Health System Resiliency and the COVID-19 Pandemic: A Case Study of a New Nationwide Contingency Staffing Program
Abstract
:1. Introduction
2. Methods
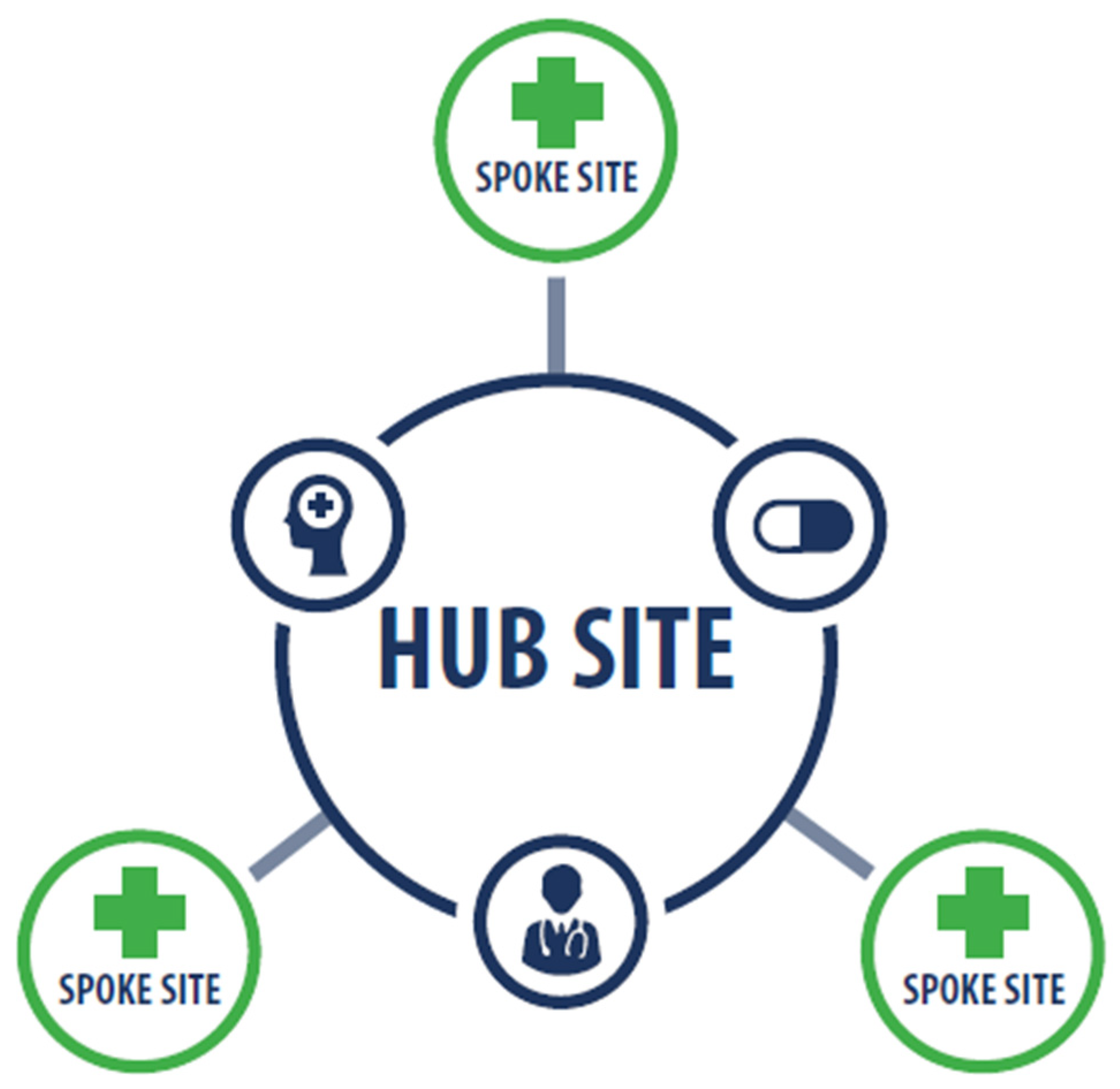
2.1. Clinical Resource Hub Program
2.2. Sample and Data Collection
2.3. Data Analysis
3. Results
3.1. CRHs Maintained Patient Access to Care during the Pandemic
3.1.1. Outpatient Clinical Coverage
So when COVID-19 started we actually proactively connected with our spoke sites and told them, ‘We committed to this 100% telehealth provider for you so, we recommend that you shift your in-person providers to assist the main facility’, because a lot of facilities were shifting their outpatient providers to inpatient care depending on where they were as a hot spot or not. And then we also suggested that if they had Veteran needs, from other [small clinics], then to map those Veterans to our CRH provider panel.(CRH director A)
We actually put two primary care providers in there to take over a team because they lost a provider out to COVID-19. And so we’ve got those folks in there actually just doing phone calls and video visits covering for them. So you know, [we say], ‘We’re here to help. I know you’re having access issues. Let us jump in.’(CRH director B)
3.1.2. Inpatient Coverage
We detailed […] full time social workers virtually […] to cover inpatient care at our VA, which was considered one of the top hot spots in the country for COVID-19. So they actually worked 100% remotely from their home or their existing facilities to cover all inpatient units. And they saw those Veterans either by phone or video on demand, which was nice because they could also include their family member in the visit. It went really well.(CRH director A)
…we have a pharmacist that was detailed to [City], virtually, to assist with providing taking care of inpatient drug orders on patients when they had people that were out.(CRH director B)
3.1.3. Triage Support
Thenurses actually started a kind of mini-COVID clinic where if people were identified as COVID positive and their sites didn’t have enough bandwidth to call and check on them for the five days after they had a positive reading, our team did that.(CRH director C)
We actually detailed a few LIPs [licensed independent practitioners], I believe like 10 to 15, to work on second-level triage support to our clinical contact center [nurse advice line] during off hours, so the evening hours and weekends. They took second-level triage calls for COVID and flu-related symptoms.(CRH director A)
3.1.4. The Provision of Patient Care in the Private Sector
3.2. CRH Providers Provided Workforce Care and Training during the Pandemic
Since we were [using] video [in our CRH work], we were able to help our region by just showing them how it worked for us and that it’s not a scary technology but one that’s, you know, could be beneficial. […] You know, we shared just best practices such as the need to obtain consent and locations and all that fun stuff.(CRH director D)
We’ve also offered services in terms of providing coaching and counseling with our providers in the region who may be involved in any palliative care decisions in COVID-19 patients.(CRH director E)
I have a psychiatrist who’s doing second-level screening of patients and employees after hours. So basically he works from 5:30 PM to 5:30 AM taking calls on anybody that screens positive.(CRH director B)
3.3. Factors Facilitating the CRH Response to COVID-19: Expertise and Acceptability of Telehealth
[CRH providers] were already ready to do this work […] we were already doing it […] so it did allow for some opportunities to deploy services to places that were really struggling(National program leader 8)
We had some initial resistance in some [regions] to adopt virtual care. But with COVID it forced that function and awakened several leaders to say, ‘Gosh this does work and we can do it and in fact it’s critical for us’(National program leader 5)
4. Discussion
5. Limitations and Areas for Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Freytas Tamura, K.; Hubler, S.; Fuchs, H.; Montgomery, D. Like ‘a Bus Accident a Day’: Hospitals Strain Under New Flood of COVID-19 Patients. New York Times, 9 July 2020, Updated 11 July 2020. Available online: https://www.nytimes.com/2020/07/09/us/coronavirus-hospitals-capacity.html (accessed on 28 August 2021).
- England, R. COVID-19: Critical Care Wards Full in Hospitals across England. BBC News. 18 January 2021. Available online: https://www.bbc.com/news/uk-england-55672901 (accessed on 28 August 2021).
- Inskeep, S. Doctor in India: Emergency Room is So Crowded, It’s Nearly Impossible to Walk; NPR: Washington, DC, USA, 2021; Available online: https://www.npr.org/sections/coronavirus-live-updates/2021/05/06/994145513/indias-covid-19-crisis-continue-to-get-worse (accessed on 28 August 2021).
- Soucheray, S. US COVID-19 Cases Surge Past 82,000, Highest Total in World; Center for Infectious Disease Research and Policy, University of Minnesota: Minneapolis, MN, USA, 2020; Available online: https://www.cidrap.umn.edu/news-perspective/2020/03/us-covid-19-cases-surge-past-82000-highest-total-world (accessed on 18 October 2021).
- Kruk, M.E.; Myers, M.; Tornorlah Varpilah, S.; Dahn, B.T. What is a Resilient Health System? Lessons from Ebola. Lancet 2015, 385, 1910–1912. [Google Scholar] [CrossRef]
- Blanchet, K.; Nam, S.L.; Ramalingam, B.; Pozo-Martin, F. Governance and Capacity to Manage Resilience of Health Systems: Towards a New Conceptual Framework. Int. J. Health Policy Manag. 2017, 6, 431–435. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanefeld, J.; Mayhew, S.; Legido-Quigley, H.; Martineau, F.; Karanikolos, M.; Blanchet, K.; Liverani, M.; Mokuwa, E.Y.; McKay, G.; Balabanova, D. Towards an Understanding of Resilience: Responding to Health Systems Shocks. Health Policy Plan. 2018, 33, 355–367. [Google Scholar] [CrossRef] [Green Version]
- Yano, E.; Soban, L.; Parkerton, P.H.; Etzioni, D.A. Primary Care Practice Organization Influences Colorectal Cancer Screening Performance. Health Serv. Res. 2007, 42, 1130–1149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soban, L.; Yano, E. The Impact of Primary Care Resources on Prevention Practices. J. Ambul. Care Manag. 2005, 28, 241–253. [Google Scholar] [CrossRef] [PubMed]
- Helfrich, C.D.; Simonetti, J.A.; Clinton, W.L.; Wood, G.B.; Taylor, L.; Schectman, G.; Stark, R.; Rubenstein, L.V.; Fihn, S.D.; Nelson, K.M. The Association of Team-Specific Workload and Staffing with Odds of Burnout among VA Primary Care Team Members. J. Gen. Intern. Med. 2017, 32, 760–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helfrich, C.D.; Dolan, E.D.; Simonetti, J.; Reid, R.J.; Joos, S.; Wakefield, B.J.; Schectman, G.; Stark, R.; Fihn, S.D.; Harvey, H.B.; et al. Elements of Team-Based Care in a Patient-Centered Medical Home Are Associated with Lower Burnout Among VA Primary Care Employees. J. Gen. Intern. Med. 2014, 29, 659–666. [Google Scholar] [CrossRef]
- Khan, Y.; O’Sullivan, T.; Brown, A.; Tracey, S.; Gibson, J.; Genereux, M.; Henry, B.; Schwartz, B. Public Health Emergency Preparedness: A Framework to Promote Resilience. BMC Public Health 2018, 18, 1344–1360. [Google Scholar] [CrossRef] [Green Version]
- Thomas, S.; Sagan, A.; Larkin, J.; Cylus, J.; Figueras, J.; Karanikolos, M. Strengthening Health Systems Resilience: Key Concepts and Strategies. World Health Organization Policy Brief 36. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/332441/Policy-brief%2036-1997-8073-eng.pdf (accessed on 18 October 2021).
- Fridell, M.; Edwin, S.; von Schreeb, J.; Saulnier, D.D. Health System Resilience: What are we Talking About? A Scoping Review Mapping Characteristics and Keywords. Int. J. Health Policy Manag. 2019, 9, 6–16. [Google Scholar] [CrossRef]
- Madrigano, J.; Chandra, A.; Costigan, T.; Acosta, J.D. Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future. Int. J. Environ. Res. Public Health 2017, 14, 1563. [Google Scholar] [CrossRef] [Green Version]
- Heyworth, L.; Kirsh, S.; Zulman, D.; Ferguson, J.M.; Kizer, K.W. Expanding Access Through Virtual Care: The VA’s Early Experience with COVID-19. NEJM Catal. Innov. Care Deliv. 2020, 1–11. [Google Scholar] [CrossRef]
- Dussault, G.; Franceschini, M.C. Not Enough There, Too Many Here: Understanding Geographical Imbalances in the Distribution of the Health Workforce. Hum. Resour. Health 2006, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.D.; Gunzburger, E.; Glorioso, T.J.; Smith, W.B.; Kenney, R.R.; Whooley, M.A.; Ho, M.P. Impact of Longitudinal Virtual Primary Care on Diabetes Quality of Care. J. Gen. Intern. Med. 2021, 36, 2585–2592. [Google Scholar] [CrossRef] [PubMed]
- Gale, R.C.; Wu, J.; Erhardt, T.; Bounthavong, M.; Reardon, C.; Damschroder, L.J.; Midboe, A.M. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement. Sci. 2019, 14, 11. [Google Scholar] [CrossRef] [Green Version]
- Taylor, B.; Henshall, C.; Kenyon, S.; Litchfield, I.; Greenfield, S. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open 2018, 8, e019993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Therrien, M.C.; Normandin, J.M.; Denis, J.L. Bridging Complexity theory and resilience to develop surge capacity in health systems. J. Health Organ. Manag. 2017, 31, 96–109. [Google Scholar] [CrossRef]
- Williams, G.A.; Maier, C.B.; Scarpetti, G.; Giulio de Belvis, A.; Fattore, G.; Morsella, A.; Pastorino, G.; Poscia, A.; Ricciardi, W.; Silenzi, A. What Strategies Are Countries Using to Expand Health Workforce Surge Capacity during the COVID-19 Pandemic? Eurohealth. 2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/336296/Eurohealth-26-2-51-57-eng.pdf?sequence=1&isAllowed=y (accessed on 18 October 2021).
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for Global Emergencies: Implications for Coronavirus Disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [Green Version]
- Seda, G.; Parrish, J.S. Augmenting Critical Care Capacity in a Disaster. Crit. Care Clin. 2019, 35, 563–573. [Google Scholar] [CrossRef]
- Rolston, D.; Meltzer, J.S. Telemedicine in the Intensive Care Unit: Its Role in Emergencies and Disaster Management. Crit. Care Clin. 2015, 31, 239–255. [Google Scholar] [CrossRef]
- Lee, J.Q.; Loke, W.; Ng, Q.X. The Role of Family Physicians in a Pandemic: A Blueprint. Healthcare 2020, 8, 198. [Google Scholar] [CrossRef]
- Barasa, E.; Mbau, R.; Gilson, L. What is Resilience and How Can it be Nurtured? A Systematic Review of Empirical Literature on Organizational Resilience. Int. J. Health Policy Manag. 2018, 7, 491–503. [Google Scholar] [CrossRef] [PubMed]
- Albott, C.S.; Wozniak, J.R.; McGlinch, B.P.; Wall, M.H.; Gold, B.S.; Vinogradov, S. Battle Buddies: Rapid Deployment of a Psychological Resilience Intervention for Health Care Workers During the Coronavirus Disease 2019 Pandemic. Int. Anesth. Res. Soc. 2020, 1–12. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cannedy, S.; Bergman, A.; Medich, M.; Rose, D.E.; Stockdale, S.E. Health System Resiliency and the COVID-19 Pandemic: A Case Study of a New Nationwide Contingency Staffing Program. Healthcare 2022, 10, 244. https://doi.org/10.3390/healthcare10020244
Cannedy S, Bergman A, Medich M, Rose DE, Stockdale SE. Health System Resiliency and the COVID-19 Pandemic: A Case Study of a New Nationwide Contingency Staffing Program. Healthcare. 2022; 10(2):244. https://doi.org/10.3390/healthcare10020244
Chicago/Turabian StyleCannedy, Shay, Alicia Bergman, Melissa Medich, Danielle E. Rose, and Susan E. Stockdale. 2022. "Health System Resiliency and the COVID-19 Pandemic: A Case Study of a New Nationwide Contingency Staffing Program" Healthcare 10, no. 2: 244. https://doi.org/10.3390/healthcare10020244
APA StyleCannedy, S., Bergman, A., Medich, M., Rose, D. E., & Stockdale, S. E. (2022). Health System Resiliency and the COVID-19 Pandemic: A Case Study of a New Nationwide Contingency Staffing Program. Healthcare, 10(2), 244. https://doi.org/10.3390/healthcare10020244





