Workshop on Blood Loss Quantification in Obstetrics: Improving Medical Student Learning through Clinical Simulation
Abstract
:1. Introduction
2. Materials and Methods
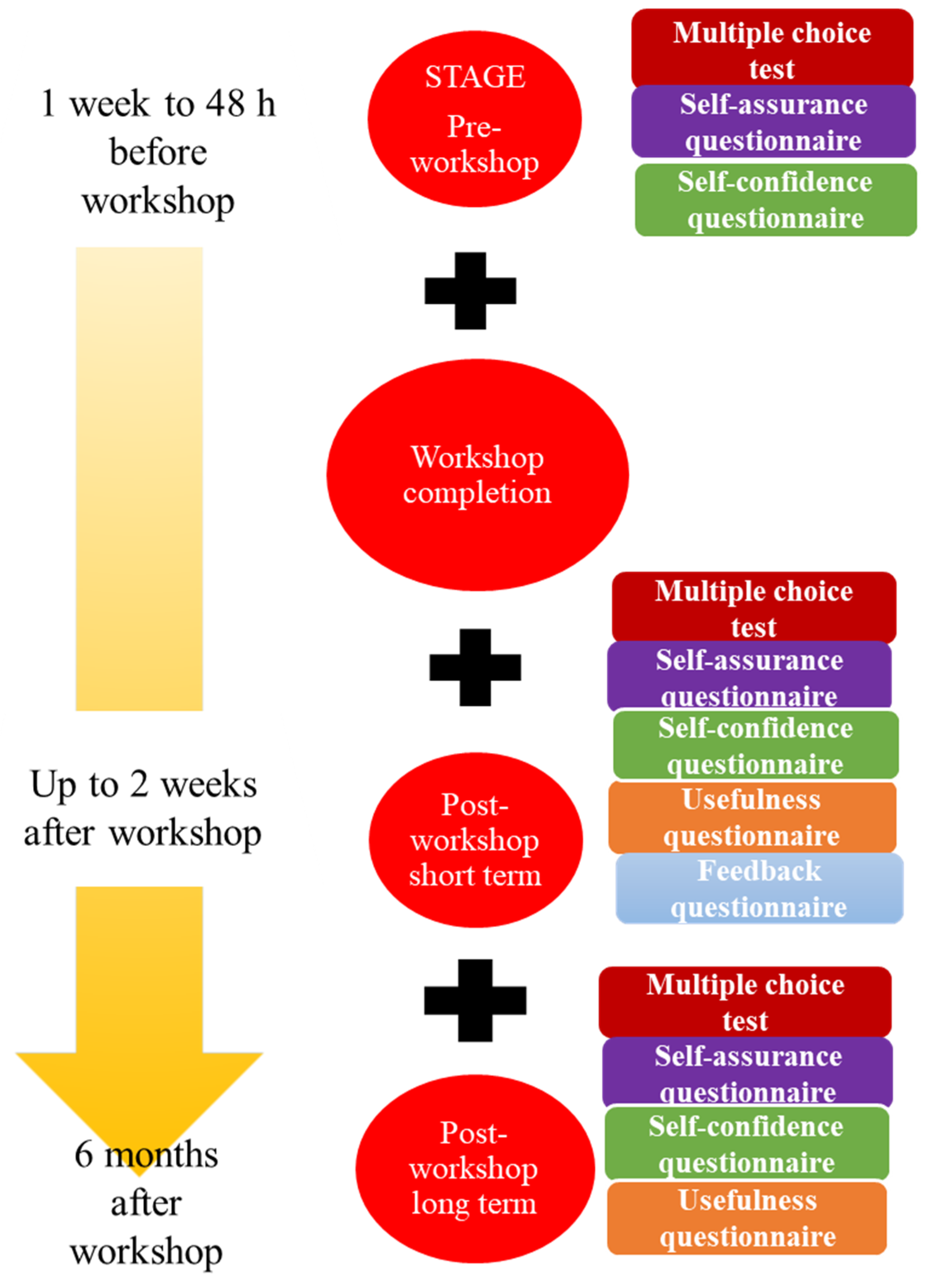
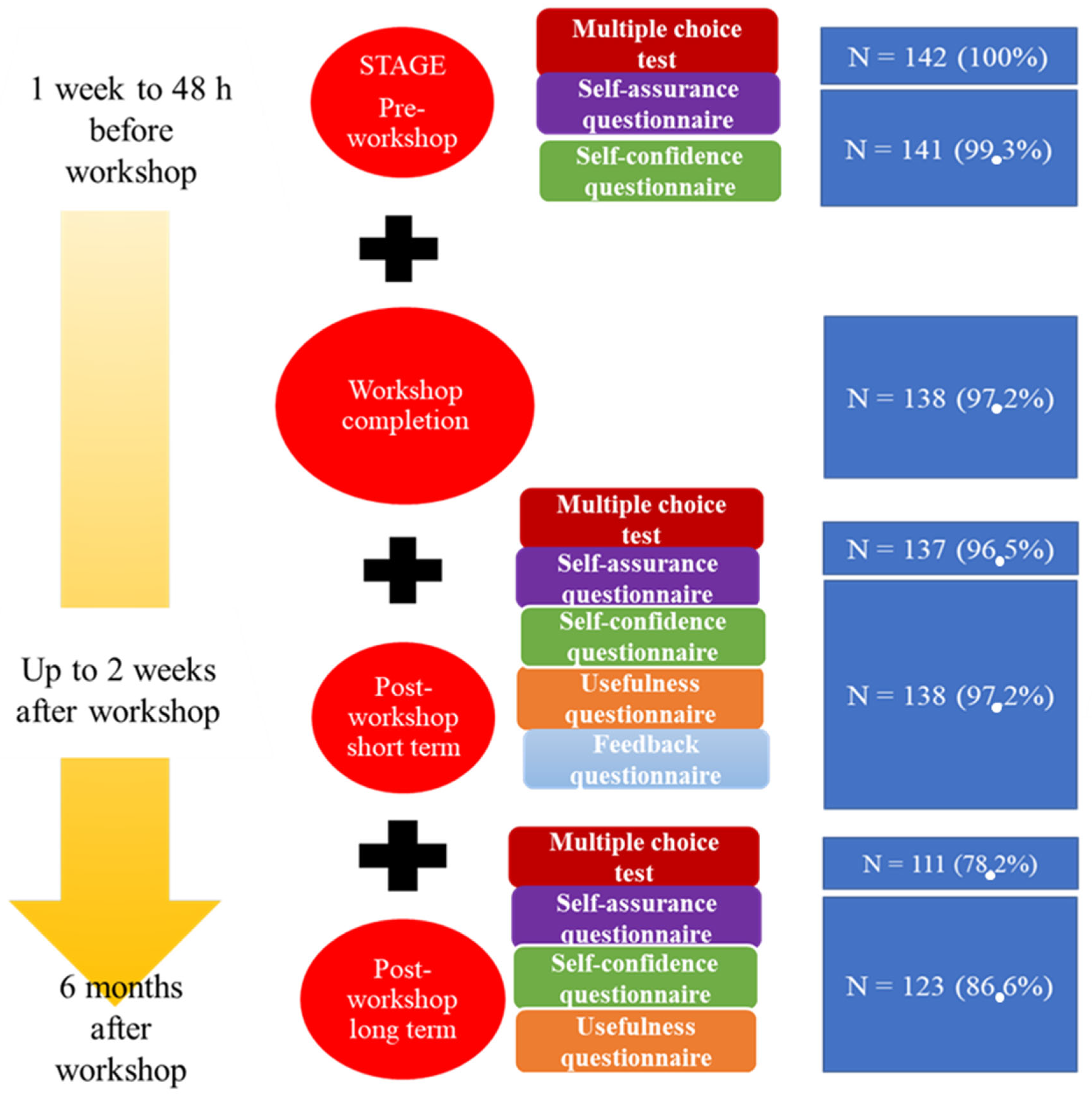
- Stage 1: This was executed “on-line” via a virtual platform (www.aleesca.es/moodle, accessed on 18 August 2021). Here, the students had access to descriptions of the workshop along with the theory (presentations and videos) related to blood loss quantification in obstetrics. The tasks to be completed were:
- A.
- Multiple choice test (MCT), in which 20 questions should be answered in 30 min to assess theoretical–practical knowledge pertaining to the subject. For each correct answer, 0.5 points were added (no points were subtracted for incorrect answers).
- B.
- Two self-administered questionnaires to assess the self-assurance and self-confidence of the students when facing a similar clinical situation. Replies were scored according to a semiquantitative Likert scale [13] (Appendix A).
- Stage 2: This was the actual clinical simulation workshop completed. Over a period of 1.5 hours, the students, in groups of 8–10, were given a brief lecture on how to quantify blood loss postpartum or during a caesarean section. The students then put their understanding of the topic into practice in different clinical scenarios with the help of a mannequin and artificial blood. Students were encouraged to ask questions during the task. A clinical scenario of a patient who had experienced postpartum haemorrhage after a normal vaginal delivery was depicted. To do this, a mannequin in the shape of a female pelvis was used, with a plastic blood collection bag located under the pelvis and textile material (compresses, gauze pads and underpads) soaked in blood. The student had to perform a gravimetric quantification of the blood lost by the patient during the immediate postpartum period. Subsequently, the students were able to design other simulated clinical scenarios (caesarean section, instrumental delivery) with the same material, to continue practicing gravimetric quantification in other situations.
- Stages 3 and 4: These stages were completed on-line and included tasks such as:
- C.
- A similar MCT to that of stage 1, but with questions designed to compare the student’s understanding of the topic and practical skills before and at two time points after the workshop.
- D.
- Three self-administered questionnaires designed to assess their self-assurance, self-confidence and perception of usefulness of the workshop, and to gain feedback (Appendix A).
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Self-Confidence, Self-Assurance, Usefulness and Feedback Questionnaires
| Self-assurance | ||||||||||
| Question | Reply | |||||||||
| 1. | How would you describe your theoretical knowledge of blood loss quantification? | Poor (0–2) | Medium (3–4) | Good (5–6) | Very good (7–8) | Excellent (9–10) | ||||
| 2. | How would you describe your practical knowledge of blood loss quantification? | Poor (0–2) | Medium (3–4) | Good (5–6) | Very good (7–8) | Excellent (9–10) | ||||
| 3. | How would you describe your practical skills in managing obstetric blood loss? | Poor (0–2) | Medium (3–4) | Good (5–6) | Very good (7–8) | Excellent (9–10) | ||||
| Self-confidence | ||||||||||
| Question | Reply | |||||||||
| 1. | How confident are you at dealing with obstetric blood loss? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 2. | How confident are you at controlling blood loss? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 3. | How confident are you at controlling the initial situation? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 4. | How confident are you at quantifying blood loss visually (subjective)? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 5. | How confident are you at quantifying blood loss gravimetrically (objective)? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 6. | How confident are you at differentiating between mild and severe blood loss? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 7. | How confident are you at coordinating with the medical staff present? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 8. | How confident are you at preventing severe blood loss? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 9. | How confident would you feel assisting a clinician during a blood loss episode? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 10. | How confident would you feel assisting an obstetrician during a blood loss episode? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 11. | How confident would you feel under the supervision of a resident doctor? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| 12. | How confident would you feel assisting a blood loss episode without supervision? | Not at all (0–2) | Scarcely (3–4) | Somewhat (5–6) | Confident (7–8) | Very (9–10) | ||||
| Perceived usefulness | ||||||||||
| Statement | Agreement level | |||||||||
| 1. | I found the workshop useful | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 2. | My theoretical knowledge of obstetric blood loss has improved | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 3. | My practical knowledge of obstetric blood loss has improved | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 4. | This workshop will reduce my stress levels when dealing with a blood loss episode in the future. | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 5. | This workshop is necessary to gain theoretical knowledge | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 6. | This workshop is necessary to gain practical knowledge | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| 7. | This workshop should be obligatory for all medical undergraduates | No, not at all (0–2) | No, not really (3–4) | Indifferent (5–6) | Yes (7–8) | Yes, definitely (9–10) | ||||
| Feedback | ||||||||||
| Question | Reply (mark one or several) | |||||||||
| 1. | How did you feel about assisting the workshop? | Curious | Unsure | Anxious | None of these | |||||
| 2. | How did you feel when conducting the simulation? | Sure of yourself | Confused | Stressed/tense | None of these | |||||
| 3. | How do you feel about the feedback session? | It was useful | It helped me connect with my peers and share our ideas | It was an opportunity to confront each other | None of these | |||||
References
- Vázquez-Mata, G.; Guillamet-Lloveras, A. El entrenamiento basado en la simulación como innovación imprescindible en la formación médica. Educ. Méd. 2009, 12, 149–155. [Google Scholar] [CrossRef] [Green Version]
- Hemorrhage, P. Practice bulletin no. 183: Postpartum hemorrhage: Postpartum hemorrhage. Obstet. Gynecol. 2017, 130, e168–e181. [Google Scholar]
- Bose, P.; Regan, F.; Paterson-Brown, S. Improving the accuracy of estimated blood loss at obstetric haemorrhage using clinical reconstructions. BJOG 2006, 113, 919–924. [Google Scholar] [CrossRef] [PubMed]
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.-B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health 2014, 2, e323–e333. [Google Scholar] [CrossRef] [Green Version]
- Larroca, S.G.-T.; Amor Valera, F.; Herrera, E.A.; Hernandez, I.C.; Lopez, Y.C.; De Leon-Luis, J. Human Development Index of the maternal country of origin and its relationship with maternal near miss: A systematic review of the literature. BMC Pregnancy Childbirth 2020, 20, 224. [Google Scholar]
- Ruiz Labarta, F.J.; Pintado Recarte, M.P.; Joigneau Prieto, L.; Bravo Arribas, C.; Bujan, J.; Ortega, M.A.; De León-Luis, J.A. Factors associated with failure of Bakri balloon tamponade for the management of postpartum haemorrhage. Case series study and systematic review. Healthcare 2021, 9, 295. [Google Scholar] [CrossRef]
- Ruiz Labarta, F.J.; Pintado Recarte, M.P.; Alvarez Luque, A.; Joigneau Prieto, L.; Perez Martín, L.; Gonzalez Leyte, M.; Abizanada Palacio, F.; Ramirez Morillas, F.; Perez Corral, A.; Quintana Ortiz, L.; et al. Outcomes of pelvic arterial embolization in the management of postpartum haemorrhage: A case series study and systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 206, 12–21. [Google Scholar] [CrossRef] [Green Version]
- American College of Obstetricians and Gynecologists. Quantitative Blood Loss in Obstetric Hemorrhage: Acog Committee Opinion, Number 794; ACOG: Washington, DC, USA, 2019. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: Postpartum hemorrhage. Obstet. Gynecol. 2006, 108, 1039–1047. [Google Scholar]
- Street, N.W. Quantification of blood loss: AWHONN practice brief number 1. J. Obstet. Gynecol. Neonatal. Nurs. 2015, 44, 158–160. [Google Scholar] [CrossRef] [PubMed]
- Al-Kadri, H.M.; Dahlawi, H.; Al Airan, M.; Elsherif, E.; Tawfeeq, N.; Mokhele, Y.; Brown, D.; Tamim, H.M. Effect of education and clinical assessment on the accuracy of post partum blood loss estimation. BMC Pregnancy Childbirth 2014, 14, 110. [Google Scholar] [CrossRef] [PubMed]
- Kato, C.; Kataoka, Y. Simulation training program for midwives to manage postpartum hemorrhage: A randomized controlled trial. Nurse Educ. Today 2017, 51, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Matas, A. Diseño del formato de escalas tipo Likert: Un estado de la cuestión. Rev. Electrón. Investig. Educ. 2018, 20, 38–47. [Google Scholar] [CrossRef]
- Mclelland, G.; Tremayne, A.; Carr, B.; Hall, H.; Plummer, V.; Kumar, A.; Corlass, A.; East, C.; Buttigieg, H.; Fernando, S.; et al. Learning together to manage simulated postpartum haemorrhage: Undergraduate midwifery and medical students’ satisfaction with simulation and impact upon self-efficacy. Women Birth. 2019, 32, S6–S7. [Google Scholar] [CrossRef]
- Mohamed, A.E.E.; Mostafa, E.H. Effect of simulation based training on maternity nurses’ performance and self-confidence regarding primary postpartum hemorrhage management. Am. J. Nurs. Res. 2018, 6, 388–397. [Google Scholar] [CrossRef] [Green Version]
- Nelissen, E.; Ersdal, H.; Mduma, E.; Evjen-Olsen, B.; Twisk, J.; Broerse, J.; van Roosmalen, J.; Stekelenburg, J. Clinical performance and patient outcome after simulation-based training in prevention and management of postpartum haemorrhage: An educational intervention study in a low-resource setting. BMC Pregnancy Childbirth 2017, 17. [Google Scholar] [CrossRef] [PubMed]

| Variable | Assessment Method | Qualifier |
|---|---|---|
| Sex | Student characteristic | Qualitative nominal |
| Age | Student characteristic | Quantitative discrete |
| Previous passive or active experience with clinical situations involving more than 1 L of blood loss | Student characteristic | Quantitative discrete 0 occasions; ≥1 occasion |
| Theoretical–practical knowledge | Multiple choice test | Quantitative discrete Score of 0–10 in 0.5-point steps |
| Self-assurance | Self-administered questionnaire | Quantitative discrete Likert scale (0–10) Poor (0–2), medium (3–4), good (5–6), very good (7–8) and excellent (9–10) |
| Self-confidence | Self-administered questionnaire | Quantitative discrete Likert scale (0–10) Not at all confident (0–2), scarcely confident (3–4), somewhat confident (5–6), confident (7–8) and very confident (9–10) |
| Perceived utility | Self-administered questionnaire | Quantitative discrete Likert scale (0–10) Not at all useful (0–2), not really useful (3–4), indifferent (5–6), useful (7–8) and definitely useful (9–10) |
| Feedback | Self-administered questionnaire | Three questions with different non-exclusive answers (students could mark as many options as they wished) Three questions with open answers |
| Results of Multiple Choice Test | |||||||
|---|---|---|---|---|---|---|---|
| Pre-WS (N = 142) | Post-WS 2 Weeks (N = 137) | Short-Term Improvement (μ post—μ pre) (N = 137) | p | Post-WS 6 Months (N =111) | Long-Term Improvement (μ 6 mo—μ 2 wk) (N =111) | p | |
| Score (/10) | 7.47 ± 1.66 | 8.52 ± 1.06 | 1.01 ± 1.60 (8.52–7.47) | <0.05 | 7.47 ± 1.51 | −1.15 ±1.24 (7.47–8.52) | <0.05 |
| Self-Assurance Questionnaire | |||||||
|---|---|---|---|---|---|---|---|
| Pre-WS (N = 141) | Post-WS 2 Weeks (N = 138) | Short-Term Improvement (μ post—μ pre) (N = 138) | p | Post-WS 6 Months (N = 123) | Long-Term Improvement (μ 6 mo—μ 2 wk) (N = 121) | p | |
| 1. Theoretical BLQ knowledge | 4.69 ± 2.21 | 7.37 ± 1.34 | 2.68 (7.37–4.69) | <0.05 | 7.47 ± 1.38 | 0.02 ± 1.36 (7.47–7.37) | 0.88 |
| 2. Practical BLQ knowledge | 4.71 ± 2.27 | 7.72 ± 1.13 | 2.98 (7.72–4.71) | <0.05 | 7.58 ± 1.31 | −0.18 ± 1.16 (7.58–7.72) | 0.09 |
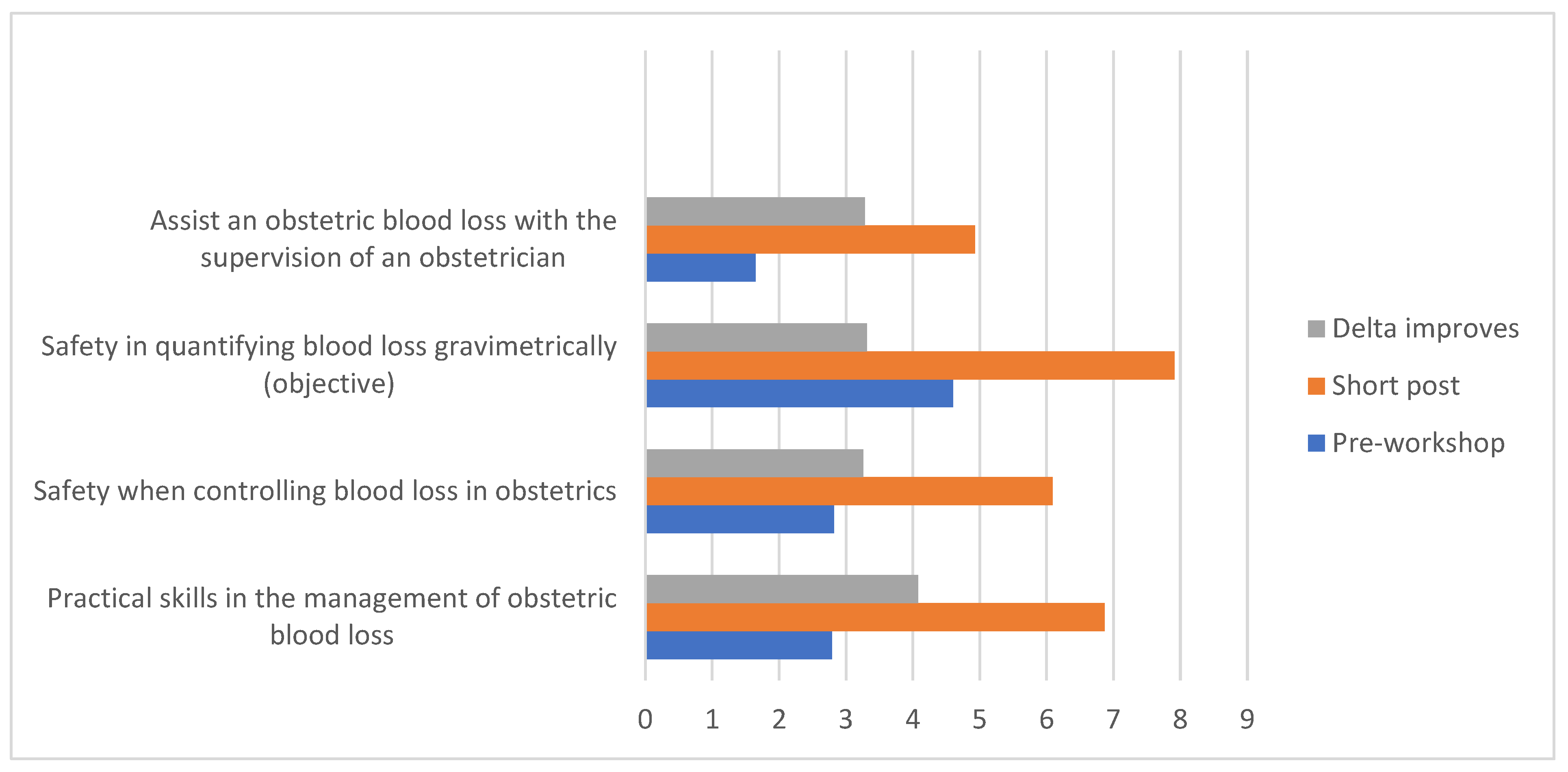
| 3. Practical management skills | 2.79 ± 2.26 | 6.87 ± 1.44 | 4.10 (6.87–2.79) | <0.05 | 6.68 ± 1.53 | −0.27 (6.68–6.87) | <0.05 |
| Self-Confidence Questionnaire | |||||||
|---|---|---|---|---|---|---|---|
| Pre-WS (N = 141) | Post-WS 2 Weeks (N = 138) | Short-Term Improvement (μ post—μ pre) (N = 138) | p | Post-WS 6 Months (N =123) | Long-Term Improvement (μ 6 mo—μ 2 wk) (N = 121) | p | |
| 4. Experience with BLQ | 3.65 ± 2.3 | 6.58 ± 1.43 | 3.02 (6.59–3.57) | <0.05 | 6.45 ± 1.66 | −0.29 (6.43–6.71) | <0.05 |
| 5. Controlling blood loss | 2.82 ± 2.13 | 6.09 ± 1.58 | 3.29 (6.09–2.80) | <0.05 | 6.00 ± 1.79 | −0.26 (5.98–6.24) | 0.093 |
| 6. Controlling initial situation | 2.94 ± 2.07 | 6.05 ± 1.68 | 3.18 (6.06–2.88) | <0.05 | 5.86 ± 1.84 | −0.31 (5.84–6.15) | 0.065 |
| 7. Visual BLQ | 3.70 ± 2.20 | 6.40 ± 1.62 | 2.79 (6.39–3.60) | <0.05 | 6.46 ± 1.65 | −0.11 (6.43–6.55) | 0.457 |
| 8. Gravimetric BLQ | 4.60 ± 2.51 | 7.91 ± 1.30 | 3.35 (7.92–4.57) | <0.05 | 7.24 ± 1.61 | −0.76 (7.24–8.00) | <0.05 |
| 9. Differentiating between mild and severe blood loss | 4.52 ± 2.22 | 7.30 ± 1.37 | 2.79 (6.39–3.60) | <0.05 | 7.11 ± 1.59 | −0.23 (7.10–7.32) | 0.10 |
| 10. Coordinating with other staff | 4.84 ± 2.35 | 7.37 ± 1.43 | 2.58 (7.38–4.80) | <0.05 | 7.32 ± 1.57 | −0.14 (7.30–7.44) | 0.31 |
| 11. Preventing severe blood loss | 3.28 ± 2.16 | 6.36 ± 1.77 | 3.11 (6.36–3.24) | <0.05 | 6.52 ± 1.60 | 0.11 (6.49–6.38) | 0.52 |
| 12. Assisting a physician during blood loss | 4.62 ± 2.44 | 7.20 ± 1.61 | 2.66 (7.22–4.56) | <0.05 | 6.99 ± 1.64 | −0.36 (6.98–7.34) | <0.05 |
| 13. Managing blood loss under supervision of obstetrician | 4.94 ± 2.46 | 7.25 ± 1.62 | 2.39 (7.26–4.88) | <0.05 | 7.10 ± 1.79 | −0.28 (7.08–7.36) | 0.10 |
| 14. Managing blood loss under supervision of a medical intern | 4.55 ± 2.33 | 6.90 ± 1.66 | 2.42 (6.91–4.49) | <0.05 | 6.92 ± 1.80 | −0.10 (6.89–6.99) | 0.55 |
| 15. Managing blood loss without supervision | 1.65 ± 1.90 | 4.93 ± 1.96 | 3.38 (4.94–1.57) | <0.05 | 4.59 ± 2.20 | −0.48 (4.56–5.04) | <0.05 |
| Perceived Usefulness Questionnaire | ||||
|---|---|---|---|---|
| Post-WS 2 Weeks (N = 138) | Post-WS 6 Months (N = 123) | Long-Term Improvement (μ 6 mo—μ 2 wk) (N = 121) | p | |
| 16. WS usefulness | 9.14 ± 1.02 | 8.98 ± 1.19 | −0.16 ± 1.19 (8.98–9.14) | 0.13 |
| 17. Improved BLQ theoretical knowledge | 8.97 ± 1.20 | 8.99 ± 1.11 | 0.06 ± 1.31 (8.98–8.93) | 0.63 |
| 18. Improved BLQ practical knowledge | 9.04 ± 1.06 | 8.68 ± 1.39 | −0.34 ± 1.41 (8.67–9.02) | <0.05 |
| 19. Reduced stress when faced with blood loss | 8.38 ± 1.30 | 8.07 ± 1.56 | −0.34 ± 1.45 (8.06–8.39) | <0.05 |
| 20. WS needed in theoretical terms | 8.96 ± 1.38 | 8.81 ± 1.57 | −0.14 ± 1.82 (8.80–8.94) | 0.40 |
| 21. WS needed in practical terms | 9.31 ± 1.04 | 9.23 ± 1.11 | −0.12 ± 1.08 (9.22–9.34) | 0.24 |
| 22. WS should be obligatory | 9.02 ± 1.39 | 8.85 ± 1.41 | −0.16 ± 1.36 (8.84–8.99) | 0.21 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Labarta, J.; Martínez Martín, A.; Pintado Recarte, P.; González Garzón, B.; Pina Moreno, J.M.; Sánchez Rodríguez, M.; Vallejo Gea, Á.; Sordo, L.; Álvarez-Mon, M.; Ortega, M.A.; et al. Workshop on Blood Loss Quantification in Obstetrics: Improving Medical Student Learning through Clinical Simulation. Healthcare 2022, 10, 399. https://doi.org/10.3390/healthcare10020399
Ruiz-Labarta J, Martínez Martín A, Pintado Recarte P, González Garzón B, Pina Moreno JM, Sánchez Rodríguez M, Vallejo Gea Á, Sordo L, Álvarez-Mon M, Ortega MA, et al. Workshop on Blood Loss Quantification in Obstetrics: Improving Medical Student Learning through Clinical Simulation. Healthcare. 2022; 10(2):399. https://doi.org/10.3390/healthcare10020399
Chicago/Turabian StyleRuiz-Labarta, Javier, Ana Martínez Martín, Pilar Pintado Recarte, Blanca González Garzón, Juan Manuel Pina Moreno, Mercedes Sánchez Rodríguez, África Vallejo Gea, Luis Sordo, Melchor Álvarez-Mon, Miguel A. Ortega, and et al. 2022. "Workshop on Blood Loss Quantification in Obstetrics: Improving Medical Student Learning through Clinical Simulation" Healthcare 10, no. 2: 399. https://doi.org/10.3390/healthcare10020399
APA StyleRuiz-Labarta, J., Martínez Martín, A., Pintado Recarte, P., González Garzón, B., Pina Moreno, J. M., Sánchez Rodríguez, M., Vallejo Gea, Á., Sordo, L., Álvarez-Mon, M., Ortega, M. A., Arribas, C. B., & De León-Luis, J. A. (2022). Workshop on Blood Loss Quantification in Obstetrics: Improving Medical Student Learning through Clinical Simulation. Healthcare, 10(2), 399. https://doi.org/10.3390/healthcare10020399









