The Effect of Physician Communication on Inpatient Satisfaction
Abstract
:1. Introduction
2. Data and Methodology
2.1. Data
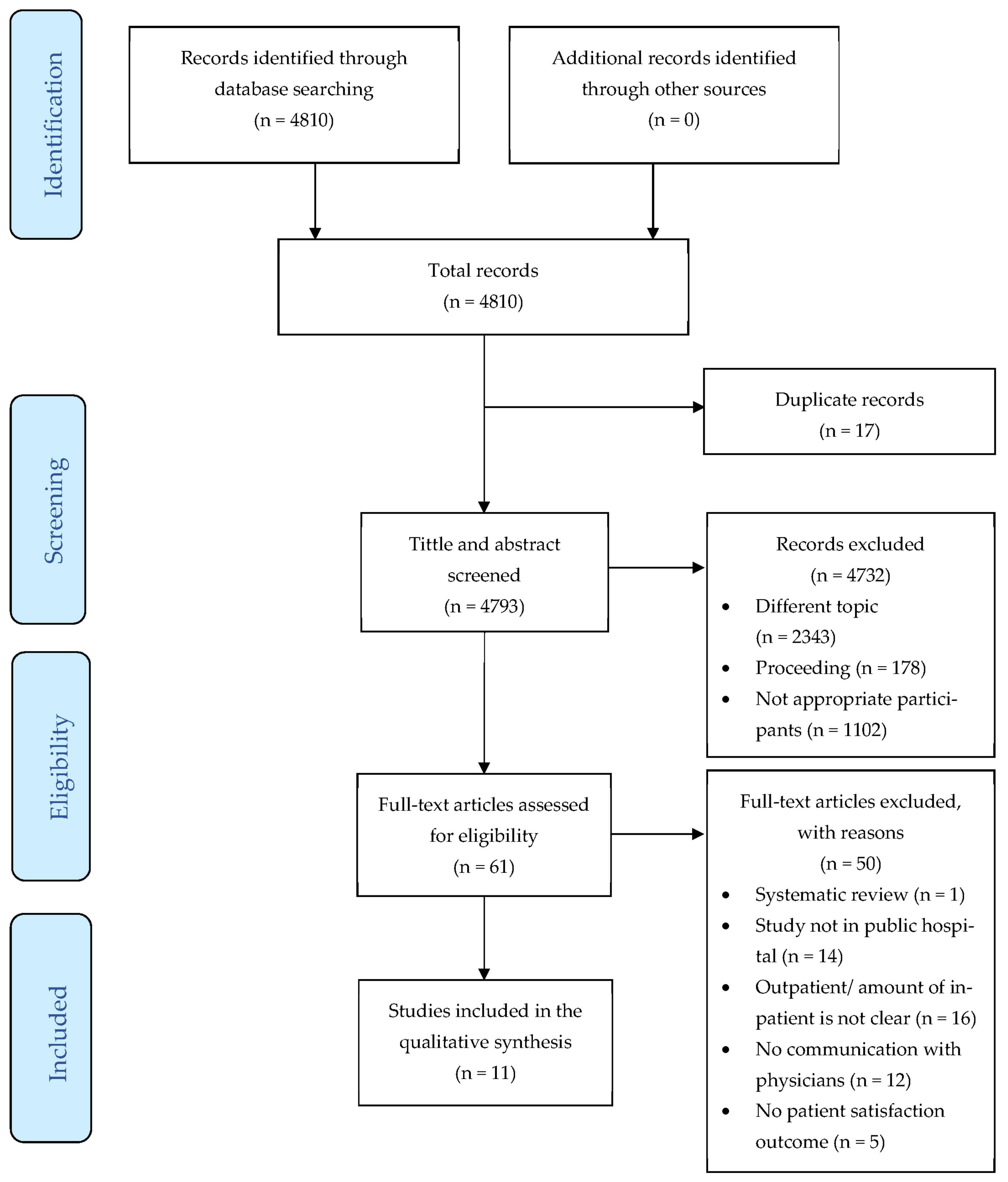
2.2. Search Strategy
2.3. Study Selection Criteria
2.4. Data Extraction and Synthesis
2.5. Quality Assessment
2.6. Statistical Analysis
3. Content Analysis and Result
3.1. Search Result
3.2. Study Characteristics
3.3. Participants’ Characteristics
4. Discussion
4.1. Overall Satisfaction
4.2. Determinant of Physician Communication Satisfaction
- Amounts of time spent with the patient: The study’s findings reveal that the amount of time spent with the patient has the most significant impact on patient satisfaction with physician communication. Five articles [25,36,37,38,43] show that patients expect physicians to spend more time communicating with them during interactions, especially in ward rounds. Even though there are no commonly agreed time limits for conversation or physical examination, most researchers believe that more time improves physician and patient treatment quality. Moreover, the frequency of ward rounds should be increased.
- Verbal and nonverbal indirect interpersonal communication: Three articles [36,39,42] explain that direct interpersonal communication is the key to patient satisfaction. In communicating with patients, physicians must be knowledgeable, friendly, informative, empathetic, be courteous, show respect, be open, be supportive, be positive, treat patients equally, be focused, show good behavior, have a good attitude, and feel valued. Moreover, the physician must be sensitive to the patient’s body movement and postural indicators. Additionally, physicians who were effective at expressing emotion through nonverbal communication received higher scores on the art of care from patients than physicians who were ineffective communicators. Furthermore, communication-based models tend to be more successful than communication-based on the picture at increasing patient satisfaction, reducing patient discomfort, improving communication ease, augmenting patient adherence, enhancing the interaction between physician and patient, and enhancing patient outcomes.
- Understand the demand of patients: The patient’s demands that affect physicians’ communication satisfaction are summarized from five articles [25,36,38,39,41,44] that support this argument. Several patient demands which affect patient satisfaction are expected to be obtained from physicians. For example, these include complete information about their illness; more input into their care and treatment decisions; listening to their views of treatment; receiving notification before treatment; having their dignity respected; allowing the patient’s family to speak with the physician; and notifying patients of danger signals regarding their disease/treatment/possible complications of the condition after they went home.
4.3. Organizational Determinants
- Interpreter service and the simplifying of medical terms into layperson terminology: The key in physician-patient communication is understanding the language being spoken in order to provide their complaints. The study revealed that some patients could not communicate with physicians and nurses owing to language barriers [36]. Almost unanimously, they expressed dissatisfaction with the lack of interpretation services. Additionally, it was discovered in this study that the language barrier was not solely due to the patient’s inability to communicate in the same language as the physician but was also due to the physician’s inability to translate medical terminology into plain terms that were easily understood by the patient [44]. Therefore, hospital management is obligated to provide translation services using terminologies that patients easily understand.
- Physician’s workload: The study results [40] found that physician workload substantially affects patient perceptions of physician communication. This result is due to the prevalence of physician fatigue, which could impact patient quality of treatment and experience. Due to the hospital’s objective in gaining market share and aligning physician incentives, the hospital relies increasingly on full-time physicians who determine physician workload or staffing levels. In addition, hospitals with a higher profit margin and a more significant physical footprint have lower patient ratings for physician communication [40]. Moreover, hospitals seeking big profits tend to use internships or residents who are paid less but also lack communication skills [37].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Świątoniowska-Lonc, N.; Polański, J.; Tański, W.; Jankowska-Polańska, B. Impact of satisfaction with physician-patient communication on self-care and adherence in patients with hypertension: Cross-sectional study. BMC Health Serv. Res. 2020, 20, 1046. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.H.Y.; Luk, B.H.K. Patient satisfaction: Concept analysis in the healthcare context. Patient Educ. Couns. 2019, 102, 790–796. [Google Scholar] [CrossRef] [PubMed]
- Avcılar, M.; Demirgüneş, B. The Effect of Cognitive Dissonance on External Information Search and Consumer Complaint Responses. Int. J. Bus. Adm. 2017, 8, 57–72. [Google Scholar]
- Andaleeb, S.S.; Siddiqui, N.; Khandakar, S. Patient satisfaction with health services in Bangladesh. Health Policy Plan. 2007, 22, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Gunaratne, R.; Pratt, D.N.; Banda, J.; Fick, D.P.; Khan, R.J.K.; Robertson, B.W. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J. Arthroplast. 2017, 32, 3854–3860. [Google Scholar] [CrossRef] [PubMed]
- Belasen, A.; Belasen, A.T. Doctor-patient communication: A review and a rationale for using an assessment framework. J. Health Organ. Manag. 2018, 32, 891–907. [Google Scholar] [CrossRef] [PubMed]
- McFarland, D.C.; Shen, M.J.; Parker, P.; Meyerson, S.; Holcombe, R.F. Does Hospital Size Affect Patient Satisfaction? Qual. Manag. Health Care 2017, 26, 205–209. [Google Scholar] [CrossRef]
- Allenbaugh, J.; Corbelli, J.; Rack, L.; Rubio, D.; Spagnoletti, C. A Brief Communication Curriculum Improves Resident and Nurse Communication Skills and Patient Satisfaction. J. Gen. Intern. Med. 2019, 34, 1167–1173. [Google Scholar] [CrossRef] [Green Version]
- Trant, A.A.; Szekely, B.; Mougalian, S.S.; DiGiovanna, M.P.; Sanft, T.; Hofstatter, E.; Silber, A.; Adelson, K.B.; Chagpar, A.; Killelea, B.; et al. The impact of communication style on patient satisfaction. Breast Cancer Res. Treat. 2019, 176, 349–356. [Google Scholar] [CrossRef]
- Steiner-Hofbauer, V.; Schrank, B.; Holzinger, A. What is a good doctor? Wien. Med. Wochenschr. 2018, 168, 398–405. [Google Scholar] [CrossRef] [Green Version]
- Tavakoly Sany, S.B.; Behzhad, F.; Ferns, G.; Peyman, N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: A randomized controlled trial. BMC Health Serv. Res. 2020, 20, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuoka, K.; Ishikawa, H.; Nakayama, T.; Honzawa, Y.; Maemoto, A.; Hirai, F.; Ueno, F.; Sato, N.; Susuta, Y.; Hibi, T. Physician-patient communication affects patient satisfaction in treatment decision-making: A structural equation modelling analysis of a web-based survey in patients with ulcerative colitis. J. Gastroenterol. 2021, 56, 843–855. [Google Scholar] [CrossRef] [PubMed]
- Hodsdon, A.; Smith, N.A.; Story, D.A. Preoperative communication between anaesthetists and patients with obesity regarding perioperative risks and weight management: A structured narrative review. Perioper. Med. 2020, 9, 24. [Google Scholar] [CrossRef] [PubMed]
- Burgener, A.M. Enhancing Communication to Improve Patient Safety and to Increase Patient Satisfaction. Health Care Manag. 2017, 36, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Zakaria, M.; Karim, R.; Rahman, M.; Cheng, F.; Xu, J. Disparity in physician-patient communication by ethnicity: Evidence from Bangladesh. Int. J. Equity Health 2021, 20, 65. [Google Scholar] [CrossRef] [PubMed]
- Licqurish, S.M.; Cook, O.Y.; Pattuwage, L.P.; Saunders, C.; Jefford, M.; Koczwara, B.; Johnson, C.E.; Emery, J.D. Tools to facilitate communication during physician-patient consultations in cancer care: An overview of systematic reviews. CA Cancer J. Clin. 2019, 69, 497–520. [Google Scholar] [CrossRef]
- Berkey, F.J.; Wiedemer, J.P.; Vithalani, N.D. Delivering Bad or Life-Altering News. Am. Fam. Physician 2018, 98, 99–104. [Google Scholar]
- Edwards, W.F.; Malik, S.; Peters, J.; Chippendale, I.; Ravits, J. Delivering Bad News in Amyotrophic Lateral Sclerosis: Proposal of Specific Technique ALS ALLOW. Neurol. Clin. Pract. 2021, 11, 521–526. [Google Scholar] [CrossRef]
- Schwartz, R.; Dubey, M.; Blanch-Hartigan, D.; Sanders, J.J.; Hall, J.A. Physician empathy according to physicians: A multi-specialty qualitative analysis. Patient Educ. Couns. 2021, 104, 2425–2431. [Google Scholar] [CrossRef]
- Kebede, B.G.; Abraha, A.; Andersson, R.; Munthe, C.; Linderholm, M.; Linderholm, B.; Berbyuk Lindström, N. Communicative challenges among physicians, patients, and family caregivers in cancer care: An exploratory qualitative study in Ethiopia. PLoS ONE 2020, 15, e0230309. [Google Scholar] [CrossRef]
- Berger, Z.D.; Boss, E.F.; Beach, M.C. Communication behaviors and patient autonomy in hospital care: A qualitative study. Patient Educ. Couns. 2017, 100, 1473–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCabe, R.; Healey, P.G.T. Miscommunication in Doctor-Patient Communication. Top. Cogn. Sci. 2018, 10, 409–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Légaré, F.; Turcotte, S.; Stacey, D.; Ratté, S.; Kryworuchko, J.; Graham, I.D. Patients’ perceptions of sharing in decisions: A systematic review of interventions to enhance shared decision making in routine clinical practice. Patient 2012, 5, 1–19. [Google Scholar] [CrossRef]
- Rudd, R.E. Health literacy skills of U.S. adults. Am. J. Health Behav. 2007, 31 (Suppl. 1), S8–S18. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.L.; Leung, M.C.; Cheung, A.W.; Yam, C.H.; Yeoh, E.K.; Griffiths, S. A population-based survey using PPE-15: Relationship of care aspects to patient satisfaction in Hong Kong. Int. J. Qual. Health Care J. Int. Soc. Qual. Health Care 2011, 23, 390–396. [Google Scholar] [CrossRef]
- Mohammadi, A.; Kamali, K. In Inpatients Perceptions of Physicians Empathy and Their Level of Satisfaction Regarding Medical Care Measured by Jefferson Scale of Patien” s Perceptions of Physician Empathy. J. Iran Med. Counc. 2019, 2, 120–127. [Google Scholar]
- Safavi, K. Patient-centered pay for performance: Are we missing the target? J. Healthc. Manag. Am. Coll. Healthc. Exec. 2006, 51, 215–218. [Google Scholar] [CrossRef]
- Janssen, S.M.; Lagro-Janssen, A.L.M. Physician’s gender, communication style, patient preferences and patient satisfaction in gynecology and obstetrics: A systematic review. Patient Educ. Couns. 2012, 89, 221–226. [Google Scholar] [CrossRef]
- Oliveira, V.C.; Refshauge, K.M.; Ferreira, M.L.; Pinto, R.Z.; Beckenkamp, P.R.; Negrao Filho, R.F.; Ferreira, P.H. Communication that values patient autonomy is associated with satisfaction with care: A systematic review. J. Physiother. 2012, 58, 215–229. [Google Scholar] [CrossRef] [Green Version]
- Henry, S.G.; Fuhrel-Forbis, A.; Rogers, M.A.M.; Eggly, S. Association between nonverbal communication during clinical interactions and outcomes: A systematic review and meta-analysis. Patient Educ. Couns. 2012, 86, 297–315. [Google Scholar] [CrossRef]
- Uitterhoeve, R.J.; Bensing, J.M.; Grol, R.P.; Demulder, P.H.M.; Van Achterberg, T. The effect of communication skills training on patient outcomes in cancer care: A systematic review of the literature. Eur. J. Cancer Care 2010, 19, 442–457. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joanna Briggs Institute. Cheklist for Sytematical Reviews and Research Syntheses. Available online: https://jbi.global/critical-appraisal-tools (accessed on 20 October 2021).
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Woldeyohanes, T.R.; Woldehaimanot, T.E.; Kerie, M.W.; Mengistie, M.A.; Yesuf, E.A. Perceived patient satisfaction with in-patient services at Jimma University Specialized Hospital, Southwest Ethiopia. BMC Res. Notes 2015, 8, 285. [Google Scholar] [CrossRef] [PubMed]
- Zewdneh, D.; Michael, K.; Kebede, S. Communication skills of physicians during patient interaction in an in-patient setting at Tikur Anbessa Specialized Teaching Hospital (TASH), Addis Ababa, Ethiopia, 2009. Ethiop. J. Health Dev. 2011, 25, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Ke, P.; Jiang, F.; Wu, D.; Ke, L.; Lin, Z.; Jia, J.; Ye, B.; Liu, B. A third-party investigation of inpatient satisfaction with a tertiary hospital in People’s Republic of China. Patient Prefer. Adherence 2018, 12, 2027–2037. [Google Scholar] [CrossRef] [Green Version]
- Hu, W.; Song, Y.; Zhong, X.; Feng, J.; Wang, P.; Huang, C. Improving doctor-patient communication: Content validity examination of a novel urinary system-simulating physical model. Patient Prefer. Adherence 2016, 10, 2519–2529. [Google Scholar] [CrossRef] [Green Version]
- Al-Amin, M.; Makarem, S.C. The Effects of Hospital-Level Factors on Patients’ Ratings of Physician Communication. J. Healthc. Manag. Am. Coll. Healthc. Exec. 2016, 61, 28–41. [Google Scholar]
- Zinn, W.; Sauer, S.; Göllner, R. The German Inpatient Satisfaction Scale. SAGE Open 2016, 6, 215824401664314. [Google Scholar] [CrossRef] [Green Version]
- Effendi, R.; Sukmayadi, V.; Pandjaitan, I. The Effects of Doctors’ Interpersonal Communication on Low-Income Inpatients’ Satisfaction Level. J. Komun. Malays. J. Commun. 2019, 35, 57–70. [Google Scholar] [CrossRef] [Green Version]
- Chae, W.; Kim, J.; Park, E.C.; Jang, S.I. Comparison of patient satisfaction in inpatient care provided by hospitalists and nonhospitalists in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 8101. [Google Scholar] [CrossRef] [PubMed]
- Chia, Y.Y.P.; Ekladious, A. Australian public hospital inpatient satisfaction related to early patient involvement and shared decision-making in discharge planning. Intern. Med. J. 2021, 51, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Pinto Taylor, E.; Mulenos, A.; Chatterjee, A.; Talwalkar, J.S. Partnering With Interpreter Services: Standardized Patient Cases to Improve Communication With Limited English Proficiency Patients. MedEdPORTAL 2019, 15, 10826. [Google Scholar] [CrossRef] [PubMed]
- Beck, R.S.; Daughtridge, R.; Sloane, P.D. Physician-patient communication in the primary care office: A systematic review. J. Am. Board Fam. Pract. 2002, 15, 25–38. [Google Scholar] [PubMed]
- Baranowska, B.; Pawlicka, P.; Kiersnowska, I.; Misztal, A.; Kajdy, A.; Sys, D.; Doroszewska, A. Woman’s Needs and Satisfaction Regarding the Communication with Doctors and Midwives during Labour, Delivery and Early Postpartum. Healthcare 2021, 9, 382. [Google Scholar] [CrossRef]
- Grocott, A.; McSherry, W. The Patient Experience: Informing Practice through Identification of Meaningful Communication from the Patient’s Perspective. Healthcare 2018, 6, 26. [Google Scholar] [CrossRef] [Green Version]
- Batbaatar, E.; Dorjdagva, J.; Luvsannyam, A.; Savino, M.M.; Amenta, P. Determinants of patient satisfaction: A systematic review. Perspect. Public Health 2017, 137, 89–101. [Google Scholar] [CrossRef]
- Salin, S.; Kaunonen, M.; Aalto, P. Explaining patient satisfaction with outpatient care using data-based nurse staffing indicators. J. Nurs. Adm. 2012, 42, 592–597. [Google Scholar] [CrossRef]
- McGrowder, D.A.; Miller, F.G.; Vaz, K.; Anderson Cross, M.; Anderson-Jackson, L.; Bryan, S.; Latore, L.; Thompson, R.; Lowe, D.; McFarlane, S.R.; et al. The Utilization and Benefits of Telehealth Services by Health Care Professionals Managing Breast Cancer Patients during the COVID-19 Pandemic. Healthcare 2021, 9, 1401. [Google Scholar] [CrossRef]
- Giansanti, D.; Veltro, G. The Digital Divide in the Era of COVID-19: An Investigation into an Important Obstacle to the Access to the mHealth by the Citizen. Healthcare 2021, 9, 371. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.; Liu, Y.; Lee, E.; Yadav, K. Telehealth Solutions for In-hospital Communication with Patients Under Isolation During COVID-19. West. J. Emerg. Med. 2020, 21, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Bains, J.; Greenwald, P.W.; Mulcare, M.R.; Leyden, D.; Kim, J.; Shemesh, A.J.; Bodnar, D.; Farmer, B.; Steel, P.; Tanouye, R.; et al. Utilizing Telemedicine in a Novel Approach to COVID-19 Management and Patient Experience in the Emergency Department. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2021, 27, 254–260. [Google Scholar] [CrossRef]
- Bhanot, N.; Dimitriou, G.; McAninch, L.; Rossi, C.; Thompson, D.; Manzi, S. Perspectives of Health Care Providers in an Integrated Health Care Delivery Network on Inpatient Electronic Consultation (e-Consult) Use During the COVID-19 Pandemic. J. Patient Exp. 2021, 8, 23743735211007696. [Google Scholar] [CrossRef] [PubMed]
- Garg, A.; Goyal, S.; Thati, R.; Thati, N. Implementation of Telemedicine in a Tertiary Hospital-Based Ambulatory Practice in Detroit During the COVID-19 Pandemic: Observational Study. JMIR Public Health Surveill. 2021, 7, e21327. [Google Scholar] [CrossRef]
- Kato-Lin, Y.C.; Thelen, S.T. Telemedicine for Acute Conditions During COVID-19: A Nationwide Survey Using Crowdsourcing. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2021, 27, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Sierra Marín, S.D.; Gomez-Vargas, D.; Céspedes, N.; Múnera, M.; Roberti, F.; Barria, P.; Ramamoorthy, S.; Becker, M.; Carelli, R.; Cifuentes, C.A. Expectations and Perceptions of Healthcare Professionals for Robot Deployment in Hospital Environments During the COVID-19 Pandemic. Front. Robot. AI 2021, 8, 612746. [Google Scholar] [CrossRef]
| Symmetric Measures | |||||
|---|---|---|---|---|---|
| Value | Asymptotic Standard Error a | Approximate T b | Approximate Significance | ||
| Measure of Agreement | Kappa | 0.666 | 0.141 | 48.928 | 0.000 |
| N of Valid Cases | 4793 | ||||
| Symmetric Measures | |||||
|---|---|---|---|---|---|
| Value | Asymptotic Standard Error a | Approximate T b | Approximate Significance | ||
| Measure of Agreement | Kappa | 0.640 | 0.192 | 5.039 | 0.000 |
| N of Valid Cases | 61 | ||||
| Symmetric Measures | |||||
|---|---|---|---|---|---|
| Value | Asymptotic Standard Error a | Approximate T b | Approximate Significance | ||
| Measure of Agreement | Kappa | 0.621 | 0.335 | 2.225 | 0.026 |
| N of Valid Cases | 11 | ||||
| Author, Year | Country | Study Design | Sample Size | Hospital Ownership | Outcome Measurement | Overall Satisfaction | Satisfaction Finding | |
|---|---|---|---|---|---|---|---|---|
| 1 | Wong et al., 2011 [25] | Hongkong | cross-sectional study | 1264 patients | public and private | Picker Patient Experience Questionnaire-15 (PPE-15) | satisfied |
|
| 2 | Zewdneh et al., 2011 [37] | Ethiopia | cross-sectional study | 211 patients | public | Lehman’s and Kraan’s standard checklist (Maastricht checklist) | needs further improvements |
|
| 3 | Woldeyohanes et al., 2015 [36] | Ethiopia | cross-sectional study | 189 patients | public | Two sets of standardized structured questionnaires were created for data collection after conducting a literature study | needs further improvements |
|
| 4 | Al-Amin and Makarem, 2016 [40] | USA | cross sectional study | 2756 hospitals | Public and private | Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) | needs further improvements |
|
| 5 | Zin et al., 2016 [41] | Germany, Switzerland, and Austria | cross-sectional study | 116,325 patients | Public and private | German Inpatient Satisfaction Scale (GISS) | satisfied |
|
| 6 | Hu et al., 2016 [39] | China | Experimental Study | 240 patients | public | Demographic Information Survey Scale and a Medical Interview and Satisfaction Scale (MISS) | satisfied |
|
| 7 | Ke et al., 2018 [38] | China | cross-sectional study | 872 patients | public | Inpatient Patient Satisfaction Questionnaire Developed by Chongqing Zhidao Hospital Management Corporation | needs further improvements |
|
| 8 | Effendi et al., 2019 [42] | Indonesia | cross-sectional study | 72 patients | public | Openness, empathy, supportiveness, positiveness, and equality | satisfied |
|
| 9 | Ali and Koorosh, 2019 [26] | Iran | cross-sectional study | 285 patients | public | The Jefferson Scale of Patient’s Perceptions of PhysicianEmpathy (JSPPPE) | satisfied |
|
| 10 | Chae et al., 2021 [43] | Korea | cross-sectional study | 2181 patients | public | The questionnaire was developed from Tools for Assessing Patient Satisfaction with Services from Hospitalists and Hospital Consumer Assessments from Healthcare Providers and Systems | satisfied |
|
| 11 | Chia and Ekladious, 2021 [44] | Australia | Cohort study | 50 patients | public | a multiple-choice questionnaire was devised specifically for the study | needs further improvements |
|
| Joanna Briggs Institute Checklists | Wong et al., 2011 | Zewdneh et al., 2011 | Woldeyohanes et al., 2015 | Al-Amin and Makarem, 2016 | Zin et al., 2016 | Hu et al., 2016 | Ke et al., 2018 | Effendi et al., 2019 | Ali and Koorosh, 2019 | Chae et al., 2021 | Chia and Ekladious, 2021 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cross-sectional studies | |||||||||||
| Are the criteria for inclusion in the sample clearly defined? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Were the study subjects and the setting described in detail? | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | ||
| Was the exposure measured validly and reliably? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Were objective, standard criteria used for measurement of the condition? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Were confounding factors identified? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Were strategies to deal with confounding factors stated? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Were the outcomes measured validly and reliably? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Was appropriate statistical analysis used? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| Experimental Studies | |||||||||||
| Are ‘cause’ and ‘effect’ clear in the study (i.e., there is no confusion about which variable comes first)? | 1 | ||||||||||
| Were the participants included in any similar comparisons? | 1 | ||||||||||
| Were the participants included in any comparisons receiving similar treatment/care other than with regard to the exposure or intervention of interest? | 1 | ||||||||||
| Was there a control group? | 1 | ||||||||||
| Were there multiple measurements of the outcome, both before and after the intervention/exposure? | 1 | ||||||||||
| Was follow-up complete, and if not, were differences between groups in terms of their follow-up adequately described and analyzed? | 1 | ||||||||||
| Were the outcomes of participants included in any comparisons measured in the same way? | 1 | ||||||||||
| Were outcomes measured reliably? | 1 | ||||||||||
| Was appropriate statistical analysis used? | 1 | ||||||||||
| Cohort Study | |||||||||||
| Were the two groups similar and recruited from the same population? | 1 | ||||||||||
| Were the exposures measured similarly to assign people to both exposed and unexposed groups? | 1 | ||||||||||
| Was the exposure measured validly and reliably? | 1 | ||||||||||
| Were confounding factors identified? | 1 | ||||||||||
| Were strategies to deal with confounding factors stated? | 1 | ||||||||||
| Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)? | 1 | ||||||||||
| Were the outcomes measured validly and reliably? | 1 | ||||||||||
| Was the follow-up time reported and sufficient to be long enough for outcomes to occur? | 1 | ||||||||||
| Was follow-up complete, and if not, were the reasons for follow-up loss described and explored? | 1 | ||||||||||
| Were strategies to address incomplete follow-up utilized? | 1 | ||||||||||
| Was appropriate statistical analysis used? | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moslehpour, M.; Shalehah, A.; Rahman, F.F.; Lin, K.-H. The Effect of Physician Communication on Inpatient Satisfaction. Healthcare 2022, 10, 463. https://doi.org/10.3390/healthcare10030463
Moslehpour M, Shalehah A, Rahman FF, Lin K-H. The Effect of Physician Communication on Inpatient Satisfaction. Healthcare. 2022; 10(3):463. https://doi.org/10.3390/healthcare10030463
Chicago/Turabian StyleMoslehpour, Massoud, Anita Shalehah, Ferry Fadzlul Rahman, and Kuan-Han Lin. 2022. "The Effect of Physician Communication on Inpatient Satisfaction" Healthcare 10, no. 3: 463. https://doi.org/10.3390/healthcare10030463
APA StyleMoslehpour, M., Shalehah, A., Rahman, F. F., & Lin, K.-H. (2022). The Effect of Physician Communication on Inpatient Satisfaction. Healthcare, 10(3), 463. https://doi.org/10.3390/healthcare10030463









