Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study
Abstract
:1. Introduction
Literature Review
2. Materials and Methods
2.1. Study Design and Data Source
2.2. Study Population
2.3. Study Variables
2.4. Statistical Analyses
3. Results
3.1. Patient Characteristics by USC Type
3.2. Outpatient Care Use by USC Type
3.3. Health Outcomes by USC Type
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Report on Diabetes. Available online: https://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf;jsessionid=4135C11AB0FBC5F273209E9BF646E47D?sequence=1 (accessed on 20 June 2021).
- International Diabetes Federation (IDF). IDF Diabetes Atlas, 9th Edition; 2019. Available online: https://diabetesatlas.org/idfawp/resource-files/2019/07/IDF_diabetes_atlas_ninth_edition_en.pdf (accessed on 20 June 2021).
- Jung, C.H.; Son, J.W.; Kang, S.; Kim, W.J.; Kim, H.S.; Kim, H.S.; Seo, M.; Shin, H.J.; Lee, S.S.; Jeong, S.J.; et al. Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status. Diabetes Metab. J. 2021, 45, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Cooperation and Development (OECD). Diabetes Care—Health at a Glance 2021: OECD Indicators; OECD Publishing: Paris, France, 2021. [Google Scholar] [CrossRef]
- Hong, J.S.; Kang, H.C. Continuity of ambulatory care and health outcomes in adult patients with type 2 diabetes in Korea. Health Policy 2013, 109, 158–165. [Google Scholar] [CrossRef] [PubMed]
- The Agency for Healthcare Research and Quality (AHRQ). AHRQ Quality Indicators—Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions; AHRQ Pub: Rockville, MD, USA, 2001. [Google Scholar]
- Hong, J.S.; Kang, H.C.; Kim, J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. J. Korean Med. Sci. 2010, 25, 1259–1271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shrivastav, M.; Gibson, W., Jr.; Shrivastav, R.; Elzea, K.; Khambatta, C.; Sonawane, R.; Sierrra, J.A.; Vigersky, R. Type 2 diabetes management in primary care management in primary care: The role of retrospective, professional continuous glucose monitoring. Diabetes Spectr. 2018, 31, 279–287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, A.M.; Cho, S.; Kim, H.J.; Jung, H.; Jo, M.W.; Lee, J.Y.; Eun, S.J. Primary Care Patients’ Preference for Hospitals over Clinics in Korea. Int. J. Environ. Res. Public Health 2018, 15, 1119. [Google Scholar] [CrossRef] [Green Version]
- Kim, D.R. The effect of having usual source of care on the choice among different types of medical facilities. Health Policy Manag. 2016, 26, 195–206. [Google Scholar] [CrossRef]
- Lee, S.S. Medical Delivery System TF Data; Ministry of Health and Welfare: Sejong, Korea, 2009.
- You, C.H.; Kwon, Y.D. Factors influencing medical institution selection for outpatient services. J. Korean Med. Assoc. 2012, 55, 898–910. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.Y.; Jo, M.W.; Yoo, W.S.; Kim, H.J.; Eun, S.J. Evidence of a broken healthcare delivery system in Korea: Unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J. Korean Med. Sci. 2014, 29, 1590–1596. [Google Scholar] [CrossRef] [Green Version]
- Organization for Economic Cooperation and Development (OECD). Realising the Potential of Primary Health Care. OECD Health Policy Studies; OECD Publishing: Paris, France, 2020. [Google Scholar] [CrossRef]
- Marcelino, M.; Nobre, E.L.; Chambel, P.; Domingues, A.; da Silva, M.P.; Santos, V.; Vilar, H.; Oliveira Lopes, L.; Carvalho, R.; Santana Lopes, M.; et al. Quality of care in diabetic outpatient clinics. Acta Med. Port. 2010, 23, 909–914. [Google Scholar]
- Harding, J.L.; Pavkov, M.E.; Magliano, D.J.; Shaw, J.E.; Gregg, E.W. Global trends in diabetes complications: A review of current evidence. Diabetologia 2019, 62, 3–16. [Google Scholar] [CrossRef] [Green Version]
- Kanumilli, N. Delivery of diabetes care in the Primary Care Network structure: A guideline. Diabetes Prim. Care 2021, 23, 37–39. [Google Scholar]
- De Berardis, G.; Pellegrini, F.; Franciosi, M.; Belfiglio, M.; Di Nardo, B.; Greenfield, S.; Kaplan, S.H.; Rossi, M.C.; Sacco, M.; Tognoni, G.; et al. Quality of care and outcomes in type 2 diabetic patients: A comparison between general practice and diabetes clinics. Diabetes Care 2004, 27, 398–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al Khaja, K.A.; Sequeira, R.P.; Damanhori, A.H. Comparison of the quality of diabetes care in primary care diabetic clinics and general practice clinics. Diabetes Res. Clin. Pract. 2005, 70, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Seo, D.H.; Kang, S.; Lee, Y.H.; Ha, J.Y.; Park, J.S.; Lee, B.W.; Kang, E.S.; Ahn, C.W.; Cha, B.S. Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea. Endocrinol. Metab. 2019, 34, 282–290. [Google Scholar] [CrossRef]
- Tobias, D.K.; Pan, A.; Jackson, C.L.; O’Reilly, E.J.; Ding, E.L.; Willett, W.C.; Manson, J.E.; Hu, F.B. Body-mass index and mortality among adults with incident type 2 diabetes. N. Engl. J. Med. 2014, 370, 233–244. [Google Scholar] [CrossRef] [Green Version]
- Hong, J.S.; Kang, H.C. Relationship between continuity of ambulatory care and medication adherence in adult patients with type 2 diabetes in Korea: A longitudinal analysis. Med. Care 2014, 52, 446–453. [Google Scholar] [CrossRef]
- Kang, H.C. Policy Direction for decreasing the concentration of patients to extra-large hospitals. Health Welf. Forum 2014, 210, 65–76. [Google Scholar]
- National Health Insurance Corporation. 2011 NHI Program. 2011. Available online: https://www.nhis.or.kr/static/html/wbd/g/a/wbdga0401.html. (accessed on 20 June 2021).
- Cho, S.J.; Chung, S.H.; Oh, J.Y. Differences between diabetic patients’ tertiary hospital and nontertiary hospital utilization according to comorbidity score. Health Policy Manag. 2011, 21, 527–540. [Google Scholar] [CrossRef]
- National Health Insurance Service and Health Insurance Review and Assessment Service. National Health Insurance Statistics Yearbook 2018; National Health Insurance Service and Health Insurance Review and Assessment Service: Wonju, Korea, 2018; Available online: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_LEE_02&conn_path=I3 (accessed on 20 June 2021).
- Hong, D.P.; Song, J. The effective distribution system for the concentration of patients to extra-large hospitals. J. Korean Surg. Soc. 2011, 80, 73–83. [Google Scholar] [CrossRef]
- Lee, J.C.; Kim, K.H.; Kim, H.N.; Kim, N.S. Factors associated with diabetes outpatient use of tertiary or general hospitals as their usual source of care in Korea. J. Korean Med. Assoc. 2012, 55, 1215–1225. [Google Scholar] [CrossRef] [Green Version]
- O’Connor, P.J.; Bodkin, N.L.; Fradkin, J.; Glasgow, R.E.; Greenfield, S.; Gregg, E.; Kerr, E.A.; Pawlson, L.G.; Selby, J.V.; Sutherland, J.E.; et al. Diabetes performance measures: Current status and future directions. Diabetes Care 2011, 34, 1651–1659. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.C.; Kim, K.H.; Kim, H.N.; Park, Y.H. Factors associated with the hypertension outpatients’ choice of health care providers in Korea. J. Korean Med. Assoc. 2011, 54, 961–970. [Google Scholar] [CrossRef] [Green Version]
| Types of USC | p-Value * | ||||||
|---|---|---|---|---|---|---|---|
| Total | TGHs | GHs | Hospital | Clinic | PHCs | ||
| 80,540 (100) | 7309 (9.1) | 11,989 (14.9) | 6399 (8.0) | 52,885 (65.7) | 1958 (2.4) | ||
| Patients’ Characteristics | |||||||
| Sex | |||||||
| Male | 44,129 (54.8) | 4157 (56.9) | 7203 (60.1) | 3864 (60.4) | 27,809 (52.6) | 1096 (56.0) | <0.001 |
| Female | 36,411 (45.2) | 3152 (43.1) | 4786 (39.9) | 2535 (39.6) | 25,076 (47.4) | 862 (44.0) | |
| Age, y (mean ± SD) † | 55.9 ± 12.4 | 53.2 ± 12.7 | 53.6 ± 12.6 | 54.5 ± 12.4 | 56.7 ± 12.2 | 62.3 ± 10.9 | <0.001 |
| 20–44 | 14,768 (18.3) | 1803 (24.7) | 2913 (24.3) | 1315 (20.6) | 8618 (16.3) | 119 (6.1) | <0.001 |
| 45–54 | 23,469 (29.1) | 2187 (29.9) | 3560 (29.7) | 2078 (32.5) | 15,287 (28.9) | 357 (18.2) | |
| 55–64 | 21,470 (26.7) | 1900 (26.0) | 3148 (26.3) | 1651 (25.8) | 14,170 (26.8) | 601 (30.7) | |
| 65+ | 20,833 (25.9) | 1419 (19.4) | 2368 (19.8) | 1355 (21.2) | 14,810 (28.0) | 881 (45.0) | |
| Income level | |||||||
| Medical Aid | 4491 (5.6) | 179 (2.5) | 707 (5.9) | 465 (7.3) | 3008 (5.7) | 132 (6.7) | <0.001 |
| Decile 1–2 | 11,895 (14.8) | 813 (11.1) | 1567 (13.1) | 997 (15.6) | 8181 (15.5) | 337 (17.2) | |
| Decile 3–4 | 11,126 (13.8) | 794 (10.9) | 1559 (13.0) | 995 (15.6) | 7490 (14.2) | 288 (14.7) | |
| Decile 5–6 | 13,418 (16.7) | 1043 (14.3) | 1988 (16.6) | 1086 (17.0) | 8989 (17.0) | 312 (15.9) | |
| Decile 7–8 | 17,182 (21.3) | 1589 (21.7) | 2696 (22.5) | 1368 (21.4) | 11,106 (21.0) | 423 (21.6) | |
| Decile 9–10 | 22,428 (27.8) | 2891 (39.6) | 3472 (29.0) | 1488 (23.3) | 14,111 (26.7) | 466 (23.8) | |
| Residence | |||||||
| Seoul | 16,976 (21.1) | 2530 (34.6) | 2123 (17.7) | 1025 (16.0) | 10,895 (20.6) | 403 (20.5) | <0.001 |
| Metropolitan | 20,251 (25.1) | 1483 (20.3) | 3180 (26.5) | 1735 (27.1) | 13,568 (25.7) | 285 (14.6) | |
| City and County | 43,313 (53.8) | 3296 (45.1) | 6686 (55.8) | 3639 (56.9) | 28,422 (53.7) | 1270 (64.9) | |
| CCI | |||||||
| 0 | 35,811 (44.5) | 2974 (40.7) | 5506 (45.9) | 3078 (48.1) | 23,151 (43.8) | 1102 (56.3) | <0.001 |
| 1 | 20,289 (25.2) | 1756 (24.0) | 2804 (23.4) | 1522 (23.8) | 13,725 (26.0) | 482 (24.6) | |
| 2+ | 24,440 (30.3) | 2579 (35.3) | 3679 (30.7) | 1799 (28.1) | 16,009 (30.3) | 374 (19.1) | |
| Outpatient Care Use (mean ± SD) † | |||||||
| No. Outpatient Visits | 20.6 ± 17.9 | 12.1 ± 10.6 | 15.4 ± 13.1 | 18.0 ± 15.5 | 23.2 ± 19.4 | 20.2 ± 13.9 | <0.001 |
| MPR | 0.41 ± 0.41 | 0.34 ± 0.40 | 0.41 ± 0.40 | 0.37 ± 0.39 | 0.42 ± 0.42 | 0.50 ± 0.41 | <0.001 |
| Hospitalization | Types of USC | ||||
|---|---|---|---|---|---|
| TGHs | GHs | Hospitals | Clinics | PHCs | |
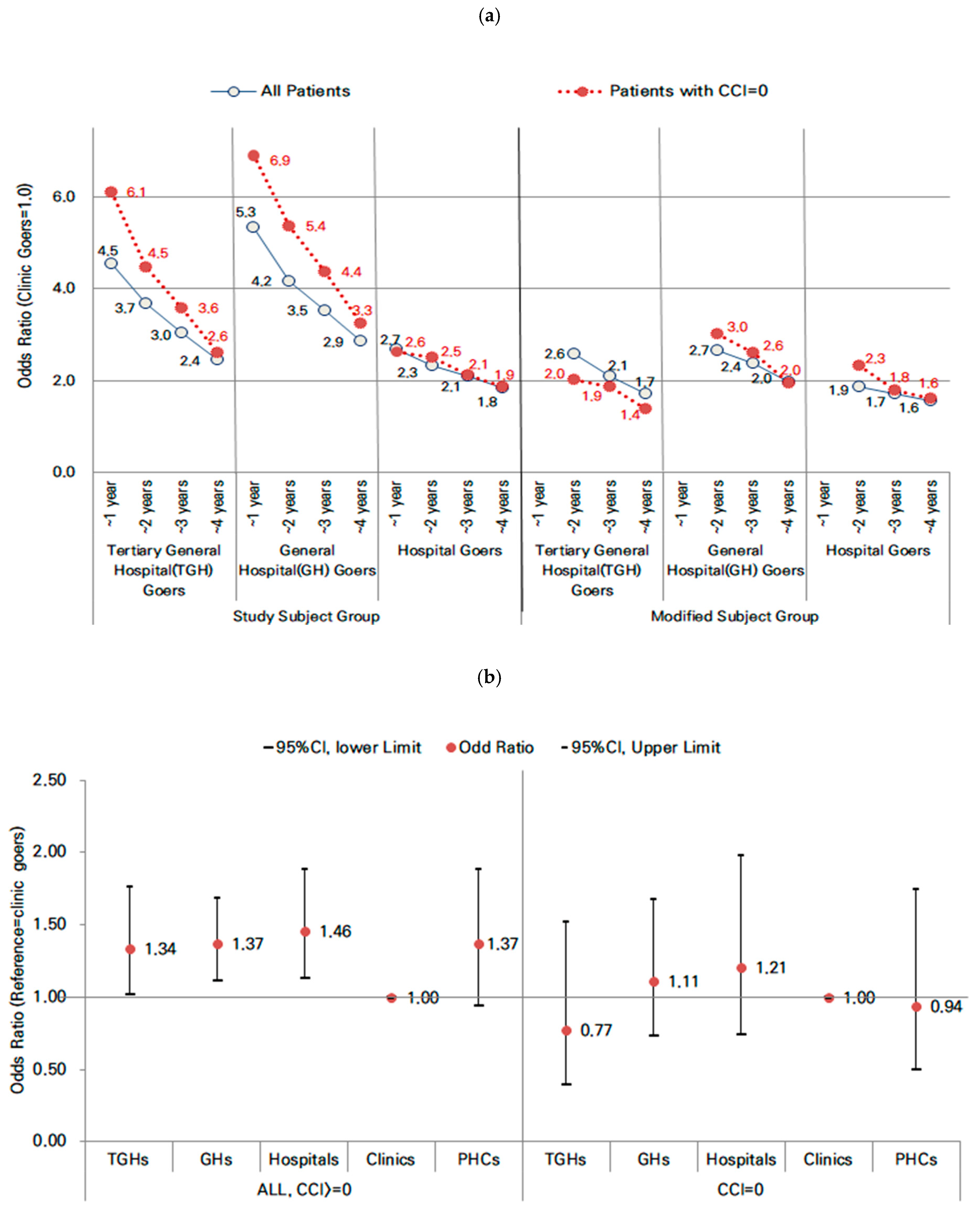
| Study Subject | |||||
| All (n = 80,540), n (%) | 7309 (9.07) | 11,989 (14.89) | 6399 (7.95) | 52,885 (65.66) | 1958 (2.43) |
| In 1 year, N. of cases (%) | 279 (0.35) | 573 (0.71) | 162 (0.20) | 511 (0.63) | 15 (0.02) |
| OR * (95% CI) | 4.54 (3.90–5.28) | 5.33 (4.72–6.03) | 2.68 (2.24–3.21) | 1.00 | 0.72 (0.43–1.21) |
| In 2 years, N. of cases (%) | 409 (0.51) | 808 (1.00) | 256 (0.32) | 952 (1.18) | 37 (0.05) |
| OR * (95% CI) | 3.68 (3.26–4.16) | 4.16 (3.78–4.59) | 2.32 (2.02–2.67) | 1.00 | 0.96 (0.69–1.34) |
| In 3 years, N. of cases (%) | 493 (0.61) | 995 (1.24) | 336 (0.42) | 1415 (1.76) | 55 (0.07) |
| OR * (95% CI) | 3.03 (2.72–3.37) | 3.53 (3.24–3.84) | 2.09 (1.84–2.36) | 1.00 | 0.95 (0.72–1.25) |
| In 4 years, N. of cases (%) | 601 (0.75) | 1211 (1.50) | 450 (0.56) | 2170 (2.69) | 81 (0.10) |
| OR * (95% CI) | 2.44 (2.21–2.68) | 2.85 (2.64–3.10) | 1.84 (0.71–1.12) | 1.00 | 0.89 (0.71–1.12) |
| CCI † = 0 (n = 35,811), n (%) | 2974 (8.30) | 5506 (15.37) | 3078 (8.60) | 23,151 (64.65) | 1102 (3.08) |
| In 1 year, N. of cases (%) | 115 (0.32) | 264 (0.74) | 60 (0.17) | 173 (0.48) | 7 (0.02) |
| OR * (95% CI) | 6.09 (4.77–7.77) | 6.90 (5.67–8.40) | 2.63 (1.96–3.54) | 1.00 | 0.76 (0.36–1.63) |
| In 2 years, N. of cases (%) | 140 (0.39) | 339 (0.95) | 95 (0.27) | 296 (0.83) | 15 (0.04) |
| OR * (95% CI) | 4.46 (3.61–5.50) | 5.36 (4.57–6.30) | 2.50 (1.98–3.17) | 1.00 | 0.92 (0.54–1.55) |
| In 3 years, N. of cases (%) | 166 (0.46) | 404 (1.13) | 119 (0.33) | 445 (1.24) | 21 (0.06) |
| OR * (95% CI) | 3.57 (2.96–4.30) | 4.37 (3.80–5.03) | 2.12 (1.73–2.61) | 1.00 | 0.83 (0.53–1.30) |
| In 4 years, N. of cases (%) | 190 (0.53) | 470 (1.31) | 163 (0.46) | 710 (1.98) | 37 (0.1) |
| OR * (95% CI) | 2.60 (2.19–3.07) | 3.25 (2.88–3.68) | 1.86 (1.56–2.22) | 1.00 | 0.89 (0.64–1.25) |
| Modified Subject: Excluding patients hospitalized within 1 year from study subject | |||||
| All (n = 79,000), n (%) | 7030 (8.90) | 11,416 (14.45) | 6237 (7.89) | 52,374 (66.30) | 1943 (2.46) |
| In 2 years, N. of cases (%) | 130 (1.85) | 235 (2.06) | 94 (1.51) | 441 (0.84) | 22 (1.13) |
| OR * (95% CI) | 2.58 (2.11–3.16) | 2.65 (2.25–3.11) | 1.86 (1.49–2.34) | 1.00 | 1.25 (0.81–1.92) |
| In 3 years, N. of cases (%) | 214 (3.04) | 422 (3.70) | 174 (2.79) | 904 (1.73) | 40 (2.06) |
| OR * (95% CI) | 2.08 (1.79–2.43) | 2.37 (2.10–2.67) | 1.72 (1.45–2.02) | 1.00 | 1.08 (0.78–1.49) |
| In 4 years, N. of cases (%) | 322 (4.58) | 638 (5.59) | 288 (4.62) | 1659 (3.17) | 66 (3.4) |
| OR * (95% CI) | 1.72 (1.52–1.95) | 1.97 (1.80–2.17) | 1.56 (1.37–1.78) | 1.00 | 0.95 (0.73–1.22) |
| CCI † = 0 (n = 35,192), n (%) | 2859 (8.12) | 5242 (14.90) | 3018 (8.58) | 22,978 (65.29) | 1095 (3.11) |
| In 2 years, N. of cases (%) | 25 (0.87) | 75 (1.43) | 35 (1.16) | 123 (0.54) | 8 (0.73) |
| OR * (95% CI) | 2.01 (1.30–3.11) | 3.00 (2.24–4.02) | 2.32 (1.58–3.39) | 1.00 | 1.08 (0.53–2.23) |
| In 3 years, N. of cases (%) | 51 (1.78) | 140 (2.67) | 59 (1.95) | 272 (1.18) | 14 (1.28) |
| OR * (95% CI) | 1.85 (1.36–2.52) | 2.59 (2.10–3.20) | 1.79 (1.35–2.38) | 1.00 | 0.85 (0.50–1.47) |
| In 4 years, N. of cases (%) | 75 (2.62) | 206 (3.93) | 103 (3.41) | 537 (2.34) | 30 (2.74) |
| OR * (95% CI) | 1.39 (1.08–1.78) | 1.95 (1.65–2.30) | 1.60 (1.29–1.99) | 1.00 | 0.91 (0.63–1.33) |
| Mortality | Types of USC | ||||
|---|---|---|---|---|---|
| TGHs | GHs | Hospitals | Clinics | PHCs | |
| All patients (n = 80,540) | |||||
| Patients, n (%) | 7309(9.07) | 11,989(14.89) | 6399 (7.95) | 52,885 (65.66) | 1958 (2.43) |
| In 4 years, N. of deaths (%) | 60(0.07) | 117(0.15) | 71 (0.09) | 437 (0.54) | 30 (0.04) |
| OR * (95% CI) | 1.34(1.02-1.77) | 1.37(1.11-1.69) | 1.46 (1.13-1.89) | 1.00 | 1.37 (0.94-1.89) |
| Patients with CCI † of = 0 (n = 35,811) | |||||
| Patients, n (%) | 2974(8.30) | 5506(15.38) | 3078(8.60) | 23,151(64.65) | 1102(3.08) |
| In 4 years, N. of deaths (%) | 9(0.03) | 27(0.08) | 18(0.05) | 137(0.38) | 11(0.03) |
| OR * (95% CI) | 0.77(0.39-1.53) | 1.11(0.73-1.68) | 1.21 (0.74-1.99) | 1.00 | 0.94 (0.50-1.75) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, H.-C.; Hong, J.-S. Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study. Healthcare 2022, 10, 334. https://doi.org/10.3390/healthcare10020334
Kang H-C, Hong J-S. Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study. Healthcare. 2022; 10(2):334. https://doi.org/10.3390/healthcare10020334
Chicago/Turabian StyleKang, Hee-Chung, and Jae-Seok Hong. 2022. "Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study" Healthcare 10, no. 2: 334. https://doi.org/10.3390/healthcare10020334






