SOFA Score Plus Impedance Ratio Predicts Mortality in Critically Ill Patients Admitted to the Emergency Department: Retrospective Observational Study
Abstract
:1. Introduction
2. Methods
2.1. Data Collection and Management
2.2. Sample Size Calculation
2.3. Statistical Analyses
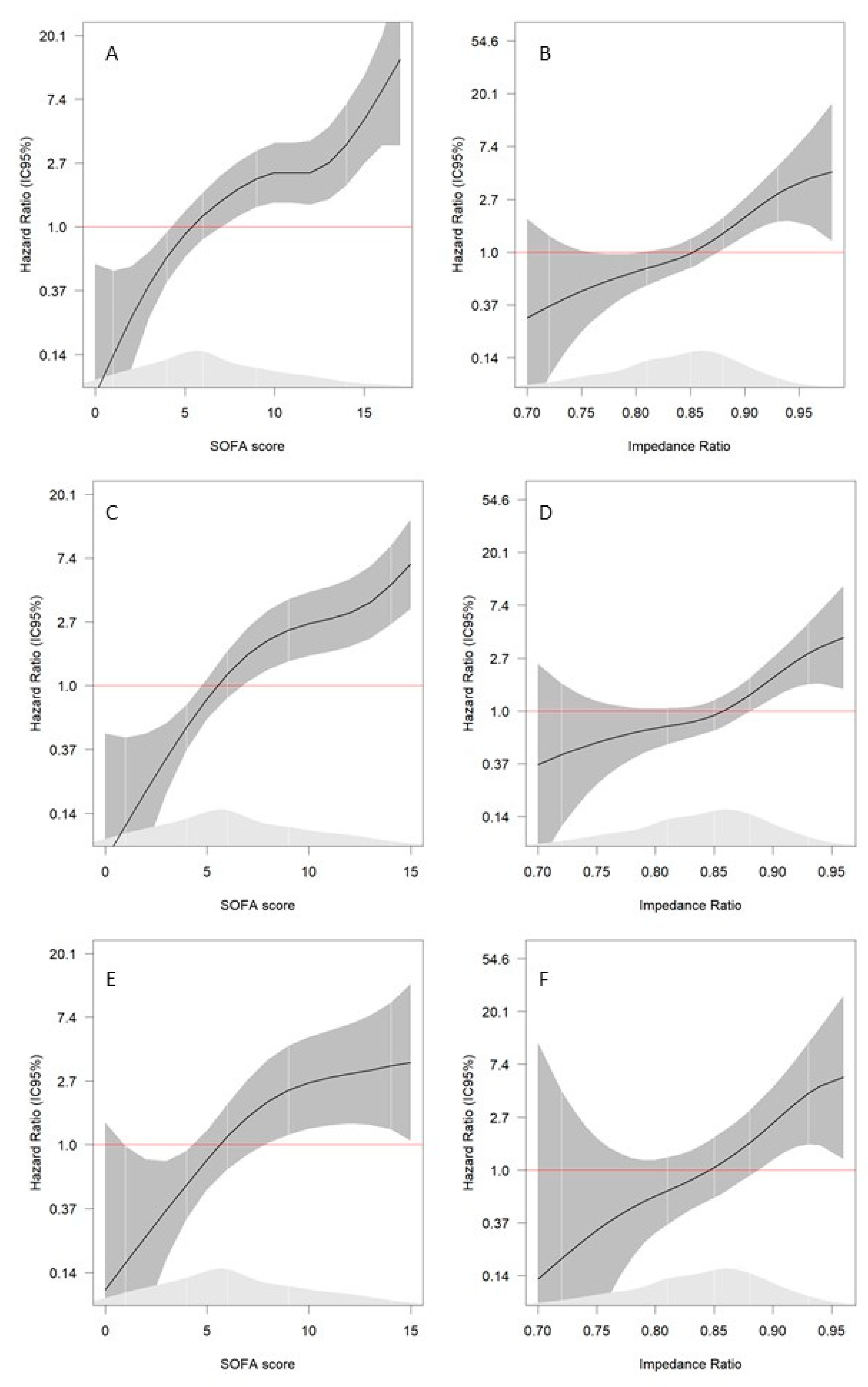
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Safari, S.; Shojaee, M.; Rahmati, F.; Barartloo, A.; Hahshemi, B.; Forouzanfar, M.M.; Mohammadi, E. Accuracy of SOFA score in prediction of 30-day outcome of critically ill patients. Turk. J. Emerg. Med. 2016, 16, 146–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chawda, M.; Hildebrand, F.; Pape, H.; Giannoudis, P. Predicting outcome after multiple trauma: Which scoring system? Injury 2004, 35, 347–358. [Google Scholar] [CrossRef]
- Garbero, R.D.F.; Simões, A.A.; Martins, G.A.; Cruz, L.; Von Zuben, V.G.M. SOFA and qSOFA at admission to the emergency department: Diagnostic sensitivity and relation with prognosis in patients with suspected infection. Turk. J. Emerg. Med. 2019, 19, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Rahmatinejad, Z.; Reihani, H.; Tohidinezhad, F.; Rahmatinejad, F.; Peyravi, S.; Pourmand, A.; Abu-Hanna, A.; Eslami, S. Predictive performance of the SOFA and mSOFA scoring systems for predicting in-hospital mortality in the emergency department. Am. J. Emerg. Med. 2018, 37, 1237–1241. [Google Scholar] [CrossRef]
- Minne, L.; Abu-Hanna, A.; De Jonge, E. Evaluation of SOFA-based models for predicting mortality in the ICU: A systematic review. Crit. Care 2009, 12, R161. [Google Scholar] [CrossRef] [Green Version]
- De Grooth, H.-J.; Geenen, I.L.; Girbes, A.R.; Vincent, J.-L.; Parienti, J.-J.; Straaten, H.M.O.-V. SOFA and mortality endpoints in randomized controlled trials: A systematic review and meta-regression analysis. Crit. Care 2017, 21, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granholm, A.; Møller, M.H.; Krag, M.; Perner, A.; Hjortrup, P.B. Predictive Performance of the Simplified Acute Physiology Score (SAPS) II and the Initial Sequential Organ Failure Assessment (SOFA) Score in Acutely Ill Intensive Care Patients: Post-Hoc Analyses of the SUP-ICU Inception Cohort Study. PLoS ONE 2016, 11, e0168948. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steele, L.; Hill, S. Using sepsis scores in emergency department and ward patients. Br. J. Hosp. Med. 2019, 80, C120–C123. [Google Scholar] [CrossRef]
- Haas, S.A.; Lange, T.; Saugel, B.; Petzoldt, M.; Fuhrmann, V.; Metschke, M.; Kluge, S. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensiv. Care Med. 2015, 42, 202–210. [Google Scholar] [CrossRef]
- Basile-Filho, A.; Lago, A.F.; Menegueti, M.G.; Nicolini, E.A.; Rodrigues, L.A.D.B.; Nunes, R.S.; Auxiliadora-Martins, M.; Ferez, M.A. The use of APACHE II, SOFA, SAPS 3, C-reactive protein/albumin ratio, and lactate to predict mortality of surgical critically ill patients. Medicine 2019, 98, e16204. [Google Scholar] [CrossRef]
- Malbrain, M.L.; Marik, P.E.; Witters, I.; Cordemans, C.; Kirkpatrick, A.W.; Roberts, D.J.; Van Regenmortel, N. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: A systematic review with suggestions for clinical practice. Anaesthesiol. Intensiv. Ther. 2014, 46, 361–380. [Google Scholar] [CrossRef]
- Chapalain, X.; Vermeersch, V.; Egreteau, P.-Y.; Prat, G.; Alavi, Z.; Vicaut, E.; Huet, O. Association between fluid overload and SOFA score kinetics in septic shock patients: A retrospective multicenter study. J. Intensiv. Care 2019, 7, 42. [Google Scholar] [CrossRef] [Green Version]
- Demirci, C.; Aşçı, G.; Demirci, M.S.; Özkahya, M.; Töz, H.; Duman, S.; Sipahi, S.; Erten, S.; Tanrısev, M.; Ok, E. Impedance ratio: A novel marker and a powerful predictor of mortality in hemodialysis patients. Int. Urol. Nephrol. 2016, 48, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Lukaski, H.C.; Kyle, U.G.; Kondrup, J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: Phase Angle and Impedance Ratio. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Mulasi, U.; Kuchnia, A.J.; Cole, A.J.; Earthman, C.P. Bioimpedance at the Bedside: Current applications, limitations, and opportunities. Nutr. Clin. Pract. 2015, 30, 180–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kammar-García, A.; Castillo-Martínez, L.; Villanueva-Juárez, J.L.; Pérez-Pérez, A.; Rocha-González, H.I.; Arrieta-Valencia, J.; Remolina-Schlig, M.; Hernández-Gilsoul, T. Comparison of Bioelectrical Impedance Analysis Parameters for the Detection of Fluid Overload in the Prediction of Mortality in Patients Admitted at the Emergency Department. J. Parenter. Enter. Nutr. 2021, 45, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Kammar-García, A.; Pérez-Morales, Z.; Castillo-Martinez, L.; Villanueva-Juárez, J.L.; Bernal-Ceballos, F.; Rocha-González, H.I.; Remolina-Schlig, M.; Hernandez-Gilsoul, T. Mortality in adult patients with fluid overload evaluated by BIVA upon admission to the emergency department. Postgrad. Med. J. 2018, 94, 386–391. [Google Scholar] [CrossRef]
- Ronco, C.; Kaushik, M.; Valle, R.; Aspromonte, N.; Peacock, W.F. Diagnosis and Management of Fluid Overload in Heart Failure and Cardio-Renal Syndrome: The “5B” Approach. Semin. Nephrol. 2012, 32, 129–141. [Google Scholar] [CrossRef]
- Bernal-Ceballos, F.; Wacher-Rodarte, N.H.; Orea-Tejeda, A.; Hernández-Gilsoul, T.; Castillo-Martínez, L. Bioimpedance vector analysis in stable chronic heart failure patients: Level of agreement between single and multiple frequency devices. Clin. Nutr. ESPEN 2021, 43, 206–211. [Google Scholar] [CrossRef]
- García-Gigorro, R.; la Fuente, I.S.-D.; Mateos, H.M.; Andrés-Esteban, E.M.; Sanchez-Izquierdo, J.A.; Montejo-González, J.C. Utility of SOFA and Δ-SOFA scores for predicting outcome in critically ill patients from the emergency department. Eur. J. Emerg. Med. 2018, 25, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Lins, P.R.G.; Padilha, W.S.C.; Pimentel, C.F.M.G.; Batista, M.C.; De Gois, A.F.T. Risk factors, mortality and acute kidney injury outcomes in cirrhotic patients in the emergency department. BMC Nephrol. 2018, 19, 277. [Google Scholar] [CrossRef] [Green Version]
- Jones, A.E.; Trzeciak, S.; Kline, J.A. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit. Care Med. 2009, 37, 1649–1654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demandt, A.M.; Geerse, D.A.; Janssen, B.J.; Winkens, B.; Schouten, H.C.; Van Mook, W.N. The prognostic value of a trend in modified SOFA score for patients with hematological malignancies in the intensive care unit. Eur. J. Haematol. 2017, 99, 315–322. [Google Scholar] [CrossRef] [Green Version]
- Suberviola, B.; Castellanos-Ortega, A.; Ruiz, A.R.; Lopez-Hoyos, M.; Santibañez, M. Hospital mortality prognostication in sepsis using the new biomarkers suPAR and proADM in a single determination on ICU admission. Intensiv. Care Med. 2013, 39, 1945–1952. [Google Scholar] [CrossRef]
- Matsumura, Y.; Nakada, T.-A.; Abe, R.; Oshima, T.; Oda, S. Serum Procalcitonin Level and SOFA Score at Discharge from the Intensive Care Unit Predict Post-Intensive Care Unit Mortality: A Prospective Study. PLoS ONE 2014, 9, e114007. [Google Scholar] [CrossRef] [Green Version]
- ffrench-O’Carroll, R.; Frohlich, S.; Murphy, N.; Conlon, N. Predictors of outcome in decompensated liver disease: Validation of the SOFA-L score. Ir. Med. J. 2015, 108, 114–116. [Google Scholar]
- Ju, M.J.; Zhu, D.M.; Tu, G.W.; He, Y.Z.; Xue, Z.G.; Luo, Z.; Wu, Z.G. Predictive value of N-terminal pro-brain natriuretic peptide in combination with the sequential organ failure assessment score in sepsis. Chin. Med. J. 2012, 125, 1893–1898. [Google Scholar] [PubMed]
- Wang, X.; Jiao, J.; Wei, R.; Feng, Y.; Ma, X.; Li, Y.; Du, Y. A new method to predict hospital mortality in severe community acquired pneumonia. Eur. J. Intern. Med. 2017, 40, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Payen, D.; De Pont, A.-C.J.; Sakr, Y.; Spies, C.; Reinhart, K.; Vincent, J.-L. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit. Care 2008, 12, R74. [Google Scholar] [CrossRef] [Green Version]
- Sakr, Y.; Vincent, J.-L.; Reinhart, K.; Groeneveld, J.; Michalopoulos, A.; Sprung, C.L.; Artigas, A.; Ranieri, V.M. High Tidal Volume and Positive Fluid Balance Are Associated with Worse Outcome in Acute Lung Injury. Chest 2005, 128, 3098–3108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mancilla-Galindo, J.; Kammar-García, A.; Martínez-Esteban, A.; Meza-Comparán, H.D.; Mancilla-Ramírez, J.; Galindo-Sevilla, N. COVID-19 patients with increasing age experience differential time to initial medical care and severity of symptoms. Epidemiol. Infect. 2021, 149, e230. [Google Scholar] [CrossRef] [PubMed]
- Askim, Å.; Moser, F.; Gustad, L.T.; Stene, H.; Gundersen, M.; Åsvold, B.O.; Dale, J.; Bjørnsen, L.P.; Damås, J.K.; Solligård, E. Poor performance of quick-SOFA (qSOFA) score in predicting severe sepsis and mortality—A prospective study of patients admitted with infection to the emergency department. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 56. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, E.; Minkov, G.; Enchev, E.; Halacheva, K.; Yovtchev, Y. A combination of C-reactive protein and quick sequential organ failure assessment (qSOFA) score has better prognostic accuracy than qSOFA alone in patients with complicated intra-abdominal infections. Acta Chir. Belg. 2019, 120, 396–400. [Google Scholar] [CrossRef]
- Yu, H.; Nie, L.; Liu, A.; Wu, K.; Hsein, Y.-C.; Yen, D.W.; Lee, M.-T.G.; Lee, C.-C. Combining procalcitonin with the qSOFA and sepsis mortality prediction. Medicine 2019, 98, e15981. [Google Scholar] [CrossRef] [PubMed]
- Krishna, G.; Kumar, S.; Sankar, R.; Raghu, K.; Sathynarayana, V.; Siripriya, P. Sequential organ failure assessment and modified early warning score system versus quick SOFA score to predict the length of hospital stay in sepsis patients—Accuracy scoring study. Crit. Care Innov. 2021, 4, 9–18. [Google Scholar] [CrossRef]
- Brantlov, S.; Jødal, L.; Andersen, R.F.; Lange, A.; Rittig, S.; Ward, L.C. An evaluation of phase angle, bioelectrical impedance vector analysis and impedance ratio for the assessment of disease status in children with nephrotic syndrome. BMC Nephrol. 2019, 20, 331. [Google Scholar] [CrossRef] [Green Version]


| Variables | Total Sample n = 240 |
|---|---|
| Sex, n (%) | |
| Female | 140 (58.3) |
| Male | 100 (41.7) |
| Age, years | 60 (46–71.8) |
| BMI, kg/m2 | 24.5 (21.5–28.3) |
| <18 | 21 (8.8) |
| 18–24.9 | 113 (47.1) |
| 25–29.9 | 70 (29.2) |
| 30–34.9 | 21 (8.8) |
| 35–39.9 | 8 (3.3) |
| ≥40 | 7 (2.9) |
| Causes of hospitalization, n (%) | |
| Neurology | 12 (5) |
| Cardiovascular | 37 (15.4) |
| Respiratory | 23 (9.6) |
| Gastrointestinal | 72 (30) |
| Oncology | 7 (2.9) |
| Endocrinology | 9 (3.8) |
| Nephrology | 19 (7.9) |
| Rheumatology | 2 (0.8) |
| Infection | 54 (21.7) |
| Hematology | 7 (2.9) |
| Comorbidity, n (%) | |
| Diabetes | 74 (30.58) |
| Hypertension | 74 (30.8) |
| Renal failure | 39 (16.3) |
| Hepatic cirrhosis | 40 (16.7) |
| Malignancy | 49 (20.4) |
| VIH | 8 (3.3) |
| Use of Vasopressors, n (%) | 70 (29.2) |
| Use of a mechanical ventilator, n (%) | |
| Yes | 31 (12.9) |
| No | 209 (87.1) |
| Initial SOFA score, n (%) | 6 (4–9) |
| 0–1 | 17 (7.1) |
| 2–7 | 140 (58.3) |
| 8–11 | 56 (23.3) |
| >11 | 27 (11.3) |
| 30-days mortality, n (%) | 75 (31.3) |
| In-hospital mortality, n (%) | 59 (24.6) |
| ED mortality, n (%) | 24 (10) |
| 30–Days Mortality | In–Hospital Mortality | In–ED Mortality | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No n = 165 | Yes n = 75 | p Value | No n = 181 | Yes n = 59 | p Value | No n = 216 | Yes n = 24 | p Value | |
| Age, years | 57 (40.5–67) | 64 (51–76) | 0.005 | 58 (42.5–69) | 64 (50–76) | 0.036 | 59 (44.3–69) | 73 (54–80.1) | 0.009 |
| BMI | 24.6 (21.7–28.1) | 24.1 (20.8–24.1) | 0.735 | 24.6 (21.6–28.1) | 24 (20.9–28.7) | 0.998 | 24.2 (21.4–27.7) | 26.9 (21.9–30) | 0.159 |
| Initial SOFA score | 5 (3–7) | 9 (6–11) | <0.001 | 5 (3–7.5) | 9 (6–12) | <0.001 | 6 (4–9) | 9 (6–11.7) | 0.001 |
| Impedance ratio | 0.84 (0.8–0.87) | 0.87 (0.83–0.9) | <0.001 | 0.84 (0.8–0.87) | 0.87 (0.83–0.9) | <0.001 | 0.84 (0.8–0.88) | 0.88 (0.85–0.9) | 0.002 |
| Creatinine, mg/dL | 1.1 (0.72–2) | 1.6 (0.81–2.68) | 0.109 | 1.1 (0.73–2.08) | 1.62 (0.87–2.75) | 0.098 | 1.21 (0.75–2.1) | 2.06 (1–4.3) | 0.077 |
| CRP, mg/L | 5.2 (0.84–15.9) | 10.7 (5.5–15.3) | 0.056 | 5 (1.1–15.7) | 11.9 (6.7–15.5) | 0.028 | 7.1 (1.6–15.5) | 14.1 (11.3–21.9) | 0.017 |
| Bilirubin, mg/dL | 0.69 (0.47–1.5) | 1.66 (0.64–6.7) | <0.001 | 0.7 (0.48–1.51) | 1.95 (0.64–8.67) | <0.001 | 0.76 (0.5–1.81) | 3.39 (0.82–6.6) | 0.004 |
| Lactate, mg/dL | 1.7 (1.2–2.8) | 3.4 (1.9–6.2) | <0.001 | 1.8 (1.3–2.8) | 4.1 (2.2–6.7) | <0.001 | 2 (1.4–3.8) | 3.3 (2–6.9) | 0.005 |
| Unadjusted Model | Adjusted Model | |||||
|---|---|---|---|---|---|---|
| β Coefficient | HR (95% CI) | p Value | β Coefficient | HR (95% CI) | p Value | |
| 30-days mortality model a | ||||||
| Initial SOFA score | 0.16 | 1.18 (1.10–1.27) | <0.001 | 0.11 | 1.12 (1.03–1.22) | 0.012 |
| Impedance ratio | 0.10 | 1.11 (1.05–1.17) | <0.001 | 0.09 | 1.10 (1.04–1.16) | 0.002 |
| In-hospitality mortality model b | ||||||
| Initial SOFA score | 0.22 | 1.25 (1.16–1.34) | <0.001 | 0.21 | 1.23 (1.14–1.33) | <0.001 |
| Impedance ratio | 0.10 | 1.10 (1.05–1.17) | <0.001 | 0.09 | 1.10 (1.03–1.16) | 0.002 |
| ED mortality model c | ||||||
| Initial SOFA score | 0.19 | 1.20 (1.09–1.34) | <0.001 | 0.18 | 1.20 (1.08–1.33) | 0.001 |
| Impedance ratio | 0.14 | 1.15 (1.05–1.25) | 0.002 | 0.12 | 1.13 (1.03–1.24) | 0.014 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kammar-García, A.; Castillo-Martínez, L.; Mancilla-Galindo, J.; Villanueva-Juárez, J.L.; Pérez-Pérez, A.; Rocha-González, H.I.; Arrieta-Valencia, J.; Remolina-Schlig, M.; Hernández-Gilsoul, T. SOFA Score Plus Impedance Ratio Predicts Mortality in Critically Ill Patients Admitted to the Emergency Department: Retrospective Observational Study. Healthcare 2022, 10, 810. https://doi.org/10.3390/healthcare10050810
Kammar-García A, Castillo-Martínez L, Mancilla-Galindo J, Villanueva-Juárez JL, Pérez-Pérez A, Rocha-González HI, Arrieta-Valencia J, Remolina-Schlig M, Hernández-Gilsoul T. SOFA Score Plus Impedance Ratio Predicts Mortality in Critically Ill Patients Admitted to the Emergency Department: Retrospective Observational Study. Healthcare. 2022; 10(5):810. https://doi.org/10.3390/healthcare10050810
Chicago/Turabian StyleKammar-García, Ashuin, Lilia Castillo-Martínez, Javier Mancilla-Galindo, José Luis Villanueva-Juárez, Anayeli Pérez-Pérez, Héctor Isaac Rocha-González, Jesús Arrieta-Valencia, Miguel Remolina-Schlig, and Thierry Hernández-Gilsoul. 2022. "SOFA Score Plus Impedance Ratio Predicts Mortality in Critically Ill Patients Admitted to the Emergency Department: Retrospective Observational Study" Healthcare 10, no. 5: 810. https://doi.org/10.3390/healthcare10050810








