Future Scenarios of the Data-Driven Healthcare Economy in South Korea
Abstract
1. Introduction
2. Literature Review
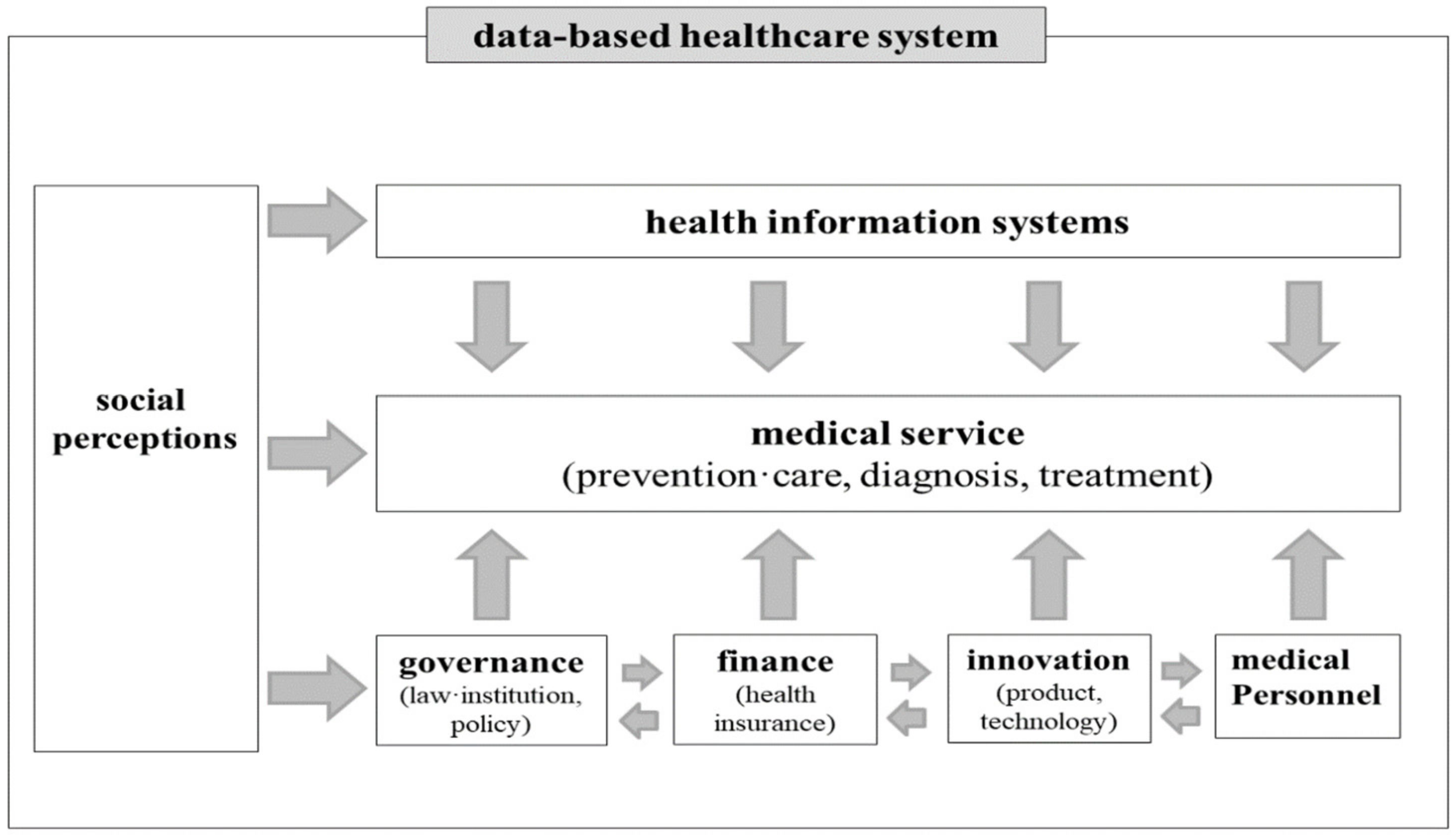
2.1. Digital Healthcare Research
2.2. Data-Driven Healthcare-Related Studies
3. Methods
3.1. Scenario Modelling through General Morphological Analysis (GMA)
3.2. Multi-Dimensional Scaling (MDS)
4. Results
4.1. Expert Evaluation and Results of GMA
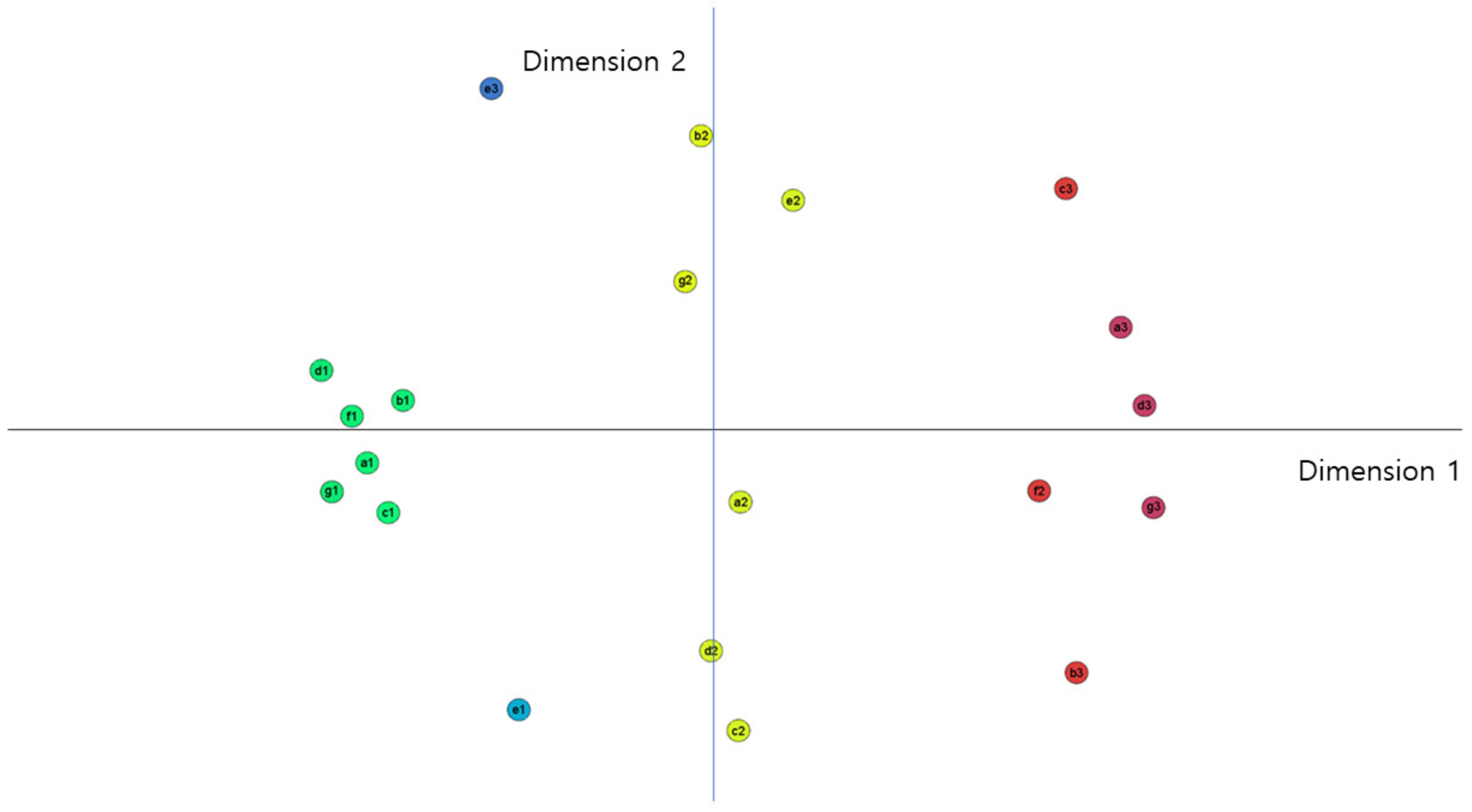
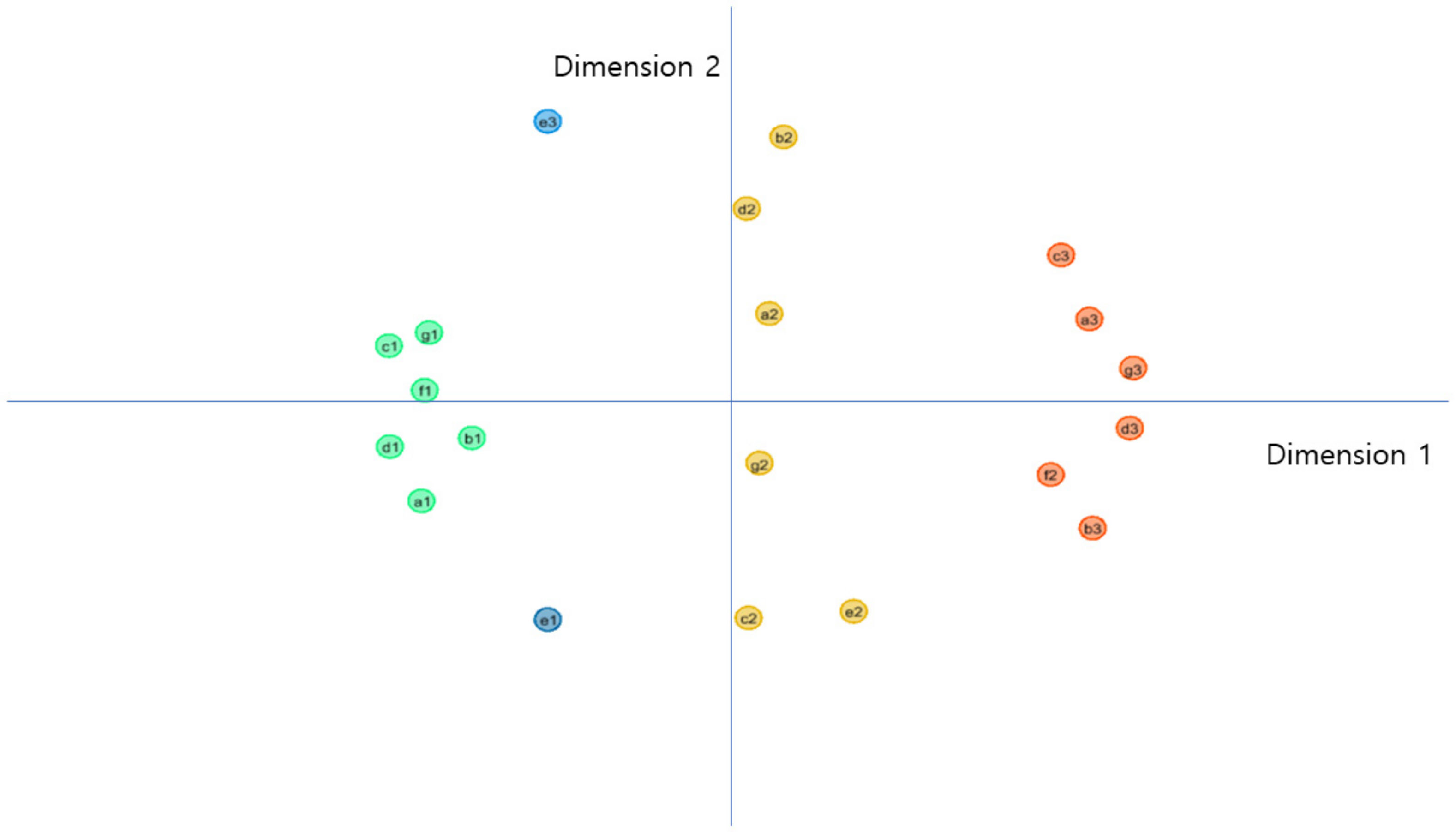
4.2. Results of MDS
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Distance between Spectra (Expert Evaluation Mean) | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion | Status Quo | Contraction | High | Status Quo | Low | Weakening | Status Quo | Reinforcement | Realization | Status Quo | Deactivation | Increase | Status Quo | Decrease | Realization | Stagnation | Expansion | Status Quo | Reduction | ||
| Acceptability of Data Utilization | Expansion | 0.000 | |||||||||||||||||||
| Status Quo | 0.712 | 0.000 | |||||||||||||||||||
| Contraction | 1.454 | 0.799 | 0.000 | ||||||||||||||||||
| Data Literacy | High | 0.141 | 0.671 | 1.369 | 0.000 | ||||||||||||||||
| Status Quo | 0.903 | 0.725 | 0.882 | 0.768 | 0.000 | ||||||||||||||||
| Low | 1.408 | 0.721 | 0.686 | 1.386 | 1.275 | 0.000 | |||||||||||||||
| Healthcare Data Regulation | Weakening | 0.106 | 0.669 | 1.437 | 0.224 | 0.950 | 1.343 | 0.000 | |||||||||||||
| Status Quo | 0.880 | 0.450 | 1.076 | 0.910 | 1.173 | 0.652 | 0.791 | 0.000 | |||||||||||||
| Reinforcement | 1.431 | 0.873 | 0.293 | 1.325 | 0.700 | 0.954 | 1.436 | 1.235 | 0.000 | ||||||||||||
| Healthcare Data System | Realization | 0.201 | 0.837 | 1.520 | 0.166 | 0.856 | 1.552 | 0.308 | 1.062 | 1.458 | 0.000 | ||||||||||
| Status Quo | 0.749 | 0.298 | 1.006 | 0.764 | 1.014 | 0.696 | 0.669 | 0.166 | 1.133 | 0.922 | 0.000 | ||||||||||
| Deactivation | 1.479 | 0.790 | 0.161 | 1.407 | 0.996 | 0.542 | 1.451 | 1.002 | 0.453 | 1.564 | 0.955 | 0.000 | |||||||||
| Medical Costs | Increase | 0.564 | 0.588 | 1.369 | 0.648 | 1.182 | 1.062 | 0.460 | 0.420 | 1.461 | 0.765 | 0.383 | 1.331 | 0.000 | |||||||
| Status Quo | 0.959 | 0.602 | 0.670 | 0.838 | 0.216 | 1.075 | 0.984 | 1.049 | 0.518 | 0.956 | 0.900 | 0.781 | 1.131 | 0.000 | |||||||
| Decrease | 0.774 | 0.942 | 1.284 | 0.636 | 0.408 | 1.599 | 0.858 | 1.349 | 1.108 | 0.643 | 1.183 | 1.389 | 1.225 | 0.613 | 0.000 | ||||||
| Convergence of ICT and Biotechnology | Realization | 0.096 | 0.756 | 1.469 | 0.102 | 0.861 | 1.465 | 0.203 | 0.960 | 1.426 | 0.107 | 0.822 | 1.504 | 0.659 | 0.938 | 0.697 | 0.000 | ||||
| Stagnation | 1.276 | 0.567 | 0.358 | 1.220 | 0.949 | 0.365 | 1.235 | 0.740 | 0.598 | 1.382 | 0.698 | 0.262 | 1.078 | 0.739 | 1.307 | 1.312 | 0.000 | ||||
| Utilization of Data in Medical Services | Expansion | 0.088 | 0.775 | 1.531 | 0.225 | 0.990 | 1.457 | 0.115 | 0.903 | 1.515 | 0.239 | 0.784 | 1.551 | 0.556 | 1.046 | 0.849 | 0.154 | 1.341 | 0.000 | ||
| Status Quo | 0.700 | 0.447 | 0.832 | 0.583 | 0.289 | 1.070 | 0.724 | 0.890 | 0.746 | 0.712 | 0.729 | 0.906 | 0.901 | 0.260 | 0.529 | 0.685 | 0.788 | 0.787 | 0.000 | ||
| Reduction | 1.494 | 0.783 | 0.361 | 1.439 | 1.129 | 0.356 | 1.452 | 0.902 | 0.650 | 1.602 | 0.886 | 0.202 | 1.269 | 0.913 | 1.503 | 1.531 | 0.219 | 1.559 | 0.994 | 0.000 | |
Appendix B
| Distance between Spectra (Expert Evaluation Mode) | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion | Status Quo | Contraction | High | Status Quo | Low | Weakening | Status Quo | Reinforcement | Realization | Status Quo | Deactivation | Increase | Status Quo | Decrease | Realization | Stagnation | Expansion | Status Quo | Reduction | ||
| Acceptability of Data Utilization | Expansion | 0.000 | |||||||||||||||||||
| Status Quo | 0.867 | 0.000 | |||||||||||||||||||
| Contraction | 1.484 | 0.678 | 0.000 | ||||||||||||||||||
| Data Literacy | High | 0.187 | 0.699 | 1.341 | 0.000 | ||||||||||||||||
| Status Quo | 1.171 | 0.430 | 0.785 | 0.985 | 0.000 | ||||||||||||||||
| Low | 1.426 | 0.861 | 0.508 | 1.335 | 1.155 | 0.000 | |||||||||||||||
| Healthcare Data Regulation | Weakening | 0.383 | 0.811 | 1.487 | 0.285 | 0.979 | 1.558 | 0.000 | |||||||||||||
| Status Quo | 0.749 | 0.740 | 1.024 | 0.732 | 1.170 | 0.762 | 1.009 | 0.000 | |||||||||||||
| Reinforcement | 1.482 | 0.635 | 0.166 | 1.326 | 0.655 | 0.667 | 1.443 | 1.103 | 0.000 | ||||||||||||
| Healthcare Data System | Realization | 0.148 | 0.867 | 1.515 | 0.175 | 1.123 | 1.504 | 0.244 | 0.867 | 1.497 | 0.000 | ||||||||||
| Status Quo | 0.990 | 0.259 | 0.774 | 0.806 | 0.191 | 1.068 | 0.829 | 0.994 | 0.676 | 0.952 | 0.000 | ||||||||||
| Deactivation | 1.513 | 0.814 | 0.279 | 1.396 | 1.020 | 0.256 | 1.585 | 0.931 | 0.445 | 1.571 | 0.972 | 0.000 | |||||||||
| Medical Costs | Increase | 0.394 | 0.879 | 1.361 | 0.470 | 1.275 | 1.177 | 0.746 | 0.425 | 1.403 | 0.538 | 1.084 | 1.320 | 0.000 | |||||||
| Status Quo | 0.955 | 0.744 | 0.868 | 0.913 | 1.162 | 0.546 | 1.178 | 0.224 | 0.970 | 1.062 | 1.004 | 0.736 | 0.649 | 0.000 | |||||||
| Decrease | 0.960 | 0.664 | 1.246 | 0.786 | 0.502 | 1.522 | 0.641 | 1.279 | 1.137 | 0.858 | 0.473 | 1.443 | 1.211 | 1.356 | 0.000 | ||||||
| Convergence of ICT and Biotechnology | Realization | 0.269 | 0.754 | 1.420 | 0.153 | 0.978 | 1.456 | 0.132 | 0.882 | 1.389 | 0.156 | 0.813 | 1.499 | 0.616 | 1.057 | 0.703 | 0.000 | ||||
| Stagnation | 1.336 | 0.713 | 0.387 | 1.231 | 0.997 | 0.158 | 1.438 | 0.729 | 0.534 | 1.403 | 0.912 | 0.203 | 1.123 | 0.534 | 1.370 | 1.343 | 0.000 | ||||
| Utilization of Data in Medical Services | Expansion | 0.409 | 0.724 | 1.401 | 0.272 | 0.890 | 1.487 | 0.091 | 0.969 | 1.354 | 0.289 | 0.739 | 1.505 | 0.742 | 1.127 | 0.572 | 0.140 | 1.363 | 0.000 | ||
| Status Quo | 0.722 | 0.364 | 0.783 | 0.613 | 0.794 | 0.725 | 0.836 | 0.376 | 0.815 | 0.785 | 0.618 | 0.791 | 0.588 | 0.412 | 0.944 | 0.731 | 0.619 | 0.769 | 0.000 | ||
| Reduction | 1.543 | 0.782 | 0.151 | 1.413 | 0.930 | 0.398 | 1.580 | 1.017 | 0.314 | 1.588 | 0.906 | 0.146 | 1.384 | 0.837 | 1.379 | 1.503 | 0.313 | 1.496 | 0.826 | 0.000 | |
References
- Yu, S.G. Ubiquitous Health. Mon. Ind. Health 2006, 217, 13–18. [Google Scholar]
- Duggal, R.; Brindle, I.; Bagenal, J. Digital healthcare: Regulating the revolution. BMJ Br. Med. J. 2018, 360, k6. [Google Scholar] [CrossRef] [PubMed]
- Haggerty, E. Healthcare and digital transformation. Netw. Secur. 2017, 8, 7–11. [Google Scholar] [CrossRef]
- Kim, K.B.; Han, K.H. A study of the digital healthcare industry in the fourth industrial revolution. J. Converg. Inf. Technol. 2020, 10, 7–15. [Google Scholar] [CrossRef]
- Jung, I.Y.; Kim, S.K.; Lee, D.E.; Lee, Y.H. Emerging Healthcare Innovations Driven by Data and Its Policy Implications. Policy Stud. 2016, 15, 25–31. [Google Scholar]
- Lee, J.S. Digital healthcare platforms and leading enterprise trends. KHIDI Brief 2014, 140, 1–12. [Google Scholar]
- Jung, I.Y.; Koo, W.M. Data Integration Plan for Healthcare Ecosystem Establishment. Trends Issues 2018, 12, 1–38. [Google Scholar]
- Hwang, Y.J.; Yeon, S.J.; Kim, S.W. A Morphological Analysis of u-Healthcare Services. Telecommun. Rev. 2008, 18, 305–314. [Google Scholar]
- Han, J.H.; Hyun, Y.G.; Chae, U.R.; Lee, G.H.; Lee, J.Y. A Study on the Healthcare Technology Trends through Patent Data Analysis. J. Digit. Converg. 2020, 18, 179–187. [Google Scholar]
- Park, J.T.; Cheon, S.M.; Go, S.J. Trends in IoT-based healthcare services and platforms. Inf. Commun. Mag. 2014, 31, 25–30. [Google Scholar]
- Park, H.J.; Kim, H.S. Case Studies and Development on Wearable Healthcare Design—Mainly with Diverse Types of User Perspectives. J. Digit. Des. 2014, 14, 135–144. [Google Scholar]
- Yi, E.S. The physical activity and smart health care of trend for the elderly. J. Digit. Converg. 2017, 15, 511–516. [Google Scholar]
- Noh, D.J. A Study on the Forecasting of Library Service with Scenarios. J. Korean Libr. Inf. Sci. Soc. 2004, 35, 361–375. [Google Scholar]
- Johansen, I. Scenario modelling with morphological analysis. Technol. Forecast. Soc. Chang. 2018, 126, 116–125. [Google Scholar] [CrossRef]
- Shim, W.H.; Park, J.W. Regulatory reform plans and strategies for the emerging digital healthcare industry. J. Regul. Stud. 2018, 27, 33–65. [Google Scholar]
- Sharma, A.; Harrington, R.A.; McClellan, M.B.; Turakhia, M.P.; Eapen, Z.J.; Steinhubl, S.; Mault, J.R.; Majmudar, M.D.; Roessig, L.; Chandross, K.J.; et al. Using digital health technology to better generate evidence and deliver evidence-based care. J. Am. Coll. Cardiol. 2018, 71, 2680–2690. [Google Scholar] [CrossRef]
- Kim, H.S.; Kwon, I.H.; Cha, W.C. Future and Development Direction of Digital Healthcare. Healthc. Inform. Res. 2021, 27, 95–101. [Google Scholar] [CrossRef]
- Lee, D.E.; Kim, S.K. Digital Healthcare Transformation Trends and Policy Implications. Trends Issues 2018, 48, 1–13. [Google Scholar]
- Kim, S.Y.; Kim, H.K. Study on the Reasonable Regulation and Use of Personal Information on Digital Healthcare Environment. IT Law Rev. 2016, 12, 217–263. [Google Scholar]
- Kim, Y.K. Revision data 3 law and Issues of insurance business: Focusing on the activation of digital healthcare services. Korea Insur. Law J. 2020, 14, 495–524. [Google Scholar] [CrossRef]
- Choi, K.H.; Yang, E.S. A Study on the Trend of Healthcare Device Technology by Biometric Signal. J. Korea Entertain. Ind. Assoc. 2020, 14, 165–176. [Google Scholar] [CrossRef]
- Jeong, Y.S. Data Storage and Security Model for Mobile Healthcare Service based on IoT. J. Digit. Converg. 2017, 15, 187–193. [Google Scholar] [CrossRef][Green Version]
- Jeong, Y.S.; Han, K.H. Design of data integration model between hospitals for healthcare information collection. J. Korea Converg. Soc. 2018, 9, 1–7. [Google Scholar]
- Asri, H.; Mousannif, H.; Al Moatassime, H.; Noel, T. Big data in healthcare: Challenges and opportunities. In Proceedings of the International Conference on Cloud Technologies and Applications (CloudTech), Marrakech, Morocco, 2–4 June 2015; pp. 1–7. [Google Scholar]
- Senthilkumar, S.A.; Rai, B.K.; Meshram, A.A.; Gunasekaran, A.; Chandrakumarmangalam, S. Big data in healthcare management: A review of literature. Am. J. Theor. Appl. Bus. 2018, 4, 57–69. [Google Scholar]
- Olaronke, I.; Oluwaseun, O. Big data in healthcare: Prospects, challenges and resolutions. In Proceedings of the Future Technologies Conference (FTC), San Francisco, CA, USA, 6–7 December 2016; pp. 1152–1157. [Google Scholar]
- Lim, J.W.; Jung, E.Y.; Jeong, B.H.; Park, D.K.; Whangbo, T. A Study for Sharing Patient Medical Information with Demographic Datasets. J. Inst. Electron. Inf. Eng. 2014, 51, 128–136. [Google Scholar] [CrossRef]
- Bae, Y.I.; Shin, H.R. Data 3 Act, Beginning of Data Economy. Issue Diagn. 2022, in press. [Google Scholar]
- Kim, E. The use of big data concerning health -focusing on the Personal Information Protection Act. Law Technol. 2020, 16, 26–42. [Google Scholar]
- Sin, S.Y. Healthcare Data Anonymization for Personal Information Protection. Commun. Korean Inst. Inf. Sci. Eng. 2017, 35, 17–21. [Google Scholar]
- Lee, Y.J.; Lee, B.M. Study for Protection of Medical Information in Mobile Health. Soc. Converg. Knowl. Trans. 2015, 3, 19–24. [Google Scholar]
- Cha, M.K. Future Scenarios of Scholarly Information Services in Academic Libraries. J. Korean Biblia Soc. Libr. Inf. Sci. 2004, 15, 137–153. [Google Scholar]
- Álvarez, A.; Ritchey, T. Applications of general morphological analysis: From Engineering Design to Policy Analysis. Acta Morphol. Gen. 2015, 4, 1–40. [Google Scholar]
- Coyle, R.G.; McGlone, G.R. Projection Scenarios for Southeast Asia and the Southwest Pacific. Futures 1995, 27, 65–79. [Google Scholar] [CrossRef]
- Coyle, R.G.; Yong, Y.C. A Scenario Projection for the South China Sea. Futures 1996, 28, 269–283. [Google Scholar] [CrossRef]
- Ritchey, T. Modeling alternative futures with general morphological analysis. World Future Rev. 2011, 3, 83–94. [Google Scholar] [CrossRef]
- Duczynski, G. Morphological analysis as an aid to organisational design and transformation. Futures 2017, 86, 36–43. [Google Scholar] [CrossRef]
- Plauché, M.; de Waal, A.; Grover, A.S.; Gumede, T. Morphological Analysis: A Method for Selecting ICT Applications in South African Government Service Delivery. Inf. Technol. Int. Dev. 2010, 6, 1–20. [Google Scholar]
- Zheng, W.; Kankaanranta, J.; Suominen, A. Morphological analysis of technologies using multidimensional scaling. J. Bus. Chem. 2012, 9, 147–160. [Google Scholar]
- World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Koltay, T. Data Literacy: In search of a Name and Identity. J. Doc. 2015, 71, 401–415. [Google Scholar] [CrossRef]
- Prado, J.C.; Marzal, M.Á. Incorporating Data Literacy into Information Literacy Programs: Core Competencies and Contents. Libri 2013, 63, 123–134. [Google Scholar]
- Grossglauser, M.; Saner, H. Data-driven healthcare: From patterns to actions. Eur. J. Prev. Cardiol. 2014, 21 (Suppl. 2), 14–17. [Google Scholar] [CrossRef]
- Haggart, B. The government’s role in constructing the data-driven economy. In Data Governance in the Digital Age; Centre for International Governance Innovation: Waterloo, ON, Canada, 2018. [Google Scholar]
| Key Factors | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services |
|---|---|---|---|---|---|---|---|
| Spectrum | Expansion | High | Weakening | Realization | Increase | Realization | Expansion |
| Status Quo | Status Quo | Status Quo | Status Quo | Status Quo | Status Quo | ||
| Contraction | Low | Reinforcement | Deactivation | Decrease | Stagnation | Reduction |
| Expert Evaluation (Mean) | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion | Status Quo | Contraction | High | Status Quo | Low | Weakening | Status Quo | Reinforcement | Realization | Status Quo | Deactivation | Increase | Status Quo | Decrease | Realization | Stagnation | Expansion | Status Quo | Reduction | ||
| Acceptability of Data Utilization | Expansion | ||||||||||||||||||||
| Status Quo | |||||||||||||||||||||
| Contraction | |||||||||||||||||||||
| Data Literacy | High | 2.0 | 1.1 | 0.7 | |||||||||||||||||
| Status Quo | 1.3 | 1.1 | 0.8 | ||||||||||||||||||
| Low | 0.5 | 0.6 | 1.5 | ||||||||||||||||||
| Healthcare Data Regulation | Weakening | 2.0 | 1.1 | 0.6 | 1.7 | 0.9 | 0.6 | ||||||||||||||
| Status Quo | 1.2 | 1.1 | 0.9 | 0.9 | 1.2 | 0.7 | |||||||||||||||
| Reinforcement | 0.2 | 0.7 | 1.7 | 1.1 | 0.7 | 0.9 | |||||||||||||||
| Healthcare Data System | Realization | 2.0 | 0.9 | 0.2 | 2.0 | 1.0 | 0.2 | 1.8 | 1.1 | 0.5 | |||||||||||
| Status Quo | 1.0 | 1.5 | 0.6 | 0.9 | 1.5 | 0.7 | 1.1 | 1.5 | 0.5 | ||||||||||||
| Deactivation | 0.2 | 0.8 | 1.9 | 0.2 | 0.8 | 1.9 | 0.5 | 0.8 | 1.6 | ||||||||||||
| Medical Costs | Increase | 1.5 | 0.9 | 0.5 | 1.2 | 1.0 | 0.9 | 1.4 | 0.9 | 0.7 | 1.4 | 1.0 | 0.5 | ||||||||
| Status Quo | 1.2 | 1.1 | 0.6 | 1.0 | 1.2 | 0.5 | 0.9 | 1.1 | 0.7 | 1.0 | 1.1 | 0.6 | |||||||||
| Decrease | 1.2 | 1.0 | 0.6 | 0.9 | 1.0 | 0.5 | 0.8 | 0.9 | 0.5 | 1.0 | 0.9 | 0.5 | |||||||||
| Convergence of ICT and Biotechnology | Realization | 1.8 | 0.8 | 0.5 | 2.0 | 1.0 | 0.2 | 1.9 | 1.1 | 0.4 | 2.0 | 0.9 | 0.2 | 1.5 | 1.0 | 1.0 | |||||
| Stagnation | 0.5 | 1.0 | 1.4 | 0.5 | 0.9 | 1.5 | 0.5 | 1.0 | 1.4 | 0.2 | 0.9 | 1.7 | 0.9 | 1.2 | 0.5 | ||||||
| Utilization of Data in Medical Services | Expansion | 2.0 | 1.0 | 0.3 | 2.0 | 0.9 | 0.5 | 2.0 | 1.0 | 0.3 | 2.0 | 0.9 | 0.1 | 1.5 | 1.0 | 1.4 | 2.0 | 0.3 | |||
| Status Quo | 1.1 | 1.3 | 0.5 | 1.1 | 1.2 | 0.6 | 1.1 | 1.1 | 0.8 | 1.0 | 1.3 | 1.0 | 1.0 | 1.2 | 1.0 | 0.9 | 0.9 | ||||
| Reduction | 0.1 | 0.8 | 1.7 | 0.4 | 0.9 | 1.5 | 0.2 | 0.7 | 1.4 | 0.0 | 0.7 | 1.6 | 0.9 | 0.7 | 0.7 | 0.1 | 1.6 | ||||
| Expert Evaluation (Mode) | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expansion | Status Quo | Contraction | High | Status Quo | Low | Weakening | Status Quo | Reinforcement | Realization | Status Quo | Deactivation | Increase | Status Quo | Decrease | Realization | Stagnation | Expansion | Status Quo | Reduction | ||
| Acceptability of Data Utilization | Expansion | ||||||||||||||||||||
| Status Quo | |||||||||||||||||||||
| Contraction | |||||||||||||||||||||
| Data Literacy | High | 2 | 1 | 0 | |||||||||||||||||
| Status Quo | 1 | 1 | 1 | ||||||||||||||||||
| Low | 0 | 1 | 2 | ||||||||||||||||||
| Healthcare Data Regulation | Weakening | 2 | 1 | 0 | 2 | 1 | 0 | ||||||||||||||
| Status Quo | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||||||||
| Reinforcement | 0 | 1 | 2 | 1 | 1 | 1 | |||||||||||||||
| Healthcare Data System | Realization | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | |||||||||||
| Status Quo | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||||||||||
| Deactivation | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | ||||||||||||
| Medical Costs | Increase | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | ||||||||
| Status Quo | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |||||||||
| Decrease | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | |||||||||
| Convergence of ICT and Biotechnology | Realization | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 1 | 1 | 1 | |||||
| Stagnation | 0 | 1 | 1 | 1 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 0 | ||||||
| Utilization of Data in Medical Services | Expansion | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 0 | 2 | 1 | 2 | 2 | 0 | |||
| Status Quo | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||||
| Reduction | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 2 | 0 | 1 | 0 | 0 | 2 | ||||
| Coordinates of Spectra (Expert Evaluation Mean) | Dimension | |||
|---|---|---|---|---|
| 1 | 2 | |||
| Acceptability of Data Utilization | Expansion | a1 | −0.645 | −0.070 |
| Status Quo | a2 | 0.063 | −0.147 | |
| Contraction | a3 | 0.785 | 0.197 | |
| Data Literacy | High | b1 | −0.577 | 0.053 |
| Status Quo | b2 | −0.012 | 0.574 | |
| Low | b3 | 0.701 | −0.483 | |
| Healthcare Data Regulation | Weakening | c1 | −0.605 | −0.168 |
| Status Quo | c2 | 0.059 | −0.597 | |
| Reinforcement | c3 | 0.681 | 0.470 | |
| Healthcare Data System | Realization | d1 | −0.732 | 0.112 |
| Status Quo | d2 | 0.007 | −0.440 | |
| Deactivation | d3 | 0.830 | 0.043 | |
| Medical Costs | Increase | e1 | −0.358 | −0.556 |
| Status Quo | e2 | 0.163 | 0.447 | |
| Decrease | e3 | −0.410 | 0.667 | |
| Convergence of ICT and Biotechnology | Realization | f1 | −0.674 | 0.022 |
| Stagnation | f2 | 0.630 | −0.125 | |
| Utilization of Data in Medical Services | Expansion | g1 | −0.712 | −0.127 |
| Status Quo | g2 | −0.042 | 0.287 | |
| Reduction | g3 | 0.847 | −0.158 | |
| Key Factors | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services |
|---|---|---|---|---|---|---|---|
| Spectrum | expansion | high | Weakening | Realization | increase | Realization | expansion |
| Status Quo | Status Quo | Status Quo | Status Quo | Status Quo | stagnation | Status Quo | |
| Contraction | low | reinforcement | Deactivation | decrease | reduction |
 —Scenario 1: Optimistic Scenario;
—Scenario 1: Optimistic Scenario;  —Scenario 2: Desirable Scenario;
—Scenario 2: Desirable Scenario;  —Scenario 3: Pessimistic Scenario;
—Scenario 3: Pessimistic Scenario;  —Scenario 4: Monotonous Scenario.
—Scenario 4: Monotonous Scenario.| Coordinates of Spectra (Expert Evaluation Mode) | Dimension | |||
|---|---|---|---|---|
| 1 | 2 | |||
| Acceptability of Data Utilization | Expansion | a1 | −0.680 | −0.255 |
| Status Quo | a2 | 0.058 | 0.200 | |
| Contraction | a3 | 0.737 | 0.187 | |
| Data Literacy | High | b1 | −0.573 | −0.102 |
| Status Quo | b2 | 0.088 | 0.629 | |
| Low | b3 | 0.744 | −0.321 | |
| Healthcare Data Regulation | Weakening | c1 | −0.749 | 0.122 |
| Status Quo | c2 | 0.014 | −0.539 | |
| Reinforcement | c3 | 0.677 | 0.342 | |
| Healthcare Data System | Realization | d1 | −0.747 | 0.123 |
| Status Quo | d2 | 0.010 | 0.455 | |
| Deactivation | d3 | 0.823 | −0.078 | |
| Medical Costs | Increase | e1 | −0.412 | −0.543 |
| Status Quo | e2 | 0.237 | −0.523 | |
| Decrease | e3 | −0.412 | 0.667 | |
| Convergence of ICT and Biotechnology | Realization | f1 | −0.673 | 0.014 |
| Stagnation | f2 | 0.655 | −0.191 | |
| Utilization of Data in Medical Services | Expansion | g1 | −0.664 | 0.154 |
| Status Quo | g2 | 0.037 | −0.163 | |
| Reduction | g3 | 0.830 | 0.068 | |
| Key Factors | Acceptability of Data Utilization | Data Literacy | Healthcare Data Regulation | Healthcare Data System | Medical Costs | Convergence of ICT and Biotechnology | Utilization of Data in Medical Services |
|---|---|---|---|---|---|---|---|
| Spectrum | expansion | High | Weakening | Realization | increase | Realization | expansion |
| Status Quo | Status Quo | Status Quo | Status Quo | Status Quo | stagnation | Status Quo | |
| Contraction | low | reinforcement | Deactivation | decrease | reduction |
 —Scenario 1: Optimistic Scenario;
—Scenario 1: Optimistic Scenario;  —Scenario 2: Desirable Scenario;
—Scenario 2: Desirable Scenario;  —Scenario 3: Pessimistic Scenario;
—Scenario 3: Pessimistic Scenario;  —Scenario 4: Monotonous Scenario.
—Scenario 4: Monotonous Scenario.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-Y.; Lee, H.-J.; Lee, M.-J. Future Scenarios of the Data-Driven Healthcare Economy in South Korea. Healthcare 2022, 10, 772. https://doi.org/10.3390/healthcare10050772
Choi J-Y, Lee H-J, Lee M-J. Future Scenarios of the Data-Driven Healthcare Economy in South Korea. Healthcare. 2022; 10(5):772. https://doi.org/10.3390/healthcare10050772
Chicago/Turabian StyleChoi, Ji-Young, Hee-Jo Lee, and Myoung-Jin Lee. 2022. "Future Scenarios of the Data-Driven Healthcare Economy in South Korea" Healthcare 10, no. 5: 772. https://doi.org/10.3390/healthcare10050772
APA StyleChoi, J.-Y., Lee, H.-J., & Lee, M.-J. (2022). Future Scenarios of the Data-Driven Healthcare Economy in South Korea. Healthcare, 10(5), 772. https://doi.org/10.3390/healthcare10050772






