Encouraging People with Spinal Cord Injury to Take Part in Physical Activity in the COVID-19 Epidemic through the mHealth ParaSportAPP
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Instruments
2.3.1. Questionnaires
Self-Reported PA
Anxiety and Depression Levels
Resilience
Independence
Quality of Life
2.3.2. Respiratory Muscle Strength
2.3.3. Spirometry and Cardiopulmonary Exercise Test
2.3.4. ParaSportAPP
2.4. Data Analysis
2.5. Statistical Analysis
3. Results
3.1. Self-Reported PA
3.2. Anxiety, Depression and Resilience Levels
3.3. Independence and Quality of Life
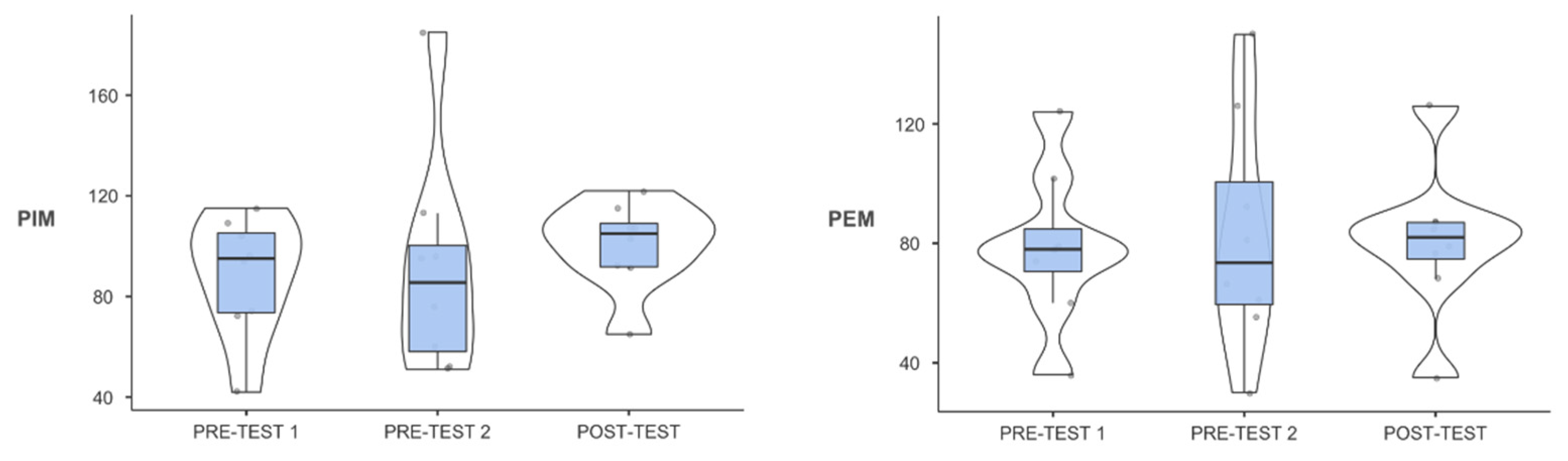
3.4. Respiratory Muscle Strength, Spirometry and Cardiopulmonary Exercise Test
 oxygen pulse (F2,14 = 2.578; p = 0.11; η2p = 0.269), RER (F2,14 = 1.937; p = 0.18; η2p = 0.217) and peak power (F2,14 = 2.48; p = 0.12; η2p = 0.262)) (Figure 2).
oxygen pulse (F2,14 = 2.578; p = 0.11; η2p = 0.269), RER (F2,14 = 1.937; p = 0.18; η2p = 0.217) and peak power (F2,14 = 2.48; p = 0.12; η2p = 0.262)) (Figure 2).4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Nomenclature
| AQoL8-D | Assessment of Quality of Life-8 Dimensions |
| FEV1 | Forced Expiratory Volume in the first second |
| FVC | Forced Vital Capacity |
| HADS | Hospital Anxiety and Depression Scale |
| PA | Physical Activity |
| PASIPD | Physical Activity Scale for Individuals with Physical Disabilities |
| PEF | Peak Expiratory Flow |
| RER | Peak Respiratory Exchange Ratio |
| RS-25 | Resilience Scale - 25 |
| SCI | Spinal Cord Injury |
| SCIM III | Spinal Cord Independence Measure III |
| VO2max | Maximal oxygen consumption |
| VO2VT1 | Oxygen Consumption during the First Ventilatory Threshold |
| VO2VT2 | Oxygen Consumption during the Second Ventilatory Threshold |
References
- Richardson, A.; Samaranayaka, A.; Sullivan, M.; Derrett, S. Secondary health conditions and disability among people with spinal cord injury: A prospective cohort study. J. Spinal Cord Med. 2021, 44, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, C.; Tonge, B.; Taleporos, G. Spinal Cord Injury and Mental Health. Aust. N. Z. J. Psychiatry 2008, 42, 309–314. [Google Scholar] [CrossRef]
- Kirshblum, S.C.; Burns, S.P.; Biering-Sørensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Johansen, M.; Jones, L.; Krassioukov, A.; Mulcahey, M.J.; et al. International standards for neurological classification of spinal cord injury (Revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef] [Green Version]
- Lala, D.; Dumont, F.S.; Leblond, J.; Houghton, P.E.; Noreau, L. Impact of Pressure Ulcers on Individuals Living with a Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2014, 95, 2312–2319. [Google Scholar] [CrossRef] [PubMed]
- Montesinos-Magraner, L.; Serra-Añó, P.; García-Massó, X.; Ramírez-Garcerán, L.; González, L.M.; González-Viejo, M.Á. Comorbidity and physical activity in people with paraplegia: A descriptive cross-sectional study. Spinal Cord 2018, 56, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Harvey, L.A. Physiotherapy rehabilitation for people with spinal cord injuries. J. Physiother. 2016, 62, 4–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montesinos-Magraner, L.; López-Bueno, L.; Gomez-Garrido, A.; Gomis, M.; González, L.M.; García-Massó, X.; Serra-Añó, P. The influence of regular physical activity on lung function in paraplegic people. Spinal Cord 2016, 54, 861–865. [Google Scholar] [CrossRef] [Green Version]
- Ginis, K.A.M.; Latimer, A.; Arbour-Nicitopoulos, K.P.; Buchholz, A.C.; Bray, S.; Craven, B.; Hayes, K.C.; Hicks, A.L.; McColl, M.A.; Potter, P.J.; et al. Leisure time physical activity in a population-based sample of people with spinal cord injury part I: Demographic and injury-related correlates. Arch. Phys. Med. Rehabil. 2010, 91, 722–728. [Google Scholar] [CrossRef]
- Fekete, C.; Rauch, A. Correlates and determinants of physical activity in persons with spinal cord injury: A review using the International Classification of Functioning, Disability and Health as reference framework. Disabil. Health J. 2012, 5, 140–150. [Google Scholar] [CrossRef]
- Marco-Ahulló, A.; Montesinos-Magraner, L.; González, L.M.; Morales, J.; Bernabéu-García, J.A.; García-Massó, X. Impact of COVID-19 on the self-reported physical activity of people with complete thoracic spinal cord injury full-time manual wheelchair users. J. Spinal Cord Med. 2021, 1–5. [Google Scholar] [CrossRef]
- Rezende, L.S.; Lima, M.B.; Salvador, E.P. Interventions for Promoting Physical Activity Among Individuals With Spinal Cord Injury: A Systematic Review. J. Phys. Act. Health 2018, 15, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Pavón, D.; Carbonell-Baeza, A.; Lavie, C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: Special focus in older people. Prog. Cardiovasc. Dis. 2020, 63, 386. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.M.; Sanchis-Gomar, F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Eur. J. Prev. Cardiolog. 2020, 27, 906–908. [Google Scholar] [CrossRef] [PubMed]
- Jee, H. Review of researches on smartphone applications for physical activity promotion in healthy adults. J. Exerc. Rehabil. 2017, 13, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Topol, E.J.; Steinhubl, S.R.; Torkamani, A. Digital Medical Tools and Sensors. JAMA 2015, 313, 353–354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marcolino, M.S.; Oliveira, J.A.Q.; D’Agostino, M.; Ribeiro, A.L.; Alkmim, M.B.M.; Novillo-Ortiz, D. The Impact of mHealth Interventions: Systematic Review of Systematic Reviews. JMIR mHealth uHealth 2018, 6, e23. [Google Scholar] [CrossRef] [Green Version]
- Medina Riaño, C.A.; Cumbal Figueroa, D.; Nieto Ortíz, L.Y.; Cano de la Cuerda, R.; Pinzón Bernal, M.Y. Aplicaciones móviles para lesión medular. Una revisión sistemática. Fisioterapia 2020, 42, 319–326. [Google Scholar] [CrossRef]
- Pérez-Tejero, J.; García-Hernández, J.J.; Coterón, J.; Benito-Peinado, P.J.; Sampedro-Molinuevo, J. Medición de los niveles de actividad física en personas con discapacidad física mediante acelerometría y cuestionario. Arch. Med. Deporte 2012, 25, 517–526. [Google Scholar]
- Herrero, M.J.; Blanch, J.; Peri, J.M.; De Pablo, J.; Pintor, L.; Bulbena, A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. Gen. Hosp. Psychiatry 2003, 25, 277–283. [Google Scholar] [CrossRef]
- Las Hayas, C.; Calvete, E.; Gómez del Barrio, A.; Beato, L.; Muñoz, P.; Padierna, J.Á. Resilience Scale-25 Spanish version: Validation and assessment in eating disorders. Eat. Behav. 2014, 15, 460–463. [Google Scholar] [CrossRef]
- Snyder, C.R.; Lopez, S.J. Oxford Handbook of Positive Psychology; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Aguilar-Rodríguez, M.; Peña-Pachés, L.; Grao-Castellote, C.; Torralba-Collados, F.; Hervás-Marín, D.; Giner-Pascual, M. Adaptation and validation of the Spanish self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2015, 53, 451–454. [Google Scholar] [CrossRef] [Green Version]
- Richardson, J.; Iezzi, A.; Khan, M.A.; Maxwell, A. Validity and Reliability of the Assessment of Quality of Life (AQoL)-8D Multi-Attribute Utility Instrument. Patient 2014, 7, 85–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- West, C.R.; Taylor, B.J.; Campbell, I.G.; Romer, L.M. Effects of inspiratory muscle training on exercise responses in Paralympic athletes with cervical spinal cord injury. Scand. J. Med. Sci. Sports 2014, 24, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Postma, K.; Haisma, J.A.; Hopman, M.T.E.; Bergen, M.P.; Stam, H.J.; Bussmann, J.B. Resistive inspiratory muscle training in people with spinal cord injury during inpatient rehabilitation: A randomized controlled trial. Phys. Ther. 2014, 94, 1709–1719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marco-Ahulló, A.; Montesinos-Magraner, L.; Gonzalez, L.M.; Llorens, R.; Segura-Navarro, X.; García-Massó, X. Validation of Using Smartphone Built-In Accelerometers to Estimate the Active Energy Expenditures of Full-Time Manual Wheelchair Users with Spinal Cord Injury. Sensors 2021, 21, 1498. [Google Scholar] [CrossRef] [PubMed]
- Ginis, K.A.M.; Van Der Scheer, J.W.; Latimer, A.; Barrow, A.; Bourne, C.; Carruthers, P.; Bernardi, M.; Ditor, D.S.; Gaudet, S.; De Groot, S.; et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: An update and a new guideline. Spinal Cord 2018, 56, 308–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chemtob, K.; Rocchi, M.; Arbour-Nicitopoulos, K.; Kairy, D.; Fillion, B.; Sweet, S.N. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychol. Sport Exerc. 2019, 43, 243–252. [Google Scholar] [CrossRef]
- Zemper, E.D.; Tate, D.G.; Roller, S.; Forchheimer, M.; Chiodo, A.; Nelson, V.S.; Scelza, W. Assessment of a holistic wellness program for persons with spinal cord injury. Am. J. Phys. Med. Rehabil. 2003, 82, 957–968. [Google Scholar] [CrossRef]
- Nooijen, C.F.; Stam, H.J.; Sluis, T.; Valent, L.; Twisk, J.; Van den Berg-Emons, R.J. A behavioral intervention promoting physical activity in people with subacute spinal cord injury: Secondary effects on health, social participation and quality of life. Clin. Rehabil. 2017, 31, 772–780. [Google Scholar] [CrossRef]
- Nightingale, T.E.; Rouse, P.C.; Walhin, J.P.; Thompson, D.; Bilzon, J.L.J. Home-Based Exercise Enhances Health-Related Quality of Life in Persons With Spinal Cord Injury: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2018, 99, 1998–2006. [Google Scholar] [CrossRef]
- Todd, K.R.; Lawrason, S.V.C.; Shaw, R.B.; Wirtz, D.; Martin Ginis, K.A. Physical activity interventions, chronic pain, and subjective well-being among persons with spinal cord injury: A systematic scoping review. Spinal Cord 2021, 59, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Fiordelli, M.; Diviani, N.; Schulz, P.J. Mapping mHealth research: A decade of evolution. J. Med. Internet Res. 2013, 15, e95. [Google Scholar] [CrossRef] [PubMed]
- Dicianno, B.E.; Parmanto, B.; Fairman, A.D.; Crytzer, T.M.; Yu, D.X.; Pramana, G.; Coughenour, D.; Petrazzi, A.A. Perspectives on the evolution of mobile (mHealth) technologies and application to rehabilitation. Phys. Ther. 2015, 95, 397–405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nussbaum, R.; Kelly, C.; Quinby, E.; Mac, A.; Parmanto, B.; Dicianno, B.E. Systematic Review of Mobile Health Applications in Rehabilitation. Arch. Phys. Med. Rehabil. 2019, 100, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Kryger, M.A.; Crytzer, T.M.; Fairman, A.; Quinby, E.J.; Karavolis, M.; Pramana, G.; Setiawan, I.M.A.; McKernan, G.P.; Parmanto, B.; Dicianno, B.E. The Effect of the Interactive Mobile Health and Rehabilitation System on Health and Psychosocial Outcomes in Spinal Cord Injury: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e14305. [Google Scholar] [CrossRef]
- MacGillivray, M.K.; Sadeghi, M.; Mills, P.B.; Adams, J.; Sawatzky, B.J.; Mortenson, W.B. Implementing a self-management mobile app for spinal cord injury during inpatient rehabilitation and following community discharge: A feasibility study. J. Spinal Cord Med. 2020, 43, 676–684. [Google Scholar] [CrossRef]
- Canori, A.; Amiri, A.M.; Thapa-Chhetry, B.; Finley, M.A.; Schmidt-Read, M.; Lamboy, M.R.; Intille, S.S.; Hiremath, S.V. Relationship between pain, fatigue, and physical activity levels during a technology-based physical activity intervention. J. Spinal Cord Med. 2020, 44, 549–556. [Google Scholar] [CrossRef]
- Hiremath, S.V.; Amiri, A.M.; Thapa-Chhetry, B.; Snethen, G.; Schmidt-Read, M.; Ramos-Lamboy, M.; Coffman, D.L.; Intille, S.S. Correction: Mobile health-based physical activity intervention for individuals with spinal cord injury in the community: A pilot study. PLoS ONE 2019, 14, e0225490. [Google Scholar] [CrossRef]
- Marco-Ahulló, A.; Montesinos-Magraner Ll Segura-Navarro, X.; Crespo-Rivero, T.; González, L.M.; García-Massó, X. Diseño y usabilidad de ParaSportAPP: Una mHealth destinada a promocionar la actividad física en personas con lesión medular. Rev. Andal. Med. Deporte, 2022; in press. [Google Scholar]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2020, 64, 108–110. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, C.M.; Eriks-Hoogland, I.; Middleton, J.W. Now, more than ever, our community is needed: Spinal cord injury care during a global pandemic. Spinal Cord Ser. Cases 2020, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M. Pandemics, climate change, and disability related to SCI. Spinal Cord Ser. Cases. 2020, 6, 36. [Google Scholar] [CrossRef] [PubMed]

| Age (Years) | Sex (Women/Men) | Thoracic Injury Level (High/Low) | Weight (kg) | Height (cm) | Injury Time (Years) | |
|---|---|---|---|---|---|---|
| Only completed questionnaires (n = 14) | 43.14 (9.49) | 3/11 | 6/8 | 70.96 (12.92) | 174.07 (9.37) | 16.57 (11.03) |
| Completed all tests (n = 8) | 47.87 (12.47) | 1/7 | 3/5 | 71.94 (18.45) | 173.25 (11.49) | 20.5 (11.02) |
| Pre-Test 1 | Pre-Test 2 | Post-Test | p-Value | χ22 | F | ||
|---|---|---|---|---|---|---|---|
| Self-reported PA | PASIPD * Total | 21.81 (20.4) | 20 (14.37) | 22.4 (29.69) | 0.88 | 0.25 | - |
| PASIPD * Recreational activities | 16.56 (15.16) | 17.13 (9.34) | 17.29 (17.65) | 0.19 | 3.31 | - | |
| PASIPD * Housework | 1.39 (5.75) | 1.17 (3.03) | 2.01 (5.53) | 0.12 | 4.16 | - | |
| PASIPD * Occupational activities | 0 (0) | 0 (0) | 0 (2.81) | 0.37 | 2.00 | - | |
| Anxiety and Depression | HADS * Total | 6 (4) | 6.5 (4.25) | 5.5 (6.25) | 0.76 | 0.54 | - |
| HADS Anxiety | 4 (2.83) | 3.93 (2.81) | 3.79 (2.91) | 0.91 | - | 0.096 | |
| HADS * Depression | 2 (2.5) | 2 (3.25) | 2 (3.25) | 0.90 | 0.20 | - | |
| Resilience | RS-25 | 151.43 (12.81) | 150.42 (12.49) | 145.29 (15.34) | 0.06 | - | 3.16 |
| Independence | SCIM III | 68.88 (6.85) | 68.57 (6.83) | 68.43 (7.7) | 0.78 | - | 0.153 |
| Quality of Life | AQoL Total | 80.15 (12,57) | 81.2 (8.15) | 80.85 (13.33) | 0.98 | 0.04 | - |
| AQoL * Independent living | 80.16 (11.67) | 77.78 (13.25) | 76.19 (15.77) | 0.52 | - | 0.68 | |
| AQoL Pain | 70 (12.5) | 80 (20) | 75 (25) | 0.28 | 2.54 | - | |
| AQoL * Senses | 96.15 (9.62) | 92.31 (15.39) | 96.15 (7.69) | 0.66 | 0.84 | - | |
| AQoL Happiness | 81.25 (14.06) | 78.12 (12.5) | 81.25 (12.5) | 0.14 | 3.95 | - | |
| AQoL Coping | 83.33 (16.66) | 83.33 (16.66) | 83.33 (16.66) | 0.79 | 0.45 | - | |
| AQoL * Mental health | 80.3 (12.88) | 78.78 (12.87) | 78.78 (15.9) | 0.33 | 2.21 | - | |
| AQoL * Personal relationships | 82.8 (7.63) | 84.13 (7.47) | 84.13 (9.57) | 0.67 | - | 0.67 | |
| AQoL Self-esteem | 75 (16.66) | 75 (16.66) | 75 (18.74) | 0.05 | 6.0 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marco-Ahulló, A.; Montesinos-Magraner, L.; González, L.-M.; Crespo-Rivero, T.; Launois-Obregón, P.; García-Massó, X. Encouraging People with Spinal Cord Injury to Take Part in Physical Activity in the COVID-19 Epidemic through the mHealth ParaSportAPP. Healthcare 2022, 10, 1069. https://doi.org/10.3390/healthcare10061069
Marco-Ahulló A, Montesinos-Magraner L, González L-M, Crespo-Rivero T, Launois-Obregón P, García-Massó X. Encouraging People with Spinal Cord Injury to Take Part in Physical Activity in the COVID-19 Epidemic through the mHealth ParaSportAPP. Healthcare. 2022; 10(6):1069. https://doi.org/10.3390/healthcare10061069
Chicago/Turabian StyleMarco-Ahulló, Adrià, Lluïsa Montesinos-Magraner, Luís-Millan González, Teresa Crespo-Rivero, Patricia Launois-Obregón, and Xavier García-Massó. 2022. "Encouraging People with Spinal Cord Injury to Take Part in Physical Activity in the COVID-19 Epidemic through the mHealth ParaSportAPP" Healthcare 10, no. 6: 1069. https://doi.org/10.3390/healthcare10061069







