How to Survive 33 min after the Umbilical of a Saturation Diver Severed at a Depth of 90 msw?
Abstract
:1. Background
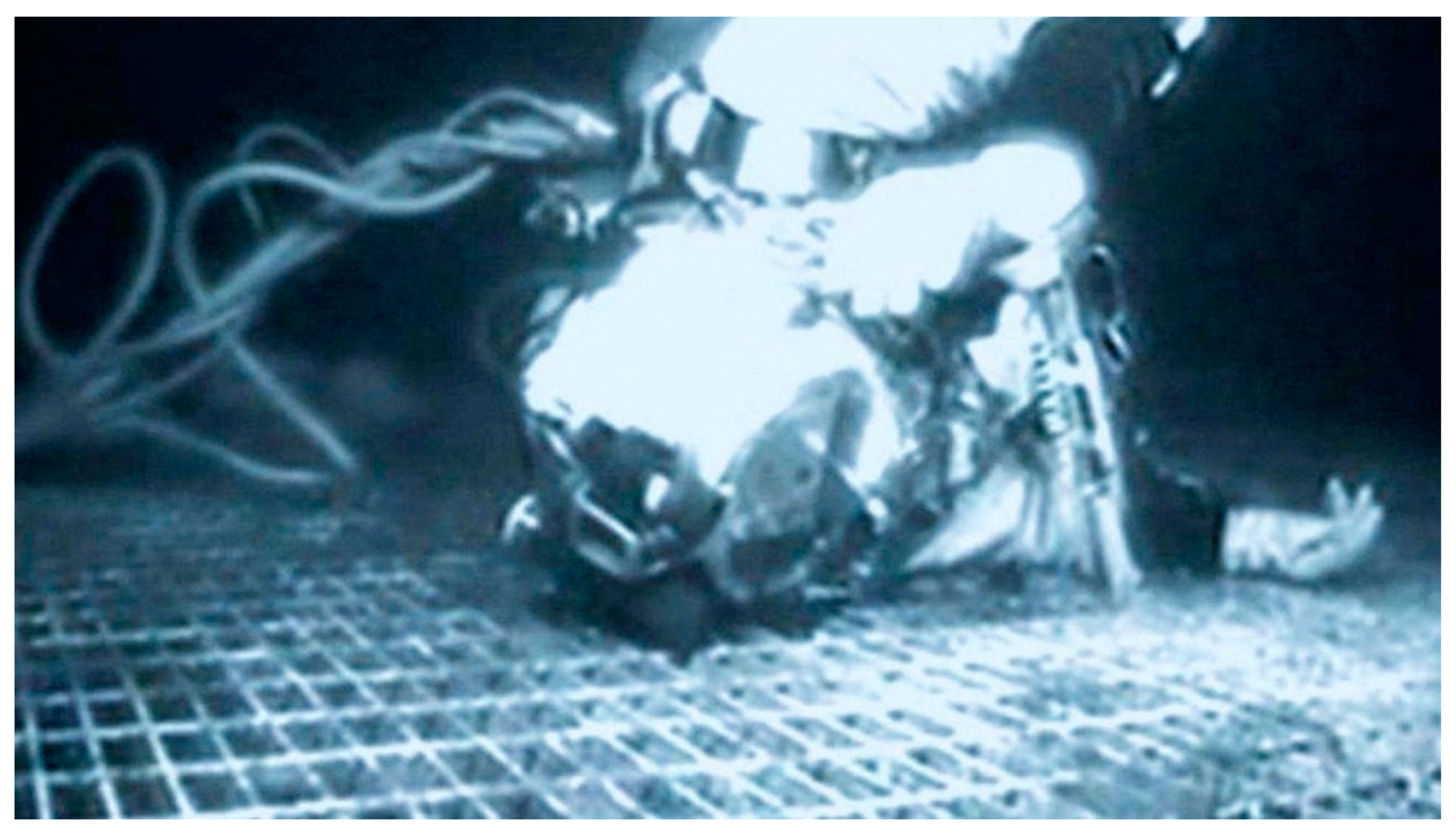
1.1. The Case
1.2. The Miracle
1.3. The Diver
1.4. Two Inconsistencies
1.5. Assessments
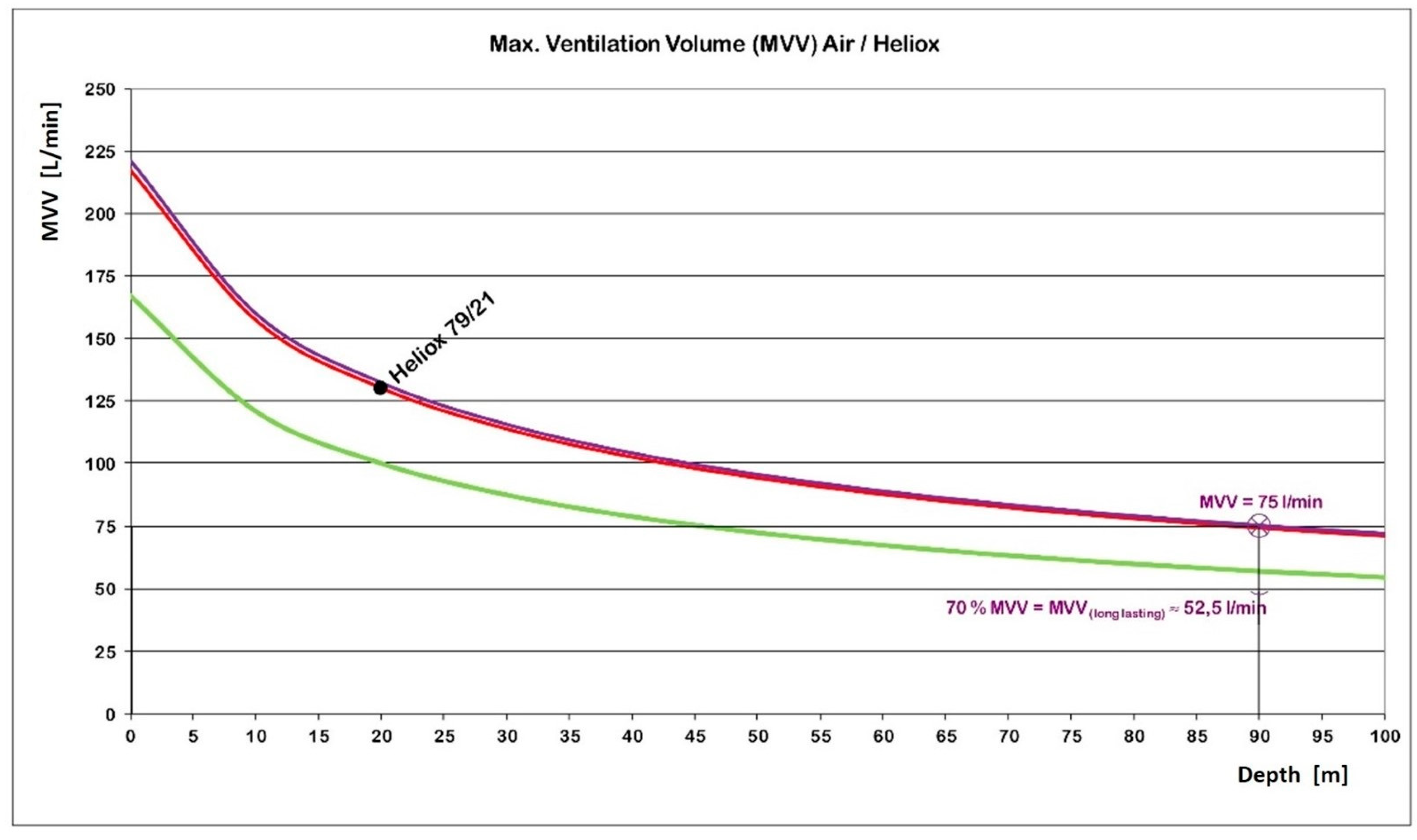
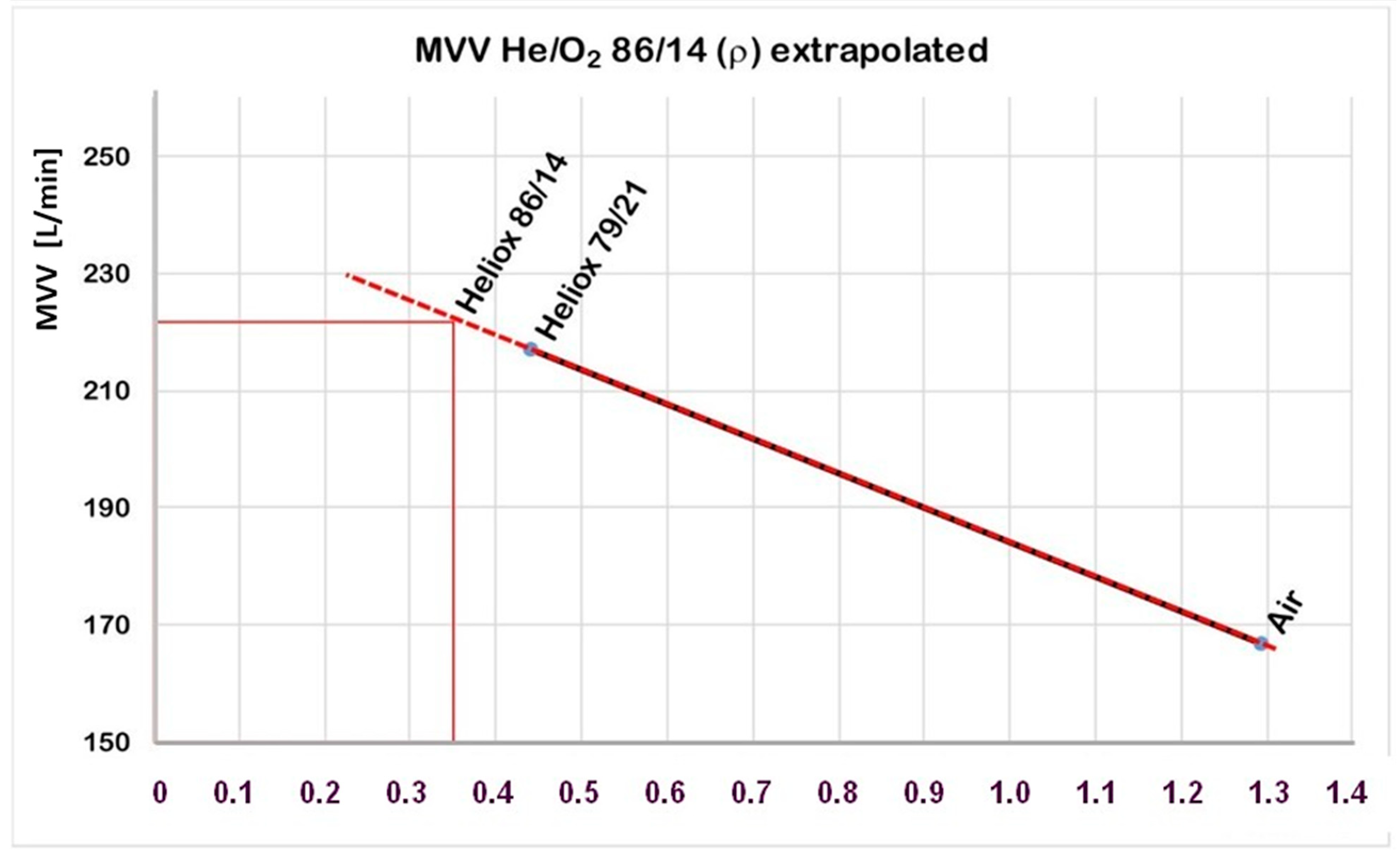
1.6. Heliox Consumption
1.7. Oxygen Reserve
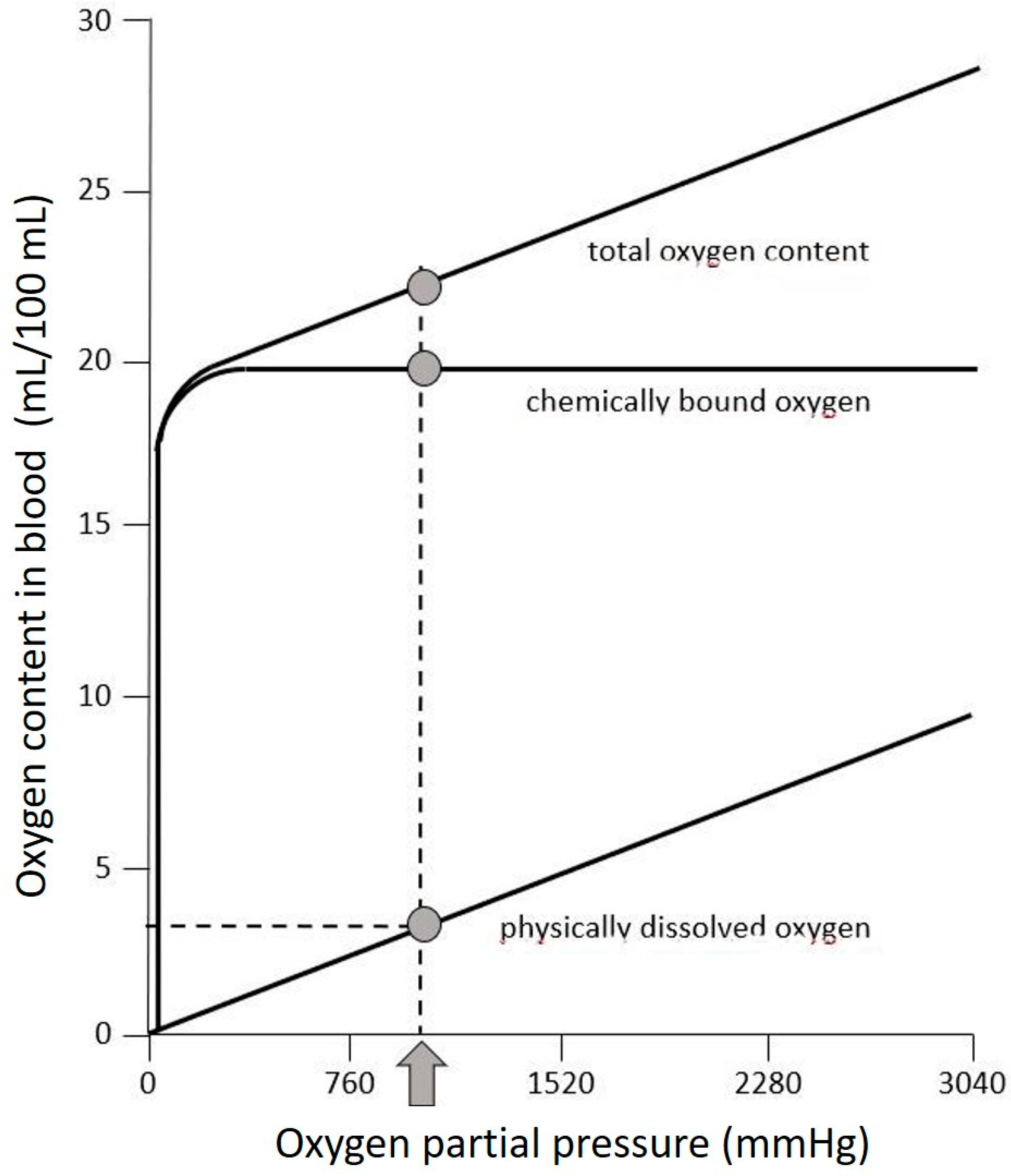
- On the surface, air contains 21% oxygen generating an O2-partial pressure of 0.21 bar (≈160 mmHg); assuming a hemoglobin concentration of 15 g/100 mL blood, this results in 20.1 mL O2/100 mL chemically bound to hemoglobin in the blood [23]. For Dc, who weighed about 95 kg, we calculated a blood volume of approximately 6.7 L, which then carries ca. 1.4 L of O2 bound to hemoglobin. We still have to add 0.3 L of physically dissolved oxygen, resulting in a total of 1.7 L O2 in blood.
- Oxygen is also dissolved in the body’s water spaces. In the case of Chris, the water space amounts to 57 L (=60% of 95 kg). At a body temperature of 37 °C, 0.024 mL O2/m L /bar can be dissolved in water [24] resulting in 1.9 L O2 at a pO2 of 1.4 bar. To err on the safe side, we have not considered any increase in dissolved O2 that would be due to the decreased body temperature.
- Further assuming a consumption of 0.5 L O2 × min−1, 3.6 L O2 would be roughly a 7-min reserve. This also means that the idea that enough oxygen was stored in Dc’s body to cover 28 min after the end of the heliox emergency supply must be dismissed.
- We estimate a functional residual capacity (FRC) according to Equation (3) [25],
- 5.
- The diving helmet and the neck area (Kirby Morgan 37) also contain heliox. With an assumed spherical shape and a diameter of approx. 23 cm, this results in a helmet volume of approx. 8.5 L. Subtracting a volume of 4 l for the head results in a heliox-filled volume of 4.5 L and an O2 quantity of 6.2 L O2 (=4.5 L × 0.14 × 10). Below the helmet (between the diving suit and neck), there is an almost cylindrical space. This heliox-filled area has a volume of about 1 land thus contains 1.4 L O2. (=1 L × 0.14 × 10). The head and neck region thus contained a total of 7.6 L O2. The heliox-filled area inside the rest of the suit was not likely to be available for breathing.
- 6.
- Myoglobin as an intramuscular O2 storage can bind 1.29 mL O2/g. With 6 g of myoglobin and an assumed muscular mass of 36 kg [26], Dc has a further reserve of 0.3 L O2. We understand that the cardiac and the skeletal muscle can also consume this relatively small O2 portion.
1.8. Hypothermia
1.9. Carbon Dioxide
1.10. Helium and Neuroprotection
2. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
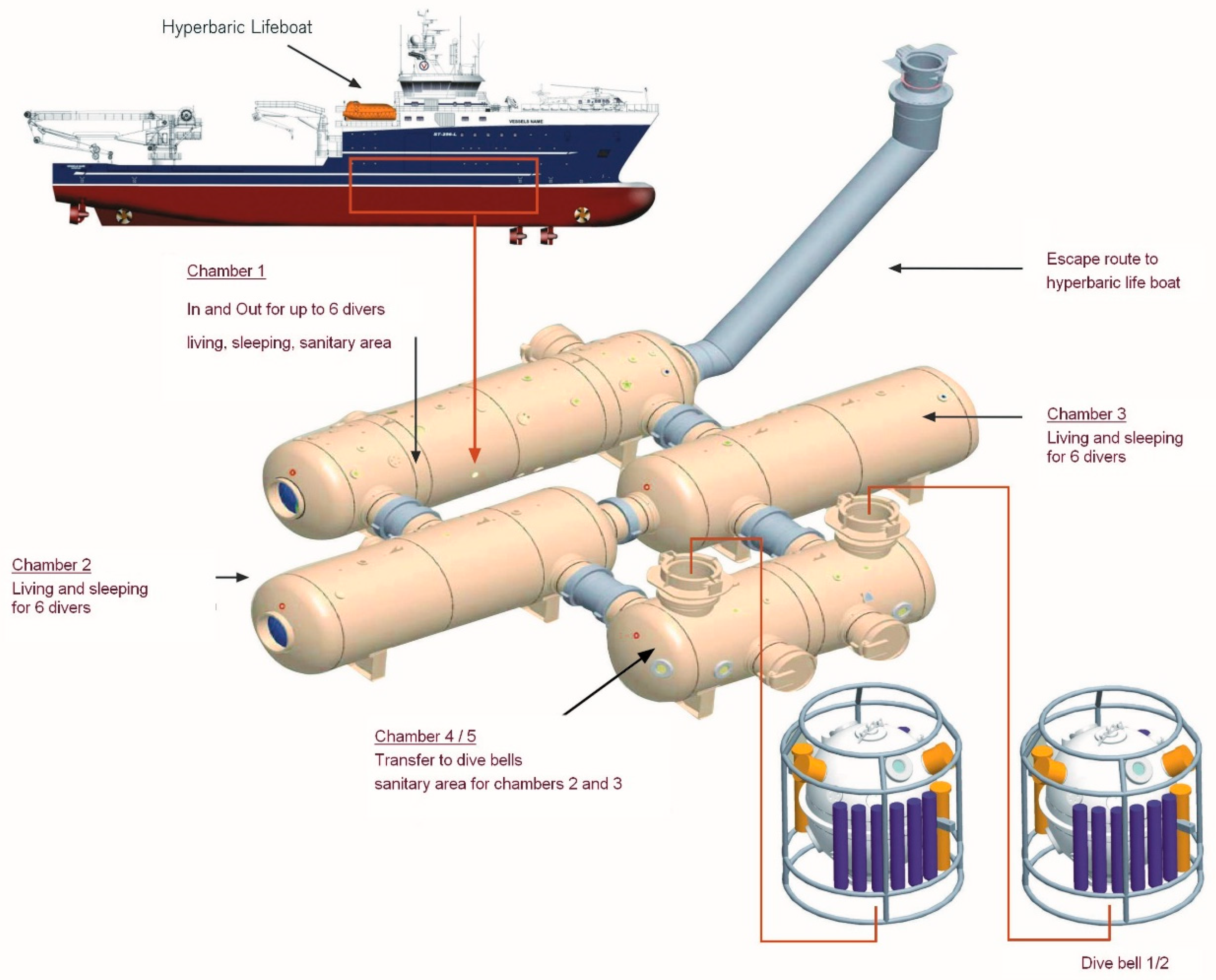
- Dillig, B. Dräger Safety Liefert Tieftauchanlage für Norwegisches Taucherbasisschiff “Bibby Topaz”. Presse Box, 23 November 2006. Available online: https://www.pressebox.de/pressemitteilung/draegerwerk-ag-co-kgaa-luebeck/Draeger-Safety-liefert-Tieftauchanlage-fuer-norwegisches-Taucherbasisschiff-Bibby-Topaz/boxid/84357(accessed on 3 February 2021).
- Subsea. Bibby Reconstructs North Sea Diving Incident. Offshore Energy, 24 September 2015. Available online: https://www.offshore-energy.biz/bibby-reconstructs-north-sea-diving-incident/(accessed on 15 February 2021).
- Oxygen Content in Open Circuit Bail-Out Bottles for Heliox Saturation Diving. The Diving Medical Advisory Committee, 2 May 2016. Available online: https://www.dmac-diving.org/guidance/DMAC04.pdf(accessed on 29 January 2022).
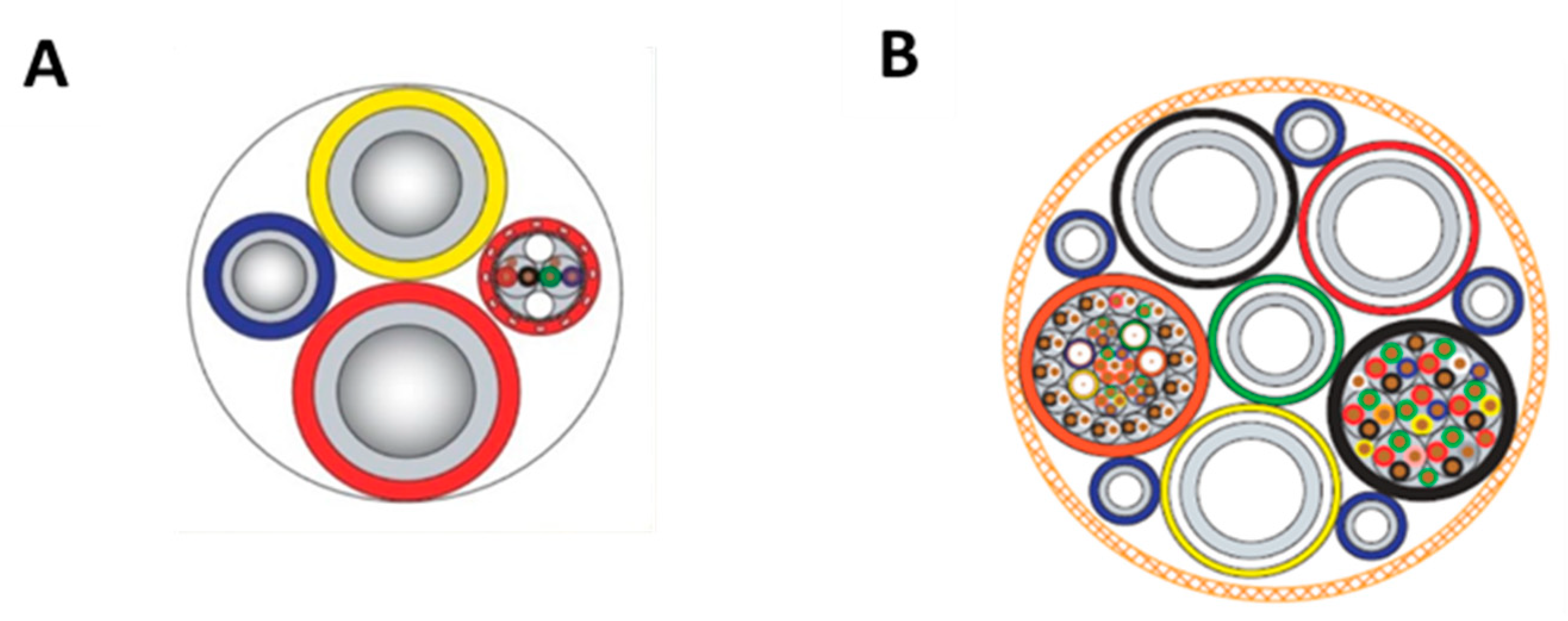
- Miller, K. Bay-Tech Industries. 2020. Available online: https://baytechrentals.com/product/divers-umbilical/ (accessed on 1 June 2021).
- Villazon Granda, A. Incident Summary 08.10.12 “Bibby Topaz.” 2012. Available online: https://de.slideshare.net/arturovillazongranda/incident-summary-081012-bibby-topaz (accessed on 15 February 2021).
- FloatingHarbour, Co., UK. Chris Lemons on Oil Rig. 2014. Available online: https://floatingharbour.co.uk/admin/resources/films/screenshot-2014-11-06-14.12.17-w1920.png (accessed on 15 February 2021).
- Perring, R. Miracle of Diver Who Cheated Death When Stranded 300ft under with NO OXYGEN for 30 Minutes. Express, 10 March 2019. Available online: https://www.express.co.uk/news/uk/1125439/life-after-death-under-water-no-oxygen-last-breath-chris-lemons-diver-video(accessed on 3 March 2021).
- Davidson, B. He was 330 Feet Deep without Anything to Breathe—and Survived. undercurrent.org. 2019. Available online: https://www.undercurrent.org/UCnow/dive_magazine/2019/330FeetDeep201906.html (accessed on 19 February 2021).
- Safar, P.; Kochanek, P. Cerebral blood flow promotion after prolonged cardiac arrest. Crit. Care Med. 2000, 28, 3104–3106. [Google Scholar] [CrossRef]
- Ergonomie der Thermischen Umgebung—Bestimmung des Körpereigenen Energieumsatzes. DIN EN ISO 8996:2005-01. 2005. Available online: https://www.beuth.de/de/norm/din-en-iso-8996/73397417 (accessed on 8 January 2021).
- Boerema, I.; Meyene, N.G.; Brummelkamp, W.H.; Bouma, S.; Mensch, M.H.; Kaermans, F.; Hanf, F.S.; van Aalderen, W. Leven Zonder Bloed. Ned. Tijdschr. Geneeska. 1960, 104, 949–954. [Google Scholar]
- Frisancho, A.R. Human Adaptation and Accommodation; University of Michigan Press: Ann Arbo, MI, USA, 1993. [Google Scholar]
- Malley, W.J. Clinical Blood Gases: Assessment and Intervention, 2nd ed.; Elsevier Saunders: St. Louis, MO, USA, 2005. [Google Scholar]
- van Hoesen, K. Hyperbaric Medicine; Chapter 78. Anesthesia Key. 1989. Available online: https://aneskey.com/hyperbaric-medicine/ (accessed on 31 January 2022).
- Baldwin, E.D.; Cournand, A.; Richards, D.W.J. Pulmonary insufficiency; physiological classification, clinical methods of analysis, standard values in normal subjects. Medicine (Baltimore) 1948, 27, 243–278. [Google Scholar] [CrossRef]
- Maio, D.A.; Farhi, L.E. Effect of Gas Density on Mechanics of Breathing. SAM-TR-70-5; USAF School of Aerospace Medicine: Dayton, OH, USA, 1970; pp. 15–21. [Google Scholar]
- Wood, W.B. Ventilatory Dynamics under Hyperbaric States; National Academy of Sciences: Washington, DC, USA, 1963; Volume 1181, pp. 108–121. [Google Scholar]
- ISO 8996:2004. ISO. 2004. Available online: https://www.iso.org/standard/34251.html (accessed on 6 April 2021).
- Linnarsson, D.; Ostlund, A.; Lind, F.; Hesser, C.M. Hyperbaric Bradycardia and Hypoventilation in Exercising Men: Effects of Ambient Pressure and Breathing Gas. J. Appl. Physiol. 1999, 87, 1428–1432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bühlmann, A.A. Physiology and pathophysiology of diving. Schweiz. Z. Sportmed. 1981, 29, 5–11. [Google Scholar]
- Beckman, T.J.; Lall, R.; Johnson, W.B. Salient personality characteristics among Navy divers. Mil. Med. 1996, 161, 717–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jackson, D. Diver Cheated Death in North Sea Miracle. BBC News, 5 April 2019. Available online: https://www.bbc.com/news/uk-scotland-north-east-orkney-shetland-47826802(accessed on 10 February 2021).
- Pittman, R.N. Oxygen Transport. In Regulation of Tissue Oxygenation; Chapter 4; Morgan & Claypool Life Sciences: San Rafael, CA, USA, 2011. [Google Scholar]
- Schmidt, R.F.; Thews, G.; Altner, H. (Eds.) Physiologie des Menschen; Springer: Berlin/Heidelberg, Germany, 1990. [Google Scholar]
- Schmidt, R.F.; Lang, F.; Heckmann, M. (Eds.) Physiologie des Menschen: Mit Pathophysiologie: Mit Online-Repetitorium; Sonderausgabe der 31; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- Heinen, E.; Heinen, E. Der Muskel-Masse-Index MMI. 2019. Available online: https://profheinen.de/koerperzusammensetzung/muskel-masse-index-mmi/ (accessed on 2 February 2021).
- Mekjavic, I.B.; Golden, F.S.C.; Eglin, M.; Tipton, M.J. Thermal Status of Saturation Divers during Operational Dives in the North Sea. Undersea Hyperb. Med. 2001, 28, 149–155. [Google Scholar]
- Barsky, S.M.; Tom, S.N. Investigating Recreational and Commercial Diving Accidents; Hammerhead Press: Ventura, CA, USA, 2003. [Google Scholar]
- Örnhagen, H. Thermal Problems in Diving. 2004. Available online: https://www.ornhagen.se/Thermal%20problems%20in%20diving%20050106%20Hemsida.pdf (accessed on 24 March 2021).
- Piantadosi, C.A.; Thalmann, E.D. Thermal Responses in Humans Exposed to Cold Hyperbaric Helium-Oxygen. J. Appl. Physiol. 1980, 49, 1099–1106. [Google Scholar] [CrossRef]
- Neves, J.; Thomas, C. Fighting Exposure—Is Helium a ‘Cold’ Gas? SDI/TDI/ERDI/PFI, 1 October 2021. Available online: https://www.tdisdi.com/portugal-blog/is-helium-a-cold-gas/(accessed on 27 April 2021).
- Tipton, M.J. The Initial Responses to Cold-Water Immersion in Man. Clin. Sci. 1989, 77, 581–588. [Google Scholar] [CrossRef] [Green Version]
- Geigel, R. Wetter und Klima: Ihr Einfluss auf den Gesunden und auf den Kranken Menschen; J.F. Bergmann: München, Germany, 1924. [Google Scholar]
- Musi, M.E.; Sheets, A.; Zafren, K.; Brugger, H.; Paal, P.; Hölzl, N.; Pasquier, M. Clinical Staging of Accidental Hypothermia: The Revised Swiss System. Resuscitation 2021, 162, 182–187. [Google Scholar] [CrossRef]
- Pasquier, M.; Zurron, N.; Weith, B.; Turini, P.; Dami, F.; Carron, P.N.; Paal, P. Deep Accidental Hypothermia with Core Temperature Below 24 °C Presenting with Vital Signs. High Alt. Med. Biol. 2014, 15, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.J.A.; Brugger, H.; Boyd, J.; Paal, P. Accidental Hypothermia. N. Engl. J. Med. 2012, 367, 1930–1938. [Google Scholar] [CrossRef] [PubMed]
- Tibes, U.; Stegemann, J. Das Verhalten der endexspiratorischen Atemgasdrucke, der O2-Aufnahme und CO2-Abgabe nach einfacher Apnoe im Wasser, an Land und apnoeischem Tauchen. Pflügers Arch. Eur. J. Physiol. 1969, 311, 300–311. [Google Scholar] [CrossRef]
- Muth, C.M.; Radermacher, P.; Pittner, A.; Steinacker, J.; Schabana, R.; Hamich, S.; Paulat, K.; Calzia, E. Arterial Blood Gases during Diving in Elite Apnea Divers. Int. J. Sports Med. 2003, 24, 104–107. [Google Scholar] [CrossRef]
- Weaver, L.K.; Howe, S.; Snow, G.L.; Deru, K. Arterial and pulmonary arterial hemodynamics and oxygen delivery/extraction in normal humans exposed to hyperbaric air and oxygen. J. Appl. Physiol. 2009, 107, 336–345. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosco, G.; Rizzato, A.; Martani, L.; Schiavo, S.; Talamonti, E.; Garetto, G.; Paganini, M.; Camporesi, E.M.; Moon, R.E. Arterial Blood Gas Analysis in Breath-Hold Divers at Depth. Front. Physiol. 2018, 9, 1558. [Google Scholar] [CrossRef]
- Pendergast, D.R.; Lindholm, P.; Wylegala, J.; Warkander, D.; Lundgren, C.E.G. Effects of Respiratory Muscle Training on Respiratory CO2 Sensitivity in SCUBA Divers. Undersea Hyperb. Med. 2006, 33, 447–453. [Google Scholar]
- Earing, C.M.N.; McKeon, D.J.; Kubis, H.P. Divers Revisited: The Ventilatory Response to Carbon Dioxide in Experienced Scuba Divers. Respir. Med. 2014, 108, 758–765. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.-Z.; Li, T.-T.; Cao, H.-L.; Yang, W.-C. Recent advances in the neuroprotective effects of medical gases. Med. Gas Res. 2019, 9, 80–87. [Google Scholar] [CrossRef]
- Höllig, A.; Coburn, M. Noble gases and neuroprotection: Summary of current evidence. Curr. Opin. Anaesthesiol. 2021, 34, 603–606. [Google Scholar] [CrossRef]
- Winkler, D.A.; Thornton, A.; Farjot, G.; Katz, I. The diverse biological properties of the chemically inert noble gases. Clin. Pharmacol. Ther. 2016, 160, 44–64. [Google Scholar] [CrossRef] [PubMed]
- Weber, N.C.; Preckel, B. Gaseous mediators: An updated review on the effects of helium beyond blowing up balloons. ICMx 2019, 7, 73. [Google Scholar] [CrossRef] [PubMed]
- Coburn, M.; Maze, M.; Franks, N.P. The neuroprotective effects of xenon and helium in an in vitro model of traumatic brain injury. Crit. Care Med. 2008, 36, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Jawad, N.; Rizvi, M.; Gu, J.; Adeyi, O.; Tao, G.; Maze, M.; Ma, D. Neuroprotection (and lack of neuroprotection) afforded by a series of noble gases in an in vitro model of neuronal injury. Neurosci. Lett. 2009, 460, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Aehling, C.; Weber, N.C.; Zuurbier, C.J.; Preckel, B.; Galmbacher, R.; Stefan, K.; Hollmann, M.W.; Popp, E.; Knapp, J. Effects of combined helium pre/post-conditioning on the brain and heart in a rat resuscitation model. Acta. Anaesthesiol. Scand. 2018, 62, 63–74. [Google Scholar] [CrossRef]
- Liu, Y.; Xue, F.; Liu, G.; Shi, X.; Liu, Y.; Liu, W.W.; Luo, X.; Sun, X.; Kang, Z.M. Helium preconditioning attenuates hypoxia/ischemia-induced injury in the developing brain. Brain Res. 2011, 1376, 122–129. [Google Scholar] [CrossRef]
- Pan, Y.; Zhang, H.; Acharya, A.B.; Cruz-Flores, S.; Panneton, W.M. The effect of heliox treatment in a rat model of focal transient cerebral ischemia. Neurosci. Lett. 2011, 497, 144–147. [Google Scholar] [CrossRef]
- Li, Y.; Liu, K.; Kang, Z.M. Helium preconditioning protects against neonatal hypoxia-ischemia via nitric oxide mediated up-regulation of antioxidases in a rat model. Behav. Brain Res. 2016, 300, 31–37. [Google Scholar] [CrossRef]
- Heinen, A.; Huhn, R.; Smeele, K.M.A.; Zuurbier, C.J.; Schlack, W.; Preckel, B.; Hollmann, M.W. Helium-induced Preconditioning in Young and Old Rat Heart. Anesthesiology 2008, 109, 830–836. [Google Scholar] [CrossRef] [Green Version]
- Pagel, P.S.; Krolikowski, J.G.; Pratt, P.F.; Shim, Y.H.; Amour, J.; Warltier, D.C.; Weihrauch, D. The Mechanism of Helium-Induced Preconditioning: A Direct Role for Nitric Oxide in Rabbits. Anesth. Analg. 2008, 107, 762–768. [Google Scholar] [CrossRef] [Green Version]
- Deng, J.; Lei, C.; Chen, Y.; Fang, Z.; Yang, Q.; Zhang, H.; Cai, M.; Shi, L.; Dong, H.; Xiong, L. Neuroprotective gases--fantasy or reality for clinical use? Prog. Neurobiol. 2014, 115, 210–245. [Google Scholar] [CrossRef] [PubMed]
- da Costa, R.; Parkinson, A. Der Letzte Atemzug—Gefangen am Meeresgrund. Arte. 2019. Available online: https://www.youtube.com/watch?v=JvUab7KhojI (accessed on 2 February 2021).
- Baker, S. A Diver Survived more than 30 Minutes at the Bottom of the North Sea after His Oxygen Cord was Severed in an Oil-rig Repair Job Gone Horribly Wrong. Businessinsider, 10 March 2019. Available online: https://www.businessinsider.com/diver-survived-38-minutes-north-sea-bed-oxygen-cord-2019-5(accessed on 10 April 2021).
- Gray, R. Can You Survive If You Run Out of Air? BBC Future, 23 April 2019. Available online: https://www.bbc.com/future/article/20190423-the-man-who-ran-out-of-air-at-the-bottom-of-the-ocean(accessed on 4 March 2021).
- Evans, C. The Last Breath: How diver Chris Lemons Survived without Oxygen for 30 Minutes on the Seabed. Inews/Film, 4 April 2019. Available online: https://inews.co.uk/culture/film/last-breath-film-diver-accident-oxygen-276006(accessed on 3 March 2021).
- Lemons, C. About Chris. 2019. Available online: https://www.chrislemons.co.uk/about-chris (accessed on 4 February 2021).
- Incident Summary 08.10.12 “Bibby Topaz.”. Docomen, 18 September 2014. Available online: https://dokumen.tips/education/incident-summary-081012-bibby-topaz.html(accessed on 2 March 2021).





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dreyer, S.; Deussen, A.; Berndt, D.; Schipke, J.D. How to Survive 33 min after the Umbilical of a Saturation Diver Severed at a Depth of 90 msw? Healthcare 2022, 10, 453. https://doi.org/10.3390/healthcare10030453
Dreyer S, Deussen A, Berndt D, Schipke JD. How to Survive 33 min after the Umbilical of a Saturation Diver Severed at a Depth of 90 msw? Healthcare. 2022; 10(3):453. https://doi.org/10.3390/healthcare10030453
Chicago/Turabian StyleDreyer, Sven, Andreas Deussen, Dietmar Berndt, and Jochen D. Schipke. 2022. "How to Survive 33 min after the Umbilical of a Saturation Diver Severed at a Depth of 90 msw?" Healthcare 10, no. 3: 453. https://doi.org/10.3390/healthcare10030453





