Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
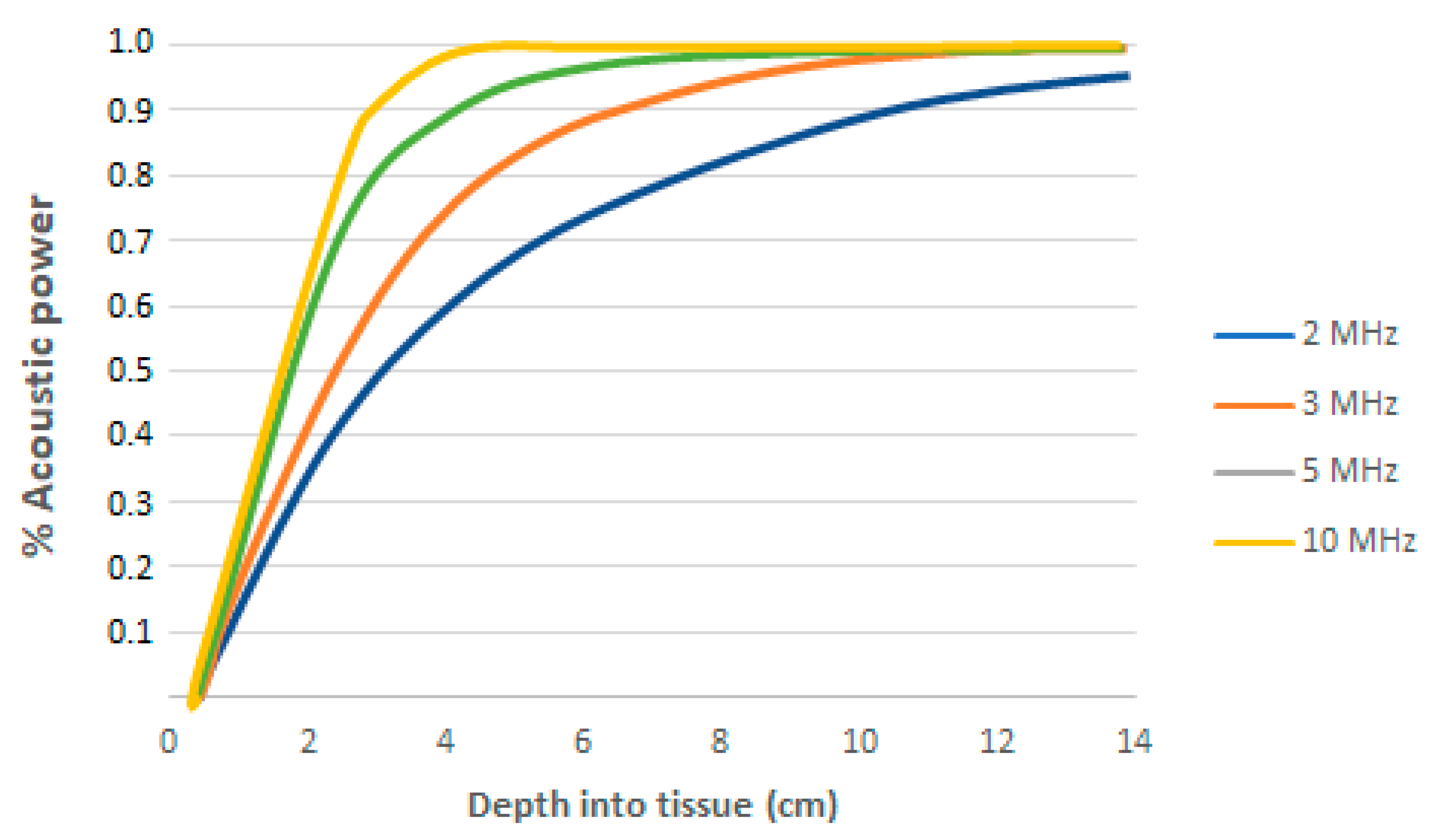
3.1. Propagation and Absorption of Ultrasound
- (1)
- A Mechanical index (MI), which is the index that indicates the mechanical damage that the device can produce (i.e., from what value the inertial cavitation starts).
- (2)
- Thermal index (TI), whose value, if exceeded, produces damage by heating the tissue.
3.2. Possible Effects on Humans
3.3. Ultrasound in the Health Field and the Workplace Environment
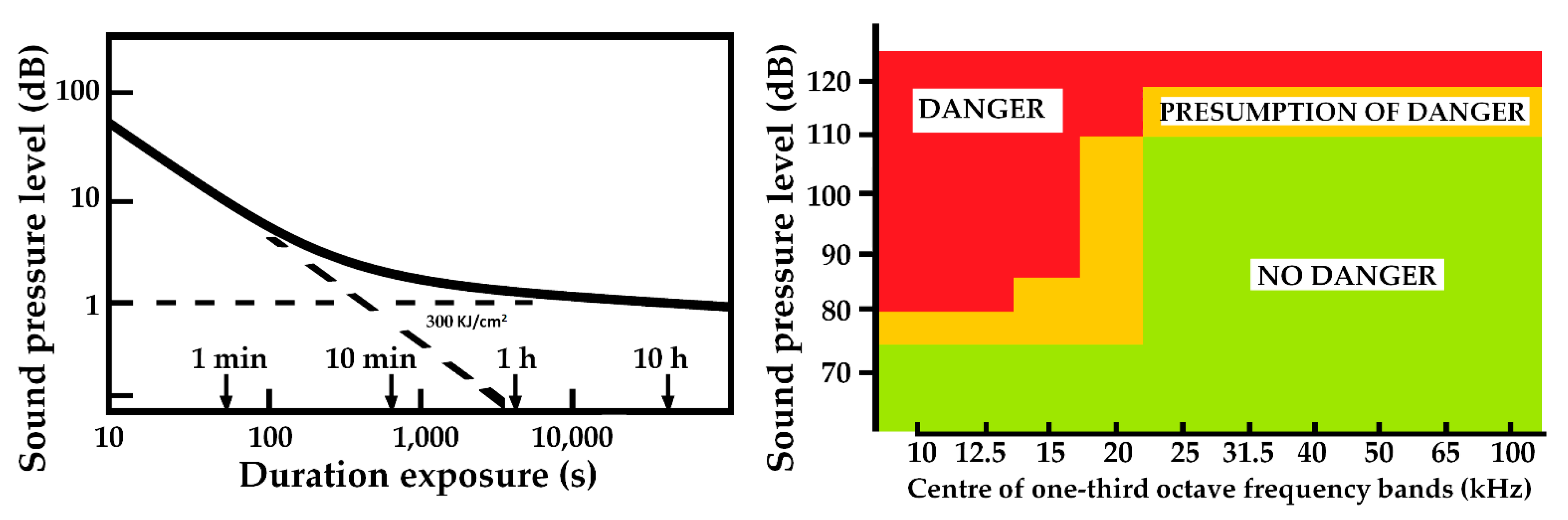
3.4. Legislation
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dávila, F.; Barros, L.A.; Reynolds, J.; Lewis, A.J.; Mogollón, I.R. El ultrasonido: Desde el murciélago hasta la cardiología no invasiva. Rev. Colomb. De Cardiol. 2017, 24, 191–195. [Google Scholar] [CrossRef] [Green Version]
- INSHT. NTP 205 Ultrasonidos: Exposición Laboral. 1985. Available online: https://www.insst.es/documents/94886/327166/ntp_205.pdf/440b750d-afe2-4a99-af33-75c16f4adf9d (accessed on 17 April 2020).
- Isbert, A.C. Diseño Acústico de Espacios Arquitectónicos; Univ. Politèc. de Catalunya: Barcelona, Spain, 1998. [Google Scholar]
- Villaseñor, C.P.; Palacios, M.M.; González, A.B. Principios físicos básicos del ultrasonido. Investig. En Discapac. 2012, 1, 25–34. [Google Scholar]
- Humphrey, V.F. Ultrasound and matter-Physical interactions. Prog. Biophys. Mol. Biol. 2007, 93, 195–211. [Google Scholar] [CrossRef] [PubMed]
- Health Protection Agency. Health Effects of Exposure to Ultrasound and Infrasound Report of the Independent Advisory Group on Non-ionising Radiation; Health Protection Agency: 2010; pp. 1–180. Available online: http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1265028759717 (accessed on 28 October 2020).
- Koton, J. Przemysłowe źródła hałasu ultradźwiękowego, Industrial sources of ultrasonic noise. Bezpieczeństwo Pracy 1988, 38, 11–15. (In Polish) [Google Scholar]
- Mikulski, W.; Smagowska, B. Ultrasonic noise at selected workplaces (paper No. 903). In Proceedings of the Thirteenth International Congress on Sound and Vibration [CD-ROM], Vienna, Austria, 2–6 July 2006. [Google Scholar]
- Pawlaczyk-Łuszczyńska, M.; Dudarewicz, A.; Śliwińska-Kowalska, M. Źródła ekspozycji zawodowej na hałas ultradźwiękowy—Ocena wybranych urządzeń. Sources of occupational exposure to ultrasonic noise—Evaluation of selected devices. Med. Pract. 2007, 58, 105–106. Available online: http://www.imp.lodz.pl/upload/oficyna/artykuly/pdf/full/2007/02-Pawlaczyk.pdf (accessed on 28 March 2013). (In Polish).
- VDI 2058 Blatt 2:2017-02; Beurteilung von Lärm hinsichtlich Gehörgefährdung. VDI-Fachgesellschaften: Düsseldorf, Germany, 2020.
- VDI 2058 Blatt 2:1988-06; Beurteilung von Lärm hinsichtlich Gehörgefährdung. VDI-Fachgesellschaften: Düsseldorf, Germany, 1988.
- VDI 3766:2012-09; Ultraschall-Arbeitsplatz-Messung, Bewertung, Beurteilung und Minderung. VDI-Fachgesellschaften: Düsseldorf, Germany, 2012.
- Śliwiński, A. Ultradźwięki i ich zastosowania. In Ultrasound and Their Applications; WNT: Warszawa, Poland, 2001. [Google Scholar]
- ter Haar, G. The Safe Use of Ultrasound in Medical Diagnosis, 3rd ed.; eBook; The British Institute of Radiology: London, UK, 2012; ISBN 978-0-905749-79-2. [Google Scholar]
- Martínez Morillo, M. Manual de Medicina Física; Harcourt Brace: Madrid, Spain, 1998. [Google Scholar]
- Hütter-Becker, A. Terapia Física; Editorial Paidotribo: Barcelona, Spain, 2005; pp. 211–219. [Google Scholar]
- Walker, F.O.; Cartwright, M.S. Principios Básicos de Ecografía. Ecografía Neuromuscul 2012, 1–23. Available online: http://media.axon.es/pdf/89612.pdf (accessed on 14 December 2020).
- Valentim da Silva, R.M.; Froes Meyer, P.; Ranaco Santos, B.; de Oliveira Félix, J.L.; Ronzio, O.A. Efectos del ultrasonido de alta potencia en la adiposidad localizada. Fisioterapia 2015, 37, 55–59. [Google Scholar] [CrossRef]
- Wu, J. Shear stress in cells generated by ultrasound. Prog. Biophys. Mol. Biol. 2007, 93, 363–373. [Google Scholar] [CrossRef]
- Leighton, T.G. What is ultrasound? Prog. Biophys. Mol. Biol. 2007, 93, 130–137. [Google Scholar] [CrossRef]
- Rodríguez Martín, J. Electroterapia en Fisioterapia; Editorial Médica Panamericana: Madrid, Spain, 2000; pp. 513–516. [Google Scholar]
- Szabo, T.L. Diagnostic Ultrasound Imaging: Inside Out. Diagnostic Ultrasound Imaging: Inside Out; Elsevier Inc.: Amsterdam, The Netherlands, 2004; pp. 1–549. [Google Scholar] [CrossRef] [Green Version]
- Dewbury, K. Ultrasound teaching manual. Clin. Radiol. 1999, 54, 700. [Google Scholar] [CrossRef]
- O’Boyle, M.K. Color Atlas of Ultrasound Anatomy. Am. J. Roentgenol. 2005, 184, 1371. [Google Scholar] [CrossRef]
- Duck, F.A. Medical and non-medical protection standards for ultrasound and infrasound. Prog. Biophys. Mol. Biol. 2007, 93, 176–191. [Google Scholar] [CrossRef] [PubMed]
- American Institute of Ultrasound in Medicine. Acoustic Output Measurement Standard for Diagnostic Ultrasound Equipment; American Institute of Ultrasound in Medicine: Laurel, MD, USA, 1998. [Google Scholar]
- National Electrical Manufacturers Association. Standard for Real-Time Display of Thermal and Mechanical Acoustic Output Indices on Diagnostic Ultrasound Equipment; National Electrical Manufacturers Association: Arlington, VA, USA, 2004. [Google Scholar]
- Ellwart, J.W.; Brettel, H.; Kober, L.O. Cell membrane damage by ultrasound at different cell concentrations. Ultrasound Med. Biol. 1988, 14, 43–50. [Google Scholar] [CrossRef]
- Brayman, A.A.; Doida, Y.; Miller, M.W. Apparent contribution of respiratory gas exchange to the in-vitro “cell density effect” in ultrasonic cell lysis. J. Acoust. Soc. Am. 1992, 91, 2430. [Google Scholar] [CrossRef]
- Taylor, K.J.W.; Newman, D.L. Electrophoretic mobility of Ehrlich cell suspensions exposed to ultrasound of varying parameters. Phys. Med. Biol. 1972, 17, 270–276. [Google Scholar] [CrossRef]
- Smith, N.B.; Temkin, J.M.; Shapiro, F.; Hynynen, K. Thermal effects of focused ultrasound energy on bone tissue. Ultrasound Med. Biol. 2001, 27, 1427–1433. [Google Scholar] [CrossRef]
- Claes, L.; Willie, B. The enhancement of bone regeneration by ultrasound. Prog. Biophys. Mol. Biol. 2007, 93, 384–398. [Google Scholar] [CrossRef]
- Chang, W.H.S.; Sun, J.S.; Chang, S.P.; Lin, J.C. Study of Thermal Effects of Ultrasound Stimulation on Fracture Healing. Bioelectromagnetics 2002, 23, 256–263. [Google Scholar] [CrossRef]
- Dyson, M.; Brookes, M. Stimulation of bone repair by ultrasound. Ultrasound Med. Biol. 1983, 8 (Suppl. S2), 61–66. [Google Scholar] [CrossRef]
- Dinno, M.A.; Dyson, M.; Young, S.R.; Mortimer, A.J.; Hart, J.; Crum, L.A. The significance of membrane changes in the safe and effective use of therapeutic and diagnostic ultrasound. Phys. Med. Biol. 1989, 34, 1543–1552. [Google Scholar] [CrossRef]
- Warden, S.J.; Favaloro, J.M.; Bennell, K.L.; McMeeken, J.M.; Ng, K.W.; Zajac, J.D.; Wark, J.D. Low-intensity pulsed ultrasound stimulates a bone-forming response in UMR-106 cells. Biochem. Biophys. Res. Commun. 2001, 286, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Kieler, H.; Cnattingius, S.; Haglund, B.; Palmgren, J.; Axelsson, O. Sinistrality—A side-effect of prenatal sonography: A comparative study of young men. Epidemiology 2001, 12, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Salvesen, K.Å. EFSUMB: Safety tutorial: Epidemiology of diagnostic ultrasound exposure during pregnancy—European committee for medical ultrasound safety (ECMUS). Eur. J. Ultrasound 2002, 15, 165–171. [Google Scholar] [CrossRef]
- Salvesen, K.Å. Ultrasound in pregnancy and non-right handedness: Meta-analysis of randomized trials. Ultrasound Obstet. Gynecol. 2011, 38, 267–271. [Google Scholar] [CrossRef]
- Grigor, E. Effect of ultrasonic vibrations on personnel working with ultrasonic equipment. Sov. Phys. Acoust. 1966, 2, 426–427. [Google Scholar]
- Williams, A.R.; Miller, D.L. Photometric detection of ATP release from human erythrocytes exposed to ultrasonically activated gas-filled pores. Ultrasound Med. Biol. 1980, 6, 251–256. [Google Scholar] [CrossRef]
- Morton, K.I.; Ter Haar, G.R.; Stratford, I.J.; Hill, C.R. The role of cavitation in the interaction of ultrasound with V79 Chinese hamster cells in vitro. Br. J. Cancer 1982, 45 (Suppl. S5), 147–150. [Google Scholar]
- Fatemi, M.; Alizad, A.; Greenleaf, J.F. Characteristics of the audio sound generated by ultrasound imaging systems. J. Acoust. Soc. Am. 2005, 117, 1448–1455. [Google Scholar] [CrossRef]
- Campbell, J.D.; Elford, R.W.; Brant, R.F. Case-control study of prenatal ultrasonography exposure in children with delayed speech. CMAJ 1993, 149, 1435–1440. [Google Scholar] [CrossRef] [Green Version]
- Acton, W.I.; Carson, M.B. Auditory and subjective effects of airborne noise from industrial ultrasonic sources. Br. J. Ind. Med. 1967, 24, 297–304. [Google Scholar] [CrossRef] [Green Version]
- Basta, G.; Venneri, L.; Lazzerini, G.; Pasanisi, E.; Pianelli, M.; Vesentini, N.; Picano, E. In vitro modulation of intracellular oxidative stress of endothelial cells by diagnostic cardiac ultrasound. Cardiovasc. Res. 2003, 58, 156–161. [Google Scholar] [CrossRef] [Green Version]
- Grazia Andreassi, M.; Venneri, L.; Picano, E. Cardiac imaging: The biological effects of diagnostic cardiac ultrasound. Prog. Biophys. Mol. Biol. 2007, 93, 399–410. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.L. Overview of experimental studies of biological effects of medical ultrasound caused by gas body activation and inertial cavitation. Prog. Biophys. Mol. Biol. 2007, 93, 314–330. [Google Scholar] [CrossRef] [PubMed]
- Mornstein, V. Cavitation-induced risks associated with contrast agents used in ultrasonography. Eur. J. Ultrasound 1997, 5, 101–111. [Google Scholar] [CrossRef]
- Cosyns, B.; Weytjens, C.; Vanderhoogstrate, M.; Daniels, C.; Schoors, D.; Van Camp, G. Tissue Doppler imaging does not show infraclinical alteration of myocardial function after contrast echocardiography. Eur. J. Echocardiogr. 2005, 6, 238–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsutsui, J.M.; Elhendy, A.; Xie, F.; O’Leary, E.L.; McGrain, A.C.; Porter, T.R. Safety of dobutamine stress real-time myocardial contrast echocardiography. J. Am. Coll. Cardiol. 2005, 45, 1235–1242. [Google Scholar] [CrossRef] [Green Version]
- Hayat, S.A.; Senior, R. Safety: The heart of the matter. Eur. J. Echocardiogr. 2005, 6, 235–237. [Google Scholar] [CrossRef]
- Renaud, L. A 5-y follow-up of the radiation exposure to in-room personnel during cardiac catheterization. Health Phys. 1992, 62, 10–15. [Google Scholar] [CrossRef]
- Andreassi, M.G. The biological effects of diagnostic cardiac imaging on chronically exposed physicians: The importance of being non-ionizing. Cardiovasc. Ultrasound 2004, 2, 25. [Google Scholar] [CrossRef] [Green Version]
- Chen, S.; Kroll, M.H.; Shohet, R.V.; Frenkel, P.; Mayer, S.A.; Grayburn, P.A. Bioeffects of myocardial contrast microbubble destruction by echocardiography. Echocardiography 2002, 19, 495–500. [Google Scholar] [CrossRef]
- Hynynen, K.; McDannold, N.; Sheikov, N.A.; Jolesz, F.A.; Vykhodtseva, N. Local and reversible blood-brain barrier disruption by noninvasive focused ultrasound at frequencies suitable for trans-skull sonications. NeuroImage 2005, 24, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Stanton, M.T.; Ettarh, R.; Arango, D.; Tonra, M.; Brennan, P.C. Diagnostic ultrasound induces change within numbers of cryptal mitotic and apoptotic cells in small intestine. Life Sci. 2001, 68, 1471–1475. [Google Scholar] [CrossRef]
- Izadifar, Z.; Babyn, P.; Chapman, D. Mechanical and Biological Effects of Ultrasound: A Review of Present Knowledge. Ultrasound Med. Biol. 2017, 43, 1085–1104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harvey, R.P. The Safe Use of Ultrasound in Medical Diagnosis. Health Phys. 2013, 105, 576. [Google Scholar] [CrossRef]
- Conrad-Hengerer, I.; Al Juburi, M.; Schultz, T.; Hengerer, F.H.; Dick, H.B. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser-assisted cataract surgery: Three-month follow-up. J. Cataract. Refract. Surg. 2013, 39, 1307–1313. [Google Scholar] [CrossRef]
- Rivero, D.R.; Perera, Y.M.; Pérez Candelaria, E.D.L.C.; Veitía Rovirosa, Z.A.; Méndez Duque de Estrada, A.M.; Vidal Castillo, M. New technologies in phacoemulsification cataract surgery. Rev. Cuba. De Oftalmol. 2013, 26, 157–169. [Google Scholar]
- Jirásková, N.; Rozsíval, P. Phacoemulsification parameters: Series 20000 Legacy Versus Legacy with AdvanTec software and NeoSoniX handpiece. J. Cataract. Refract. Surg. 2004, 30, 144–148. [Google Scholar] [CrossRef]
- Garaj-Vrhovac, V.; Kopjar, N. Cytogenetic monitoring of cardiology unit hospital workers exposed to Doppler ultrasound. J. Appl. Toxicol. 2000, 20, 259–264. [Google Scholar] [CrossRef]
- Smagowska, B.; Pawlaczyk-Łuszczyńska, M. Effects of ultrasonic noise on the human body—A bibliographic review. Int. J. Occup. Saf. Ergon. 2013, 19, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Lawton, B.W. Damage to Human Hearing by Airborne Sound of very High Frequency or Ultrasonic Frequency; Health & Safety Executive: Merseyside, UK, 2001. [Google Scholar]
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Tambs, K. Occupational noise exposure and hearing: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [Green Version]
- Ullisch-Nelken, C.; Kusserow, H.; Wolff, A. Analysis of the noise exposure and the distribution of machine types at ultrasound related industrial workplaces in Germany. In Acta Acustica united with Acustica; Hirzel Verlag, S., Ed.; GmbH: Stuttgart, Germany, 2018; Volume 104, pp. 733–736. [Google Scholar] [CrossRef]
- Kilpatrick, H.C. Decibel ratings of dental office sounds. J. Prosthet. Dent. 1981, 45, 175–178. [Google Scholar] [CrossRef]
- Ultraschall–Arbeitsplatz–Messung, Bewertung, Beurteilung und Minderung. Ultrasound–Workplace–Measurement, Assessment, Judgement and Reduction; Technical Rule: Guideline; Association of German Engineers (VDI): Düsseldorf, Germany, 2012. [Google Scholar]
- Rozporządzenie Ministra Pracy i Polityki Socjalnej w Sprawie Najwyższych Dopuszczalnych Stężeń i Natężeń Czynników Szkodliwych dla Zdrowia w Środowisku pracy. Act on the Highest Permissible Concentrations and Intensities of Health Damaging Factors in Working Environment. Dz. U. 2002. item 1833. Available online: http://www.ilo.org/dyn/natlex/natlex4.detail?p_lang=en&p_isn=99664 (accessed on 13 April 2021).
- Health Canada. Guidelines for the Safe Use of Ultrasound: Part II—Industrial and Commercial Applications. Safety Code 24; Ministry of Supply and Services Canada: Ottawa, ON, Canada, 1991; Available online: http://www.hc-sc.gc.ca/ewhsemt/alt_formats/hecs-sesc/pdf/pubs/radiation/safety-code_24-securite/safety-code_24-securite-eng.pdf (accessed on 28 March 2013).
- Schust, M. Biologische Wirkung von Luftgeleitetem Ultraschall. Biological Effects of Airborne Ultrasound (Technical Report); Federal Institute for Occupational Safety and Health: Bremerhaven, Germany, 1996. [Google Scholar]
- Il’nitskaia, A.V.; Pal’tsev, I.P. Combined action of ultrasonics and noise of standard parameters. Gig. Sanit. 1973, 38, 50–53. (In Russian) [Google Scholar]
- Pleban, D.; Smagowska, B.; Radosz, J. Occupational risk assessment related to ultrasonic noise. In INTER-NOISE 2018—47th International Congress and Exposition on Noise Control Engineering: Impact of Noise Control Engineering; Institute of Noise Control Engineering: Reston, VA, USA, 2018. [Google Scholar]
- Grzesik, J.; Pluta, E. High-frequency hearing risk of operators of industrial ultrasonic devices. Int. Arch. Occup. Environ. Health 1983, 53, 77–88. [Google Scholar] [CrossRef] [PubMed]
- Smagowska, B. The assessment of nuisance of ultrasonic noise in the working environment. In Proceedings of the 22nd International Congress on Sound and Vibration, International Institute of Acoustics and Vibrations, Florence, Italy, 12–16 July 2015. [Google Scholar]
- Leighton, T.G. Are some people suffering as a result of increasing massexposure of the public to ultrasound in air? Proc. R. Soc. A 2016, 472, 20150624. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N.; Fileni, A. Occupational risk caused by ultrasound in medicine. Radiol. Med. 1994, 88, 107–111. [Google Scholar] [PubMed]
- Maccà, I.; Scapellato, M.L.; Carrieri, M.; Maso, S.; Trevisan, A.; Bartolucci, G.B. High-frequency hearing thresholds: Effects of age, occupational ultrasound and noise exposure. Int. Arch. Occup. Environ. Health 2014, 88, 197–211. [Google Scholar] [CrossRef]
- Wolff, A. Airborne ultrasound at german workplaces. In Proceedings of the INTER-NOISE 2016—45th International Congress and Exposition on Noise Control Engineering: Towards a Quieter Future, German Acoustical Society (DEGA), Hamburg, Germany, 21–24 August 2016; pp. 2863–2867. [Google Scholar]
- Pleban, D. Admissible Values and Methods of Measurement of Noise, Ultrasonic Noise and Infrasonic Noise at Workplaces in Poland, Proceedings ICA 2019, Admissible Values and Methods of Measurement of Noise, Ultrasonic Noise and Infrasonic Noise at Workplaces in Poland (dega-akustik.de). Available online: https://pub.dega-akustik.de/ICA2019/data/articles/000695.pdf (accessed on 10 March 2021).
- Pawlaczyk-Łuszczyńska, M.; Koton, J.; Śliwińska-Kowalska, M.; Augustyńska, D.; Komeduła, M. Hałas ultradźwiękowy. Dokumentacja proponowanych wartości dopuszczalnych poziomów narażenia zawodowego. Ultrasonic noise. Documentation of propositions of new limit values for occupational exposure. Podstawy I Metod. Oceny Sr. Pracy. 2001, 2, 55–88. (In Polish) [Google Scholar]
- Ullisch-Nelken, C.; Schöneweiß, R.; Wolff, A. Ears II-Development of an ultrasound measurement technique for use in occupational safety. In Proceedings of the 12th ICBEN Congress on Noise as a Public Health Problem, Zurich, Switzerland, 18–22 June 2017. [Google Scholar]
- EI EN 61689. 2013 Ultrasonics—Physiotherapy ystems—Field specifications and methods of measurement in the frequency range 0.5 MHz to 5 MHz. IEC: Geneva, Switzerland, 2013.
- Nyborg, W.L.; Carson, P.L.; Dunn, F.; Miller, D.L.; Miller, M.W.; Ziskin, M.C.; Cain, C.A. Biological Effects of Ultrasound: Mechanisms and Clinical Implications; National Council on Radiation Protection and Measurements of United States (NCRP): Bethesda, MD, USA, 1983; ISBN 0-913392-64-2. [Google Scholar]
- Guidelines for the safe use of diagnostic ultrasound equipment. Ultrasound 2010, 18, 52–59. [CrossRef]
- Guidelines for the Safe Use of Ultrasound: Part I—Medical and Paramedical Applications (Excerpt from Safety Code 23, 1989). Available online: https://www.canada.ca/en/health-canada/services/environmental-workplace-health/reports-publications/radiation/guidelines-safe-use-ultrasound-part-medical-paramedical-applications-excerpt-safety-code-23-1989-health-canada.html (accessed on 20 April 2020).
- Marketing Clearance of Diagnostic Ultrasound Systems and Transducers Guidance for Industry and Food and Drug Administration Staff Document Issued on: 27 June 2019. Available online: https://www.fda.gov/media/71100/download (accessed on 13 April 2021).
- International Electrotechnical Commission. 60601-2-37: 2007+ AMD1: 2015 CSV Medical Electrical Equipment—Part 2-37: Particular Requirements for the Basic Safety and Essential Performance of Ultrasonic Medical Diagnostic and Monitoring Equipment; International Electrotechnical Commission: Geneva, Switzerland, 2015. [Google Scholar]
- Hekkenberg, R.T.; Oosterbaan, W.A.; Teirlinck, C.J.P.M. Handling IEC1157: Complicated output measurements—A challenge. Ultrasonics 1996, 34, 139–145. [Google Scholar] [CrossRef]
- IEC 61161; Ultrasonics-Power Measurement-Radiation Force Balances and Performance Requirements. International Electrotechnical Commission: Geneva, Switzerland, 2006.
- IEC 62127-1; Ultrasonics–Hydrophones–Part 1: Measurement and Characterization of Medical Ultrasonic Fields up to 40 MHz. International Electrotechnical Commission: Geneva, Switzerland, 2007.
- IEC 62359; Ultrasonics-Field Characterization-Test Methods for the Determination of Thermal and Mechanical Indices Related to Medical Diagnostic Ultrasonic Fields. International Electrotechnical Commission: Geneva, Switzerland, 2010.
- Kusserow, H. Kritische Betrachtung der Deutschen Beurteilungskriterien für Berufliche Ultraschalleinwirkungen auf Das Gehör im Rahmen Eines Internationalen Vergleichs und am Beispiel von Ultraschall-Schweißmaschinen. Deutsche Gesetzliche Unfallversicherung e. V.; Institut für Arbeitsschutz: Berlin, Germany, 2016. [Google Scholar]
- Maue, J. Geräuschanalysen von Ultraschall-Schweißmaschinen; Deutsche Gesetzliche Unfallversicherung (DGUV): Berlin, Germany, 2014. [Google Scholar]
- Smagowska, B. Ultrasonic noise sources in a work environment. Arch. Acoust. 2013, 38, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Moyano, D.B.; González Lezcano, R.A. Effects of infrasound on health: Looking for improvements in housing conditions. Int. J. Occup. Saf. Ergon. 2020, 1–34. [Google Scholar] [CrossRef] [PubMed]
- Pawlaczyk-Luszczynska, M.; Dudarewicz, A.; Sliwinska-Kowalska, M. Zródla ekspozycji zawodowej na halas ultradzwiekowy-ocena wybranych urzadzen (sources of occupationalexposure to ultrasonic noise). Med. Pract. 2007, 58, 105–116. [Google Scholar]
- Kaufman, G.E.; Miller, M.W.; Dan Griffiths, T.; Ciaravino, V.; Carstensen, E.L. Lysis and viability of cultured mammalian cells exposed to 1 MHz ultrasound. Ultrasound Med. Biol. 1977, 3, 21–25. [Google Scholar] [CrossRef]
- Hallow, D.M.; Mahajan, A.D.; McCutchen, T.E.; Prausnitz, M.R. Measurement and correlation of acoustic cavitation with cellular bioeffects. Ultrasound Med. Biol. 2006, 32, 1111–1122. [Google Scholar] [CrossRef]
- Lai, C.Y.; Wu, C.H.; Chen, C.C.; Li, P.C. Quantitative relations of acoustic inertial cavitation with sonoporation and cell viability. Ultrasound Med. Biol. 2006, 32, 1931–1941. [Google Scholar] [CrossRef]
- Ryaby, J.P. Low-intensity pulsed ultrasound modulates adenylate cyclase activity and transforming growth factor beta synthesis. Electromagn. Biol. Med. 1991, 95–100. [Google Scholar]
- Rawool, N.M.; Goldberg, B.B.; Forsberg, F.; Winder, A.A.; Hume, E. Power doppler assessment of vascular changes during fracture treatment with low-intensity ultrasound. J. Ultrasound Med. 2003, 22, 145–153. [Google Scholar] [CrossRef]
- WHO. Environmental Heath Criteria 22. Ultrasound; WHO: Geneva, Switzerland, 1982. [Google Scholar]


| Application | Frequency (kHz) | Intensity Range (W/cm2) |
|---|---|---|
| Low-frequency underwater signals | 16–20 | — |
| Aerosol reactions and agitation | 16–20 | — |
| Ultrasonic control devices, door opening | 25 | — |
| Welding | 16–20 | 3–32 |
| Industrial cleaning and degreasing | 20–25 | <6 |
| Plastic welding | 20 | 1000 |
| Metal welding | 10–60 | 10,000 |
| Mechanization | 20 | variable |
| Extraction | 10 | 500 |
| Automation | 20–300 | variable |
| Thickness measurement | 300 | — |
| Experimental biological work | 760 | — |
| Effects | Mechanism |
|---|---|
| Vasodilation | Release of tissue stimulants. Reduction in muscle tone. |
| Muscle relaxation | Elimination of tissue stimulants. Post-excitatory depression orthosympathetic. |
| Increased membrane permeability | Forcing the tissue fluid through. pH less acidic. |
| Increased tissue regeneration | Mechanical effect. |
| Thermal effect | Can block conduction. Nervous tissue possesses special sensitivity to ultrasound. |
| Decrease in pain | Normalization of muscle tone. Decrease in pH. |
| Material | Speed (m/s) |
|---|---|
| Air | 331 |
| Fat | 1450/1465 |
| Water (50 °C) | 1540 |
| Human soft tissue | 1540 |
| Liver | 1549 |
| Kidney | 1561 |
| Blood | 1570/1584 |
| Muscle | 1585 |
| Non-fatty tissue | 1575 |
| Cortical bone | 3635 |
| Amniotic fluid | 1535 |
| Group | Characteristics |
|---|---|
| Sectorial | Provide a triangular or fan-shaped image format with a small echo emission start base. Used for cardiac and abdominal explorations since they facilitate a costal approach, and to view deep structures. Usual working frequency between 3.5 and 5 MHz. |
| Convex | Waves have a curved shape and provide a trapezoid-shaped image format. Used in abdominal and obstetrical to view deep structures. Usual working frequency between 3.5 and 5 MHz. |
| Linear | Provide a rectangular image format. Used for the study of more superficial structures, such as muscles, tendons, breasts, thyroid, vessels, etc. Usual working frequency between 7.5 and 13 MHz, although some go up to 20 MHz. |
| Intra-cavity | Linear or convex. Used for intrarectal or intravaginal examinations. Usual working frequency between 5 and 7.5 MHz |
| Ultrasound Use | Frequencies |
|---|---|
| Clean jewelry, lenses, watches, instruments | 20–40 kHz |
| Clean teeth (break down bacterial plaque) | 1.6 MHz |
| Lithotripsy | 100–200 kHz |
| Phacoemulsification cataract (torsional Ozil) | 32 kHz |
| Phacoemulsification cataract (NeoSoniX system) | 120 Hz |
| 1/3-Octave Band Frequency, f (kHz) | Lf, eq, 8 h, adm Lf, eq, wk, adm (dB) | Lf, max, adm (dB) |
|---|---|---|
| 10, 12.5, 16 | 80 | 100 |
| 20 | 90 | 110 |
| 25 | 105 | 125 |
| 31.5, 40 | 110 | 130 |
| Temperature Increase | Maximum Time Exposure |
|---|---|
| 39 °C (2 degrees above normal) | 60 min |
| 40 °C (3 degrees above normal) | 15 min |
| 41 °C (4 degrees above normal) | 4 min |
| 42 °C (5 degrees above normal) | 1 min |
| 43 °C (6 degrees above normal) | 0.25 min |
| Use | ISPTA.3 (mW/cm2) | ISPTA.3 (W/cm2) | MI |
|---|---|---|---|
| Peripheral Vessel | 720 | 190 | 1.9 |
| Cardiac | 430 | 190 | 1.9 |
| Fetal Imaging and Other | 94 | 190 | 1.9 |
| Ophthalmic | 17 | 28 | 0.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moyano, D.B.; Paraiso, D.A.; González-Lezcano, R.A. Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review. Healthcare 2022, 10, 423. https://doi.org/10.3390/healthcare10030423
Moyano DB, Paraiso DA, González-Lezcano RA. Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review. Healthcare. 2022; 10(3):423. https://doi.org/10.3390/healthcare10030423
Chicago/Turabian StyleMoyano, David Baeza, Daniel Arranz Paraiso, and Roberto Alonso González-Lezcano. 2022. "Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review" Healthcare 10, no. 3: 423. https://doi.org/10.3390/healthcare10030423
APA StyleMoyano, D. B., Paraiso, D. A., & González-Lezcano, R. A. (2022). Possible Effects on Health of Ultrasound Exposure, Risk Factors in the Work Environment and Occupational Safety Review. Healthcare, 10(3), 423. https://doi.org/10.3390/healthcare10030423







