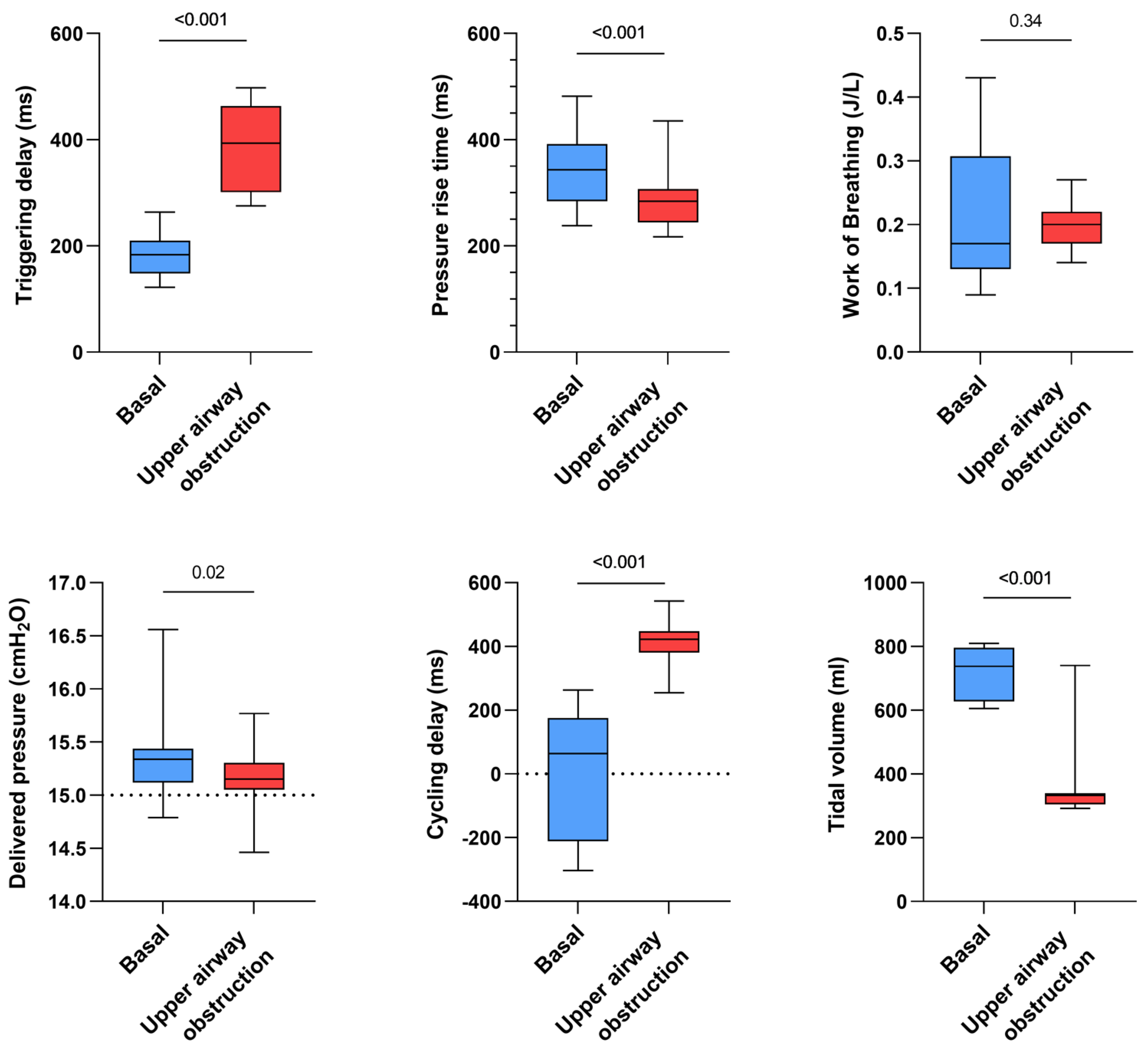
- Influence of simulated upper airway obstruction
- Influence of respiratory models
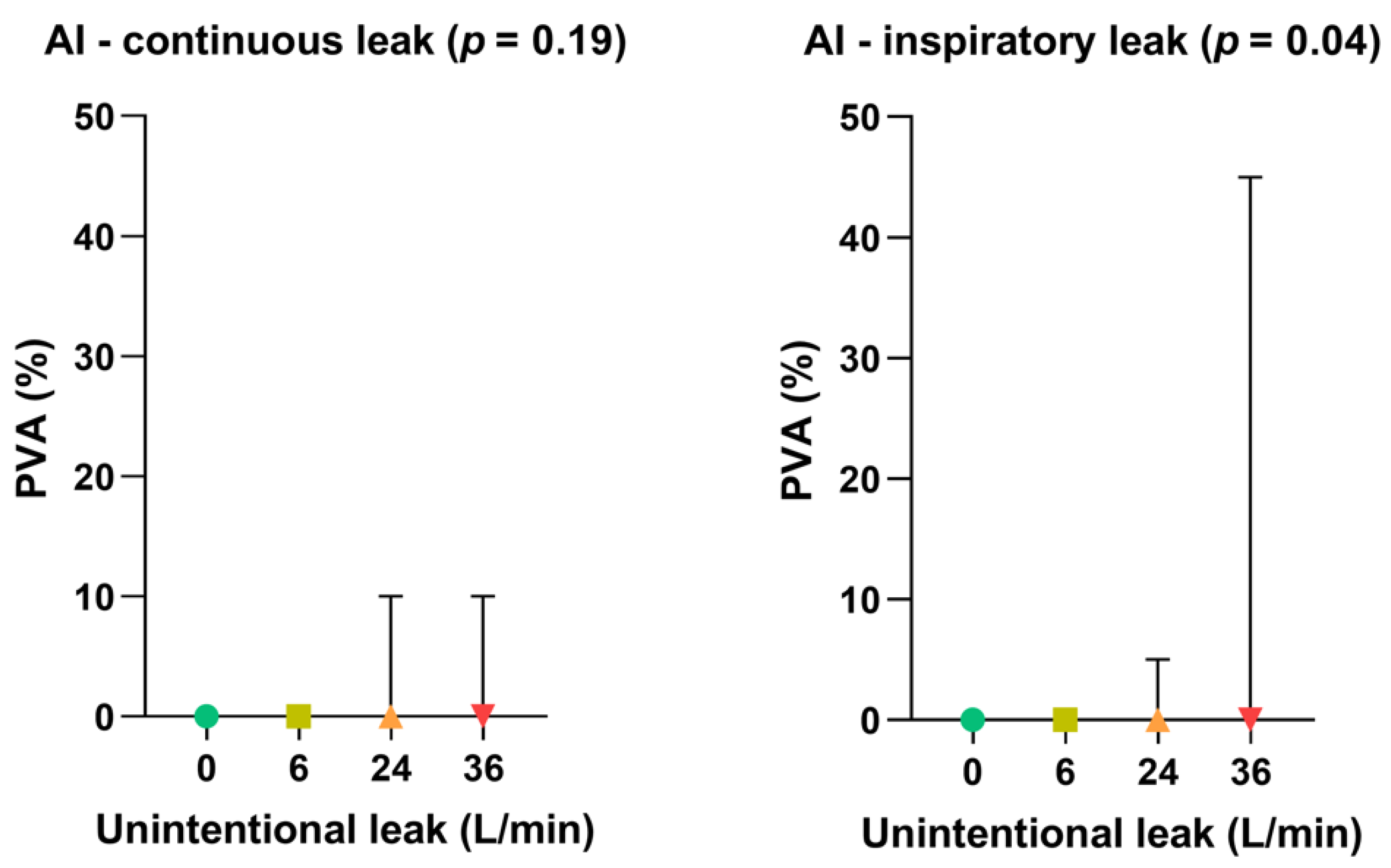
- Impact of leak patterns on asynchrony index
- Difference between ventilators
4. Discussion
- (i)
- Leak compensation algorithms probably calculate the mean unintentional leakage rate. if the leakage appears only during the inspiratory phase, thus the mean leakage rate is likely to be underestimated assuming a situation of continuous leakage (expiratory and inspiratory leak). In these conditions, the device may interpret the unintentional leak as patient flow, which leads to cycling delays since the patient flow drop is not correctly distinguished from the leak flow;
- (ii)
- On the other hand, during exhalation, the unintentional leak is probably overestimated since the averaging considers the inspiration additional leak. This may lead to a decreased sensitivity of the inspiratory trigger thresholds.
- (iii)
- Last, during the conception phase, ventilator devices are designed and tested using calibrated leak port only, providing continuous and rather stable leakage rates.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Simonds, A.K. Home Mechanical Ventilation: An Overview. Ann. Am. Thorac. Soc. 2016, 13, 2035–2044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cantero, C.; Adler, D.; Pasquina, P.; Uldry, C.; Egger, B.; Prella, M.; Janssens, J.P. Long Term Noninvasive Ventilation in the Geneva Lake Area: Indications, Prevalence and Modalities. Available online: http://www.sciencedirect.com/science/article/pii/S0012369220305511 (accessed on 1 September 2022).
- Sancho, J.; Servera, E.; Morelot-Panzini, C.; Salachas, F.; Similowski, T.; Gonzalez-Bermejo, J. Non-invasive ventilation effectiveness and the effect of ventilatory mode on survival in ALS patients. Amyotroph. Lateral Scler. Front. Degener. 2013, 15, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Masa, J.F.; Mokhlesi, B.; Benítez, I.; de Terreros, F.J.G.; Sánchez-Quiroga, M.Á.; Romero, A.; Bengoa, M. Long-term clinical effectiveness of continuous positive airway pressure therapy versus non-invasive ventilation therapy in patients with obesity hypoventila-tion syndrome: A multicentre, open-label, randomised controlled trial. Lancet 2019, 393, 1721–1732. [Google Scholar] [CrossRef] [PubMed]
- Murphy, P.B.; Rehal, S.; Arbane, G.; Bourke, S.; Calverley, P.M.; Crook, A.M.; Hart, N. Effect of Home Noninvasive Ventilation with Oxygen Therapy vs Oxygen Therapy Alone on Hospital Readmission or Death After an Acute COPD Exacerbation: A Ran-domized Clinical Trial. JAMA 2017, 317, 2177–2186. [Google Scholar] [CrossRef] [PubMed]
- Köhnlein, T.; Windisch, W.; Köhler, D.; Drabik, A.; Geiseler, J.; Hartl, S.; Karg, O.; Laier-Groeneveld, G.; Nava, S.; Schönhofer, B.; et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: A prospective, multicentre, randomised, controlled clinical trial. Lancet Respir. Med. 2014, 2, 698–705. [Google Scholar] [CrossRef]
- Fanfulla, F.; Taurino, A.E.; Lupo, N.D.; Trentin, R.; D’Ambrosio, C.; Nava, S. Effect of sleep on patient/ventilator asynchrony in patients undergoing chronic non-invasive mechanical ventilation. Respir. Med. 2007, 101, 1702–1707. [Google Scholar] [CrossRef] [Green Version]
- Crescimanno, G.; Canino, M.; Marrone, O. Asynchronies and sleep disruption in neuromuscular patients under home noninva-sive ventilation. Respir. Med. 2012, 106, 1478–1485. [Google Scholar] [CrossRef] [Green Version]
- Teschler, H.; Stampa, J.; Ragette, R.; Konietzko, N.; Berthon-Jones, M. Effect of mouth leak on effectiveness of nasal bilevel venti-latory assistance and sleep architecture. Eur. Respir. J. 1999, 14, 1251–1257. [Google Scholar] [CrossRef] [Green Version]
- Rabec, C.; Rodenstein, D.; Leger, P.; Rouault, S.; Perrin, C.; Gonzalez-Bermejo, J. Ventilator modes and settings during non-invasive ventilation: Effects on respiratory events and implications for their identification. Thorax 2010, 66, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Meyer, T.J.; Pressman, M.R.; Benditt, J.; McCool, F.D.; Millman, R.P.; Natarajan, R.; Hill, N.S. Air leaking through the mouth during noc-turnal nasal ventilation: Effect on sleep quality. Sleep 1997, 20, 561–569. [Google Scholar] [CrossRef]
- Gonzalez-Bermejo, J.; Janssens, J.-P.; Rabec, C.; Perrin, C.; Lofaso, F.; Langevin, B.; Carlucci, A.; Luján, M. Framework for patient-ventilator asynchrony during long-term non-invasive ventilation. Thorax 2019, 74, 715–717. [Google Scholar] [CrossRef]
- Gonzalez, J.; Sharshar, T.; Hart, N.; Chadda, K.; Raphaël, J.C.; Lofaso, F. Air leaks during mechanical ventilation as a cause of per-sistent hypercapnia in neuromuscular disorders. Intensive Care Med. 2003, 29, 596–602. [Google Scholar] [CrossRef]
- Mansell, S.K.; Cutts, S.; Hackney, I.; Wood, M.J.; Hawksworth, K.; Creer, D.D.; Kilbride, C.; Mandal, S. Using domiciliary non-invasive ventilator data downloads to inform clinical decision-making to optimise ventilation delivery and patient compliance. BMJ Open Respir. Res. 2018, 5, e000238. [Google Scholar] [CrossRef] [Green Version]
- Borel, J.; Palot, A.; Patout, M. Technological advances in home non-invasive ventilation monitoring: Reliability of data and effect on patient outcomes. Respirology 2019, 24, 1143–1151. [Google Scholar] [CrossRef]
- Contal, O.; Vignaux, L.; Combescure, C.; Pepin, J.L.; Jolliet, P.; Janssens, J.P. Monitoring of noninvasive ventilation by built-in soft-ware of home bilevel ventilators: A bench study. Chest 2012, 141, 469–476. [Google Scholar] [CrossRef] [Green Version]
- Ueno, Y.; Nakanishi, N.; Oto, J.; Imanaka, H.; Nishimura, M. A Bench Study of the Effects of Leak on Ventilator Performance During Noninvasive Ventilation. Respir. Care 2011, 56, 1758–1764. [Google Scholar] [CrossRef] [Green Version]
- Rabec, C.; Georges, M.; Kabeya, N.K.; Baudouin, N.; Massin, F.; Reybet-Degat, O.; Camus, P. Evaluating noninvasive ventilation using a monitoring system coupled to a ventilator: A bench-to-bedside study. Eur. Respir. J. 2009, 34, 902–913. [Google Scholar] [CrossRef] [Green Version]
- Zhu, K.; Rabec, C.; Gonzalez-Bermejo, J.; Hardy, S.; Aouf, S.; Escourrou, P.; Roisman, G. Combined effects of leaks, respiratory system properties and upper airway patency on the performance of home ventilators: A bench study. BMC Pulm. Med. 2017, 17, 145. [Google Scholar] [CrossRef] [Green Version]
- Lebret, M.; Arnol, N.; Martinot, J.-B.; Lambert, L.; Tamisier, R.; Pepin, J.-L.; Borel, J.-C. Determinants of Unintentional Leaks During CPAP Treatment in OSA. Chest 2018, 153, 834–842. [Google Scholar] [CrossRef]
- Fresnel, E.; Muir, J.-F.; Letellier, C. Realistic human muscle pressure for driving a mechanical lung. EPJ Nonlinear Biomed. Phys. 2014, 2, 7. [Google Scholar] [CrossRef]
- Olivieri, C.; Costa, R.; Conti, G.; Navalesi, P. Bench studies evaluating devices for non-invasive ventilation: Critical analysis and future perspectives. Intensiv. Care Med. 2011, 38, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Carteaux, G.; Lyazidi, A.; Cordoba-Izquierdo, A.; Vignaux, L.; Jolliet, P.; Thille, A.W.; Brochard, L. Patient-ventilator asynchrony during noninvasive ventilation: A bench and clinical study. Chest 2012, 142, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.F.; Sforza, E.; Janssens, J.P. Respiratory patterns during sleep in obesity-hypoventilation patients treated with nocturnal pressure support: A preliminary report. Chest 2007, 131, 1090–1099. [Google Scholar] [CrossRef] [PubMed]
- Goutorbe, P.; Daranda, E.; Asencio, Y.; Esnault, P.; Prunet, B.; Bordes, J.; Meaudre, E. Leaks can dramatically decrease FiO2 on home venti-lators: A bench study. BMC Res Notes 2013, 6, 282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebret, M.; Martinot, J.B.; Arnol, N.; Zerillo, D.; Tamisier, R.; Pepin, J.L.; Borel, J.C. Factors Contributing to Unintentional Leak During CPAP Treatment: A Systematic Review. Chest 2017, 151, 707–719. [Google Scholar] [CrossRef]
- Genta, P.R.; Kaminska, M.; Edwards, B.A.; Ebben, M.R.; Krieger, A.C.; Tamisier, R.; Strollo, P. The Importance of Mask Selection on Con-tinuous Positive Airway Pressure Outcomes for Obstructive Sleep Apnea. An Official American Thoracic Society Workshop Report. Ann. ATS 2020, 17, 1177–1185. [Google Scholar] [CrossRef]
- Pierucci, P.; Portacci, A.; Carpagnano, G.E.; Banfi, P.; Crimi, C.; Misseri, G.; Gregoretti, C. The right interface for the right patient in noninva-sive ventilation: A systematic review. Expert Rev. Respir. Med. 2022, 16, 931–944. [Google Scholar] [CrossRef]
- Lebret, M.; Jaffuel, D.; Suehs, C.M.; Mallet, J.P.; Lambert, L.; Rotty, M.C.; Borel, J.C. Feasibility of Type 3 Polygraphy for Evaluating Leak Determinants in CPAP-Treated OSA Patients: A Step Toward Personalized Leak Management. Chest 2020, 158, 2165–2171. [Google Scholar] [CrossRef]
- Rowland, S.; Aiyappan, V.; Hennessy, C.; Catcheside, P.; Chai-Coezter, C.L.; McEvoy, D.; Antic, N.A. Comparing the Efficacy, Mask Leak, Patient Adherence, and Patient Preference of Three Different CPAP Interfaces to Treat Moderate-Severe Obstructive Sleep Apnea. J. Clin. Sleep Med. 2018, 14, 101–108. [Google Scholar] [CrossRef]
- Valentin, A.; Subramanian, S.; Quan, S.F.; Berry, R.B.; Parthasarathy, S. Air Leak is Associated with Poor Adherence to Autopap Therapy. Sleep 2011, 34, 801–806. [Google Scholar] [CrossRef]
- Schwab, R.J.; Badr, S.M.; Epstein, L.J.; Gay, P.C.; Gozal, D.; Kohler, M.; Weaver, T.E. An Official American Thoracic Society Statement: Con-tinuous Positive Airway Pressure Adherence Tracking Systems. The Optimal Monitoring Strategies and Outcome Measures in Adults. Am. J. Respir. Crit. Care Med. 2013, 188, 613–620. [Google Scholar] [CrossRef] [Green Version]
- Jolly, G.; Razakamanantsoa, L.; Fresnel, E.; Gharsallaoui, Z.; Cuvelier, A.; Patout, M. Defining successful non-invasive ventilation initiation: Data from a real-life cohort. Respirology 2021, 26, 1067–1075. [Google Scholar] [CrossRef]
- Luján, M.; Sogo, A.; Pomares, X.; Monsó, E.; Sales, B.; Blanch, L. Effect of leak and breathing pattern on the accuracy of tidal vol-ume estimation by commercial home ventilators: A bench study. Respir Care 2013, 58, 770–777. [Google Scholar] [CrossRef] [Green Version]
- Sogo, A.; Montanyà, J.; Monsó, E.; Blanch, L.; Pomares, X.; Lujàn, M. Effect of dynamic random leaks on the monitoring accuracy of home mechanical ventilators: A bench study. BMC Pulm. Med. 2013, 13, 75. [Google Scholar] [CrossRef] [Green Version]
- Lujàn, M.; Sogo, A.; Grimau, C.; Pomares, X.; Blanch, L.; Monso, E. Influence of Dynamic Leaks in Volume-Targeted Pressure Support Noninvasive Ventilation: A Bench Study. Respir. Care 2014, 60, 191–200. [Google Scholar] [CrossRef]

| Model | Simulated Airway Obstruction (Flow Limitation) | Inspiratory Resistance (cmH2O/L.s) | Expiratory Resistance (cmH2O/L.s) | Compliance (mL/cmH2O) | P0.1 (Pmax) (cmH2O) | RR (Breaths/min) |
|---|---|---|---|---|---|---|
| OHS | no | 8 | 5 | 30 | 3 [12] | 15 |
| yes | 40 | |||||
| COPD | no | 20 | 25 | 50 | 3 [14] | 12 |
| yes | 60 | |||||
| NMD | no | 5 | 60 | 1 [5] | 20 | |
| yes | 25 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lebret, M.; Fresnel, E.; Prouvez, N.; Zhu, K.; Kerfourn, A.; Richard, J.-C.; Patout, M. Responses of Bilevel Ventilators to Unintentional Leak: A Bench Study. Healthcare 2022, 10, 2416. https://doi.org/10.3390/healthcare10122416
Lebret M, Fresnel E, Prouvez N, Zhu K, Kerfourn A, Richard J-C, Patout M. Responses of Bilevel Ventilators to Unintentional Leak: A Bench Study. Healthcare. 2022; 10(12):2416. https://doi.org/10.3390/healthcare10122416
Chicago/Turabian StyleLebret, Marius, Emeline Fresnel, Nathan Prouvez, Kaixian Zhu, Adrien Kerfourn, Jean-Christophe Richard, and Maxime Patout. 2022. "Responses of Bilevel Ventilators to Unintentional Leak: A Bench Study" Healthcare 10, no. 12: 2416. https://doi.org/10.3390/healthcare10122416
APA StyleLebret, M., Fresnel, E., Prouvez, N., Zhu, K., Kerfourn, A., Richard, J. -C., & Patout, M. (2022). Responses of Bilevel Ventilators to Unintentional Leak: A Bench Study. Healthcare, 10(12), 2416. https://doi.org/10.3390/healthcare10122416







