Factors Associated with Vaginal/Cesarean Birth Attitudes among Medical Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Research Group
2.2. Research Tools
Introductory Section
3. Results
3.1. Demographic Characteristics of the Sampled Students
3.2. Overall Knowledge of Polish Perinatal Care and Opinions Concerning Vaginal Birth (VB) and Cesarean Birth (CB)
3.3. Student Opinions Regarding VB and CS
3.4. Students’ Opinions about Pain Levels after VB and CS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Betrán, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gülmezoglu, A.M.; et al. Interventions to reduce unnecessary cesarean sections in healthy women and babies. Lancet 2018, 392, 1358–1368. [Google Scholar] [CrossRef]
- Betran, A.P.; Ye, J.; Moller, A.B.; Souza, J.P.; Zhang, J. Trends and projections of cesarean section rates: Global and regional estimates. BMJ Glob. Health 2021, 6, e005671. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, Ö.; Vogel, J.P.; et al. What is the optimal rate of cesarean section at population level? A systematic review of ecologic studies. Reprod. Health 2015, 12, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betran, A.P.; Torloni, M.R.; Zhang, J.J.; Gülmezoglu, A.M. WHO statement on cesarean section rates. BJOG Int. J. Obstet. Gynaecol. 2016, 123, 667–670. [Google Scholar] [CrossRef]
- Pallasmaa, N.; Ekblad, U.; Aitokallio-Tallberg, A.; Uotila, J.; Raudaskoski, T.; Ulander, V.M.; Hurme, S. Cesarean delivery in Finland: Maternal complications and obstetric risk factors. Acta Obs. Gynecol. Scand. 2010, 89, 896–902. [Google Scholar] [CrossRef]
- Coates, D.; Thirukumar, P.; Henry, A. Women’s experiences and satisfaction with having a cesarean birth: An integrative review. Birth 2020, 47, 169–182. [Google Scholar] [CrossRef]
- Opiyo, N.; Kingdon, C.; Oladapo, O.T.; Souza, J.P.; Vogel, J.P.; Bonet, M.; Bucagu, M.; Portela, A.; McConville, F.; Downe, S.; et al. Non-clinical interventions to reduce unnecessary cesarean sections: WHO recommendations. Bull. World Health Organ. 2020, 98, 66–68. [Google Scholar] [CrossRef]
- Demographical Atlas of Poland [Internet]. Warsaw: Central Statistical Office of Poland [Internet]. 2021. Available online: https://stat.gov.pl/download/gfx/portalinformacyjny/pl/defaultaktualnosci/5501/28/1/1/atlas_demograficzny_polski.pdf (accessed on 19 February 2022).
- Wielgos, M.; Bomba-Opon, D.; Breborowicz, G.H.; Czajkowski, K.; Debski, R.; Leszczynska-Gorzelak, B.; Oszykowski, P.; Radowicki, S.; Zimmer, M. Recommendations of the Polish Society of Gynecologists and Obstetricians regarding cesarean sections. Ginekol. Pol. 2018, 89, 644–657. [Google Scholar] [CrossRef]
- Zeitlin, J.; Alexander, S.; Barros, H.; Blondel, B.; Delnord, M.; Durox, M.; Gissler, M.; Hindori-Mohangoo, A.D.; Hocquette, A.; Szamotulska, K.; et al. Report, European Perinatal Health 2015, Core Indicators of the Health and Care of Pregnant Women and Babies in Europe in. Available online: www.europeristat.com (accessed on 12 December 2021).
- Macfarlane, A.J.; Blondel, B.; Mohangoo, A.D.; Cuttini, M.; Nijhuis, J.; Novak, Z.; Ólafsdóttir, H.S.; Zeitlin, J.; The Euro-Peristat Scientific Committee. Wide differences in mode of delivery within Europe: Risk-stratified analyses of aggregated routine data from the Euro-Peristat study. BJOG Int. J. Obs. Gynaecol. 2016, 123, 559–568. [Google Scholar] [CrossRef]
- Adamska-Sala, I.; Baranowska, B.; Doroszewska, A.; Piekarek, M.P.J. Polish Perinatal Care Monitoring Report. Perinatal Care in Poland in Womens’ Experience; Childbirth with Dignity Foundation: Warsaw, Poland, 2018. [Google Scholar]
- Kopeć-Godlewska, K.; Pac, A.; Różańska, A.; Wójkowska-Mach, J. Is vaginal birth without an episiotomy a rarity in the 21st century? Cross-sectional studies in southern Poland. Int. J. Environ. Res. Public Health 2018, 15, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Baranowska, B.; Doroszewska, A.; Kubicka-Kraszyńska, U.; Pietrusiewicz, J.; Adamska-Sala, I.; Kajdy, A.; Sys, D.; Tataj-Puzyna, U.; Bączek, G.; Crowther, S. Is there respectful maternity care in Poland? Women’s views about care during labor and birth. BMC Pregnancy Childbirth 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCulloch, P.; Nagendran, M.; Campbell, W.B.; Price, A.; Jani, A.; Birkmeyer, J.D.; Gray, M. Strategies to reduce variation in the use of surgery. Lancet 2013, 382, 1130–1139. [Google Scholar] [CrossRef]
- Dominiek, C.; Natasha, D.; Foureur, M.; Spear, V.; Amanda, H. Exploring unwarranted clinical variation: The attitudes of midwives and obstetric medical staff regarding induction of labour and planned cesarean section. Women Birth 2021, 34, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Potter, J.E.; Hopkins, K.; Faúndes, A.; Perpétuo, I. Women’s autonomy and scheduled cesarean sections in Brazil: A cautionary tale. Birth 2008, 35, 33–40. [Google Scholar] [CrossRef]
- Panda, S.; Begley, C.; Daly, D. Clinicians’ views of factors influencing decision-making for cesarean section: A systematic review and metasynthesis of qualitative, quantitative and mixed methods studies. PLoS ONE 2018, 13, e0200941. [Google Scholar]
- Leppert, W.; Majkowicz, M. Ból przewlekły. Ujęcie kliniczne i psychologiczne. In Chronic Pain. Clinical and Psychological Approach; PZWL: Warsaw, Poland, 2018. [Google Scholar]
- Jones, L.E.; Whitburn, L.Y.; Davey, M.A.; Small, R. Assessment of pain associated with childbirth: Women’s perspectives, preferences and solutions. Midwifery 2015, 31, 708–712. [Google Scholar] [CrossRef]
- Boerma, T.; Ronsmans, C.; Melesse, D.Y.; Barros, A.J.D.; Barros, F.C.; Juan, L.; Moller, A.-B.; Say, L.; Hosseinpoor, A.R.; Yi, M.; et al. Global epidemiology of use of and disparities in cesarean sections. Lancet 2018, 392, 1341–1348. [Google Scholar] [CrossRef]
- White VanGompel, E.; Perez, S.; Wang, C.; Datta, A.; Cape, V.; Main, E. Measuring labor and delivery unit culture and clinicians’ attitudes toward birth: Revision and validation of the Labor Culture Survey. Birth 2019, 46, 300–310. [Google Scholar] [CrossRef]
- Mulchandani, R.; Power, H.S.; Cavallaro, F.L. The influence of individual provider characteristics and attitudes on cesarean section decision-making: A global review. J. Obstet. Gynaecol. 2020, 40, 1–9. [Google Scholar] [CrossRef]
- Litorp, H.; Mgaya, A.; Kidanto, H.L.; Johnsdotter, S.; Essén, B. ‘What about the mother?’ Women׳s and caregivers׳ perspectives on cesarean birth in a low-resource setting with rising cesarean section rates. Midwifery 2015, 31, 713–720. [Google Scholar] [CrossRef]
- Varnakioti, D.; Gourounti, K.; Sarantaki, A. Students’ Attitudes Towards Birth Decisions. Mædica 2021, 16, 107. [Google Scholar]
- Heidari, Z.; Kohan, S. The comparison of knowledge and attitude of midwifery and nursing students towards natural childbirth and cesarean section. J. Midwifery Reprod. Health 2015, 3, 437–443. [Google Scholar]
- Watanabe, T.; Knobel, R.; Suchard, G.; Franco, M.J.; D’Orsi, E.; Consonni, E.B.; Consonni, M. Medical students’ personal choice for mode of delivery in Santa Catarina, Brazil: A cross-sectional, quantitative study. BMC Med. Educ. 2012, 12, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Knobel, R.; Takemoto, M.L.S.; Andreucci, C.B.; Docusse, P.; McKinley, D.W.; Amaral, E. Factors Associated with Preference for Vaginal Birth among Undergraduate Students from Southern Brazil. Birth 2016, 43, 263–267. [Google Scholar] [CrossRef]
- Lampman, C.; Phelps, A. College Students’ Knowledge and Attitudes About Cesarean Birth. Birth 1997, 24, 159–164. [Google Scholar] [CrossRef]
- Kringeland, T.; Daltveit, A.K.; Møller, A. What characterizes women in Norway who wish to have a cesarean section? Scand. J. Public Health 2009, 37, 364–371. [Google Scholar] [CrossRef]
- Michalik, A.; Wojcicka, L.; Czerwińska-Osipiak, A.; Zdun-Ryżewska, A.; Jakitowicz, K.; Olszewska, J.; Krauze, M.; Jakitowicz, M. Preferences of women with low obstetric risk for cesarean or vaginal birth in Poland: Areas for intervention. Birth 2021, 48, 265–273. [Google Scholar] [CrossRef] [PubMed]
- Stoll, K.; Fairbrother, N.; Carty, E.; Jordan, N.; Miceli, C.; Vostrcil, Y.; Willihnganz, L. “It’s all the rage these days”: University students’ attitudes toward vaginal and cesarean birth. Birth 2009, 36, 133–140. [Google Scholar] [CrossRef]
- Stoll, K.; Hall, W.; Janssen, P.; Carty, E. Why are young Canadians afraid of birth? A survey study of childbirth fear and birth preferences among Canadian University students. Midwifery 2014, 30, 220–226. [Google Scholar] [CrossRef]
- Marshall, J.L.; Spiby, H.; McCormick, F. Evaluating the ‘Focus on Normal Birth and Reducing Cesarean section Rates Rapid Improvement Programme’: A mixed method study in England. Midwifery 2015, 31, 332–340. [Google Scholar] [CrossRef] [Green Version]
- Thompson, S.M.; Nieuwenhuijze, M.J.; Low, L.K.; de Vries, R. Exploring Dutch midwives’ attitudes to promoting physiological childbirth: A qualitative study. Midwifery 2016, 42, 67–73. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | N | % |
|---|---|---|
| Age, mean ± SD (standard deviation) 22.22 ± 2.61 | 748 | |
| Place of residence | ||
| Rural | 176 | 23.5 |
| Urban | 572 | 76.4 |
| Sex | ||
| Female | 646 | 86.4 |
| Male | 102 | 13.6 |
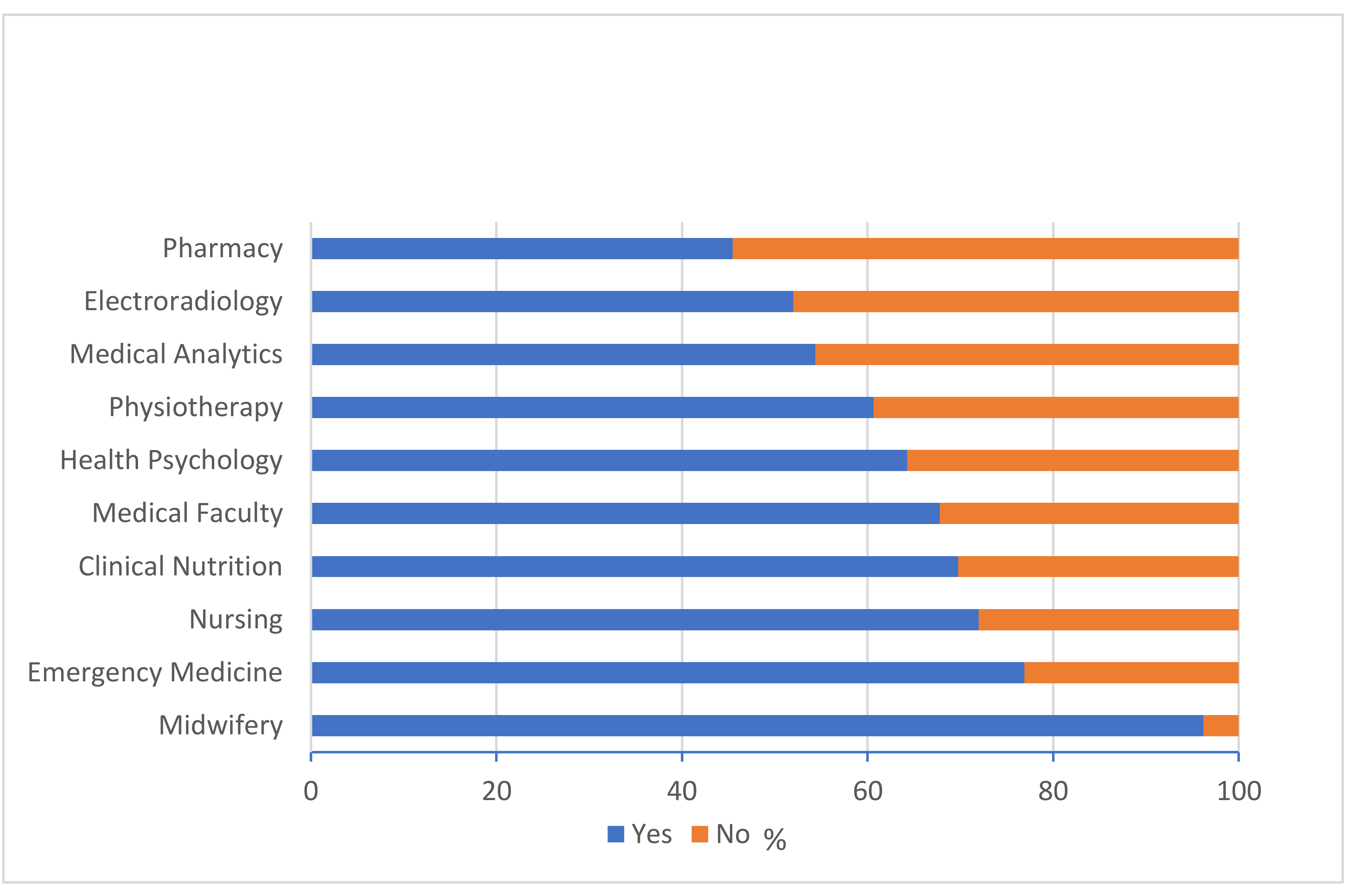
| Field of study | ||
| Midwifery | 131 | 17.5 |
| Nursing | 82 | 11 |
| Medical Faculty | 236 | 31.6 |
| Clinical Nutrition | 43 | 5.7 |
| Physiotherapy | 61 | 8.2 |
| Pharmacy | 88 | 1.8 |
| Emergency Medicine | 13 | 1.7 |
| Medical Analytics | 46 | 6.1 |
| Health Psychology | 14 | 1.9 |
| Electroradiology | 25 | 3.3 |
| Public Health | 5 | 0.7 |
| Dentistry | 4 | 0.5 |
| Year of study | ||
| I | 213 | 28.5 |
| II | 183 | 24.5 |
| III | 141 | 18.9 |
| IV | 78 | 10.4 |
| V | 96 | 12.8 |
| VI | 37 | 4.9 |
| The future professional practice include the care of pregnant and birthing women | ||
| Yes | 488 | 65.2 |
| No | 260 | 34.8 |
| Your biological capacity of having children (in your knowledge and opinion) | ||
| Yes | 734 | 98.1 |
| No | 14 | 1.9 |
| Statements | N | % |
|---|---|---|
| Most births in Poland are | ||
| VB | 617 | 82.5 |
| CB | 131 | 17.5 |
| The current proportion of VB in Poland is | ||
| 0–20% | 4 | 0.5 |
| 21–40% | 114 | 15.2 |
| 41–60% | 414 | 55.3 |
| More than 60% | 216 | 28.9 |
| The current proportion of CB in Poland is | ||
| 0–20% | 62 | 8.3 |
| 21–40% | 460 | 61.5 |
| 41–60% | 188 | 25.1 |
| More than 60% | 38 | 5.1 |
| The Polish CB rate follows WHO recommendations | ||
| Yes | 85 | 11.4 |
| No | 350 | 46.8 |
| I don’t know | 313 | 41.8 |
| Type of birth recommended for pregnant women from groups at low risk for vaginal birth (VB)-related complications | ||
| VB | 716 | 95.7 |
| CB | 32 | 4.3 |
| VB is safer and more beneficial for the mother and baby compared with CB | ||
| Yes | 515 | 68.9 |
| No | 233 | 31.1 |
| Every woman should have the right to opt for CB in any situation, independent of existing medical indications | ||
| Yes | 625 | 83.6 |
| No | 123 | 16.4 |
| The lack of trust in one’s own body and lack of acceptance of one’s femininity influence the decision to choose childbirth delivery options | ||
| Yes | 628 | 84 |
| No | 120 | 16 |
| The rate of your own knowledge of pregnancy and childbirth | ||
| Very good | 89 | 11.9 |
| Good | 220 | 29.4 |
| Sufficient | 214 | 28.6 |
| Small | 219 | 29.3 |
| Lack of any knowledge | 6 | 0.8 |
| VAS Score for Birth Pain Intensity | N | Min | Max | M | SD |
|---|---|---|---|---|---|
| VAS score for VB pain level | 748 | 4 | 10 | 9.03 | 1.04 |
| VAS score for CS pain level | 748 | 0 | 10 | 4.11 | 2.65 |
| VAS score for pain level 24 h after VB | 748 | 0 | 10 | 5.41 | 2.19 |
| VAS score for pain level 24 h after CS | 748 | 0 | 10 | 5.76 | 2.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michalik, A.; Czerwińska-Osipiak, A.; Szablewska, A.; Pracowity, M.; Olszewska, J. Factors Associated with Vaginal/Cesarean Birth Attitudes among Medical Students. Healthcare 2022, 10, 571. https://doi.org/10.3390/healthcare10030571
Michalik A, Czerwińska-Osipiak A, Szablewska A, Pracowity M, Olszewska J. Factors Associated with Vaginal/Cesarean Birth Attitudes among Medical Students. Healthcare. 2022; 10(3):571. https://doi.org/10.3390/healthcare10030571
Chicago/Turabian StyleMichalik, Anna, Agnieszka Czerwińska-Osipiak, Anna Szablewska, Michalina Pracowity, and Jolanta Olszewska. 2022. "Factors Associated with Vaginal/Cesarean Birth Attitudes among Medical Students" Healthcare 10, no. 3: 571. https://doi.org/10.3390/healthcare10030571






