The Effectiveness of Equine Therapy Intervention on Activities of Daily Living, Quality of Life, Mood, Balance and Gait in Individuals with Parkinson’s Disease
Abstract
:1. Introduction
2. Methods
2.1. Participants
2.2. Assessment Tools
2.3. Intervention
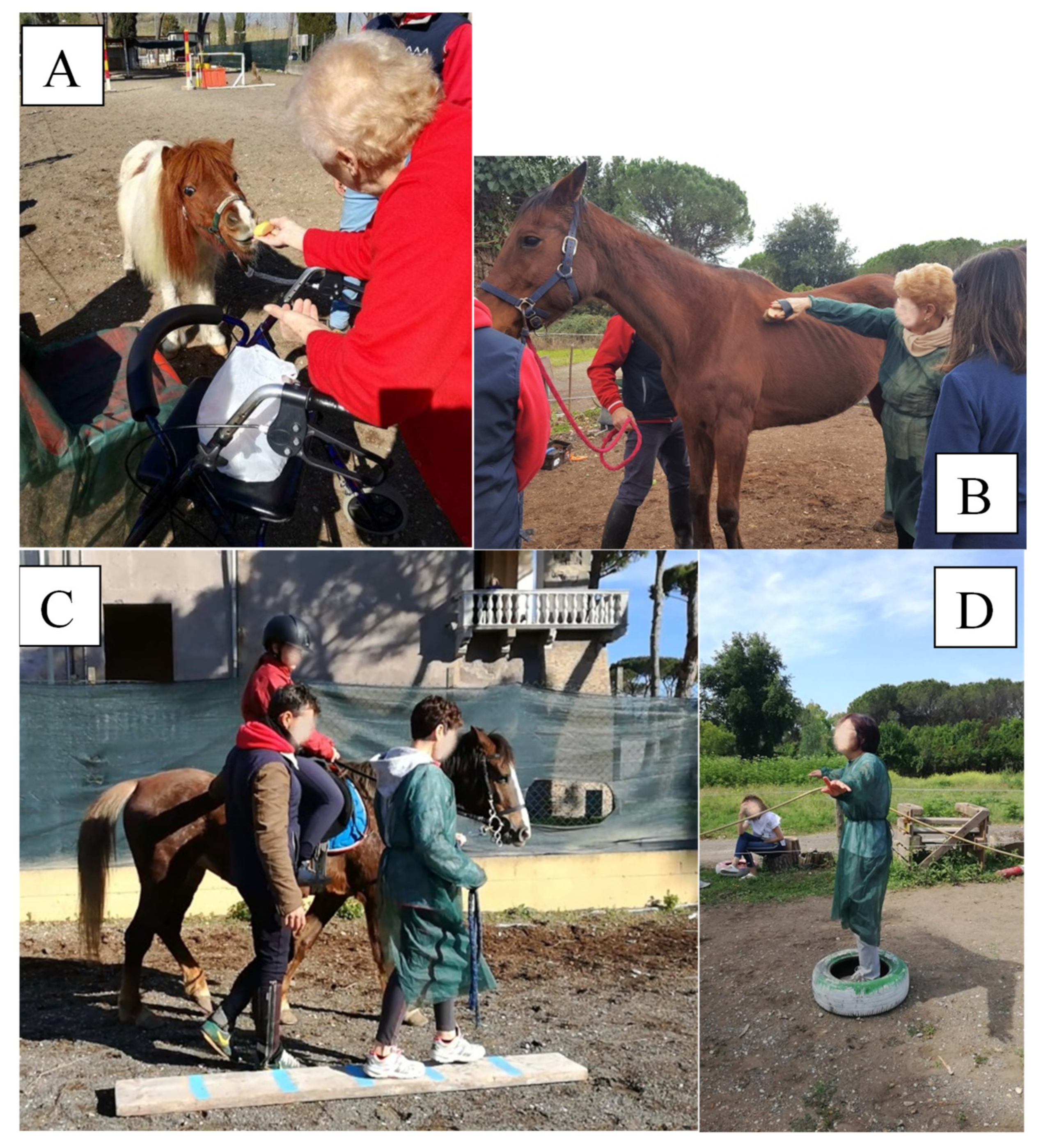
- A caring and cleaning activity that allowed the participant to develop motor skills and coordination, cognitive skills (attention, memory), proprioception, and social–relational skills (Figure 1A).
- A horse-assisted walking activity that could be carried out in different ways, including inside or outside the equestrian area, and on a path, with or without obstacles, on which the individual was asked to define times of pause and resumption of activity (Figure 1B).
- A feeding activity that allowed the participant to develop relational and behavioral skills, with the creation of an even greater understanding with the animal (Figure 1C).
- Vocalisation exercises to call the horse or provide commands during the activities, which contributed to increasing self-confidence.
- Breathing exercises, assisted by the horse, with the aim of relaxing and reassuring the participant (Figure 1D).
- Other activities, based on individual preferences
2.4. Data Analysis
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reich, S.G.; Savitt, J.M. Parkinson’s Disease. Med. Clin. N. Am. 2019, 103, 337–350. [Google Scholar] [CrossRef] [PubMed]
- Abbruzzese, G.; Marchese, R.; Avanzino, L.; Pelosin, E. Rehabilitation for Parkinson’s disease: Current outlook and future challenges. Parkinsonism Relat. Disord. 2016, 22 (Suppl. S1), S60–S64. [Google Scholar] [CrossRef] [PubMed]
- Dockx, K.; Bekkers, E.M.; Van den Bergh, V.; Ginis, P.; Rochester, L.; Hausdorff, J.M.; Mirelman, A.; Nieuwboerst, A. Virtual reality for rehabilitation in Parkinson’s disease. Cochrane Database Syst. Rev. 2016, 12, CD010760. [Google Scholar] [CrossRef] [PubMed]
- Cano Porras, D.; Siemonsma, P.; Inzelberg, R.; Zeilig, G.; Plotnik, M. Advantages of virtual reality in the rehabilitation of balance and gait: Systematic review. Neurology 2018, 90, 1017–1025. [Google Scholar] [CrossRef]
- Friedman, E.; Krause-Parello, C.A. Companion animals and human health: Benefits, challenges, and the road ahead for human–animal interaction. Rev. Sci. Tech. L’OIE 2018, 37, 71–82. [Google Scholar] [CrossRef]
- Carillon, B.; Jarzebowski, W.; Fulpin, B.; Miliotis, A.; Bernadac, A.; Saint-Georges Chaumet, Y.; Belmin, J. Effects of pony-assisted therapy on the behavior of older people with neurocognitive disorders living in nursing homes. Geriatr. Psychol. Neuropsychiatr. Vieil. 2020, 18, 273–282. [Google Scholar] [CrossRef]
- Fiori, G.; Marzi, T.; Bartoli, F.; Bruni, C.; Ciceroni, C.; Palomba, M.; Zolferino, M.; Corsi, E.; Galimberti, M.; Moggi Pignone, A.; et al. The challenge of pet therapy in systemic sclerosis: Evidence for an impact on pain, anxiety, neuroticism and social interaction. Clin. Exp. Rheumatol. 2018, 36 (Suppl. S113), 135–141. [Google Scholar]
- Srinivasan, S.M.; Cavagnino, D.T.; Bhat, A.N. Effects of Equine Therapy on Individuals with Autism Spectrum Disorder: A Systematic Review. Rev. J. Autism Dev. Disord. 2018, 5, 156–175. [Google Scholar] [CrossRef]
- Vermöhlen, V.; Schiller, P.; Schickendantz, S.; Drache, M.; Hussack, S.; Gerber-Grote, A.; Pöhlau, D. Hippotherapy for patients with multiple sclerosis: A multicenter randomized controlled trial (MS-HIPPO). Mult. Scler. J. 2018, 24, 1375–1382. [Google Scholar] [CrossRef] [Green Version]
- Park, E.S.; Rha, D.W.; Shin, J.S.; Kim, S.; Jung, S. Effects of hippotherapy on gross motor function and functional performance of children with cerebral palsy. Yonsei Med. J. 2014, 55, 1736–1742. [Google Scholar] [CrossRef] [Green Version]
- Moraes, A.; Silva, M.; Copetti, F.; Abreu, A.C.; David, A.C. Hippotherapy in the postural control and balance in individuals with cerebral palsy: Systematic review. Rev. Neurociências 2015, 23, 546–554. [Google Scholar] [CrossRef]
- Peppe, A.; Costa, A.; Cerino, S.; Caltagirone, C.; Alleva, E.; Borgi, M.; Cirulli, F. Targeting gait and life quality in persons with Parkinson’s disease: Potential benefits of Equine-Assisted Interventions. Parkinsonism Relat. Disord. 2018, 47, 94–95. [Google Scholar] [CrossRef] [PubMed]
- Galeoto, G.; Turriziani, S.; Berardi, A.; Sansoni, J.; Santilli, V.; Mascio, M.; Paoloni, M. Levels of Cognitive Functioning Assessment Scale: Italian cross-cultural adaptation and validation. Ann. Ig. 2020, 32, 16–26. [Google Scholar] [PubMed]
- Galeoto, G.; Scialpi, A.; Grassi, M.L.; Berardi, A.; Valente, D.; Tofani, M.; Paoloni, M. General Sleep Disturbance Scale: Translation, cultural adaptation, and psychometric properties of the Italian version. Cranio 2021, 39, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Ruotolo, I.; Berardi, A.; Sellitto, G.; Panuccio, F.; Polimeni, A.; Valente, D.; Galeoto, G. Criterion Validity and Reliability of SF-12 Health Survey Version 2 (SF-12v2) in a Student Population during COVID-19 Pandemic: A Cross-Sectional Study. Depress. Res. Treat. 2021, 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Regoli, E.; Tofani, M.; Valente, D.; Fabbrini, G.; Fabbrini, A.; Ruggieri, M.; Panuccio, F.; Galeoto, G. Tools to assess the quality of life in patients with Parkinson’s disease: A systematic review. Expert Rev. Pharmacoecon. Outcomes Res. 2021, 21, 55–68. [Google Scholar] [CrossRef]
- Miniera, F.; Berardi, A.; Panuccio, F.; Valente, D.; Tofani, M.; Galeoto, G. Measuring Environmental Barriers: Validation and Cultural Adaptation of the Italian Version of the Craig Hospital Inventory of Environmental Factors (CHIEF) Scale. Occup. Ther. Health Care 2020, 34, 373–385. [Google Scholar] [CrossRef]
- Ioncoli, M.; Berardi, A.; Tofani, M.; Panuccio, F.; Servadio, A.; Valente, D.; Galeoto, G. Crosscultural Validation of the Community Integration Questionnaire-Revised in an Italian Population. Occup. Ther. Int. 2020, 2020, 8916541. [Google Scholar] [CrossRef]
- Panuccio, F.; Berardi, A.; Marquez, M.A.; Messina, M.P.; Valente, D.; Tofani, M.; Galeoto, G. Development of the Pregnancy and Motherhood Evaluation Questionnaire (PMEQ) for evaluating and measuring the impact of physical disability on pregnancy and the management of motherhood: A pilot study. Disabil. Rehabil. 2020, 1–7. [Google Scholar] [CrossRef]
- Tofani, M.; Castelli, E.; Sabbadini, M.; Berardi, A.; Murgia, M.; Servadio, A.; Galeoto, G. Examining Reliability and Validity of the Jebsen-Taylor Hand Function Test Among Children with Cerebral Palsy. Percept. Mot. Ski. 2020, 127, 684–697. [Google Scholar] [CrossRef]
- Berardi, A.; Galeoto, G.; Lucibello, L.; Panuccio, F.; Valente, D.; Tofani, M. Athletes with disability’ satisfaction with sport wheelchairs: An Italian cross sectional study. Disabil. Rehabil. Assist. Technol. 2020, 16, 420–424. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, B.; Berardi, A.; Tofani, M.; Panuccio, F.; Ruotolo, I.; Sellitto, G.; Galeoto, G. A systematic review of the psychometric properties of the Jebsen–Taylor Hand Function Test (JTHFT). Hand Surg. Rehabil. 2021, 40, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Panuccio, F.; Pilli, L.; Tofani, M.; Valente, D.; Galeoto, G. Evaluation instruments for executive functions in children and adolescents: A systematic review. Expert Rev. Pharm. Outcomes Res. 2021, 21, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Galeoto, G.; De Santis, R.; Marcolini, A.; Cinelli, A.; Cecchi, R. II consenso informato in Terapia Occupazionale: Proposta di una modulistica. G. Ital. Med. Lav. Ergon. 2016, 38, 107–115. [Google Scholar]
- Galeoto, G.; Mollica, R.; Astorino, O.; Cecchi, R. II consenso informato in fisioterapia: Proposta di una modulistica. G. Ital. Med. Lav. Ergon. 2015, 37, 245–254. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatry Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Pangman, V.C.; Sloan, J.; Guse, L. An examination of psychometric properties of the Mini-Mental State Examination and the standardized Mini-Mental State Examination: Implications for clinical practice. Appl. Nurs. Res. 2000, 13, 209–213. [Google Scholar] [CrossRef]
- Galeoto, G.; Colalelli, F.; Massai, P.; Berardi, A.; Tofani, M.; Pierantozzi, M.; Servadio, A.; Fabbrini, A.; Fabbrini, G. Quality of life in Parkinson’s disease: Italian validation of the Parkinson’s Disease Questionnaire (PDQ-39-IT). Neurol. Sci. 2018, 39, 1903–1909. [Google Scholar] [CrossRef] [Green Version]
- Franchignoni, F.; Tesio, L.; Benevolo, E.; Ottonello, M. Psychometric properties of the rivermead mobility index in Italian stroke rehabilitation inpatients. Clin. Rehabil. 2003, 17, 273–282. [Google Scholar] [CrossRef]
- Innamorati, M.; Lelli, M.; Aiello, S.; Di lorenzo del Casale, F.L.; Russo, S.; Ferrari, V. Convergent and discriminant validation of the Italian version of the Zung Self-Rating Depression Scale. Psicoter. Cogn. E Comport. 2006, 12, 343–353. [Google Scholar]
- Ricci, G.; Barrionuevo, M.L.; Bodini, S.; Cosso, P.; Locati, L.; Pagliari, P.; Sala, S.; Ianes, A.B. Il Performance-Oriented Mobility Assessment (Scala di Tinetti) nell’assessment delle cadute: Analisi dell’importanza dei singoli item. G. Gerontol. 2013, 1, 126–135. [Google Scholar]
- Cova, I.; Di Battista, M.E.; Vanacore, N.; Papi, C.P.; Alampi, G.; Rubino, A.; Valente, M.; Meco, G.; Contri, P.; Di Pucchio, A.; et al. Validation of the Italian version of the Non Motor Symptoms Scale for Parkinson’s disease. Parkinsonism Relat. Disord. 2017, 34, 38–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peto, V.; Jenkinson, C.; Fitzpatrick, R.; Greenhall, R. The development and validation of a short measure of functioning and well being for individuals with Parkinson’s disease. Qual. Life Res. 1995, 4, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, N.B.; Edmans, J.A. A re-validation of the rivermead ADL scale for elderly patients with stroke. Age Ageing 1990, 19, 19–24. [Google Scholar] [CrossRef]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef] [Green Version]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef]
- Martínez-Martín, P.; Gil-Nagel, A.; Gracia, L.M.; Gómez, J.B.; Martínez-Sarriés, J.; Bermejo, F. Unified Parkinson’s disease rating scale characteristics and structure. Mov. Disord. 1994, 9, 76–83. [Google Scholar] [CrossRef]
- Antonini, A.; Abbruzzese, G.; Ferini-Strambi, L.; Tilley, B.; Huang, J.; Stebbins, G.T.; Goetz, C.G.; Barone, P.; di Poggio, M.B.; Fabbrini, G.; et al. Validation of the Italian version of the Movement Disorder Society—Unified Parkinson’s Disease Rating Scale. Neurol. Sci. 2013, 34, 683–687. [Google Scholar] [CrossRef]
- Scoppa, F.; Capra, R.; Gallamini, M.; Shiffer, R. Clinical stabilometry standardization. Basic definitions—Acquisition interval—Sampling frequency. Gait Posture 2013, 37, 290–292. [Google Scholar] [CrossRef]
- Ajzenman, H.F.; Standeven, J.W.; Shurtleff, T.L. Effect of hippotherapy on motor control, adaptive behaviors, and participation in children with autism spectrum disorder: A pilot study. Am. J. Occup. Ther. 2013, 67, 653–663. [Google Scholar] [CrossRef] [Green Version]
- Scorza, C.A.; Guimarães-Marques, M.; Nejm, M.; Victorino, D.B.; Fiorini, A.C.; Finsterer, J.; Scorza, F.A. Improving the quality of life of patients with Parkinson’s disease: Animal-assisted therapy in focus. Psychogeriatrics 2020, 20, 810. [Google Scholar] [CrossRef] [PubMed]
- Boldig, C.M.; Butala, N. Pet Therapy as a Nonpharmacological Treatment Option for Neurological Disorders: A Review of the Literature. Cureus 2021, 13, e16167. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Suarez-Jimenez, B.; Zilcha-Mano, S.; Lazarov, A.; Arnon, S.; Lowell, A.L.; Bergman, M.; Ryba, M.; Hamilton, A.J.; Hamilton, J.F.; et al. Neural changes following equine-assisted therapy for posttraumatic stress disorder: A longitudinal multimodal imaging study. Hum. Brain Mapp. 2021, 42, 1930–1939. [Google Scholar] [CrossRef] [PubMed]
- Ridgel, A.L.; Muller, M.D.; Kim, C.-H.; Fickes, E.J.; Mera, T.O. Acute Effects of Passive Leg Cycling on Upper Extremity Tremor and Bradykinesia in Parkinson’s Disease. Phys. Sportsmed. 2011, 39, 83–93. [Google Scholar] [CrossRef] [Green Version]
- Frazzitta, G.; Bertotti, G.; Riboldazzi, G.; Turla, M.; Uccellini, D.; Boveri, N.; Guaglio, G.; Perini, M.; Comi, C.; Balbi, P.; et al. Effectiveness of Intensive Inpatient Rehabilitation Treatment on Disease Progression in Parkinsonian Patients. Neurorehabil. Neural Repair 2012, 26, 144–150. [Google Scholar] [CrossRef]
| Sample 17 | |
|---|---|
| Gender male n° (%) | 6 (35.3%) |
| Age mean ± SD (range) | 67.94 ± 10.77 (52–78) |
| Years of diagnosis | 7.35 ± 3.06 |
| Height mean ± SD (range) | 168.13 ± 10.42 (154–188) |
| Body weight mean ± SD (range) | 67.63 ± 13.48 (45–90) |
| Body mass index mean ± SD (range) | 23.84 ± 2.66 (29.40–18.73) |
| Comorbidity n° (%) | |
| Cognitive decline | 1 (5.9%) |
| Pisa syndrome | 13 (76.5%) |
| Cognitive decline and Pisa syndrome | 2 (11.8%) |
| No comorbidity | 1 (5.9%) |
| MMSE mean ± SD | 29.88 ± 2.78 |
| Hoehn and Yahr n° (%) | |
| Stage 2 | 4 (23.5%) |
| Stage 3 | 13 (76.5%) |
| Rating Scale | T0 Median ± Standard Deviation | T1 Median ± Standard Deviation | Wilcoxon Signed-Rank Test | Statistical Significance | Effect Size | Power Analysis |
|---|---|---|---|---|---|---|
| SDS | 42.00 ± 7.45 | 34.00 ± 6.84 | −3.212 | p < 0.001 * | −0.55 | 0.86 |
| UPDRS | 16.00 ± 8.45 | 11.00 ± 7.43 | −3.189 | p < 0.001 * | −0.54 | 0.85 |
| RAS | 30.00 ± 6.12 | 38.00 ± 4.05 | −3.520 | p < 0.0004 * | −0.60 | 0.91 |
| Tinetti Total | 16.00 ± 4.70 | 20.00 ± 4.82 | −2.911 | p < 0.004 * | −0.49 | 0.72 |
| Tinetti Gait | 6.00 ± 2.52 | 8.00 ± 2.37 | −2.822 | p < 0.005 * | −0.48 | 0.75 |
| Tinetti Balance | 9.00 ± 2.91 | 12.00 ± 2.65 | −2.064 | p < 0.039 | −0.35 | 0.49 |
| PDQ−39 Total | 70.00 ± 29.09 | 52.00 ± 19.77 | −3.55 | p < 0.0003 * | −0.60 | 0.91 |
| Mobility Items | 21.00 ± 11.64 | 10.00 ± 7.24 | −3.578 | p < 0.0003 * | −0.61 | 0.92 |
| Daily Life Activities Items | 9.00 ± 6.89 | 6.00 ± 5.16 | −3.066 | p < 0.002 * | −0.52 | 0.81 |
| Emotional Well-being Items | 11.00 ± 5.48 | 8.00 ± 4.87 | −2.778 | p < 0.005 * | −0.47 | 0.74 |
| Stigma Items | 4.00 ± 3.78 | 3.00 ± 2.87 | −2.023 | p > 0.043 | −0.34 | 0.47 |
| Social Support Items | 8.00 ± 2.45 | 8.00 ± 2.48 | −1.633 | p > 0.102 | −0.28 | 0.34 |
| Cognitive Skills Items | 5.00 ± 3.06 | 4.00 ± 2.02 | −2.483 | p < 0.013 | −0.42 | 0.64 |
| Communication Items | 3.00 ± 2.89 | 2.00 ± 2.36 | −1.913 | p > 0.056 | −0.32 | 0.43 |
| Physical Discomforts Items | 5.00 ± 2.91 | 6.00 ± 3.43 | −1.44 | p > 0.150 | −0.24 | 0.26 |
| Values | Open Eyes | Closed Eyes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 Median ± Standard Deviation | T1 Median ± Standard Deviation | Wilcoxon Signed-Rank Test | Statistical Significance | Effect Size | Power Analysis | T0 Median ± Standard Deviation | T1 Median ± Standard Deviation | Wilcoxon Signed-Rank Test | Statistical Significance | Effect Size | Power Analysis | |
| Number of readings taken | 3000 ± 0.00 | 3000 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 | 3000 ± 0.00 | 3000± 0.00 | 0 | p = 1.00 | 0 | 0.05 |
| Middle coronal center (DX-SX) (unit) | −70 ± 9.85 | −4.00 ± 12.83 | −0.059 | p < 0.95 | −0.01 | 0.05 | 5.00 ± 7.887 | 2.00 ± 7.64 | −0.598 | p < 0.55 | −0.10 | 0.08 |
| Middle sagittal center (PST-ANT) (unit) | −11.60 ± 17.44 | −6.80 ± 21.89 | −1.958 | p < 0.50 | −0.33 | 0.44 | −3 ± 18.656 | −5.50 ± 12.15 | −0.889 | p < 0.374 | −0.15 | 0.13 |
| Curved length (unit) | 560 ± 83.71 | 600 ± 173.59 | −2.073 | p < 0.038 | −0.35 | 0.49 | 586 ± 226.18 | 626 ± 155.14 | −1.125 | p < 0.260 | −0.19 | 0.18 |
| 90% confidence ellipse area (unit) | 32.00 ± 68.07 | 35 ± 63.31 | −0.593 | p < 0.553 | −0.10 | 0.08 | 42 ± 72.729 | 50 ± 114.55 | −1.007 | p < 0.314 | −0.17 | 0.15 |
| Average speed (unit/ms) | 0.00 ± 0.00 | 0.00 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 |
| Sampling frequency (Hz) | 100 ± 0.00 | 100 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 | 100± 0.00 | 100 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 |
| Fundamental harmonic frequency (DX-SX) (Hz) | 0.00 ± 0.00 | 0.00 ± 0.00 | 0 | p = 1.00 | 0 | 0.05 | 0.00 ± 0.00 | 0.00 ± 0.33 | −1 | p < 0.317 | −0.17 | 0.15 |
| Fundamental harmonic frequency (PST-ANT) (Hz) | 0.00 ± 0.33 | 0.00 ± 0.00 | −1 | p < 0.317 | −0.17 | 0.15 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0 | p < 1.00 | 0 | 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berardi, A.; Di Napoli, G.; Ernesto, M.; Fabbrini, G.; Conte, A.; Ferrazzano, G.; Viselli, F.; Galeoto, G. The Effectiveness of Equine Therapy Intervention on Activities of Daily Living, Quality of Life, Mood, Balance and Gait in Individuals with Parkinson’s Disease. Healthcare 2022, 10, 561. https://doi.org/10.3390/healthcare10030561
Berardi A, Di Napoli G, Ernesto M, Fabbrini G, Conte A, Ferrazzano G, Viselli F, Galeoto G. The Effectiveness of Equine Therapy Intervention on Activities of Daily Living, Quality of Life, Mood, Balance and Gait in Individuals with Parkinson’s Disease. Healthcare. 2022; 10(3):561. https://doi.org/10.3390/healthcare10030561
Chicago/Turabian StyleBerardi, Anna, Giorgia Di Napoli, Monica Ernesto, Giovanni Fabbrini, Antonella Conte, Gina Ferrazzano, Fabio Viselli, and Giovanni Galeoto. 2022. "The Effectiveness of Equine Therapy Intervention on Activities of Daily Living, Quality of Life, Mood, Balance and Gait in Individuals with Parkinson’s Disease" Healthcare 10, no. 3: 561. https://doi.org/10.3390/healthcare10030561
APA StyleBerardi, A., Di Napoli, G., Ernesto, M., Fabbrini, G., Conte, A., Ferrazzano, G., Viselli, F., & Galeoto, G. (2022). The Effectiveness of Equine Therapy Intervention on Activities of Daily Living, Quality of Life, Mood, Balance and Gait in Individuals with Parkinson’s Disease. Healthcare, 10(3), 561. https://doi.org/10.3390/healthcare10030561








