The Effect of Competency-Based Triage Education Application on Emergency Nurses’ Triage Competency and Performance
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
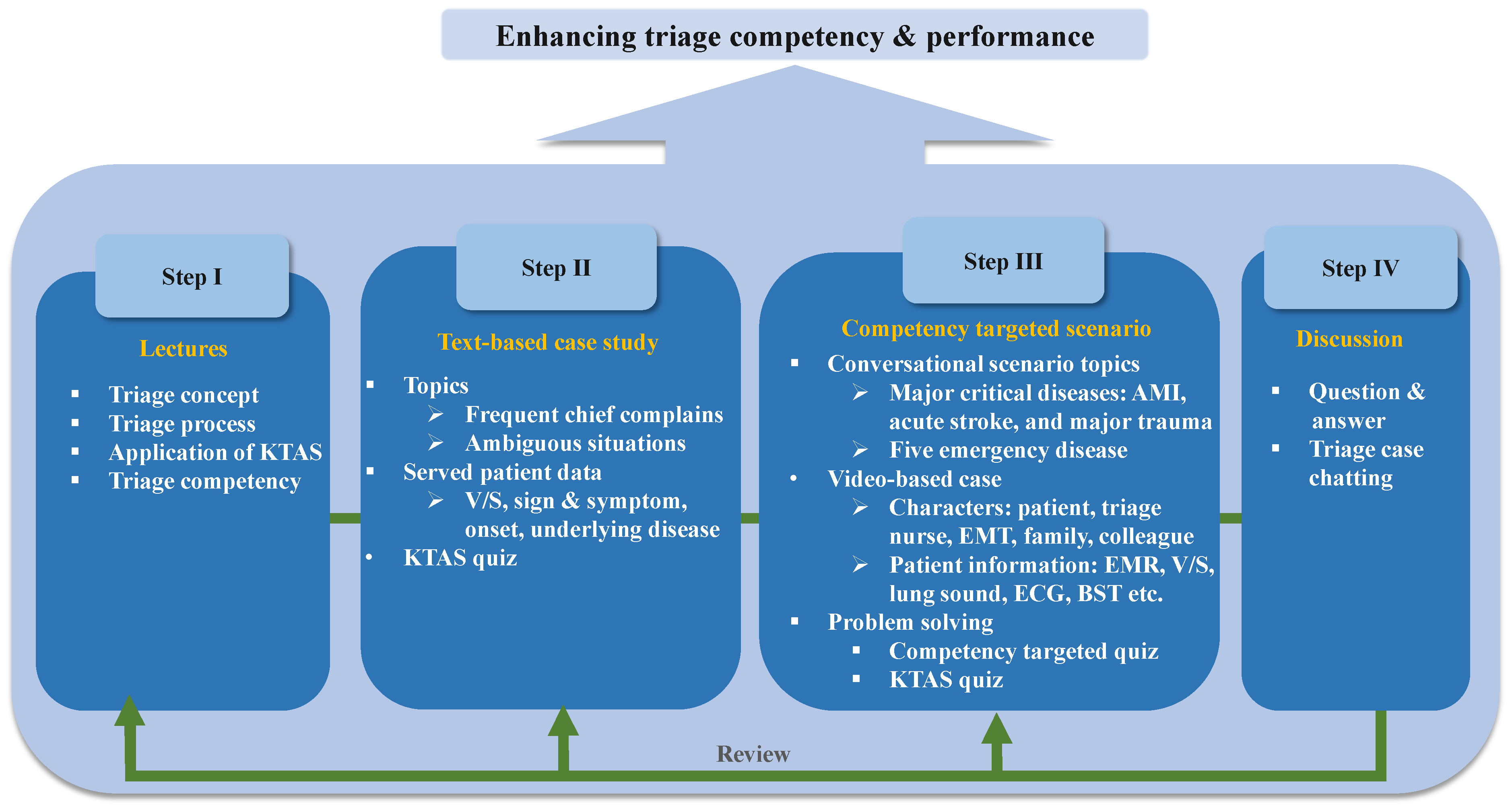
2.2. The CTEA Development
2.3. Outcome Measurements
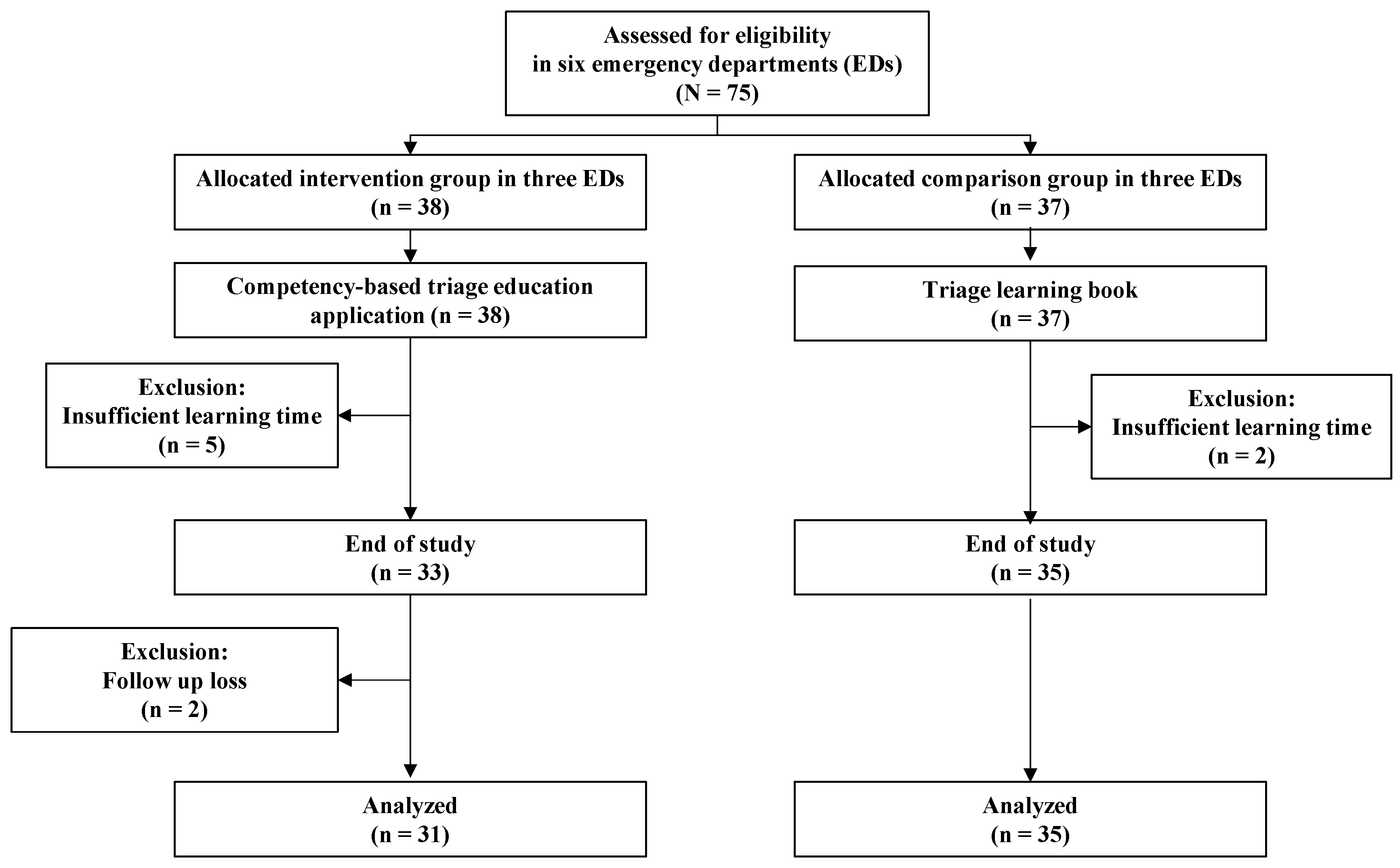
2.4. Participants and Data Collection
2.5. Data Analysis
2.6. Ethical Approval
3. Results
3.1. Baseline Characteristics
3.2. Comparison of Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moon, S.H.; Park, Y.H. Concept analysis of triage competency in emergency nursing. J. Korean Crit. Care Nurs. 2017, 10, 41–52. [Google Scholar]
- Fry, M.; Burr, G. Review of the triage literature: Past, present, future? Aust. Emerg. Nurs. J. 2002, 5, 33–38. [Google Scholar] [CrossRef]
- Moon, S.-H.; Jeon, M.-K.; Ju, D. Facilitators and Barriers of the Triage Process based on Emergency Nurses’ Experience with the Korean Triage and Acuity Scale: A Qualitative Content Analysis. Asian Nurs. Res. 2021, 15, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Christ, M.; Grossmann, F.; Winter, D.; Bingisser, R.; Platz, E. Modern triage in the emergency department. Dtsch. Ärzteblatt Int. 2010, 107, 892. [Google Scholar] [CrossRef]
- Park, J.; Lim, T. Korean triage and acuity scale (KTAS). J. Korean Soc. Emerg. Med. 2017, 28, 547–551. [Google Scholar]
- Recznik, C.T.; Simko, L.M. Pediatric triage education: An integrative literature review. J. Emerg. Nurs. 2018, 44, 605–613.e609. [Google Scholar] [CrossRef]
- Hardy, A.; Calleja, P. Triage education in rural remote settings: A scoping review. Int. Emerg. Nurs. 2019, 43, 119–125. [Google Scholar] [CrossRef] [Green Version]
- Ricciardi, F.; De Paolis, L.T. A comprehensive review of serious games in health professions. Int. J. Comput. Games Technol. 2014, 2014, 9. [Google Scholar] [CrossRef]
- Austin, E.E.; Blakely, B.; Tufanaru, C.; Selwood, A.; Braithwaite, J.; Clay-Williams, R. Strategies to measure and improve emergency department performance: A scoping review. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 55. [Google Scholar] [CrossRef]
- Foronda, C.L.; Shubeck, K.; Swoboda, S.M.; Hudson, K.W.; Budhathoki, C.; Sullivan, N.; Hu, X. Impact of virtual simulation to teach concepts of disaster triage. Clin. Simul. Nurs. 2016, 12, 137–144. [Google Scholar] [CrossRef]
- Anderson, M.; Guido-Sanz, F.; Díaz, D.A.; Lok, B.; Stuart, J.; Akinnola, I.; Welch, G. Augmented Reality in Nurse Practitioner Education: Using a Triage Scenario to Pilot Technology Usability and Effectiveness. Clin. Simul. Nurs. 2021, 54, 105–112. [Google Scholar] [CrossRef]
- Korean Triage and Acuity Scale Committee. KTAS Training Course. Available online: http://www.ktas.org/education/info.php (accessed on 5 June 2021).
- Kim, J.H.; Park, H. Effects of smartphone-based mobile learning in nursing education: A systematic review and meta-analysis. Asian Nurs. Res. 2019, 13, 20–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koohestani, H.R.; Arabshahi, S.K.S.; Fata, L.; Ahmadi, F. The educational effects of mobile learning on students of medical sciences: A systematic review in experimental studies. J. Adv. Med. Educ. Prof. 2018, 6, 58. [Google Scholar]
- Visser, L.S.; Montejano, A.S. An Orientation and Care Guide. In Fast Facts for the Triage Nurse, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Visser, L.S.; Montejano, A.S. Rapid Access Guide for Triage and Emergency Nurses: Chief Complaints with High Risk Presentations; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Manchester Triage Group. Emergency Triage; Wiley: Hoboken, NJ, USA, 2008. [Google Scholar]
- Korean Triage and Acuity Scale Committee. KTAS Provider Manual 2nd; Koonja: Paju, Korea, 2021. [Google Scholar]
- Tintinalli, J.E.; Stapczynski, J.S.; Ma, O.J.; Cline, D.M.; Meckler, G.D. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th ed.; McGraw-Hill Education: New York, NY, USA, 2016. [Google Scholar]
- Kwon, I.S.; Lee, G.E.; Kim, G.D.; Kim, Y.H.; Park, K.M.; Park, H.S.; Sohn, S.K.; Lee, W.S.; Jang, K.S.; Chung, B.Y. Development of a critical thinking disposition scale for nursing students. J. Korean Acad. Nurs. 2006, 36, 950–958. [Google Scholar] [CrossRef]
- Moon, S.H.; Park, Y.H. Development of a triage competency scale for emergency nurses. J. Korean Acad. Nurs. 2018, 48, 362–374. [Google Scholar] [CrossRef]
- Cook, D.A.; Erwin, P.J.; Triola, M.M. Computerized virtual patients in health professions education: A systematic review and meta-analysis. Acad. Med. 2010, 85, 1589–1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, K.-S. A Study on Establishment of Clinical Career Development Model of Nurses. Ph.D. Thesis, Yonsei University, Seoul, Korea, 2000. Unpublished. [Google Scholar]
- McCoy, L.; Lewis, J.H.; Dalton, D. Gamification and multimedia for medical education: A landscape review. J. Osteopath. Med. 2016, 116, 22–34. [Google Scholar] [CrossRef] [Green Version]
- Montano, I.H.; de la Torre Díez, I.; López-Izquierdo, R.; Villamor, M.A.C.; Martín-Rodríguez, F. Mobile triage applications: A systematic review in literature and play store. J. Med. Syst. 2021, 45, 86. [Google Scholar] [CrossRef]
- Emergency Nurses Association. Triage Qualifications and Competency. J. Emerg. Nurs. 2017, 43, 571–574. [Google Scholar] [CrossRef]
- Aysha, Z.M.S.; Allam, Z.A. Efficacy of START Triage Algorithm Scenario-Based Education on Nursing Students’ Knowledge, Attitude, Competencies, and Clinical Judgment. IOSR J. Nurs. Health Sci. IOSR-JNHS 2020, 9, 39–56. [Google Scholar]
- Huh, S.S.; Kang, H.Y. Effects of an educational program on disaster nursing competency. Public Health Nurs. 2019, 36, 28–35. [Google Scholar] [CrossRef]
- Tam, H.L.; Chung, S.F.; Lou, C.K. A review of triage accuracy and future direction. BMC Emerg. Med. 2018, 18, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, K.; Jo, E.; Song, K.J. Effect of problem-based learning on severity classification agreement by triage nurses. BMC Nurs. 2021, 20, 256. [Google Scholar] [CrossRef] [PubMed]
- Moon, S.-H.; Shim, J.L.; Park, K.-S.; Park, C.-S. Triage accuracy and causes of mistriage using the Korean Triage and Acuity Scale. PLoS ONE 2019, 14, e0216972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.H.; Park, Y.S.; Park, I.C.; Lee, H.S.; Kim, J.H.; Park, J.M.; Chung, S.P.; Kim, M.J. Over-triage occurs when considering the patient’s pain in Korean Triage and Acuity Scale (KTAS). PLoS ONE 2019, 14, e0216519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grossmann, F.F.; Zumbrunn, T.; Frauchiger, A.; Delport, K.; Bingisser, R.; Nickel, C.H. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann. Emerg. Med. 2012, 60, 317–325.e313. [Google Scholar] [CrossRef]
- Kim, H.-J.; Kang, H.-Y. Effects of a Web-Based Korean Triage and Acuity Scale Learning Program on Triage Self-Efficacy and Triage Performance Ability for Nurses in Emergency Department. J. Korean Acad. Nurs. 2019, 49, 171–180. [Google Scholar] [CrossRef]
- Nah, F.F.-H.; Zeng, Q.; Telaprolu, V.R.; Ayyappa, A.P.; Eschenbrenner, B. Gamification of education: A review of literature. In Proceedings of the International Conference on HCI in Business, Crete, Greece, 22–24 June 2014; pp. 401–409. [Google Scholar]
- Deterding, S.; Khaled, R.; Nacke, L.E.; Dixon, D. Gamification: Toward a definition. In Proceedings of the CHI 2011 Gamification Workshop Proceedings, Vancouver, BC, Canada, 7 May 2011; pp. 12–15. [Google Scholar]
- Hamari, J.; Koivisto, J.; Sarsa, H. Does gamification work?—A literature review of empirical studies on gamification. In Proceedings of the 2014 47th Hawaii International Conference on System Sciences, Waikoloa, HI, USA, 6–9 January 2014; pp. 3025–3034. [Google Scholar]
- Mohan, D.; Angus, D.C.; Ricketts, D.; Farris, C.; Fischhoff, B.; Rosengart, M.R.; Yealy, D.M.; Barnato, A.E. Assessing the validity of using serious game technology to analyze physician decision making. PLoS ONE 2014, 9, e105445. [Google Scholar] [CrossRef] [Green Version]
- Zhao, J.; Zhou, K.; Ding, Y. Digital Games-Based Learning Pedagogy Enhances the Quality of Medical Education: A Systematic Review and Meta-Analysis. Asia-Pac. Educ. Res. 2021, 1–12. [Google Scholar] [CrossRef]
- Colliver, J.A.; Kucera, K.; Verhulst, S.J. Meta-analysis of quasi-experimental research: Are systematic narrative reviews indicated? Med. Educ. 2008, 42, 858–865. [Google Scholar] [CrossRef]


| Characteristics | Classification | IG (n = 31) n (%) or Mean ± SD | CG (n = 35) n (%) or Mean ± SD | Total (N = 66) n (%) or Mean ± SD | χ2 or t (p) |
|---|---|---|---|---|---|
| Age | Total (years) | 34.09 ± 8.19 | 30.42 ± 6.41 | 32.15 ± 7.47 | 2.00 (0.050) |
| 20~29 | 11 (16.7) | 20 (30.3) | 31 (47.0) | 4.66 (0.097) | |
| 30~39 | 12 (18.2) | 12 (18.2) | 24 (36.4) | ||
| ≥40 | 8 (12.1) | 3 (4.5) | 11 (16.7) | ||
| Gender | Female | 26 (39.4) | 30 (45.5) | 56 (84.8) | 0.04 (0.834) |
| Male | 5 (7.6) | 5 (7.6) | 10 (15.2) | ||
| Education level | Associate degree | 11 (16.7) | 5 (7.6) | 16 (24.2) | 4.93 (0.085) |
| Bachelor’s degree | 18 (27.3) | 29 (43.9) | 47 (71.2) | ||
| Over master’s degree | 2 (3.0) | 1 (1.5) | 3 (4.5) | ||
| Experience in nursing | Total (year) | 10.46 ± 8.19 | 7.42 ± 6.72 | 8.85 ± 7.54 | 1.65 (0.104) |
| Novice (<1) | 2 (3.0) | 2 (3.0) | 4 (6.1) | 2.53 (0.471) | |
| Advanced beginner (1≤~<3) | 4 (6.1) | 7 (10.6) | 11 (16.7) | ||
| Competent (3≤~<7) | 6 (9.1) | 11 (16.7) | 17 (25.8) | ||
| Proficient (≥7) | 19 (28.8) | 15 (22.7) | 34 (51.5) | ||
| Experience in the ED | Total (year) | 4.06 ± 3.12 | 4.02 ± 3.93 | 4.04 ± 3.54 | 0.05 (0.960) |
| Novice (<1) | 5 (7.6) | 5 (7.6) | 10 (15.2) | 0.13 (0.989) | |
| Advanced beginner (1≤~<3) | 9 (13.6) | 11 (16.7) | 20 (30.3) | ||
| Competent (3≤~<7) | 11 (16.7) | 13 (19.7) | 24 (36.4) | ||
| Proficient (≥7) | 6 (9.1) | 6 (9.1) | 12 (18.2) | ||
| Experience of triage (year) | 1.27 ± 1.77 | 1.23 ± 1.14 | 1.25 ± 1.46 | 0.10 (0.920) | |
| Variables | IG (n = 31) Mean ± SD | CG (n = 35) Mean ± SD | Total (N = 66) Mean ± SD | t (p) |
|---|---|---|---|---|
| Critical thinking disposition | 113.70 ± 9.62 | 112.34 ± 10.28 | 112.34 ± 10.28 | −0.55 (0.581) |
| Triage competency | 79.51 ± 16.68 | 82.88 ± 12.63 | 82.88 ± 12.63 | 0.93 (0.355) |
| Triage knowledge | 20.35 ± 3.15 | 22.22 ± 2.77 | 22.22 ± 2.77 | 2.56 (0.013 *) |
| Triage accuracy | 3.90 ± 1.86 | 4.02 ± 1.85 | 4.02 ± 1.85 | 0.27 (0.786) |
| Variables | Groups | Pre (a) Mean ± SD | Post (b) Mean ± SD | Difference (b − a) Mean ± SD | t (p) |
|---|---|---|---|---|---|
| Critical thinking disposition | IG | 113.70 ± 9.62 | 115.45 ± 10.31 | 1.74 ± 8.89 | −0.47 (0.633) |
| CG | 112.34 ± 10.28 | 115.14 ± 10.93 | 2.80 ± 8.98 | ||
| Triage competency | IG | 79.51 ± 16.68 | 86.25 ± 15.79 | 6.74 ± 14.42 | 2.55 (0.013 *) |
| CG | 82.88 ± 12.63 | 82.54 ± 12.65 | -0.34 ± 7.40 | ||
| Clinical judgment | IG | 34.12 ± 6.65 | 37.00 ± 6.37 | 2.87 ± 6.41 | 2.39 (0.021 *) |
| CG | 35.62 ± 5.33 | 35.45 ± 5.26 | −0.17 ± 3.13 | ||
| Expert assessment | IG | 10.00 ± 3.01 | 11.09 ± 2.59 | 1.09 ± 2.97 | 1.22 (0.225) |
| CG | 9.85 ± 2.46 | 10.20 ± 2.13 | 0.34 ± 1.79 | ||
| Management of medical resources | IG | 11.29 ± 2.84 | 11.87 ± 2.26 | 0.58 ± 2.87 | 1.99 (0.051) |
| CG | 12.22 ± 2.27 | 11.62 ± 2.34 | −0.60 ± 1.89 | ||
| Timely decisions | IG | 10.51 ± 2.95 | 11.41 ± 2.93 | 0.90 ± 1.90 | 2.89 (0.005 *) |
| CG | 10.71 ± 2.29 | 10.31 ± 2.45 | −0.40 ± 1.75 | ||
| Communication | IG | 13.58 ± 3.26 | 14.87 ± 3.09 | 1.29 ± 3.01 | 1.30 (0.197) |
| CG | 14.45 ± 2.44 | 14.94 ± 2.02 | 0.48 ± 1.72 | ||
| Triage knowledge | IG | 20.35 ± 3.15 | 22.41 ± 2.72 | 2.06 ± 2.95 | 3.11 (0.003 *) |
| CG | 22.22 ± 2.77 | 22.28 ± 2.39 | 0.05 ± 2.27 | ||
| Triage accuracy | IG | 3.90 ± 1.86 | 4.77 ± 1.68 | 0.87 ± 2.34 | 2.11 (0.039 *) |
| CG | 4.03 ± 1.85 | 3.80 ± 1.71 | −0.22 ± 1.88 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, S.-H.; Cho, I.-Y. The Effect of Competency-Based Triage Education Application on Emergency Nurses’ Triage Competency and Performance. Healthcare 2022, 10, 596. https://doi.org/10.3390/healthcare10040596
Moon S-H, Cho I-Y. The Effect of Competency-Based Triage Education Application on Emergency Nurses’ Triage Competency and Performance. Healthcare. 2022; 10(4):596. https://doi.org/10.3390/healthcare10040596
Chicago/Turabian StyleMoon, Sun-Hee, and In-Young Cho. 2022. "The Effect of Competency-Based Triage Education Application on Emergency Nurses’ Triage Competency and Performance" Healthcare 10, no. 4: 596. https://doi.org/10.3390/healthcare10040596
APA StyleMoon, S.-H., & Cho, I.-Y. (2022). The Effect of Competency-Based Triage Education Application on Emergency Nurses’ Triage Competency and Performance. Healthcare, 10(4), 596. https://doi.org/10.3390/healthcare10040596






