Impact of Statewide Mandatory Medicaid Managed Care (SMMC) Programs on Hospital Obstetric Outcomes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Outcome Variables
2.3. Statistical Analyses
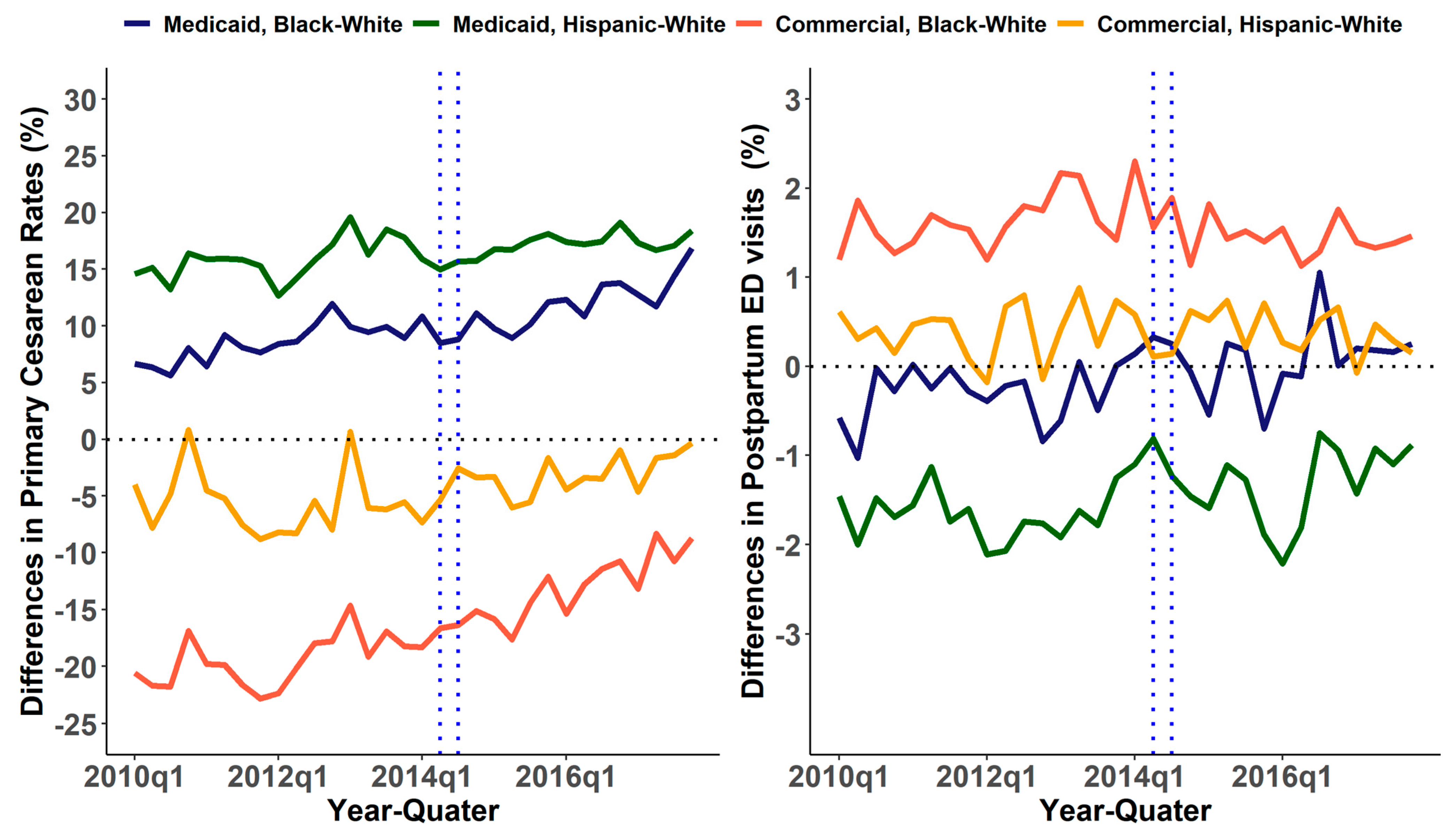
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Medicaid. November 2020 Medicaid & CHIP Enrollment Data Highlights. Available online: https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html (accessed on 18 May 2021).
- KFF. Medicaid Financing: The Basics. Available online: https://www.kff.org/medicaid/issue-brief/medicaid-financing-the-basics/ (accessed on 18 May 2021).
- Garfield, R.; Orgera, K.; Damico, A. The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid. Available online: http://files.kff.org/attachment/Issue-Brief-The-Coverage-Gap-Uninsured-Poor-Adults-in-States-that-Do-Not-Expand-Medicaid (accessed on 5 January 2020).
- KFF. Analysis of Recent National Trends in Medicaid and CHIP Enrollment. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/analysis-of-recent-national-trends-in-medicaid-and-chip-enrollment/ (accessed on 18 May 2021).
- Zhang, S.; Cardarelli, K.; Shim, R.; Ye, J.; Booker, K.L.; Rust, G. Racial Disparities in Economic and Clinical Outcomes of Pregnancy among Medicaid Recipients. Matern. Child Health J. 2013, 17, 1518–1525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flores, G. Racial and Ethnic Disparities in the Health and Health Care of Children. Pediatrics 2010, 125, 979. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basseyn, S.; Saloner, B.; Kenney, G.M.; Wissoker, D.; Polsky, D.; Rhodes, K.V. Primary Care Appointment Availability for Medicaid Patients. Med. Care 2016, 54, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Sastow, D.L.; White, R.S.; Mauer, E.; Chen, Y.; Gaber-Baylis, L.K.; Turnbull, Z.A. The Disparity of Care and Outcomes for Medicaid Patients Undergoing Colectomy. J. Surg. Res. 2019, 235, 190–201. [Google Scholar] [CrossRef]
- Rovner, B.W.; Casten, R.J. Emergency Department Visits in African Americans with Mild Cognitive Impairment and Diabetes. J. Diabetes Complicat. 2021, 35, 107905. [Google Scholar] [CrossRef]
- Hu, T.; Mortensen, K. Mandatory Statewide Medicaid Managed Care in Florida and Hospitalizations for Ambulatory Care Sensitive Conditions. Health Serv. Res. 2018, 53, 293–311. [Google Scholar] [CrossRef]
- Medicaid. Managed Care Authorities. Available online: https://www.medicaid.gov/medicaid/managed-care/managed-care-authorities/index.html (accessed on 18 May 2021).
- KFF. 10 Things to Know about Medicaid Managed Care. Available online: https://www.kff.org/medicaid/issue-brief/10-things-to-know-about-medicaid-managed-care/ (accessed on 18 May 2021).
- KFF. Total Medicaid MCO Enrollment. Available online: https://www.kff.org/other/state-indicator/total-medicaid-mco-enrollment/?activeTab=map¤tTimeframe=0&selectedDistributions=percent-of-state-medicaid-enrollment&sortModel=%7B%22colId%22:%22PercentofStateMedicaidEnrollment%22,%22sort%22:%22desc%22%7D (accessed on 18 May 2021).
- KFF. State Category. Medicaid/CHIP Eligibility Limits. Available online: https://www.kff.org/state-category/medicaid-chip/medicaidchip-eligibility-limits/ (accessed on 18 May 2021).
- Alker, J.; Hoadley, J. Medicaid Managed Care in Florida: Federal Waiver Approval and Implementation Medicaid Reform. Available online: http://ccf.georgetown.edu/wp-content/uploads/2013/10/Florida-Medicaid-Brief_Fall2013.pdf (accessed on 18 May 2021).
- Dubault, R.; Petrella, J.; Loftis, C. Evaluation of the Florida Medicaid MediPass Program Agency for Health Care Administration. 2002. Available online: https://fcmu.phhp.ufl.edu/research/focus/pdf/Report01-01-2002-EvalOfTheFlMedicaidMedipassProg.pdf (accessed on 18 May 2021).
- Florida Statewide Medicaid Monthly Enrollment Report. Available online: https://ahca.myflorida.com/medicaid/finance/data_analytics/enrollment_report/index.shtml (accessed on 18 May 2021).
- 2018 Share of Medicaid Enrollees in Managed Care. Available online: https://data.medicaid.gov/Enrollment/2018-Share-of-Medicaid-Enrollees-in-Managed-Care/cfcx-qyg7/data (accessed on 18 May 2021).
- Bindman, A.B.; Chattopadhyay, A.; Osmond, D.H.; Huen, W.; Bacchetti, P. The Impact of Medicaid Managed Care on Hospitalizations for Ambulatory Care Sensitive Conditions. Health Serv. Res. 2005, 40, 19–38. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Lee, K.H. The Association between Managed Care Enrollments and Potentially Preventable Hospitaliza-Tion among Adult Medicaid Recipients in Florida. BMC Health Serv. Res. 2014, 14, 247. [Google Scholar] [CrossRef] [Green Version]
- Zhan, C.; Miller, M.R.; Wong, H.; Meyer, G.S. The Effects of HMO Penetration on Preventable Hospitalizations. Health Serv. Res. 2004, 39, 345–361. [Google Scholar] [CrossRef] [Green Version]
- Powers, R.D. Emergency Department Use by Adult Medicaid Patients after Implementation of Managed Care. Acad. Emerg. Med. 2000, 7, 1416–1420. [Google Scholar] [CrossRef] [Green Version]
- Garrett, B.; Davidoff, A.J.; Yemane, A. Effects of Medicaid Managed Care Programs on Health Services Access and Use. Health Serv. Res. 2003, 38, 575–594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lowe, R.A.; Localio, A.R.; Schwarz, D.F.; Williams, S.; Tuton, L.W.; Maroney, S.; Nicklin, D.; Goldfarb, N.; Vojta, D.D.; Feldman, H.I. Association between Primary Care Practice Characteristics and Emergency Department Use in a Medicaid Managed Care Organization. Med. Care 2005, 43, 792–800. [Google Scholar] [CrossRef] [PubMed]
- HCUP State Inpatient Databases (SID). Healthcare Cost and Utilization Project (HCUP). 2016–2017. Available online: www.hcup-us.ahrq.gov/sidoverview.jsp (accessed on 6 June 2019).
- Kuklina, E.V.; Whiteman, M.K.; Hillis, S.D.; Jamieson, D.J.; Meikle, S.F.; Posner, S.F.; Marchbanks, P.A. An Enhanced Method for Identifying Obstetric Deliveries: Implications for Estimating Maternal Morbidity. Matern. Child Health J. 2008, 12, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Cahill, A.G.; Stamilio, D.M.; Odibo, A.O.; Peipert, J.; Stevens, E.; Macones, G.A. Racial Disparity in the Success and Complications of Vaginal Birth After Cesarean Delivery. Obstet. Gynecol. 2008, 111, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Y.J.; Liu, T.-L.; Howell, E.A. Insurance Differences in Preventive Care Use and Adverse Birth Outcomes Among Pregnant Women in a Medicaid Nonexpansion State: A Retrospective Cohort Study. J. Women’s Health 2020, 29, 29–37. [Google Scholar] [CrossRef]
- Aseltine, R.H.; Yan, J.; Fleischman, S.; Katz, M.; DeFrancesco, M. Racial and Ethnic Disparities in Hospital Readmissions After Delivery. Obstet. Gynecol. 2015, 126, 1040–1047. [Google Scholar] [CrossRef]
- Armstrong, J.C.; Kozhimannil, K.B.; McDermott, P.; Saade, G.R.; Srinivas, S.K. Comparing Variation in Hospital Rates of Cesarean Delivery among Low-Risk Women Using 3 Different Measures. Am. J. Obstet. Gynecol. 2016, 214, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Clapp, M.A.; Little, S.E.; Zheng, J.; Robinson, J.N. A Multi-State Analysis of Postpartum Readmissions in the United States. Am. J. Obstet. Gynecol. 2016, 215, e1–e113. [Google Scholar] [CrossRef]
- Mascha, E.J.; Sessler, D.I. Segmented Regression and Difference-in-Difference Methods. Anesth. Analg. 2019, 129, 618–633. [Google Scholar] [CrossRef]
- Rainham, D. Do Differences in Health Make a Difference? A Review for Health Policymakers. Health Policy 2007, 84, 123–132. [Google Scholar] [CrossRef]
- Grafova, I.B.; Freedman, V.A.; Lurie, N.; Kumar, R.; Rogowski, J. The Difference-in-Difference Method: Assessing the Selection Bias in the Effects of Neighbor-Hood Environment on Health. Econ. Hum. Biol. 2014, 13, 20–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wing, C.; Simon, K.; Bello-Gomez, R.A. Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annu. Rev. Public Health 2018, 39, 453–469. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bateman, B.T.; Mhyre, J.M.; Hernandez-Diaz, S.; Huybrechts, K.F.; Fischer, M.A.; Creanga, A.A.; Callaghan, W.M.; Gagne, J.J. Development of a Comorbidity Index for Use in Obstetric Patients. Obstet. Gynecol. 2013, 122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Postlethwaite, D.; Armstrong, M.A.; Hung, Y.Y.; Shaber, R. Pregnancy Outcomes by Pregnancy Intention in a Managed Care Setting. Matern. Child Health J. 2010, 14, 227–234. [Google Scholar] [CrossRef]
- Oleske, D.M.; Linn, E.S.; Nachman, K.L.; Marder, R.J.; Sangl, J.A.; Smith, T. Effect of Medicaid Managed Care on Pregnancy Complications. Obstet. Gynecol. 2000, 95, 6–13. [Google Scholar] [CrossRef]
- Tai-Seale, M.; LoSasso, A.T.; Freund, D.A.; Gerber, S.E. The Long-Term Effects of Medicaid Managed Care on Obstetric Care in Three California Coun-Ties. Health Serv. Res. 2001, 36, 751–75171. [Google Scholar]
- Gottlieb, L.M.; Garcia, K.; Wing, H.; Manchanda, R. Clinical Interventions Addressing Nonmedical Health Determinants in Medicaid Managed Care. Am. J. Manag. Care 2016, 22, 370–376. [Google Scholar]
- Marín, H.A.; Ramírez, R.; Wise, P.H.; Peña, M.; Sánchez, Y.; Torres, R. The Effect of Medicaid Managed Care on Prenatal Care: The Case of Puerto Rico. Matern. Child Health J. 2009, 13, 187–197. [Google Scholar] [CrossRef]
- Cogan, L.W.; Josberger, R.E.; Gesten, F.C.; Roohan, P.J. Can Prenatal Care Impact Future Well-Child Visits? The Experience of a Low Income Population in New York State Medicaid Managed Care. Matern. Child Health J. 2012, 16, 92–99. [Google Scholar] [CrossRef]
- Deshpande, N.A.; Oxford, C.M. Management of Pregnant Patients Who Refuse Medically Indicated Cesarean Delivery. Rev. Obstet. Gynecol. 2012, 5, e144–e150. [Google Scholar]
- O’Donovan, C.; O’Donovan, J. Why Do Women Request an Elective Cesarean Delivery for Non-medical Reasons? A Systematic Review of the Qualitative Literature. Birth 2018, 45, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Al Shamsi, H.; Almutairi, A.G.; Al Mashrafi, S.; Al Kalbani, T. Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med. J. 2020, 35, e122. [Google Scholar] [CrossRef]
- Bromley, E.; Nunes, A.; Phipps, M.G. Disparities in Pregnancy Healthcare Utilization between Hispanic and Non-hispanic White Women in Rhode Island. Matern. Child Health J. 2012, 16, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Timmins, C.L. The Impact of Language Barriers on the Health Care of Latinos in the United States: A Review of the Literature and Guidelines for Practice. J. Midwifery Women’s Health 2002, 47, 80–96. [Google Scholar] [CrossRef]
- Shaffer, C.F. Factors Influencing the Access to Prenatal Care by Hispanic Pregnant Women. J. Am. Acad. Nurse Pract. 2002, 14, 93–96. [Google Scholar] [CrossRef]
- Guglielminotti, J.; Deneux-Tharaux, C.; Wong, C.A.; Li, G. Hospital-Level Factors Associated with Anesthesia-Related Adverse Events in Cesarean Deliver-Ies, New York State, 2009–2011. Anesth. Analg. 2016, 122, 1947–1956. [Google Scholar] [CrossRef]
- Sebastião, Y.V.; Womack, L.; Vamos, C.A.; Louis, J.M.; Olaoye, F.; Caragan, T.; Bubu, O.M.; Detman, L.A.; Curran, J.S.; Sappenfield, W.M. Hospital Variation in Cesarean Delivery Rates: Contribution of Individual and Hospital Factors in Florida. Am. J. Obstet. Gynecol. 2016, 214, 123.e1–123.e18. [Google Scholar] [CrossRef]
- Kingdon, C.; Downe, S.; Betran, A.P. Non-clinical Interventions to Reduce Unnecessary Caesarean Section Targeted at Organisations, Facilities and Systems: Systematic Review of Qualitative Studies. PLoS ONE 2018, 13, e0203274. [Google Scholar] [CrossRef]
- Kozhimannil, K.B.; Hardeman, R.R.; Alarid-Escudero, F.; Vogelsang, C.A.; Blauer-Peterson, C.; Howell, E.A. Modeling the Cost-Effectiveness of Doula Care Associated with Reductions in Preterm Birth and Cesarean Delivery. Birth 2016, 43, 20–27. [Google Scholar] [CrossRef]
- Miami Herald. Florida Says Privatizing Medicaid Cut Costs, but Insurers Say They’re Underpaid by State. Available online: https://www.miamiherald.com/news/health-care/article27532903.html (accessed on 21 May 2021).
- Britton, M.C.; Ouellet, G.M.; Minges, K.E.; Gawel, M.; Hodshon, B.; Chaudhry, S.I. Care Transitions between Hospitals and Skilled Nursing Facilities: Perspectives of Sending and Receiving Providers. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 565–572. [Google Scholar] [CrossRef] [Green Version]
- Berry, J.G.; Hall, D.E.; Kuo, D.Z.; Cohen, E.; Agrawal, R.; Feudtner, C.; Hall, M.; Kueser, J.; Kaplan, W.; Neff, J. Hospital Utilization and Characteristics of Patients Experiencing Recurrent Readmissions within Children’s Hospitals. JAMA 2011, 305, 682–690. [Google Scholar] [CrossRef] [Green Version]
- Hirko, K.A.; Kerver, J.M.; Ford, S.; Szafranski, C.; Beckett, J.; Kitchen, C.; Wendling, A.L. TeleHealth in Response to the COVID-19 Pandemic: Implications for Rural Health Disparities. J. Am. Med. Inform. Assoc. 2020, 27, 1816–1818. [Google Scholar] [CrossRef] [PubMed]
- Shang, J.; Chastain, A.M.; Perera, U.G.E.; Quigley, D.D.; Fu, C.J.; Dick, A.W.; Pogorzelska-Maziarz, M.; Stone, P.W. COVID-19 Preparedness in US Home Health Care Agencies. J. Am. Med. Dir. Assoc. 2020, 21, 924–927. [Google Scholar] [CrossRef] [PubMed]
- Michael Sparer Medicaid Managed Care: Costs, Access, and Quality of Care. Available online: https://www.rwjf.org/en/library/research/2012/09/medicaid-managed-care.html (accessed on 15 May 2021).
- KFF. Medicaid Managed Care Market Tracker. Available online: https://www.kff.org/data-collection/medicaid-managed-care-market-tracker/ (accessed on 17 May 2021).
- MacDorman, M.; Declercq, E. Trends and State Variations in Out-Of-Hospital Births in the United States, 2004–2017. Birth 2019, 46, 279–288. [Google Scholar] [CrossRef] [PubMed]

| Overall, N = 1,499,994, n (%) | Pre SMMC Period N = 791,718, n (%) | Post SMMC Period N = 662,981, n (%) | p Value | |
|---|---|---|---|---|
| Cesarean delivery | ||||
| Yes | 584,604(38.9) | 310,779 (39.3) | 256,113 (38.6) | p < 0.05 |
| No | 915,390 (61.1) | 480,939 (60.7) | 4,066,868 (61.4) | |
| Primary cesarean delivery | ||||
| Yes | 313,127 (20.8) | 170,287 (21.5) | 133,524 (20.1) | p < 0.05 |
| No | 118,686 (79.2) | 621,431 (78.5) | 529,457 (79.9) | |
| Preterm birth | ||||
| Yes | 122,566 (8.1) | 57,266 (7.2) | 62,488 (9.4) | p < 0.05 |
| No | 1,377,428 (91.9) | 734,452 (92.7) | 600,493 (90.6) | |
| Postpartum readmission | ||||
| Yes | 29,872 (2.0) | 14,882 (1.9) | 141,21 (2.1) | p < 0.05 |
| No | 1,470,122(98.0) | 776,836 (98.1) | 648,860 (97.9) | |
| Postpartum ED visit | ||||
| Yes | 53,152 (3.5) | 29,183 (3.7) | 22,351 (3.4) | p < 0.05 |
| No | 1,446,842 (96.5) | 762,535 (96.3) | 640,630 (96.6) | |
| Prior Cesarean | ||||
| Yes | 287,554 (19.2) | 147,551 (18.6) | 131,124 (19.7) | p < 0.05 |
| No | 1,212,440 (80.8) | 644,167 (81.4) | 531,857 (80.3) | |
| Vaginal delivery after cesarean | ||||
| Yes | 16,077 (1.1) | 7059 (0.9) | 8535 (1.3) | p < 0.05 |
| No | 1,483,917 (98.9) | 784,659 (91.1) | 654,446 (98.7) | |
| Age (years) | ||||
| <18 | 27,026 (1.8) | 17,608 (2.2) | 8743 (1.3) | p < 0.05 |
| 18–30 | 858,875 (57.2) | 465,166 (58.8) | 368,082 (55.5) | |
| 30–40 | 566,371 (37.8) | 284,143 (35.9) | 264,686 (39.9) | |
| >40 | 477,22 (3.2) | 24,801 (3.1) | 21,470 (3.2) | |
| Race/ethnicity | ||||
| Non-Hispanic white | 724,174 (48.3) | 385,544 (48.7) | 316,442 (47.7) | p < 0.05 |
| Non-Hispanic Black | 347,720 (23.2) | 186,190 (23.5) | 151,323 (22.8) | |
| Hispanic | 329,438 (22.0) | 168,357 (21.3) | 151,295 (22.8) | |
| Others | 79,979 (5.3) | 41,697 (5.3) | 35,721 (5.3) | |
| Payor | ||||
| Medicaid | 778,662 (51.9) | 421,623 (53.3) | 333,341 (50.3) | p < 0.05 |
| Commercial | 646,442 (43.1) | 326,714 (41.3) | 300,091 (40.3) | |
| Others | 74,890 (5.0) | 43,381 (5.4) | 29,549 (4.4) | |
| Comorbidity score | ||||
| 0 | 1,196,338(79.8) | 649,319 (82.0) | 510,534 (77.0) | p < 0.05 |
| 1–2 | 232,181 (15.5) | 112,014 (14.1) | 113,321 (17.1) | |
| >2 | 71,475 (4.8) | 30,385 (3.8) | 39,126 (5.9) | |
| SMMC: Statewide Mandatory Managed Care | ||||
| Outcomes | Overall Insurance × PostSMMC | Racial/Ethnic Disparities Insurance × Race/Ethnicity × PostSMMC | |
|---|---|---|---|
| Medicaid Beneficiaries Incidence Ratio (95% CI) | Medicaid Non-Hispanic Black Incidence Ratio (95% CI) | Medicaid Hispanic Beneficiaries Incidence Ratio (95% CI) | |
| Primary cesarean rates | 0.91 (0.88–0.93) | 1.04 (0.99–1.10) | 1.14 (1.08–1.19) |
| Preterm birth rates | 0.94 (0.91–0.98) | 1.03 (0.97–1.05) | 1.05 (0.97–0.98) |
| Postpartum ED visits | 0.87 (0.82–0.93) | 1.13 (1.02–1.26) | 1.07 (0.96–1.21) |
| Postpartum preventable readmissions rates | 0.86 (0.80–0.93) | 1.11 (0.98–1.26) | 1.02 (0.88–1.17) |
| Vaginal birth after cesarean (VBAC) rates | 1.02 (0.92–1.12) | 1.04 (0.86–1.26) | 1.11 (0.90–1.36) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Symum, H.; Zayas-Castro, J. Impact of Statewide Mandatory Medicaid Managed Care (SMMC) Programs on Hospital Obstetric Outcomes. Healthcare 2022, 10, 874. https://doi.org/10.3390/healthcare10050874
Symum H, Zayas-Castro J. Impact of Statewide Mandatory Medicaid Managed Care (SMMC) Programs on Hospital Obstetric Outcomes. Healthcare. 2022; 10(5):874. https://doi.org/10.3390/healthcare10050874
Chicago/Turabian StyleSymum, Hasan, and José Zayas-Castro. 2022. "Impact of Statewide Mandatory Medicaid Managed Care (SMMC) Programs on Hospital Obstetric Outcomes" Healthcare 10, no. 5: 874. https://doi.org/10.3390/healthcare10050874





