Can Music Therapy Improve the Quality of Life of Institutionalized Elderly People?
Abstract
1. Introduction
2. Theoretical Framework
3. Method
3.1. Inclusion and Exclusion Criteria
3.2. Participants
3.3. Ethical Considerations
3.4. Instruments
3.4.1. Quantitative Instruments
3.4.2. Qualitative Instruments
3.5. Procedure and Data Analysis
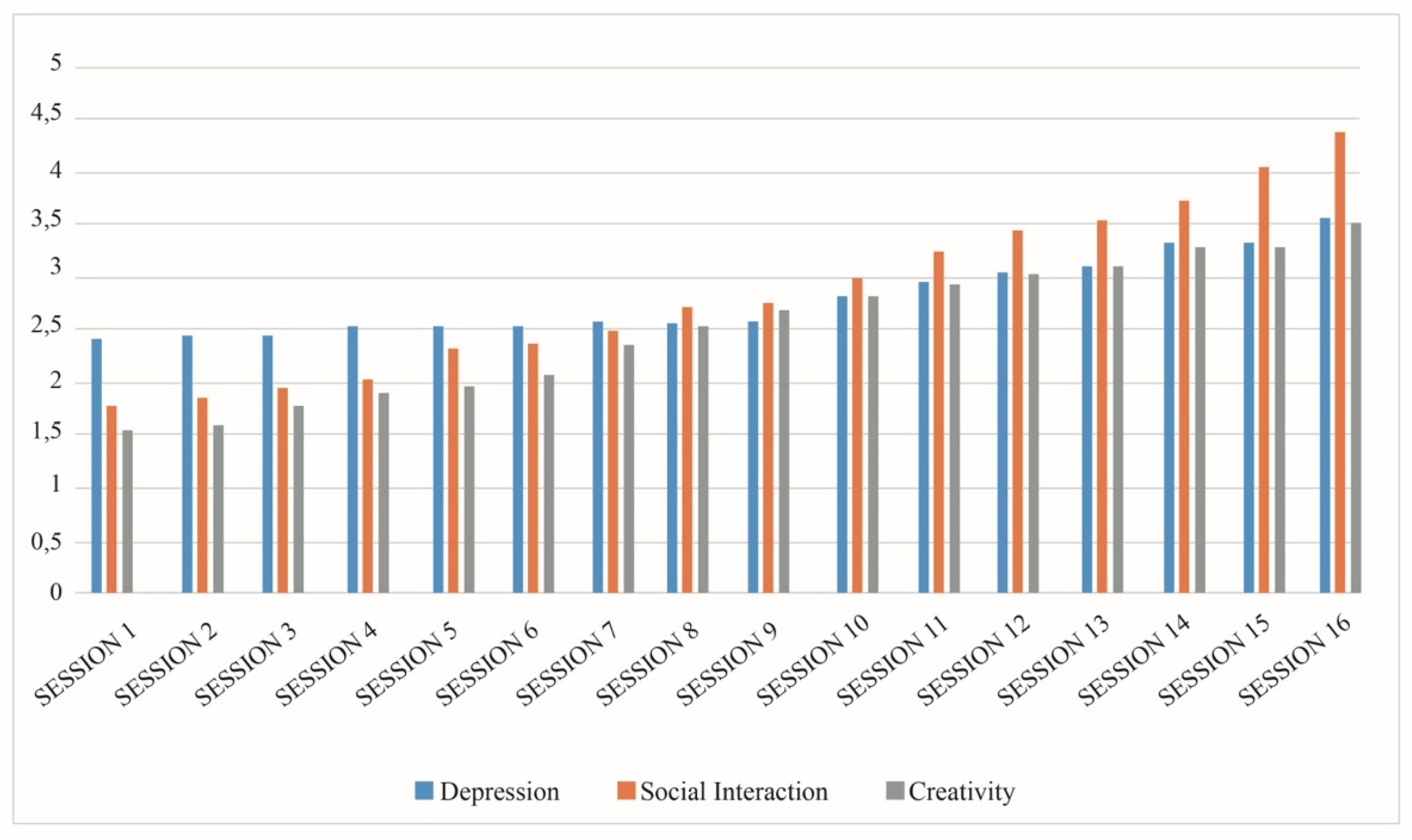
4. Results
4.1. Depression
4.2. Quality of Life
5. Discussion and Conclusions
Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Domínguez, M.J.V.; Azcona, J.M.L.; Durantez, P.C.; Muñoz, A.M.; Doblas, J.L.; Navarro, A.M.; Landwerling, G.M. Informe 2016. Las Personas Mayores en España; INSERSO: Madrid, Spain, 2017. [Google Scholar]
- Weening-Dijksterhuis, E.; De Greef, M.H.; Scherder, E.J.; Slaets, J.P.; Van der Schans, C.P. Frail institutionalized older persons: A comprehensive review on physical exercise, physical fitness, activities of daily living, and quality-of-life. Am. J. Phys. Med. Rehabil. 2011, 90, 156–168. [Google Scholar] [CrossRef]
- Creech, A.; Hallam, S.; McQueen, H.; Varvarigou, M. The power of music in the lives of older adults. Res. Stud. Music Ed. 2013, 35, 87–102. [Google Scholar] [CrossRef]
- Beer, L.E. The role of the music therapist in training caregivers of people who have advanced dementia. Nord J. Music Ther. 2017, 26, 185–199. [Google Scholar] [CrossRef]
- Hanzeliková, A.P.; López-Muñoz, F.; Fusté, R.M. Pérfil socio-demográfico de los cuidadores de pacientes geriátricos hospitalizados mayores de 75 años y su relación con la satisfacción. Enferm. Glob. 2017, 16, 375–388. [Google Scholar] [CrossRef]
- Martínez Sabater, A.; Pascual Ruiz, M.F. Musicoterapia en geriatría. Enferm. Int. 2004, 33–36. [Google Scholar] [CrossRef]
- Domínguez Lloria, S.; González Ojea, M.J.; Pino Juste, M. Efficiency of music therapy as a non-pharmacological treatment for the elderly. Int. J. Health Wellness Soc. 2019, 9, 27–34. [Google Scholar] [CrossRef]
- Yap, A.F.; Kwan, Y.H.; Tan, C.S.; Ibrahim, S.; Ang, S.B. Rhythm-centred music making in community living elderly: A randomized pilot study. BMC Complement. Altern. Med. 2017, 17, 311. [Google Scholar] [CrossRef] [PubMed]
- Guetin, S.; Charras, K.; Berard, A.; Arbus, C.; Berthelon, P.; Blanc, F.; Ducourneau, G. An overview of the use of music therapy in the context of Alzheimer’s disease: A report of a French expert group. Dementia 2013, 12, 619–634. [Google Scholar] [CrossRef]
- Park, A.L. Can musical activities promote healthy ageing? Int. J. Emerg. Ment. Health 2015, 17, 258–261. [Google Scholar] [CrossRef]
- WHO. Depresión; Organización Mundial de la Salud: Madrid, Spain, 2020; Available online: https://www.who.int/topics/depression/es/ (accessed on 3 June 2018).
- Wojtalik, J.A.; Eack, S.M.; Smith, M.J.; Keshavan, M.S. Using cognitive neuroscience to improve mental health treatment: A comprehensive review. J. Soc. Soc. Work Res. 2018, 9, 223–260. [Google Scholar] [CrossRef]
- Sánchez, R.O.; De Juan, T.F. Salud mental y envejecimiento: Una experiencia comunitaria de musicoterapia con ancianos deprimidos. Psicol. Salud 2006, 16, 93–101. [Google Scholar] [CrossRef]
- Lazo González, D.F. Programa de Musicoterapia Grupal para Mejorar el Estado Emocional en Pacientes de la Tercera Edad que Presentan Depresión Moderada. Bachelor’s Thesis, Universidad del Azuay, Cuenca, Ecuador, 2013. [Google Scholar]
- Gallego, M.G.; García, J.G. Musicoterapia en la enfermedad de Alzheimer: Efectos cognitivos, psicológicos y conductuales. Neurología 2017, 32, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Dev, A.; Smitha, K.V.; Pillai, R.R. Music therapy for institutionalised elderly persons with depression. Open J. Psychiatry Allied Sci. 2015, 6, 15–19. [Google Scholar]
- Chu, H.; Yang, C.Y.; Lin, Y.; Ou, K.L.; Lee, T.Y.; O’Brien, A.P.; Chou, K.R. The impact of group music therapy on depression and cognition in elderly persons with dementia: A randomized controlled study. Biol. Res. Nurs. 2014, 16, 209–217. [Google Scholar] [CrossRef]
- Cardona-Arias, J.A.; Higuita-Gutiérrez, L.F. Aplicaciones de un instrumento diseñado por la OMS para la evaluación de la calidad de vida. Rev. Cub. Salud Públ. 2014, 40, 175–189. [Google Scholar]
- Leubner, D.; Hinterberger, T. Reviewing the effectiveness of music interventions in treating depression. Fronts Psychol. 2017, 8, 1109. [Google Scholar] [CrossRef]
- Soria-Urios, G.; Duque-San Juan, P.; García-Moreno, J.M. Terapias musicales en la rehabilitación del lenguaje y musicoterapia en personas con demencia. Alzheimer Realid Invest. Dem. 2013, 54, 35–41. [Google Scholar] [CrossRef]
- Särkämö, T. Musical leisure activities to support cognitive and emotional functioning in aging and dementia: A review of current evidence. In Music and Dementia: From Cognition to Therapy; Baird, A., Garrido, S., Tamplin, J., Eds.; Oxford University Press: New York, NY, USA, 2020; pp. 103–121. [Google Scholar]
- Yin, R.K. Case study Research: Design and Methods; Sage: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Souza, F.; Souza, D.; Costa, A. Investigação Qualitativa: Inovação, Dilemas e Desafíos; Edita Ludomedia: Lisboa, Portugal, 2015. [Google Scholar]
- Domínguez-Lloria, S.; González-Ojea, M.; Pino-Juste, J. Design of a Music Therapy Program as a Non-Pharmacological Treatment; Intervention in Clinical and Health Contexts; del Mar Molero, M., del Carmen Pércz-Fuentes, M., Gázquez, J.J., del Mar Simón, M., Barragán, A.B., Martos, A., Sisto, M., Eds.; ASUNIVEP: Madrid, Spain, 2018; pp. 399–407. [Google Scholar]
- Committee on Publication Ethics (COPE) Promoting Integrity in Scholarly Research and Its Publication. 2020. Available online: https://bit.ly/3w7qkvL (accessed on 2 June 2020).
- AERA. Ethical Standards of AERA, American Educational Research Association. Available online: https://bit.ly/3tIDQEc (accessed on 3 June 2018).
- APA. Ethical Principles of Psychologist and Code of Conduct. Available online: https://bit.ly/3tIa8zd (accessed on 3 June 2017).
- Cid-Ruzafa, J.; Damián-Moreno, J. Valoración de la discapacidad física: El índice de Barthel. Rev. Esp. Salud Pública 1997, 71, 127–137. [Google Scholar] [CrossRef]
- De la Iglesia, J.M.; Dueñas Herrero, R.; Onís Vilches, M.C.; Aguado Taberné, C.; Albert Colomer, C.; Luque Luque, R. Adaptación y validación al castellano del cuestionario de Pfeiffer (SPMSQ) para detectar la existencia de deterioro cognitivo en personas mayores de 65 años. Med. Clin. 2001, 117, 129–134. [Google Scholar] [CrossRef]
- Beck, A.; Epstein, N.; Brown, G.; Steer, R. An inventory for measuring clinical anxiety. Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef]
- Vázquez, C.; Sanz, J. Fiabilidad y validez de la versión española del Inventario para la Depresión de Beck de 1978 en pacientes con trastornos psicológicos. Clin. Salud 1999, 10, 59–81. [Google Scholar]
- Beck, R.; Perkins, T.S. Cognitive content-specificity for anxiety and depression: A meta-analysis. Cognit. Ther. Res. 2001, 25, 651–663. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Manual. BDI–FS. Inventario de Depresión de Beck para Pacientes Médicos (Adaptación Española: Sanz, J., Izquierdo, A., y García-Vera, M.P.). Pearson, 2011b. Available online: https://www.redalyc.org/pdf/1806/180617972001.pdf (accessed on 3 June 2018).
- Sanz, J.; Perdigón, A.; Vásquez, C. The spanish adaptation of Beck’s Depression Inventory-II (BDI-II): 2 Psychometric properties in the general population. Clín. Salud 2003, 14, 249–280. [Google Scholar]
- Wołoszyn, N.; Grzegorczyk, J.; Wiśniowska-Szurlej, A.; Kilian, J.; Kwolek, A. Psychophysical health factors and its correlations in elderly wheelchair users who live in nursing homes. Int. J. Environ. Public Health 2020, 17, 1706. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Padilla, L.M.; González Pérez, U.; Alerm González, A.; Bacallao Gallestey, J. Calidad de vida psíquica y estado de salud física en el adulto mayor. Rev. Hab. Cienc. Med. 2014, 13, 337–349. [Google Scholar]
- Wang, J.; Zhu, W.H.; Li, Y.F.; Zhu, W.W. Interaction between worsening cognitive function and deteriorating functional status on depressive symptoms among Chinese community-dwelling elders. Geriatr. Gerontol. Int. 2020, 20, 343–347. [Google Scholar] [CrossRef]
- Benavides-Caro, C.A. Deterioro cognitivo en el adulto mayor. Rev. Mexicana Anest. 2017, 40, 107–112. [Google Scholar]
- Blackburn, R.; Bradshaw, T. Music therapy for service users with dementia: A critical review of the literature. J. Psychiatric Ment. Health Nurs. 2014, 21, 879–888. [Google Scholar] [CrossRef]
- Im, M.L.; Lee, J.I. Effects of art and music therapy on depression and cognitive function of the elderly. Technol. Health Care 2014, 22, 453–458. [Google Scholar] [CrossRef]
- Zhao, K.; Bai, Z.G.; Bo, A.; Chi, I. A systematic review and meta-analysis of music therapy for the older adults with depression. Int. J. Geriatr. Psychiatry 2016, 1, 1188–1198. [Google Scholar] [CrossRef] [PubMed]
- Aalbers, S.; Fusar-Poli, L.; Freeman, R.E.; Spreen, M.; Ket, J.C.F.; Vink, A.C.; Maratos, A.; Crawford, M.; Chen, X.J.; Gold, C. Music therapy for depression. Cochrane Database Syst. Rev. 2017, 11, CD004517. [Google Scholar] [CrossRef] [PubMed]
- Van der Steen, J.T.; Van Soest-Poortvliet, M.C.; Van der Wouden, J.C.; Bruinsma, M.S.; Scholten, R.J.; Vink, A.C. Music-Based Therapeutic Interventions for People with Dementia. Cochrane Database Syst. Rev. 2017, 5, CD003477. [Google Scholar] [CrossRef] [PubMed]
- Bergman, Y.S.; Bodner, E. Age is not just a number: Age awareness, subjective nearness-to-death, self-esteem, and depressive symptoms among older adults. Aging Ment. Health 2020, 24, 906–913. [Google Scholar] [CrossRef]
- Bastida-González, R.; Valdez-Medina, J.L.; Valor-Segura, I.; Fuentes, N.; Rivera-Aragón, S. Satisfacción marital y estado civil como factores protectores de la depresión y ansiedad. Rev. Arg. Clin. Psicol. 2017, 26, 95–102. [Google Scholar]
- Lozano, L.G.; Quiñones, F.M.; Reoyo, I.M.; Parrilla, M.G.; Romero, A.D.; Ramos, R.M.; Escalera, C.R. La depresión del anciano y el papel de la dinámica familiar. Atención Primaria 2000, 25, 226–229. [Google Scholar] [CrossRef][Green Version]
- González-Celis, A.L.; Padilla, A. Calidad de vida y estrategias de afrontamiento ante problemas y enfermedades en ancianos de Ciudad de México. Univ. Psychol. 2006, 5, 501–509. [Google Scholar]
| Variable | N | Mean (Pre) | Mean (Post) | SD (Pre) | SD (Post) | T (Pre) | T (Post) | Sig. (Pre) | Sig. (Post) | ES (Pre) | ES (Post) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BDI | Single | 23 | 5.73 | 5.21 | 5.585 | 4.389 | −0.660 | −2.048 | 0.513 | 0.046 | −0.091 | −0.269 |
| Marri/Widow | 29 | 6.72 | 8.41 | 5.154 | 6.806 | |||||||
| Children yes | 34 | 6.38 | 8.14 | 4.625 | 6.481 | 0.173 | 1.937 | 0.863 | 0.035 * | 0.0023 | 0.0285 | |
| Children no | 18 | 6.11 | 4.83 | 6.578 | 4.449 | |||||||
| Female | 37 | 6.32 | 7.51 | 5.607 | 6.572 | 0.076 | 0.964 | 0.940 | 0.339 | 0.011 | 0.157 | |
| Male | 15 | 6.20 | 5.73 | 4.708 | 4.333 | |||||||
| Single | 23 | 2.52 | 2.21 | 3.231 | 2.411 | −0.204 | −1.513 | 0.839 | 0.137 | −0.026 | −0.214 | |
| Marri/Widow | 29 | 2.68 | 3.41 | 2.713 | 3.122 | |||||||
| Primary School | 47 | 6.29 | 7.04 | 5.421 | 6.230 | 0.039 | 0.155 | 0.969 | 878 | 0.008 | 0.041 | |
| Secondary School | 5 | 6.20 | 6.60 | 4.764 | 4.037 | |||||||
| Children yes | 34 | 2.55 | 3.38 | 2.451 | 3.123 | −0.190 | 1.755 | 0.850 | 0.085 | −0.026 | 0.262 | |
| Children no | 18 | 2.72 | 1.94 | 3.738 | 2.071 | |||||||
| COGNITIVE | Female | 37 | 2.67 | 3.10 | 3.249 | 3.142 | 0.231 | 0.881 | 0.818 | 0.383 | 0.039 | 0.144 |
| Male | 15 | 2.46 | 2.33 | 1.995 | 2.023 | |||||||
| Single | 23 | 3.21 | 3.00 | 3.118 | 2.662 | −0.891 | −2.053 | 0.377 | 0.046 * | −0.124 | −0.369 | |
| Marri/Widow | 29 | 4.03 | 5.00 | 3.406 | 4.309 | |||||||
| Primarios | 47 | 2.68 | 2.95 | 3.008 | 2.918 | 0.491 | 0.558 | 0.625 | 0.579 | 0.129 | 0.137 | |
| Bachiller | 5 | 2.00 | 2.20 | 2.121 | 2.489 | |||||||
| Children yes | 34 | 3.82 | 4.76 | 3.261 | 4.119 | 0.452 | 1.737 | 0.654 | 0.088 | 0.066 | 0.260 | |
| Children no | 18 | 3.38 | 2.88 | 3.380 | 2.720 | |||||||
| SOMATIC | Female | 37 | 3.64 | 4.40 | 3.343 | 4.139 | −0.084 | 0.868 | 0.934 | 0.390 | −0.013 | 0.142 |
| Male | 15 | 3.73 | 3.40 | 3.217 | 2.667 | |||||||
| Primarios | 47 | 3.61 | 4.08 | 3.172 | 3.821 | −0.375 | −0.176 | 0.709 | 0.861 | −0.075 | −0.042 | |
| Bachiller | 5 | 4.20 | 4.40 | 4.549 | 3.714 |
| Variable | N | Mean (Pre) | Mean (Post) | SD (Pre) | SD (Post) | T (Pre) | T (Post) | Sig. (Pre) | Sig. (Post) | ES (Pre) | ES (Post) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PHYSICAL HEALTH | Single | 23 | 21.26 | 23.56 | 3.910 | 4.550 | 2.984 | 3.307 | 0.004 * | 0.002 * | 0.488 | 0.516 |
| Marri/Widow | 29 | 17.68 | 19.62 | 4.559 | 4.039 | |||||||
| Children yes | 34 | 18.35 | 20.38 | 4.702 | 4.206 | −2.138 | −2.160 | 0.039 * | 0.036 * | −0.391 | −0.292 | |
| Children no | 18 | 21.00 | 23.22 | 3.985 | 5.047 | |||||||
| Female | 37 | 18.43 | 20.24 | 4.173 | 3.839 | −2.127 | −2.915 | 0.038 * | 0.005 * | −0.397 | −0.480 | |
| Male | 15 | 21.33 | 24.13 | 5.108 | 5.475 | |||||||
| Primary School | 47 | 18.97 | 21.04 | 4.527 | 4.606 | −1.408 | −1.549 | 0.165 | 0.128 | −0.304 | −0.342 | |
| Secondary School | 5 | 22.00 | 24.40 | 4.949 | 4.615 | |||||||
| PSYCHOLOGICAL HEALTH | Single | 23 | 20.91 | 20.86 | 3.423 | 2.989 | 1.199 | 2.072 | 0.236 | 0.043 * | 0.167 | 0.357 |
| Marri/Widow | 29 | 19.62 | 18.86 | 4.169 | 3.805 | |||||||
| Children yes | 34 | 19.61 | 19.05 | 3.884 | 3.716 | −1.487 | −2.105 | 0.143 | 0.041 * | −0.213 | −0.285 | |
| Children no | 18 | 21.27 | 21.05 | 3.722 | 2.979 | |||||||
| Female | 37 | 20.16 | 19.40 | 4.146 | 3.685 | −0.087 | −1.092 | 0.931 | 0.280 | −0.013 | −0.226 | |
| Male | 15 | 20.26 | 20.60 | 3.239 | 3.268 | |||||||
| Primary School | 47 | 19.91 | 19.36 | 19.91 | 3.522 | −3.282 | −4.746 | 0.007 * | 0.001 * | −0.535 | −0.597 | |
| Secondary School | 5 | 22.80 | 23.40 | 22.80 | 1.516 | |||||||
| ENVIRONMENT | Single | 23 | 31.00 | 30.73 | 3.477 | 3.346 | −0.166 | 1.875 | 0.869 | 0.067 | −0.022 | 0.255 |
| Marri/Widow | 29 | 31.17 | 28.82 | 3.910 | 3.873 | |||||||
| Children yes | 34 | 30.88 | 28.79 | 4.035 | 3.764 | −0.570 | −2.439 | 0.571 | 0.018 * | −0.087 | −0.434 | |
| Children no | 18 | 31.50 | 31.33 | 2.995 | 3.162 | |||||||
| Female | 37 | 31.40 | 29.48 | 3.515 | 3.761 | 0.948 | −0.561 | 0.348 | 0.577 | 0.138 | −0.086 | |
| Male | 15 | 30.33 | 30.13 | 4.117 | 3.777 | |||||||
| Primary School | 47 | 30.70 | 29.19 | 3.568 | 3.548 | −2.477 | −3.073 | 0.017 * | 0.003 * | −0.535 | −0.743 | |
| Secondary School | 5 | 34.80 | 34.20 | 2.863 | 2.280 | |||||||
| SOCIAL RELATION SHIP | Single | 23 | 8.56 | 8.69 | 1.590 | 1.459 | 0.325 | 1.316 | 0.747 | 0.194 | 0.047 | 0.184 |
| Marri/Widow | 29 | 8.37 | 8.03 | 2.351 | 2.026 | |||||||
| Children yes | 34 | 8.61 | 8.32 | 2.243 | 1.995 | 0.758 | −0.018 | 0.452 | 0.985 | 0.115 | −0.002 | |
| Children no | 18 | 8.16 | 8.33 | 1.581 | 1.455 | |||||||
| Female | 37 | 8.78 | 8.59 | 1.945 | 1.640 | 1.836 | 1.704 | 0.072 | 0.095 | 0.267 | 0.240 | |
| Male | 15 | 7.66 | 7.66 | 2.093 | 2.093 | |||||||
| Primary School | 47 | 8.617 | 8.46 | 1.917 | 1.666 | 1.723 | 1.757 | 0.091 | 0.085 | 0.323 | 0.307 | |
| Secondary School | 5 | 7.00 | 7.00 | 2.738 | 2.738 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Ojea, M.J.; Domínguez-Lloria, S.; Pino-Juste, M. Can Music Therapy Improve the Quality of Life of Institutionalized Elderly People? Healthcare 2022, 10, 310. https://doi.org/10.3390/healthcare10020310
González-Ojea MJ, Domínguez-Lloria S, Pino-Juste M. Can Music Therapy Improve the Quality of Life of Institutionalized Elderly People? Healthcare. 2022; 10(2):310. https://doi.org/10.3390/healthcare10020310
Chicago/Turabian StyleGonzález-Ojea, María José, Sara Domínguez-Lloria, and Margarita Pino-Juste. 2022. "Can Music Therapy Improve the Quality of Life of Institutionalized Elderly People?" Healthcare 10, no. 2: 310. https://doi.org/10.3390/healthcare10020310
APA StyleGonzález-Ojea, M. J., Domínguez-Lloria, S., & Pino-Juste, M. (2022). Can Music Therapy Improve the Quality of Life of Institutionalized Elderly People? Healthcare, 10(2), 310. https://doi.org/10.3390/healthcare10020310






