Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital
Abstract
:1. Introduction
1.1. Background
1.2. Literature Review
2. Materials and Methods
2.1. Instrumentation
2.2. Study Design
2.3. Statistical Data Analysis
3. Results
4. Discussion
“I want to be recognized for my hard work, but I feel like it will swing back to the other side, to mistrust and lack of support. If you think about traditional societies, the position of a healer is very respected, but it is also accountable to the community.”[40]
Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wen, T.; Zhang, Y.; Wang, X.; Tang, G. Factors influencing turnover intention among primary care doctors: A cross-sectional study in Chongqing, China. Hum. Resour. Health 2018, 16, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, H.A.; McGeary, C.A.; Finley, E.P.; Ketchum, N.S.; McGeary, D.D.; Peterson, A.L. Burnout among psychiatrists in the Veterans Health Administration. Burn. Res. 2015, 2, 108–114. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Mental Health in the Workplace. 2019. Available online: https://www.who.int/news-room/commentaries/detail/mental-health-in-the-workplace (accessed on 18 February 2022).
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welsh, D. Predictors of depressive symptoms in female medical-surgical hospital nurses. Issues Ment. Health Nurs. 2009, 30, 320–326. [Google Scholar] [CrossRef] [PubMed]
- McManus, I.C.; Winder, B.C.; Gordon, D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002, 359, 2089–2090. [Google Scholar] [CrossRef]
- Leon, G.R. Overview of the psychosocial impact of disasters. Prehospital Disaster Med. 2004, 19, 4–9. [Google Scholar] [CrossRef]
- Adams, J.G.; Walls, R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA 2020, 323, 1439–1440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic: Interim Report, 27 August 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. World Health Organization Coronavirus (COVID-19) Dashboard 2021. 2021. Available online: https://covid19.who.int/ (accessed on 17 February 2022).
- HSY. Health Statistics Yearbook the Ministry of Health of Turkey Health Statistics Yearbook 2018. 2018. Available online: https://ohsad.org/wp-content/uploads/2020/01/SB_istatistik-y%C4%B1ll%C4%B1%C4%9F%C4%B1-2018_en.pdf (accessed on 17 February 2022).
- Yanchus, N.J.; Periard, D.; Osatuke, K. Further examination of predictors of turnover intention among mental health professionals. J. Psychiatr. Ment. Health Nurs. 2017, 24, 41–56. [Google Scholar] [CrossRef]
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baxter, A.J.; Scott, K.M.; Vos, T.; Whiteford, H.A. Global prevalence of anxiety disorders: A systematic review and meta-regression. Psychol. Med. 2013, 43, 897–910. [Google Scholar] [CrossRef]
- RIOS KA, B.D.; Belasco, A. Evaluation of quality of life and depression in nursing technicians and nursing assistants. Rev. Latino-Am. Enferm. 2010, 18, 413–420. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T.; Guth, D.; Steer, R.A.; Ball, R. Screening for major depression disorders in medical inpatients with the Beck Depression Inventory for Primary Care. Behav. Res. Ther. 1997, 35, 785–791. [Google Scholar] [CrossRef]
- Brantley, P.J.; Dutton, G.R.; Wood, K.B. The Beck Depression Inventory-II (BDI-II) and the Beck Depression Inventory-Primary Care (BDI-PC). In The Use of Psychological Testing for Treatment Planning and Assessment Outcome; Maruish, M.E., Ed.; Lawrence Erlbaum Associates Publishers: Mahwah, NJ, USA, 2004. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Swift, P.; Cyhlarova, E.; Goldie, I.; O’Sullivan, C.; Bristow, P.; Carson, J.; Biggs, H.; Edwards, J. Living with anxiety: Understanding the role and impact of anxiety in our lives. Ment. Health Found. 2014, 1–48. Available online: https://www.mentalhealth.org.uk/sites/default/files/living-with-anxiety-report.pdf (accessed on 16 February 2022).
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chlan, L.; Savik, K.; Weinert, C. Development of a shortened state anxiety scale from the Spielberger State-Trait Anxiety Inventory (STAI) for patients receiving mechanical ventilatory support. J. Nurs. Meas. 2003, 11, 283–293. [Google Scholar] [CrossRef] [PubMed]
- Spielberger, C.D.; Gonzalez-Reigosa, F.; Martinez-Urrutia, A.; Natalicio, L.F.; Natalicio, D.S. The state-trait anxiety inventory. Rev. Interam. De Psicol./Interam. J. Psychol. 1971, 5. Available online: https://journal.sipsych.org/index.php/IJP/article/view/620 (accessed on 18 February 2022).
- Freudenberger, H.J. Staff burn-out. J. Soc. Issues 1974, 30, 159–165. [Google Scholar] [CrossRef]
- Carson, J.; Maal, S.; Roche, S.; Fagin, L.; De Villiers, N.; O’Malley, P.; Brown, D.; Leary, J.; Holloway, F. Burnout in mental health nurses: Much ado about nothing? Stress Med. 1999, 15, 127–134. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B.; Nachreiner, F.; Schaufeli, W.B. A model of burnout and life satisfaction amongst nurses. J. Adv. Nurs. 2000, 32, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach Burnout Inventory. In Evaluating Stress: A Book of Resources, 3rd ed.; Zalaquett, C.P., Wood, R.J., Eds.; Scarecrow Education: Lanham, MD, USA, 1997; pp. 191–218. [Google Scholar]
- Malach-Pines, A. The burnout measure, short version. Int. J. Stress Manag. 2005, 12, 78. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B.; Hoogduin, K.; Schaap, C.; Kladler, A. On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol. Health 2001, 16, 565–582. [Google Scholar] [CrossRef]
- Demerouti, E.; Bakker, A.B. The Oldenburg Burnout Inventory: A good alternative to measure burnout and engagement. Handb. Stress Burn. Health Care 2008, 65, 78. [Google Scholar]
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work. Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Prices, J.; Mueller, C. A causal model of turnover for nurses. Acad. Manag. 1986, 24, 543–565. [Google Scholar] [CrossRef]
- Steel, R.P.; Ovalle, N.K. A review and meta-analysis of research on the relationship between behavioral intentions and employee turnover. J. Appl. Psychol. 1984, 69, 673. [Google Scholar] [CrossRef]
- Krausz, M.; Müller-Thomsen, T.; Haasen, C. Suicide among schizophrenic adolescents in the long-term course of illness. Psychopathology 1995, 28, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.; Leiter, M. Maslach Burnout Inventory Manual, 3rd ed.; Consult. Psychol. Press Inc.: Palo Alto, CA, USA, 1996. [Google Scholar]
- Walsh, J.P.; Ashford, S.J.; Hill, T.E. Feedback obstruction: The influence of the information environment on employee turnover intentions. Hum. Relat. 1985, 38, 23–46. [Google Scholar] [CrossRef]
- Liu, Z.; Han, B.; Jiang, R.; Huang, Y.; Ma, C.; Wen, J.; Zhang, T.; Wang, Y.; Chen, H.; Ma, Y. Mental health status of doctors and nurses during COVID-19 epidemic in China. Ann. Glob. Health 2020. [Google Scholar] [CrossRef]
- Johnson, S.B.; Butcher, F. Doctors during the COVID-19 pandemic: What are their duties and what is owed to them? J. Med. Ethics 2021, 47, 12–15. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
- Jilian Mock, J.S. How Doctors and Nurses Manage Coronavirus Grief. In Scientific American; 2021; Available online: https://www.scientificamerican.com/interactive/grief-on-the-front-line-and-beyond/ (accessed on 16 February 2022).
- Ramírez, M.R.; Otero, P.; Blanco, V.; Ontaneda, M.P.; Díaz, O.; Vázquez, F.L. Prevalence and correlates of burnout in health professionals in Ecuador. Compr. Psychiatry 2018, 82, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Fischhoff, B. Making Decisions in a COVID-19 World. JAMA 2020, 324, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Masum, A.K.M.; Azad, M.A.K.; Hoque, K.E.; Beh, L.-S.; Wanke, P.; Arslan, Ö. Job satisfaction and intention to quit: An empirical analysis of nurses in Turkey. PeerJ 2016, 4, e1896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ansmann, L.; Wirtz, M.; Kowalski, C.; Pfaff, H.; Visser, A.; Ernstmann, N. The impact of the hospital work environment on social support from physicians in breast cancer care. Patient Educ. Couns. 2014, 96, 352–360. [Google Scholar] [CrossRef] [PubMed]
- Elkefi, S.; Yu, Z.; Asan, O. Online medical record nonuse Among patients: Data analysis study of the 2019 health information national trends survey. J. Med. Internet Res. 2021, 23, e24767. [Google Scholar] [CrossRef] [PubMed]


| Predictors | PHQ9 | ANXIETY1 | ANXIETY2 | Burnout | Total % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L 1 | M 2 | S 3 | L | M | S | L | M | S | L | M | S | |||
| Sex | Male | 17.21% | 4.84% | 25.93% | 24.00% | 17.14% | 14.61% | 16.28% | 11.67% | 17.78% | 17.50% | 14.08% | 16.54% | 15.97% |
| Female | 82.79% | 95.16% | 74.07% | 76.00% | 82.86% | 85.39% | 83.72% | 88.33% | 82.22% | 82.50% | 85.92% | 83.46% | 84.03% | |
| Education | Middle School | 62.30% | 69.35% | 75.93% | 76.00% | 62.86% | 66.85% | 79.07% | 60.00% | 66.67% | 52.50% | 56.34% | 77.95% | 67.23% |
| High School | 20.49% | 14.52% | 5.56% | 12.00% | 11.43% | 16.85% | 9.30% | 18.33% | 16.30% | 30.00% | 16.90% | 10.24% | 15.55% | |
| University | 4.10% | 14.52% | 12.96% | 12.00% | 5.71% | 8.99% | 4.65% | 5.00% | 11.85% | 12.50% | 14.08% | 4.72% | 8.82% | |
| Doctorate | 13.11% | 1.61% | 5.56% | 0.00% | 20.00% | 7.30% | 6.98% | 16.67% | 5.19% | 5.00% | 12.68% | 7.09% | 8.40% | |
| Job Position | Health Staff | 56.56% | 50.00% | 44.44% | 52.00% | 48.57% | 52.81% | 46.51% | 51.67% | 54.07% | 67.50% | 57.75% | 44.09% | 52.10% |
| Nurse or Midwife | 18.85% | 40.32% | 40.74% | 28.00% | 22.86% | 30.90% | 30.23% | 21.67% | 32.59% | 17.50% | 19.72% | 38.58% | 29.41% | |
| Doctor | 24.59% | 9.68% | 14.81% | 20.00% | 28.57% | 16.29% | 23.26% | 26.67% | 13.33% | 15.00% | 22.54% | 17.32% | 18.49% | |
| Department | Other | 36.89% | 16.13% | 20.37% | 48.00% | 31.43% | 24.16% | 30.23% | 30.00% | 25.93% | 42.50% | 29.58% | 22.05% | 27.73% |
| ER | 41.80% | 43.55% | 40.74% | 20.00% | 42.86% | 44.94% | 41.86% | 45.00% | 40.74% | 27.50% | 45.07% | 44.88% | 42.02% | |
| Inpatient Unit | 18.03% | 27.42% | 29.63% | 24.00% | 20.00% | 23.60% | 23.26% | 18.33% | 25.19% | 20.00% | 18.31% | 26.77% | 23.11% | |
| ICU | 3.28% | 12.90% | 9.26% | 8.00% | 5.71% | 7.30% | 4.65% | 6.67% | 8.15% | 10.00% | 7.04% | 6.30% | 7.14% | |
| Age | Young Adults | 57.38% | 58.06% | 64.81% | 64.00% | 62.86% | 57.87% | 60.47% | 61.67% | 57.78% | 60.00% | 47.89% | 65.35% | 59.24% |
| Middle Age or More | 42.62% | 41.94% | 35.19% | 36.00% | 37.14% | 42.13% | 39.53% | 38.33% | 42.22% | 40.00% | 52.11% | 34.65% | 40.76% | |
| Total % | 51.26% | 26.05% | 22.69% | 10.50% | 14.71% | 74.79% | 18.07% | 25.21% | 56.72% | 16.81% | 29.83% | 53.36% | 51.26% | |
| Predictors | People Who Have the Intention to Leave (%) | p-Value | |
|---|---|---|---|
| Sex | Male | 51.52% | 0.542 |
| Female | 48.48% | ||
| Education | Middle School | 75.76% | 0.233 |
| High School | 10.61% | ||
| University | 1.52% | ||
| Doctorate | 12.12% | ||
| Job Position | Health Staff | 39.39% | 0.0517 * |
| Nurse or Midwife | 37.88% | ||
| Doctor | 22.73% | ||
| Department | Other | 19.70% | 0.0423 * |
| ER | 45.45% | ||
| Inpatient Unit | 28.79% | ||
| ICU | 6.06% | ||
| Age | Young Adults | 86.36% | 0.594 |
| Middle Age or More | 13.64% | ||
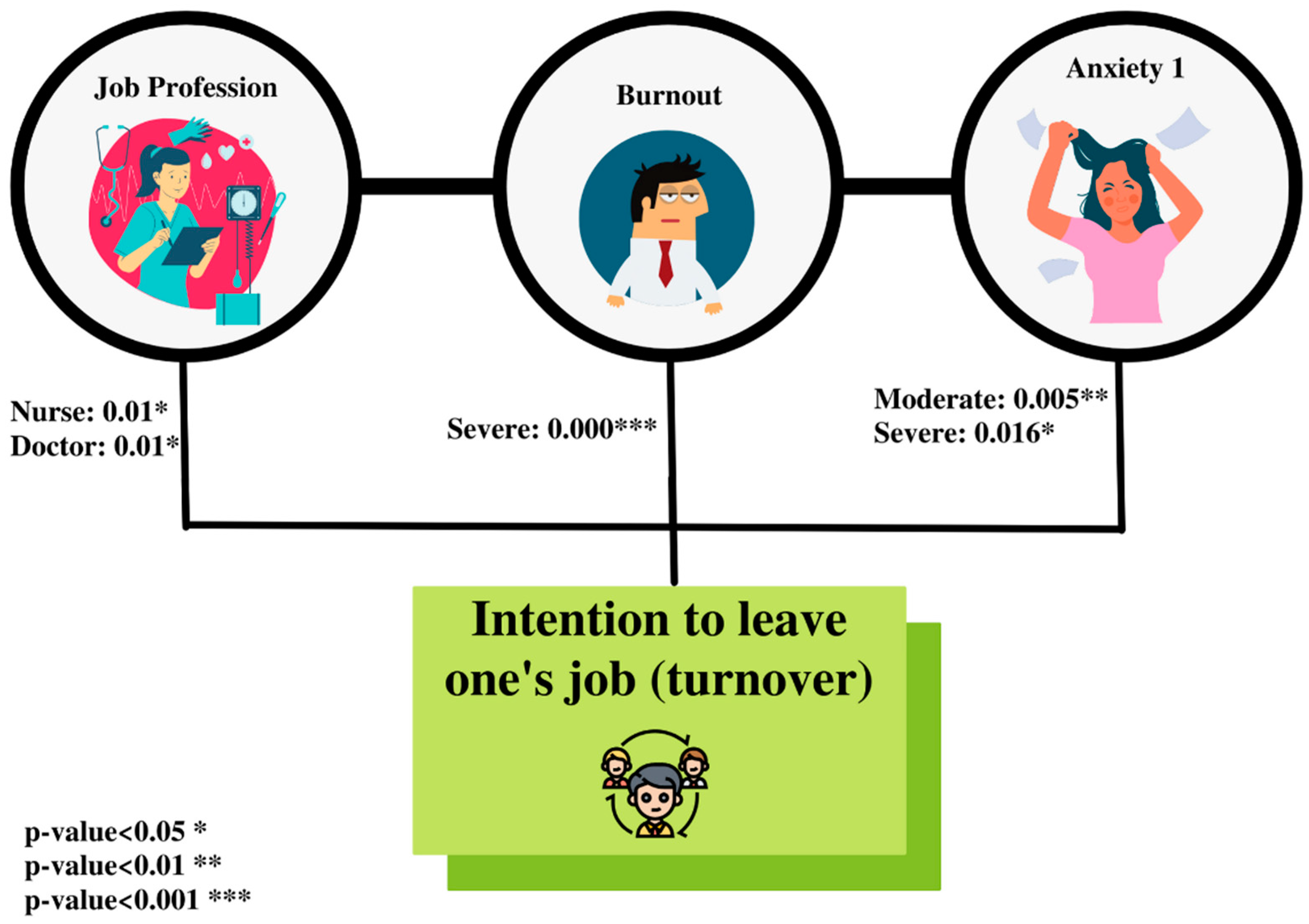
| Predictors | Odds Ratios | p-Value | |
|---|---|---|---|
| PHQ9 | Low | NA | |
| Moderate | 4.79 (0.90–33.06) | 0.08 | |
| Severe | 12.53 (1.18–368.37) | 0.06 | |
| Anxiety 1 | Low | NA | |
| Moderate | 18.96 (6.75–137.69) | 0.005 ** | |
| Severe | 37.94 (2.46–107.40) | 0.016 * | |
| Anxiety 2 | Low | NA | |
| Moderate | 0.16 (0.008–1.88) | 0.17 | |
| Severe | 0.14 (0.008–1.43) | 0.12 | |
| Burnout | Low | NA | |
| Moderate | 9.97 (1.03–164.48) | 0.06 | |
| Severe | 13.05 (1.10–33.48) | 0.000 *** | |
| Department | Other | NA | |
| ER | 3.22 (0.56–22.40) | 0.2 | |
| Inpatient Unit | 2.83 (0.39–23.74) | 0.3 | |
| ICU | 3.30 (0.06–576.09) | 0.57 | |
| Job Position | Health staff | NA | |
| Nurse/midwife | 22.28 (2.78–41.25) | 0.01 * | |
| Doctor | 18.13 (2.22–25.27) | 0.01 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tabur, A.; Elkefi, S.; Emhan, A.; Mengenci, C.; Bez, Y.; Asan, O. Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital. Healthcare 2022, 10, 525. https://doi.org/10.3390/healthcare10030525
Tabur A, Elkefi S, Emhan A, Mengenci C, Bez Y, Asan O. Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital. Healthcare. 2022; 10(3):525. https://doi.org/10.3390/healthcare10030525
Chicago/Turabian StyleTabur, Ayhan, Safa Elkefi, Abdurrahim Emhan, Cengiz Mengenci, Yasin Bez, and Onur Asan. 2022. "Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital" Healthcare 10, no. 3: 525. https://doi.org/10.3390/healthcare10030525







