The Effect of a Comprehensive Corrective Exercise Program on Kyphosis Angle and Balance in Kyphotic Adolescents
Abstract
1. Introduction
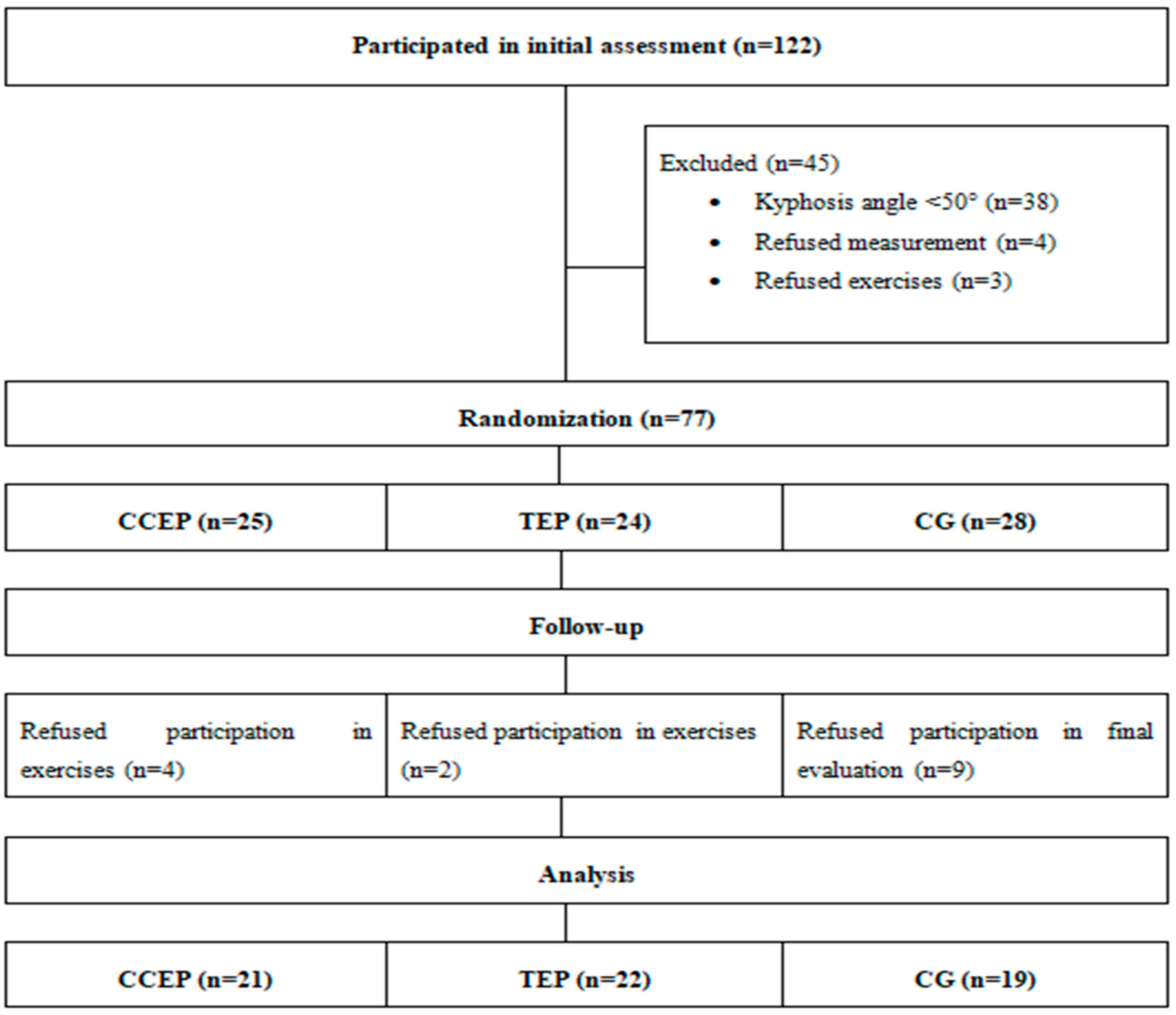
2. Materials and Methods
2.1. Participants
2.2. Outcome Measures
2.3. Intervention
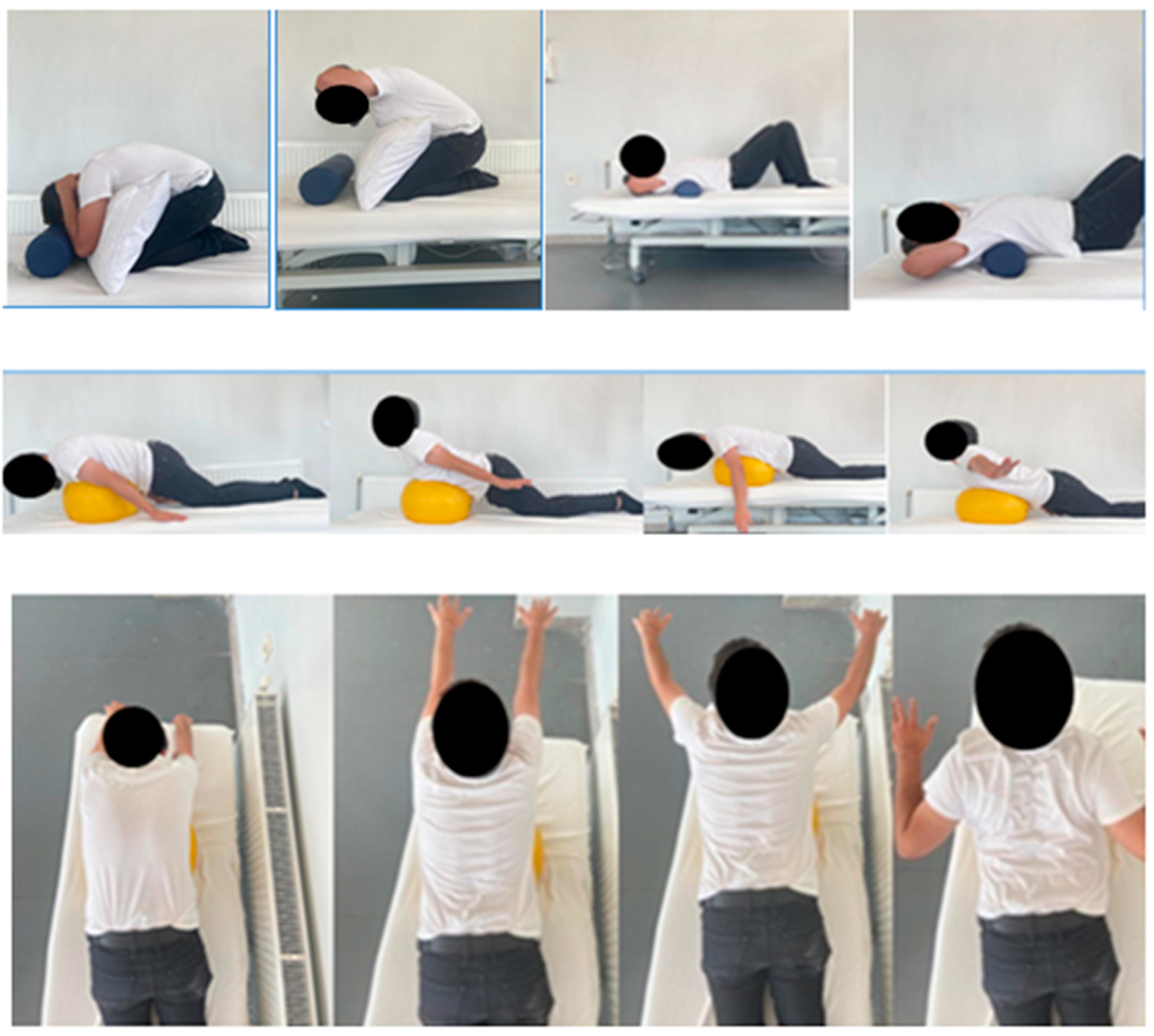
2.3.1. Comprehensive Corrective Exercise Program
2.3.2. Thoracic Exercise Program
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Exercise Schedule
| Weeks | Exercises | Exercise intensity |
| Weeks 1–2 | Stretching exercises | 30 s/3 reps |
| Self-mobilization | 1 min/2 reps | |
| Exercises | 5 × 2 | |
| Weeks 3–4 | Stretching exercises | 30 s/3 reps |
| Self-mobilization | 1 min/2 reps | |
| Exercises | 10 × 2 | |
| Weeks 5–8 | Stretching exercises | 30 s/3 reps |
| Self-mobilization | 1 min/2 reps | |
| Exercises | 10 × 3 | |
| Weeks 9–12 | Stretching exercises | 30 s/3 reps |
| Self-mobilization | 1 min/2 reps | |
| Exercises | 15 × 3 |
Appendix B. Comprehensive Corrective Exercise Program and Postural Perception Training Program
| Weeks | Comprehensive Corrective Exercise Program Plus Postural Perception Training Program (CCEP) |
| Weeks 1–4 | Chin-tuck exercises |
| Stretching neck extensor muscles | |
| Stretching pectoral muscle groups in standing and supine positions | |
| Supine bridging on a stable surface | |
| Postural perception training | |
| Weeks 5–8 | Chin-tuck exercises |
| Supine bridging with knees flexed on an unstable surface (ball) | |
| Unilateral lifting of the arms and legs in crawling position | |
| Activation of the transversus abdominus muscle and unilateral arm and leg movements in sitting position on an unstable surface | |
| Cat–camel exercise | |
| Stretching pectoral muscle groups in standing and supine positions | |
| Postural perception training | |
| Weeks 9–12 | Chin-tuck exercise |
| Supine bridging with knees extended on an unstable surface | |
| Ipsilateral/contralateral raising of arms and legs in crawling position | |
| Activation of the transversus abdominus muscle and contralateral arm and leg movements in sitting position on an unstable surface | |
| Cat–camel exercise | |
| Stretching pectoral muscle groups in standing and supine positions | |
| Postural perception training | |
| Thoracic Exercise Program (TEP) | |
| Weeks 1–4 | Thoracic extension exercise in kneeling position |
| Stretching pectoral muscle groups in standing and supine positions | |
| Self-mobilization | |
| Weeks 5–8 | T exercise in prone position |
| Y exercise in prone position | |
| W exercise in prone position | |
| I exercise in prone position | |
| Cat–camel exercise | |
| Stretching pectoral muscle groups in standing and supine positions | |
| Self-mobilization | |
| Weeks 9–12 | T exercise in prone position |
| Y exercise in prone position | |
| W exercise in prone position | |
| I exercise in prone position | |
| Cat–camel exercise | |
| Stretching pectoral muscle groups in standing and supine positions | |
| Self-mobilization |
References
- Hertling, D.K.R. Management of Common Musculoskeletal Disorders: Physical Therapy Principles and Methods; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Yakut, Y. Aksiyal İskelet. In Kas-İskelet Sistemi Kinezyolojisi, 1st ed.; Hipokrat Yayıncılık: Ankara, Turkey, 2018; pp. 317–476. [Google Scholar]
- Lizak, D.; Czarny, W.; Niewczas, M. The problem of postural defects in children and adolescents and the role of school teachers and counselors in their prevention. Sci. Rev. Phys. Cult. 2014, 4, 11–18. [Google Scholar]
- Bansal, S.; Katzman, W.B.; Giangregorio, L.M. Exercise for improving age-related hyperkyphotic posture: A Systematic Review. Arch. Phys. Med. Rehabil. 2014, 95, 129–140. [Google Scholar] [CrossRef]
- Brzęk, A.; Dworrak, T.; Strauss, M.; Gomar, F.S.; Sabbah, I.; Dworrak, B.; Leischik, R. The weight of pupils’ schoolbags in early school age and its influence on body posture. BMC Musculoskelet Disord. 2017, 18, 117. [Google Scholar] [CrossRef] [PubMed]
- Feng, Q.; Wang, M.; Zhang, Y.; Zhou, Y. The effect of a corrective functional exercise program on postural thoracic kyphosis in teenagers: A randomized controlled trial. Clin. Rehabil. 2018, 32, 48–56. [Google Scholar] [CrossRef]
- Liu, S.; Diebo, B.G.; Henry, J.K.; Smith, J.S.; Hostin, R.; Cunningham, M.E.; Mundis, G.; Ames, C.P.; Burton, D.; Bess, S.; et al. The benefit of nonoperative treatment for adult spinal deformity: Identifying predictors for reaching a minimal clinically important difference. Spine J. 2016, 16, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Kolarova, M.; Kutiš, P.; Rusnak, R.; Hrčková, Z.; Hudáková, Z.; Lysá, L.; Luliak, M.; Babel’a, R. Analysis of body segments and postural state in school children. Neuro Endocrinol. Lett. 2019, 40, 17–23. [Google Scholar] [PubMed]
- Mitova, S. Frequency and prevalence of postural disorders and spinal deformities in children of primary school age. Res. Kinesiol. 2015, 43, 21–24. [Google Scholar]
- Kamaci, S.; Yucekul, A.; Demirkiran, G.; Berktas, M.; Yazici, M. The evolution of sagittal spinal alignment in sitting position during childhood. Spine (Phila. Pa. 1976) 2015, 40, 787–793. [Google Scholar] [CrossRef]
- Nikolova, E.; Lekina, D. Complex methodology for the treatment of children with spinal curvatures of school age. In Proceedings: Scientific Conference with International Participation “Physical Education and Sport in the Educational System”; Southwest University Neofit: Blagoevgrad, Bulgaria, 2003; pp. 236–243. [Google Scholar]
- Tarasi, Z.; Rajabi, R.; Minoonejad, H.; Shahrbanian, S. The Effect of spine strengthening exercises and posture training on functional thoracic hyper kyphosis in young individuals. J. Adv. Med. Biomed. Res. 2019, 27, 23–31. [Google Scholar] [CrossRef]
- Kratenová, J.; Zejglicová, K.; Malý, M.; Filipová, V. Prevalence and risk factors of poor posture in school children in the Czech Republic. J. Sch. Health 2007, 77, 131–137. [Google Scholar] [CrossRef]
- Gh, M.E.; Alilou, A.; Ghafurinia, S.; Fereydounnia, S. Prevalence of faulty posture in children and youth from a rural region in Iran. Biomed. Hum. Kinet. 2012, 4, 121–126. [Google Scholar] [CrossRef]
- Dolphens, M.; Vansteelandt, S.; Cagnie, B.; Vleeming, A.; Nijs, J.; Vanderstraeten, G.; Danneels, L. Multivariable modeling of factors associated with spinal pain in young adolescence. Eur. Spine J. 2016, 25, 2809–2821. [Google Scholar] [CrossRef] [PubMed]
- Edmondston, S.J.; Chan, H.Y.; Ngai, G.C.W.; Warren, M.L.R.; Williams, J.M.; Glennon, S.; Netto, K. Postural neck pain: An investigation of habitual sitting posture, perception of ‘good’ posture and cervicothoracic kinaesthesia. Man. Ther. 2007, 12, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Bomen, B.B.; Kulkarni, S. The relationship between addiction to smartphone usage and protracted shoulders, forward head posture and thoracic kyphosis in college students. Int. J. Health Sci. Res. 2022, 12, 220–226. [Google Scholar] [CrossRef]
- Katzman, W.B.; Vittinghoff, E.; Kado, D.M.; Schafer, A.L.; Wong, S.S.; Gladin, A.; Lane, N.E. Study of hyperkyphosis, exercise and function (SHEAF) protocol of a randomized controlled trial of multimodal spine-strengthening exercise in older adults with hyperkyphosis. Phys. Ther. 2016, 96, 371–381. [Google Scholar] [CrossRef]
- Katzman, W.B.; Vittinghoff, E.; Lin, F.; Schafer, A.; Long, R.K.; Wong, S.; Gladin, A.; Fan, B.; Allaire, B.; Kado, D.M.; et al. Targeted spine strengthening exercise and posture training program to reduce hyperkyphosis in older adults: Results from the study of hyperkyphosis, exercise, and function (SHEAF) randomized controlled trial. Osteoporos. Int. 2017, 28, 2831–2841. [Google Scholar] [CrossRef]
- Katzman, W.B.; Parimi, N.; Gladin, A.; Poltavskiy, E.A.; Schafer, A.L.; Long, R.K.; Fan, B.; Wong, S.S.; Lane, N.E. Sex differences in response to targeted kyphosis specific exercise and posture training in community-dwelling older adults: A randomized controlled trial. BMC Musculoskelet. Disord. 2017, 18, 509. [Google Scholar] [CrossRef]
- Greig, A.M.; Bennell, K.L.; Briggs, A.M.; Hodges, P.W. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man. Ther. 2008, 13, 249–257. [Google Scholar] [CrossRef]
- Bennell, K.; Khan, K.; McKay, H. The role of physiotherapy in the prevention and treatment of osteoporosis. Man. Ther. 2000, 5, 198–213. [Google Scholar] [CrossRef]
- Briggs, A.M.; Wrigley, T.V.; Tully, E.A.; Adams, P.E.; Greig, A.M.; Bennell, K.L. Radiographic measures of thoracic kyphosis in osteoporosis: Cobb and vertebral centroid angles. Skeletal Radiol. 2007, 36, 761–767. [Google Scholar] [CrossRef]
- Kamali, F.; Shirazi, S.A.; Ebrahimi, S.; Mirshamsi, M.; Ghanbari, A. Comparison of manual therapy and exercise therapy for postural hyperkyphosis: A randomized clinical trial. Physiother. Theory Pract. 2016, 32, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Katzman, W.B.; Parimi, N.; Gladin, A.; Wong, S.; Lane, N.E. Long-Term efficacy of treatment effects after a kyphosis exercise and posture training intervention in older community-dwelling adults: A Cohort Study. J. Geriatr. Phys. Ther. 2021, 44, 127–138. [Google Scholar] [CrossRef]
- Peterson Kendall, F.; McCreary, K.E.; Provance, G.P. Function: With Posture and Pain; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
- Park, S.J.; Kim, S.H.; Kim, S.H. Effects of thoracic mobilization and extension exercise on thoracic alignment and shoulder function in patients with subacromial impingement syndrome: A randomized controlled pilot study. Healthcare 2020, 8, 316. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Hwang, U.; Ahn, S.; Kim, J.; Kwon, O. Effects of manual therapy and mechanical massage on spinal alignment, extension range of motion, back extensor electromyographic activity, and thoracic extension strength in individuals with thoracic hyperkyphosis: A Randomized Controlled Trial. Evid.-Based Complement. Altern. Med. 2020, 2020, 6526935. [Google Scholar] [CrossRef]
- Hrysomallıs, C.; Goodman, C. A review of resistance exercise and posture realignment. J. Strength Cond. Res. 2001, 15, 385–390. [Google Scholar] [PubMed]
- Seidi, F.; Rajabi, R.; Ebrahimi, I.; Alizadeh, M.H.; Minoonejad, H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. J. Back Musculoskelet. Rehabil. 2014, 27, 7–16. [Google Scholar] [CrossRef]
- Naderi, A.; Rezvani, M.H.; Shaabani, F.; Bagheri, S. Effect of kyphosis exercises on physical function, postural control and quality of life in elderly men with hyperkyphosis. Salmand 2019, 13, 464–479. [Google Scholar] [CrossRef]
- Singla, D.; Veqar, Z. Association Between Forward Head, Rounded Shoulders, and Increased Thoracic Kyphosis: A Review of the Literature. J. Chiropr. Med. 2017, 16, 220–229. [Google Scholar] [CrossRef]
- McDaniels-Davidson, C.; Davis, A.; Wing, D.; Macera, C.; Lindsay, S.P.; Schousboe, J.T.; Nichols, J.F.; Kado, D.M. Kyphosis and incident falls among community-dwelling older adults. Osteoporos. Int. 2018, 29, 163–169. [Google Scholar] [CrossRef]
- Tominaga, R.; Fukuma, S.; Yamazaki, S.; Sekiguchi, M.; Otani, K.; Kikuchi, S.-I.; Sasaki, S.; Kobayashi, S.; Fukuhara, S.; Konno, S.-I. Relationship between kyphotic posture and falls in community-dwelling men and women. Spine.. 2016, 41, 1232–1238. [Google Scholar] [CrossRef]
- Katzman, W.B.; Vittinghoff, E.; Kado, D.M.; Lane, N.E.; Ensrud, K.E.; Shipp, K. Thoracic kyphosis and rate of incident vertebral fractures: The Fracture Intervention Trial. Osteoporos. Int. 2016, 27, 899–903. [Google Scholar] [CrossRef]
- Katzman, W.B.; Harrison, S.L.; Fink, H.A.; Marshall, L.M.; Orwoll, E.; Barrett, C.; Elizabeth, C.; Peggy, M.; Kado, D.M. Physical Function in Older Men With Hyperkyphosis. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 70, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Katzman, W.; Cawthon, P.; Hicks, G.E.; Vittinghoff, E.; Shepherd, J.; Cauley, J.A.; Harris, T.; Simonsick, E.M.; Strotmeyer, E.; Womack, C.; et al. Association of Spinal Muscle Composition and Prevalence of Hyperkyphosis in Healthy Community-Dwelling Older Men and Women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2012, 67, 191–195. [Google Scholar] [CrossRef]
- Jang, H.; Kim, M.; Kim, S. Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis. J. Phys. Ther. Sci. 2015, 27, 1161–1164. [Google Scholar] [CrossRef]
- Yazıcı, A.G.; Mohammadı, M. The effect of corrective exercises on the thoracic kyphosis and lumbar lordosis of boy students. Turkish J. Sport Exerc. 2017, 19, 177–181. [Google Scholar] [CrossRef]
- Bayram, C.; Britt, H.; Fahridin, S. Adolescent attendances in general practice. Aust. Fam. Physician. 2007, 36, 586–587. [Google Scholar] [PubMed]
- Henschke, N.; Harrison, C.; McKay, D.; Broderick, C.; Latimer, J.; Britt, H.; Maher, C.G. Musculoskeletal conditions in children and adolescents managed in Australian primary care. BMC Musculoskelet. Disord. 2014, 15, 164. [Google Scholar] [CrossRef]
- Grimmer, K.A.; Jones, D.; Williams, J. Prevalence of adolescent injury from recreational exercise: An Australian perspective. J. Adolesc. Health 2000, 27, 266–272. [Google Scholar] [CrossRef]
- Faramarzi Kohneh Shahri, Y.; Ghani Zadeh Hesar, N. Validity and reliability of smartphone-based Goniometer-Pro app for measuring the thoracic kyphosis. Musculoskelet. Sci. Pract. 2020, 49, 102216. [Google Scholar] [CrossRef]
- Barrett, E.; Lenehan, B.; O’sullivan, K.; Lewis, J.; McCreesh, K. Validation of the manual inclinometer and flexicurve for the measurement of thoracic kyphosis. Physiother. Theory Pract. 2018, 34, 301–308. [Google Scholar] [CrossRef]
- Barrett, E.; McCreesh, K.; Lewis, J. Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: A systematic review. Man. Ther. 2014, 19, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Greendale, G.A.; Nili, N.S.; Huang, M.-H.; Seeger, L.; Karlamangla, A.S. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos. Int. 2011, 22, 1897–1905. [Google Scholar] [CrossRef]
- Teixeira, F.; Carvalho, G. Reliability and validity of thoracic kyphosis measurements using flexicurve method. Braz. J. Phys. Ther 2007, 11, 199–204. [Google Scholar]
- Bucke, J.; Spencer, S.; Fawcett, L.; Sonvico, L.; Rushton, A.; Heneghan, N.R. Validity of the Digital Inclinometer and iPhone When Measuring Thoracic Spine Rotation. J. Athl. Train. 2017, 52, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Barrett, E.; McCreesh, K.; Lewis, J. Intrarater and interrater reliability of the flexicurve index, flexicurve angle, and manual inclinometer for the measurement of thoracic kyphosis. Rehabil. Res. Pract. 2013, 2013, 475870. [Google Scholar] [CrossRef]
- Lafage, R.; Steinberger, J.; Pesenti, S.; Assi, A.; Elysee, J.C.; Iyer, S.; Lenke, L.G.; Schwab, F.J.; Kim, H.J.; Lafage, V. Understanding Thoracic Spine Morphology, Shape, and Proportionality. Spine 2020, 45, 149–157. [Google Scholar] [CrossRef]
- Billis, E.V.; Foster, N.E.; Wright, C.C. Reproducibility and repeatability: Errors of three groups of physiotherapists in locating spinal levels by palpation. Man. Ther. 2003, 8, 223–232. [Google Scholar] [CrossRef]
- Furlanetto, T.S.; Candotti, C.T.; Comerlato, T.; Loss, J.F. Validating a postural evaluation method developed using a Digital Image-based Postural Assessment (DIPA) software. Comput. Methods Programs Biomed. 2012, 108, 203–212. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chen, B.; Liu, P.; Xiao, F.; Liu, Z.; Wang, Y. Review of the upright balance assessment based on the force plate. Int. J. Environ. Res. Public Health 2021, 18, 2696. [Google Scholar] [CrossRef]
- Ratamess, N.; Alvar, B.A.; Evetoch, T.K.; Housh, T.J. Progression Models in Resistance Training for Healthy Adults. Med. Sci. Sport. Exerc. 2009, 41, 687–708. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Yoo, W. Effect of thoracic stretching, thoracic extension exercise and exercises for cervical and scapular posture on thoracic kyphosis angle and upper thoracic pain. J. Phys. Ther. Sci. 2013, 25, 1509–1510. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, D.; Brown, E. The influence of an in-home based therapeutic exercise program on thoracic kyphosis angles. J. Back Musculoskelet. Rehabil. 2007, 20, 155–165. [Google Scholar] [CrossRef]
- Fryer, G. Muscle energy technique: An evidence-informed approach. Int. J. Osteopath. Med. 2011, 14, 3–9. [Google Scholar] [CrossRef]
- Chaitow, L.; Crenshaw, K. Muscle Energy Techniques; Elsevier Churchill Livingstone: London, UK, 2006. [Google Scholar]
- Granacher, U.; Gollhofer, A.; Hortobágyi, T.; Kressig, R.W.; Muehlbauer, T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: A Systematic Review. Sport. Med. 2013, 43, 627–641. [Google Scholar] [CrossRef]
- Korakakis, V.; O’Sullivan, K.; O’Sullivan, P.B.; Evagelinou, V.; Sotiralis, Y.; Sideris, A.; Sakellariou, K.; Karanasios, S.; Giakas, G. Physiotherapist perceptions of optimal sitting and standing posture. Musculoskelet. Sci. Pract. 2019, 39, 24–31. [Google Scholar] [CrossRef]
- Lederman, E. Neuromuscular Rehabilitation in Manual and Physical Therapies; Elsevier Churchill Livingstone: London, UK, 2010. [Google Scholar]
- Neptune, R.R.; Vistamehr, A. Dynamic balance during human movement: Measurement and control mechanisms. J. Biomech. Eng. 2019, 141, 070801. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, M.G.; Berti, L.; Presti, C.; Frizziero, A.; Giannini, S. Effects of an adapted physical activity program in a group of elderly subjects with flexed posture: Clinical and instrumental assessment. J. Neuroeng. Rehabil. 2008, 5, 32. [Google Scholar] [CrossRef] [PubMed]
- Gunendi, Z.; Ozyemisci-Taskiran, O.; Demirsoy, N. The effect of 4-week aerobic exercise program on postural balance in postmenopausal women with osteoporosis. Rheumatol. Int. 2008, 28, 1217–1222. [Google Scholar] [CrossRef]

| Demographic Characteristics | CCEP (n = 21) X ± SD (Min–Max) | TEP (n = 22) X ± SD (Min–Max) | CG (n = 19) X ± SD (Min–Max) | p |
|---|---|---|---|---|
| Age (years) | 14.7 ± 1.3 (13–18) | 13.5 ± 1.1 (12–16) | 13.9 ± 1.9 (10–17) | 0.650 |
| Height (cm) | 170.5 ± 8.6 (147–185 | 169 ± 5.8 (157–178) | 168.3 ± 10.6 (145–187) | 0.528 |
| Body weight (kg) | 61.8 ± 11.8 (39–82) | 62.9 ± 11.8 (38–80) | 61.9 ± 12.6 (40–88) | 0.893 |
| BMI (kg/m2) | 21.5 ± 3.2 (14.1–25.8) | 21.7 ± 3.5 (14.1–27) | 21.7 ± 2.8 (13.8–25.6) | 0.748 |
| CCEP | TEP | CG | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre X ± SD | Post X ± SD | t | p | Pre X ± SD | Post X ± SD | t | p | Pre X ± SD | Post X ± SD | t | p | p × t (eta2) | p G × t (eta2) | p G (eta2) | |
| Flexible Ruler (KA) | 34.10 ± 6.03 | 25.17 ± 3.83 | 5.128 | 0.000 ** | 32.98 ± 6.38 | 28.65 ± 5.90 | 4.064 | 0.001 ** | 34.94 ± 3.87 | 35.28 ± 4.46 | 0.217 | 0.830 | 0.000 * (0.304) | 0.000 * (0.247) | 0.000 * (0.254) |
| PPT | 2.14 ± 2.54 | 12.62 ± 4.07 | 11.555 | 0.000 ** | 3.18 ± 3.63 | 3.41 ± 3.23 | 0.439 | 0.665 | 2.63 ± 2.57 | 2.11 ± 2.54 | 1.455 | 0.163 | 0.000 * (0.580) | 0.000 * (0.753 | 0.000 * (0.385) |
| RI | 146.30 ± 86.1 | 27.71 ± 25.39 | 4.122 | 0.006 ** | 68,11 ± 62,1 | 87,13 ± 175,23 | 0.299 | 0.775 | 55.75 ± 40.4 | 54.03 ± 45.63 | 0.065 | 0.952 | 0.209 (0.091) | 0.085 (0.252) | 0.699 (0.041) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elpeze, G.; Usgu, G. The Effect of a Comprehensive Corrective Exercise Program on Kyphosis Angle and Balance in Kyphotic Adolescents. Healthcare 2022, 10, 2478. https://doi.org/10.3390/healthcare10122478
Elpeze G, Usgu G. The Effect of a Comprehensive Corrective Exercise Program on Kyphosis Angle and Balance in Kyphotic Adolescents. Healthcare. 2022; 10(12):2478. https://doi.org/10.3390/healthcare10122478
Chicago/Turabian StyleElpeze, Gönül, and Günseli Usgu. 2022. "The Effect of a Comprehensive Corrective Exercise Program on Kyphosis Angle and Balance in Kyphotic Adolescents" Healthcare 10, no. 12: 2478. https://doi.org/10.3390/healthcare10122478
APA StyleElpeze, G., & Usgu, G. (2022). The Effect of a Comprehensive Corrective Exercise Program on Kyphosis Angle and Balance in Kyphotic Adolescents. Healthcare, 10(12), 2478. https://doi.org/10.3390/healthcare10122478





