Development of a General Health Score Based on 12 Objective Metabolic and Lifestyle Items: The Lifestyle and Well-Being Index
Abstract
:1. Introduction
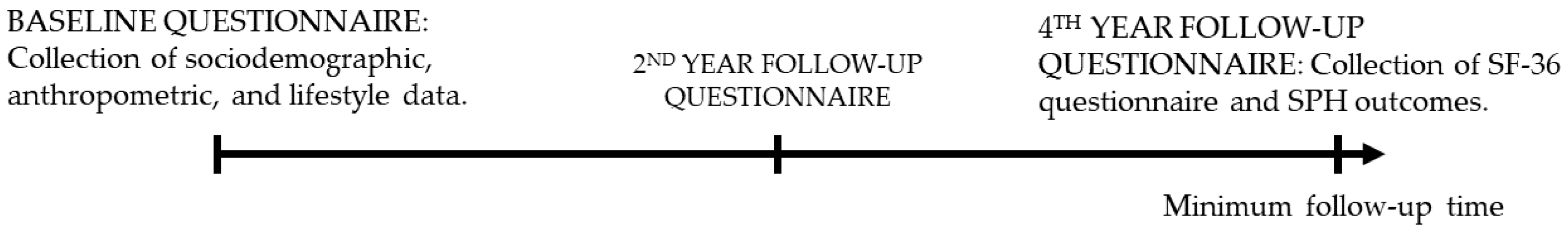
2. Materials and Methods
2.1. Study Type and Population
2.2. Primary Outcome: Health Related Quality of Life (SF-36)
2.3. Sociodemographic, Dietary and Lifestyle Items Included in the LWB-Index
2.4. Statistical Analyses
3. Results
3.1. Development of the LWB-I
3.2. Defining LWB-I Cut Points
4. Discussion
4.1. Lifestyle and Well-Being
4.2. Lifestyle Characteristics in Association with Well-Being
4.3. Metabolic Characteristics and Their Associations with Well-Being
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Karimi, M.; Brazier, J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics 2016, 34, 645–649. [Google Scholar] [CrossRef]
- Kivits, J.; Erpelding, M.L.; Guillemin, F. Social determinants of health-related quality of life. Rev. Epidemiol. Sante Publique 2013, 61 (Suppl. 3), S189–S194. [Google Scholar] [CrossRef]
- Bauldry, S.; Shanahan, M.J.; Boardman, J.D.; Miech, R.A.; Macmillan, R. A life course model of self-rated health through adolescence and young adulthood. Soc. Sci. Med. 2012, 75, 1311–1320. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Gyori, D.; Farkas, B.F.; Horvath, L.O.; Komaromy, D.; Meszaros, G.; Szentivanyi, D.; Balazs, J. The Association of Nonsuicidal Self-Injury with Quality of Life and Mental Disorders in Clinical Adolescents-A Network Approach. Int. J. Environ. Res. Public Health 2021, 18, 1840. [Google Scholar] [CrossRef]
- Katz, D.A.; McHorney, C.A. The relationship between insomnia and health-related quality of life in patients with chronic illness. J. Fam. Pract. 2002, 51, 229–235. [Google Scholar]
- Woo, D.; Lee, Y.; Park, S. Associations among working hours, sleep duration, self-rated health, and health-related quality of life in Korean men. Health Qual. Life Outcomes 2020, 18, 287. [Google Scholar] [CrossRef]
- Pano, O.; Sayon-Orea, C.; Gea, A.; Bes-Rastrollo, M.; Martinez-Gonzalez, M.A.; Martinez, J.A. Nutritional Determinants of Quality of Life in a Mediterranean Cohort: The SUN Study. Int. J. Environ. Res. Public Health 2020, 17, 3897. [Google Scholar] [CrossRef]
- Islami, F.; Goding Sauer, A.; Miller, K.D.; Siegel, R.L.; Fedewa, S.A.; Jacobs, E.J.; McCullough, M.L.; Patel, A.V.; Ma, J.; Soerjomataram, I.; et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J. Clin. 2018, 68, 31–54. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Chen, Y.; Long, K.; Kim, E.S.; Trudel-Fitzgerald, C.; Kubzansky, L.D. Positive Epidemiology? Epidemiology 2020, 31, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Fontaine, K.R.; Barofsky, I. Obesity and health-related quality of life. Obes. Rev. 2001, 2, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The RAND 36-Item Health Survey 1.0. Health Econ. 1993, 2, 217–227. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- WHOQOL Group, T. The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [Google Scholar] [CrossRef]
- Sullivan, L.M.; Massaro, J.M.; D’Agostino, R.B., Sr. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat. Med. 2004, 23, 1631–1660. [Google Scholar] [CrossRef]
- Chida, Y.; Steptoe, A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosom. Med. 2008, 70, 741–756. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; McNeely, E.; Koh, H.K. Reimagining Health-Flourishing. JAMA 2019, 321, 1667–1668. [Google Scholar] [CrossRef]
- Vellas, B.; Guigoz, Y.; Garry, P.J.; Nourhashemi, F.; Bennahum, D.; Lauque, S.; Albarede, J.-L. The mini nutritional assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 1999, 15, 116–122. [Google Scholar] [CrossRef]
- Hershey, M.S.; Sotos-Prieto, M.; Ruiz-Canela, M.; Christophi, C.A.; Moffatt, S.; Martinez-Gonzalez, M.A.; Kales, S.N. The Mediterranean lifestyle (MEDLIFE) index and metabolic syndrome in a non-Mediterranean working population. Clin. Nutr. 2021, 40, 2494–2503. [Google Scholar] [CrossRef]
- Hershey, M.S.; Sanchez-Villegas, A.; Sotos-Prieto, M.; Fernandez-Montero, A.; Pano, O.; Lahortiga-Ramos, F.; Martinez-Gonzalez, M.A.; Ruiz-Canela, M. The Mediterranean Lifestyle and the Risk of Depression in Middle-Aged Adults. J. Nutr. 2022, 152, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Pano, O.; Martinez-Lapiscina, E.H.; Sayon-Orea, C.; Martinez-Gonzalez, M.A.; Martinez, J.A.; Sanchez-Villegas, A. Healthy diet, depression and quality of life: A narrative review of biological mechanisms and primary prevention opportunities. World J. Psychiatry 2021, 11, 997–1016. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Xiang, Q.; Yan, C.; Liao, H.; Wang, J. Relationship between chronic diseases and depression: The mediating effect of pain. BMC Psychiatry 2021, 21, 436. [Google Scholar] [CrossRef]
- Hohls, J.K.; Konig, H.H.; Quirke, E.; Hajek, A. Anxiety, Depression and Quality of Life-A Systematic Review of Evidence from Longitudinal Observational Studies. Int. J. Environ. Res. Public Health 2021, 18, 2022. [Google Scholar] [CrossRef]
- Carlos, S.; De La Fuente-Arrillaga, C.; Bes-Rastrollo, M.; Razquin, C.; Rico-Campa, A.; Martinez-Gonzalez, M.A.; Ruiz-Canela, M. Mediterranean Diet and Health Outcomes in the SUN Cohort. Nutrients 2018, 10, 439. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr. SF-36 health survey update. Spine 2000, 25, 3130–3139. [Google Scholar] [CrossRef] [PubMed]
- de Cuevillas, B.; Alvarez Alvarez, I.; Cuervo, M.; Fernandez Montero, A.; Navas Carretero, S.; Martinez, J.A. Definition of nutritionally qualitative categorizing (proto)nutritypes and a pilot quantitative nutrimeter for mirroring nutritional well-being based on a quality of life health related questionnaire. Nutr. Hosp. 2019, 36, 862–874. [Google Scholar] [CrossRef]
- Bes-Rastrollo, M.; Pérez Valdivieso, J.R.; Sánchez-Villegas, A.; Alonso, Á.; Martínez-González, M.Á. Validación del peso e índice de masa corporal auto-declarados de los participantes de una cohorte de graduados universitarios. Rev. Esp. Obes. 2005, 3, 352–358. [Google Scholar]
- Greaney, M.L.; Cohen, S.A.; Blissmer, B.J.; Earp, J.E.; Xu, F. Age-specific trends in health-related quality of life among US adults: Findings from National Health and Nutrition Examination Survey, 2001–2016. Qual. Life Res. 2019, 28, 3249–3257. [Google Scholar] [CrossRef]
- Martinez-Gonzalez, M.A.; Lopez-Fontana, C.; Varo, J.J.; Sanchez-Villegas, A.; Martinez, J.A. Validation of the Spanish version of the physical activity questionnaire used in the Nurses’ Health Study and the Health Professionals’ Follow-up Study. Public Health Nutr. 2005, 8, 920–927. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Girón, P. Is age associated with self-rated health among older people in Spain? Cent. Eur. J. Public Health 2012, 20, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Fluss, R.; Faraggi, D.; Reiser, B. Estimation of the Youden Index and its associated cutoff point. Biom. J. 2005, 47, 458–472. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Bryan, J.; Wilson, C.; Hodgson, J.M.; Davis, C.R.; Murphy, K.J. The Mediterranean Diet and Cognitive Function among Healthy Older Adults in a 6-Month Randomised Controlled Trial: The MedLey Study. Nutrients 2016, 8, 579. [Google Scholar] [CrossRef]
- Kilani, H.A.; Bataineh, M.F.; Al-Nawayseh, A.; Atiyat, K.; Obeid, O.; Abu-Hilal, M.M.; Mansi, T.; Al-Kilani, M.; Al-Kitani, M.; El-Saleh, M.; et al. Healthy lifestyle behaviors are major predictors of mental wellbeing during COVID-19 pandemic confinement: A study on adult Arabs in higher educational institutions. PLoS ONE 2020, 15, e0243524. [Google Scholar] [CrossRef]
- Speer, D.C. Clinically significant change: Jacobson and Truax (1991) revisited. J. Consult Clin. Psychol. 1992, 60, 402–408. [Google Scholar] [CrossRef]
- Cummins, R.A. Subjective Wellbeing, Homeostatically Protected Mood and Depression: A Synthesis. J. Happiness Stud. 2009, 11, 1–17. [Google Scholar] [CrossRef]
- Tomyn, A.J.; Weinberg, M.K.; Cummins, R.A. Intervention Efficacy Among ‘At Risk’ Adolescents: A Test of Subjective Wellbeing Homeostasis Theory. Soc. Indic. Res. 2014, 120, 883–895. [Google Scholar] [CrossRef]
- Mujcic, R.; Oswald, A.J. Evolution of Well-Being and Happiness After Increases in Consumption of Fruit and Vegetables. Am. J. Public Health 2016, 106, 1504–1510. [Google Scholar] [CrossRef]
- Nguyen, B.; Ding, D.; Mihrshahi, S. Fruit and vegetable consumption and psychological distress: Cross-sectional and longitudinal analyses based on a large Australian sample. BMJ Open 2017, 7, e014201. [Google Scholar] [CrossRef] [PubMed]
- Sayon-Orea, C.; Razquin, C.; Bullo, M.; Corella, D.; Fito, M.; Romaguera, D.; Vioque, J.; Alonso-Gomez, A.M.; Warnberg, J.; Martinez, J.A.; et al. Effect of a Nutritional and Behavioral Intervention on Energy-Reduced Mediterranean Diet Adherence Among Patients With Metabolic Syndrome: Interim Analysis of the PREDIMED-Plus Randomized Clinical Trial. JAMA 2019, 322, 1486–1499. [Google Scholar] [CrossRef] [PubMed]
- Oftedal, S.; Kolt, G.S.; Holliday, E.G.; Stamatakis, E.; Vandelanotte, C.; Brown, W.J.; Duncan, M.J. Associations of health-behavior patterns, mental health and self-rated health. Prev. Med. 2019, 118, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Ruano, C.; Henriquez, P.; Martinez-Gonzalez, M.A.; Bes-Rastrollo, M.; Ruiz-Canela, M.; Sanchez-Villegas, A. Empirically derived dietary patterns and health-related quality of life in the SUN project. PLoS ONE 2013, 8, e61490. [Google Scholar] [CrossRef]
- Assaf, A.R.; Beresford, S.A.A.; Risica, P.M.; Aragaki, A.; Brunner, R.L.; Bowen, D.J.; Naughton, M.; Rosal, M.C.; Snetselaar, L.; Wenger, N. Low-Fat Dietary Pattern Intervention and Health-Related Quality of Life: The Women’s Health Initiative Randomized Controlled Dietary Modification Trial. J. Acad. Nutr. Diet 2016, 116, 259–271. [Google Scholar] [CrossRef]
- Selenius, J.S.; Wasenius, N.S.; Kautiainen, H.; Salonen, M.; von Bonsdorff, M.; Eriksson, J.G. Impaired glucose regulation, depressive symptoms, and health-related quality of life. BMJ Open Diabetes Res. Care 2020, 8, e001568. [Google Scholar] [CrossRef]
- Poll, F.A.; Miraglia, F.; D’Avila, H.F.; Reuter, C.P.; Mello, E.D. Impact of intervention on nutritional status, consumption of processed foods, and quality of life of adolescents with excess weight. J. Pediatr. 2020, 96, 621–629. [Google Scholar] [CrossRef]
- Sari, S.; Bilberg, R.; Sogaard Nielsen, A.; Roessler, K.K. The effect of exercise as adjunctive treatment on quality of life for individuals with alcohol use disorders: A randomized controlled trial. BMC Public Health 2019, 19, 727. [Google Scholar] [CrossRef]
- Boberska, M.; Szczuka, Z.; Kruk, M.; Knoll, N.; Keller, J.; Hohl, D.H.; Luszczynska, A. Sedentary behaviours and health-related quality of life. A systematic review and meta-analysis. Health Psychol. Rev. 2018, 12, 195–210. [Google Scholar] [CrossRef]
- Gu, J.; Chao, J.; Chen, W.; Xu, H.; Zhang, R.; He, T.; Deng, L. Multimorbidity and health-related quality of life among the community-dwelling elderly: A longitudinal study. Arch. Gerontol. Geriatr. 2018, 74, 133–140. [Google Scholar] [CrossRef]
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Res. Rev. 2019, 53, 100903. [Google Scholar] [CrossRef] [PubMed]
- Cepeda Marte, J.L.; Ruiz-Matuk, C.; Mota, M.; Perez, S.; Recio, N.; Hernandez, D.; Fernandez, J.; Porto, J.; Ramos, A. Quality of life and metabolic control in type 2 diabetes mellitus diagnosed individuals. Diabetes Metab. Syndr. 2019, 13, 2827–2832. [Google Scholar] [CrossRef] [PubMed]
- Lash, T.L.; VanderWeele, T.J.; Heaneause, S.; Rothman, K. Modern Epidemiology, 4th ed.; Wolters Kluwer Health: Waltham, MA, USA, 2021. [Google Scholar]
- Bao, Y.; Bertoia, M.L.; Lenart, E.B.; Stampfer, M.J.; Willett, W.C.; Speizer, F.E.; Chavarro, J.E. Origin, Methods, and Evolution of the Three Nurses’ Health Studies. Am. J. Public Health 2016, 106, 1573–1581. [Google Scholar] [CrossRef] [PubMed]
- Rimm, E.B.; Stampfer, M.J.; Colditz, G.A.; Giovannucci, E.; Willett, W.C. Effectiveness of various mailing strategies among nonrespondents in a prospective cohort study. Am. J. Epidemiol. 1990, 131, 1068–1071. [Google Scholar] [CrossRef]


| Characteristics | Total (n = 15,168) | Poor SPH (n = 803) | Transition SPH (n = 12,919) | Excellent SPH (n = 1446) | p-Value |
|---|---|---|---|---|---|
| Female Sex (%) | 59.8 | 58.9 | 59.8 | 60.0 | 0.805 |
| Age (years) | 38.4 (12.0) | 44.3 (13.2) | 38.5 (11.9) | 34.4 (10.9) | <0.001 |
| BMI (kg/m2) | 23.5 (3.5) | 24.7 (4.2) | 23.6 (3.5) | 22.7 (3.0) | <0.001 |
| Underweight (<18.5 kg/m2; %) | 3.7 | 3.7 | 3.5 | 5.4 | <0.001 |
| Normal weight (18.5–24.9 kg/m2; %) | 66.3 | 55.0 | 66.1 | 74.1 | |
| Overweight (25.0–29.9 kg/m2; %) | 25.4 | 31.3 | 25.8 | 18.4 | |
| Obesity (>30.0 kg/m2; %) | 4.6 | 10.0 | 4.6 | 2.1 | |
| Smoking status (%) | <0.001 | ||||
| Never | 49.3 | 38.9 | 48.9 | 58.8 | |
| Current | 21.2 | 23.0 | 21.5 | 18.0 | |
| Former | 29.5 | 38.1 | 29.6 | 23.2 | |
| Family history of diseases a (%) | <0.001 | ||||
| 0 | 36.0 | 26.5 | 35.7 | 44.0 | |
| 1 | 43.7 | 42.7 | 44.0 | 41.4 | |
| 2 | 20.3 | 30.8 | 20.3 | 14.7 | |
| Pre-existing diseases b (%) | <0.001 | ||||
| 0 | 75.0 | 59.0 | 74.7 | 86.7 | |
| 1 | 19.9 | 25.3 | 20.4 | 12.4 | |
| 2 | 4.6 | 13.3 | 4.5 | 0.8 | |
| 3 | 0.5 | 2.4 | 0.4 | 0.1 | |
| Insomnia (%) | <0.001 | ||||
| Never | 34.1 | 15.2 | 33.6 | 48.8 | |
| Rarely | 47.4 | 46.3 | 48.4 | 39.2 | |
| Yes | 18.5 | 38.5 | 18.0 | 12.0 | |
| Physical activity (METs-h/week) | 21.7 (22.7) | 18.5 (20.7) | 21.3 (22.0) | 27.4 (27.7) | <0.001 |
| Fruits + vegetables (serv/day) | 4.7 (2.8) | 4.7 (3.0) | 4.7 (2.8) | 4.7 (2.7) | 0.789 |
| Added sugars c (total servings) | <0.001 | ||||
| None | 5.4 | 7.3 | 5.4 | 4.5 | |
| <1/day | 91.8 | 87.7 | 91.9 | 93.3 | |
| >1/day | 2.8 | 5.0 | 2.7 | 2.1 | |
| SF-36 score | 82.1 (12.6) | 56.7 (16.8) | 82.7 (10.7) | 90.9 (6.9) | <0.001 |
| SF-33 score | 82.1 (12.7) | 56.8 (19.9) | 82.7 (10.8) | 90.7 (6.9) | <0.001 |
| LWB-I Items | Beta Coefficient (β) | Lower Bound | Upper Bound | p-Value |
|---|---|---|---|---|
| Sex (female vs. male) | −1.13 | −1.47 | −0.78 | <0.001 |
| Age (for each year) | −0.04 | −0.05 | −0.02 | <0.001 |
| BMI category a | ||||
| Underweight (<18.5 kg/m2) | 0.05 | −0.74 | 0.83 | 0.911 |
| Normal (18.5–24.9 kg/m2) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Overweight (25.0–29.9 kg/m2) | −0.64 | −1.01 | −0.27 | 0.002 |
| Obesity (>30.0 kg/m2) | −2.03 | −2.75 | −1.30 | <0.001 |
| Smoking status | ||||
| Never | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Current | −0.86 | −1.24 | −0.48 | <0.001 |
| Former | −0.56 | −0.91 | −0.20 | 0.002 |
| Family History of Disease b | ||||
| 0 | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| 1 | −0.14 | −0.47 | 0.19 | 0.420 |
| 2 | −0.45 | −0.86 | −0.03 | 0.035 |
| Number of Pre-existing Diseases | ||||
| 0 | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| 1 | −0.68 | −1.07 | −0.30 | 0.001 |
| 2 | −2.39 | −3.12 | −1.65 | <0.001 |
| 3 | −4.11 | −6.20 | −2.02 | <0.001 |
| Insomnia | ||||
| Never | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Rarely | −1.48 | −1.81 | −1.15 | <0.001 |
| Yes, currently, or in the past | −3.46 | −3.90 | −3.03 | <0.001 |
| Physical Activity | ||||
| Below recommendations c | −0.58 | −0.90 | −0.27 | <0.001 |
| Recommended c | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Above recommendations c | 0.05 | −0.47 | 0.57 | 0.843 |
| Fruits + vegetables (for each serv./d) | 0.07 | 0.01 | 0.12 | 0.017 |
| Sugary products d (serv./d) | ||||
| None | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Less than 1 | −0.32 | −0.97 | 0.34 | 0.343 |
| More than 1 | −1.45 | −2.53 | −0.38 | 0.008 |
| Have you felt downhearted and blue? (Item 28, SF-36) | ||||
| All of the time | −20.45 | −23.53 | −17.37 | <0.001 |
| Most of the time | −26.22 | −28.10 | −24.35 | <0.001 |
| A good bit of time | −21.07 | −21.94 | −20.20 | <0.001 |
| Some of the time | −10.85 | −11.3 | −10.38 | <0.001 |
| A little of the time | −3.53 | −3.87 | −3.20 | <0.001 |
| None of the time | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Did you feel tired? (Item 31, SF-36) | ||||
| All of the time | −25.37 | −27.46 | −23.28 | <0.001 |
| Most of the time | −23.39 | −24.52 | −22.25 | <0.001 |
| A good bit of time | −13.83 | −14.58 | −13.09 | <0.001 |
| Some of the time | −7.65 | −8.32 | −6.99 | <0.001 |
| A little of the time | −3.36 | −4.02 | −2.71 | <0.001 |
| None of the time | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) | 0 (Ref.) |
| Constant | 98.11 | 96.97 | 99.24 | <0.001 |
| Lower Cut-off | |||
| AUC (CI: 95%) a | 0.80 (0.79, 0.82) | ||
| Method | Proposed Cut-off | Sensitivity (%) | Specificity (%) |
| Jacobson-Traux formula | 77.9 | 69.0 | 77.3 |
| Youden index | 80.7 | 77.8 | 70.3 |
| Exploratory * | 80.0 | 75.7 | 72.3 |
| Exploratory b | 81.0 | 78.6 | 69.2 |
| Upper Cut-off | |||
| AUC (CI: 95%) a | 0.67 (0.66, 0.69) | ||
| Method | Proposed Cut-off | Sensitivity (%) | Specificity (%) |
| Jacobson-Traux formula | 84.3 | 71.0 | 52.9 |
| Youden index | 86.0 | 61.6 | 63.1 |
| Exploratory * | 85.0 | 66.1 | 56.9 |
| Exploratory b | 86.0 | 61.4 | 63.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pano, O.; Sayón-Orea, C.; Hershey, M.S.; Bes-Rastrollo, M.; Martínez-González, M.A.; Martínez, J.A. Development of a General Health Score Based on 12 Objective Metabolic and Lifestyle Items: The Lifestyle and Well-Being Index. Healthcare 2022, 10, 1088. https://doi.org/10.3390/healthcare10061088
Pano O, Sayón-Orea C, Hershey MS, Bes-Rastrollo M, Martínez-González MA, Martínez JA. Development of a General Health Score Based on 12 Objective Metabolic and Lifestyle Items: The Lifestyle and Well-Being Index. Healthcare. 2022; 10(6):1088. https://doi.org/10.3390/healthcare10061088
Chicago/Turabian StylePano, Octavio, Carmen Sayón-Orea, María Soledad Hershey, Maira Bes-Rastrollo, Miguel A. Martínez-González, and J. Alfredo Martínez. 2022. "Development of a General Health Score Based on 12 Objective Metabolic and Lifestyle Items: The Lifestyle and Well-Being Index" Healthcare 10, no. 6: 1088. https://doi.org/10.3390/healthcare10061088
APA StylePano, O., Sayón-Orea, C., Hershey, M. S., Bes-Rastrollo, M., Martínez-González, M. A., & Martínez, J. A. (2022). Development of a General Health Score Based on 12 Objective Metabolic and Lifestyle Items: The Lifestyle and Well-Being Index. Healthcare, 10(6), 1088. https://doi.org/10.3390/healthcare10061088







