Abstract
Background: Lateral elbow pain (LEP) represents a musculoskeletal disorder affecting the epicondyloid region of the elbow. The terminological framework of this problem in literature, to date, is confusing. This systematic review (SR) aims to analyse the panorama of the scientific literature concerning the pathogenetic framework, treatment, and clinical diagnosis of LEP. Methods: We conducted an SR according to the guidelines of the PRISMA statement. We performed research using the electronic Medline, Epistemonikos, and Cochrane Library databases. The research started on 12 January 2022 and finished on 30 April 2022. We included all systematic reviews and meta-analyses published, in English, between 1989 and 2022. The articles’ selection was based on critical appraisal using Amstar 2. In the selected reviews we obtained the etiopathogenic terminology used to describe the symptoms, treatment, and diagnostic criteria of LEP. Results: Twenty-five SRs met the eligibility criteria and were included in the study. From these SRs, 227 RCT articles were analysed and different treatments proposals were extracted, such as exercise, manipulation corticosteroid injection, and surgery. In the selected articles, 10 different terms emerged to describe LEP and 12 different clinical tests. The most common treatments detected in this SR were a conservative multimodal approach (e.g., eccentric exercises, manual therapy, acupuncture, ultrasound), then surgery or other invasive treatments (e.g., corticosteroid injection, tenotomy). The most common term detected in this SR was “lateral epicondylitis” (n = 95, 51.6%), followed by “tennis elbow” (n = 51, 28.1%) and “lateral epicondylalgia” (n = 18, 9.4%). Among the diagnostic tests were painful palpation (n = 101, 46.8%), the Cozen test (n = 91, 42.1%), the pain-free grip-strength test (n = 41, 19.0%), and the Maudsley test (n = 48, 22.2%). A total of 43.1% of RCTs (n = 96) included subjects with LEP > 3 months, 40.2% (n = 85) included patients with LEP < 3 months, and 16.7% of the items (n = 35) were not specified by the inclusion criteria on the onset of symptoms. Conclusions: In this SR, a considerable terminological heterogeneity emerged in the description of LEP, associated with the lack of clear and recognised diagnostic criteria in evaluating and treating patients with lateral elbow pain.
1. Introduction
Lateral elbow pain (LEP) represents a musculoskeletal condition, between musculoskeletal disorders (MSDs), affecting the epicondyloid region of the elbow [1,2]. It mainly affects workers between 35 and 54 years of age, with a prevalence of between 1% and 3%. The incidence in general practice is about 4–7 people per 1000 patients per year, producing a heavy economic burden due to loss of productivity, high costs for access to care services, and the impossibility of carrying out one’s work, which can last for several weeks [3,4].
Repetitive movements of flexion–extension and prone–supination of the elbow, lifting of heavy loads, and frequent extensions of the wrist against resistance contribute to the onset of this pathology, leading the person to reduced participation in daily life activities [5,6].
The management of lateral elbow pain has been a real challenge for clinicians and researchers for years, although several studies have been produced over the years on the treatment and mechanisms of this condition [7]. Several conservative treatments have been proposed, such as eccentric exercise and manual therapy. Corticosteroid infiltrations and platelet-rich plasma (PRP) showed efficacy in the short term but led to worse long-term results when compared to exercise [7].
Despite the high number of studies in the literature, LEP is a very recurrent pathology to date: One out of three people, after 12 months, still complained of painful and disabling symptoms despite rehabilitative treatment, and up to 5% of patients considered surgery [7,8].
These data suggest investigating the aetiology, diagnosis, and treatment of this musculoskeletal disorder to improve its clinical management.
In the literature, to date, the terminological framework of this problem is confusing. Indeed, researchers adopted more than 10 names (i.e., lateral elbow tendinopathy, lateral epicondylitis, tennis elbow, lateral epicondylalgia, lateral epicondylosis) to define LEP [9,10,11].
A tendon-centred etiological and diagnostic framework was perceived for the term “lateral elbow tendinopathy” (LET) [9,10].
The diagnosis of LET is based on an accurate medical history and the administration of specific tests to provoke the patient’s symptoms. For a correct differential diagnosis, clinicians should exploit imaging like ultrasound (US) and magnetic resonance imaging (MRI) [7,12].
However, in the literature, no reliable and validated test cluster allows for the identification and categorization of subjects with LEP to set up an effective therapeutic plan and reduce failures [8,13].
Only one primary study, with limited sample size, analysed the diagnostic accuracy of the Cozen and Maudsley tests, the two most commonly used provocative tests in diagnosing lateral elbow pain [8].
Coombes et al. [7], in 2015, were the first authors to propose a preliminary algorithm to guide clinicians in identifying different subgroups of patients with LEP and facilitate the decision-making process regarding the treatment choice. The subgrouping of patients with LEP was based on the analysis of prognostic factors (i.e., the severity of pain, disability, the presence of central sensitisation, neuromuscular impairments) and specific self-assessment questionnaires.
Numerous systematic reviews (SR) of LEP have been produced in recent years but none focus precisely on diagnostic labels and specific tests. The main goal is to “tidy up” this widespread and disabling condition to identify in future valuable tools to create a precise and reliable algorithm for the management of subjects with LEP, and moreover, to clarify whether the current terminologies used are accurate. An overview of SR represents a logical next step to provide decision-makers in healthcare and summarize the results generated by the SRs relating to a given topic [14].
This overview of SRs analyses the panorama of the scientific literature concerning the pathogenetic framework, the clinical diagnosis, and treatments of LEP. In particular, we considered the inclusion criteria and clinical tests used to identify patients with LEP within the studies and the terminology adopted to describe the symptomatology.
In light of what has been described in the literature to date, it would be appropriate for the authors to propose an “umbrella” term that includes different clinical pictures attributable to LEP and embraces the terminology, classification, and management.
In this umbrella term, specific subgroups of patients with lateral elbow pain should be considered, for which it would be helpful to propose the use of more current diagnostic tools for a clinical setting that helps to more carefully determine, where possible, the structure predominantly involved in the development of signs and symptoms, and define therapeutic paths according to different prognoses, capable of guiding clinicians towards more appropriate treatments for the patient, taking into account their relative impact on psycho-social aspects.
2. Methods
This overview of SRs was prospectively registered in PROSPERO (CRD42021266790) [15].
2.1. Study Design
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol was used to design and report the present SR of SRs [16].
Moreover, due to the overviews of systematic reviews being relatively new approaches to synthesising evidence, the methods were described in the literature, and relevant research was used to plan the present overview [15].
2.2. Purpose of the Study
The following question was defined: “What are the most commonly used treatments, etiopathogenetic terminologies, and diagnostic criteria adopted to identify patients with LEP?”
2.3. Search Strategy
We performed research on the three main electronic databases for systematic reviews: Medline (1996–2021), the Epistemonikos Database (2009–2021), and Cochrane Library (1996–2021).
The keywords used for the purposes of the research were: “tennis elbow” (MeSH terms), “lateral epicondylitis,” “lateral elbow tendinopathy,” and “lateral epicondylalgia.” The Boolean operator OR allowed for the selection of most of the target SR. PubMed Clinical Queries was used on PubMed Central as a tool to enter the query string and select the systematic reviews and the meta-analysis on the topic.
This step was finally completed and integrated with manual research of the bibliographic references. The research started on 12 January 2022 and ended on 31 January 2022.
We have reported the complete search strategies in Appendix A.
2.4. Eligibility Criteria
We included articles according to the following criteria: (a) published from 1989 to 2022, (b) written in English, (c) relating to the diagnosis and treatment (conservative and surgical) of LEP, (d) defined one or more terms of classification of LEP, and (e) reported a study design as SR with or without metanalysis (MA).
We excluded articles published before 1989. RCTs, scoping reviews, literature reviews, and case studies were not included in our SR. Studies that were not exclusively about LEP were excluded.
2.5. Study Selection
Two reviewers (SV and DP) performed the selection and data collection process under the supervision of a third author (FM). First, all records were screened by the management software for Rayyan systematic reviews (https://rayyan.qcri.org, accessed on 14 January 2022), whereas references were managed by the Mendeley software (https://www.mendeley.com, accessed on 31 January 2022). Then, after removing the duplicates, the titles and abstracts were screened. Lastly, full texts of the identified studies were obtained for further assessment and analysed independently according to the eligibility criteria by two reviewers (S.V. and D.P.). Where appropriate, the authors were contacted in order to obtain the full text.
The language did not pose any barrier to the analysis of the articles, and a native US translator was consulted when necessary.
2.6. Data Collection
For each SR, the following data were extracted: study design (SR o SR with MA); author, year of publication; the number and characteristics of participants/populations; treatments; definition and/or any diagnostic criteria for LEP (e.g., specific diagnostic test or a diagnostic cluster); analysis of the variables and the outcome of the studies; and study settings/country.
Overlapping of RCTs within each SR was considered to avoid entering study data twice in the data analysis, as suggested from other overviews of SRs [15].
2.7. Quality Assessment
Furthermore, to make sure no methodological low-quality publications were included, only systematic reviews or metanalyses were selected through AMSTAR II (Assessing the Methodological Quality of Systematic Reviews) [17] and then analysed with the RoBis tool (Risk of Bias in Systematic Reviews) [18].
Although AMSTAR 2 is not aimed at generating an overall score cut-off, to judge the quality of the SRs, it recommends defining critical items, which helps identify any weaknesses in these items to make an overall assessment of the reliability of the results of the selected SRs. All SRs that received a low or very low overall rating (one point or more of a critical point) were excluded [17].
AMSTAR II is the most widely used SR assessment tool but focuses on the overall critical assessment of reviews and does not analyse the risk of bias in the systematic review. RoBis’s approach aligns with the most recent methods used to develop the risk of bias assessment tools and promises to improve the assessment process in the overview and guidelines. A recent study evaluated the interrater reliability (IRR) of AMSTAR II and RoBis in judging individual domains and the general methodological quality/risk of bias of systematic reviews, the concurrent validity of the instruments, and the time needed to apply them. The results showed that AMSTAR II and RoBis have overlapping IRRs, though they are different in construction and applicability [19].
According to the specific study design, the risk of bias (RoB) of the included studies was analysed using the RoBis tool [18]. The RoBis tool was used by two independent reviewers (S.V. and L.D.F.) to assess the risk of bias in selected SRs. All the studies included RCTs of a methodologically medium–high quality level that considered subjects displaying unilateral LEP. The score of the RoBis was not adopted as a criterion to include or exclude studies in this SR.
2.8. Agreement
Cohen’s Kappa (K) was used to assess the interrater agreement between the two authors (S.V., D.P.) for full-text selection (K = 0.78; 0.61–0.80 IC 95%). Cohens’ K was interpreted according to Altman’s definition: k < 0.20 poor; 0.20 < k < 0.40 fair; 0.41 < k < 0.60 moderate; 0.61 < k < 0.80 good; and 0.81 < k < 1.00 excellent [20].
2.9. Data Analysis
A standardized set of data was extracted for the selected SRs. Data collected included study design, sample characteristics, inclusion/exclusion criteria, participants, number of RCTs included, intervention, outcome, risk of bias, limits, and author’s conclusion. In addition, the terminology used to describe LEP was extracted from the studies.
A statistician implemented statistical data elaboration by using Excel© (Microsoft, Washington, DC, USA, 2019) calculation sheets.
Data related to the internal and external validity of each selected study were also retrieved based on the RoBis criteria for quality assessment purposes.
3. Results
3.1. Study Selection Process
Electronic database searches yielded 118 SRs and 26 MAs about LEP.
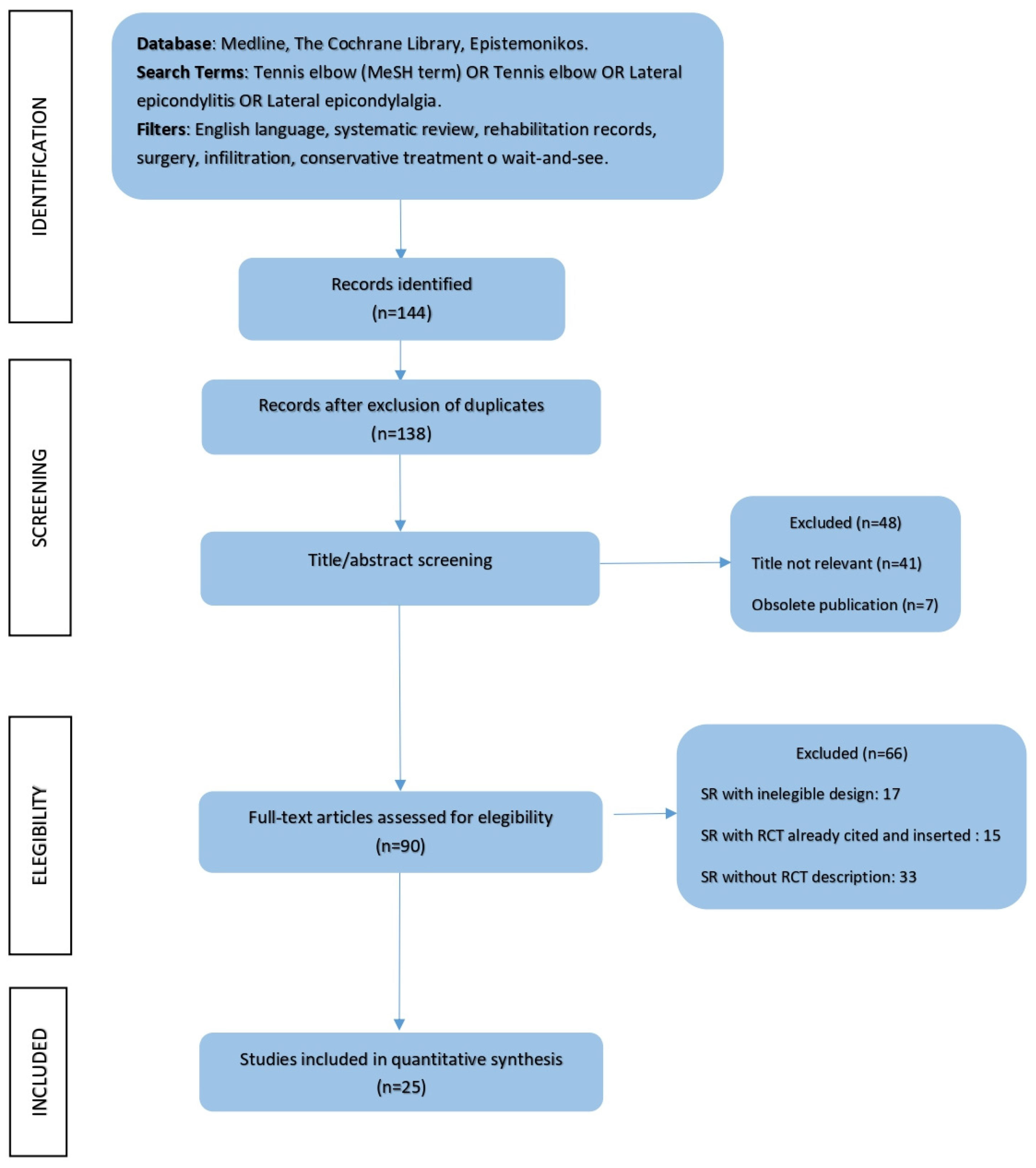
After leaving out six duplicates, the articles underwent screening of pertinence according to the title and the abstract. Forty-eight articles were eliminated due to non-pertinence to the topic title.
The 90 remaining full texts were analysed and underwent eligibility criteria of the AMSTAR 2 checklist [17]. Sixty-six articles were left out because the authors did not adequately describe the included studies (setting study and research design). The systematic reviews that did not provide a detailed description of the studies’ selection and the included criteria were not considered. The full-text analysis was carried out by two not-blinded editors (S.V. and D.P.); for further counsel, a third editor (L.D.F.) was asked for advice (Figure 1).
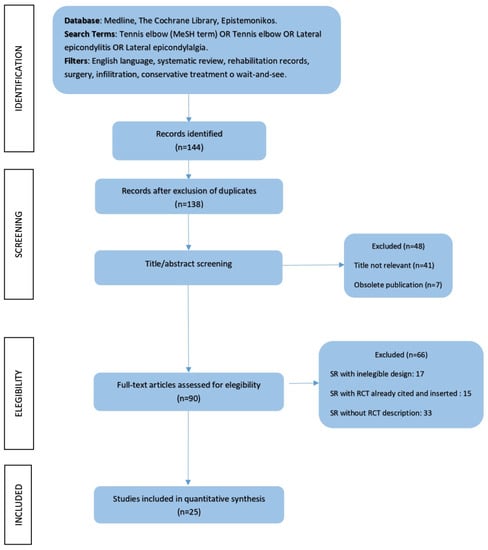
Figure 1.
PRISMA flow diagram summarising the study selection process [16].
The research and the following selection of the studies led to the inclusion of 19 SRs and 6 SRs with MAs for 25 selected articles (Table 1).

Table 1.
Data extraction.
3.2. Characteristics of Treatment and Patients
Within the included SRs, a range of the most used clinical treatment strategies in the case of LEP was analysed, among which were ultrasound therapy, the use of splints, acupuncture, extracorporeal shockwave therapy (ESWT), manipulations, low-level laser therapy (LLLT), therapeutic exercise, dry needling, surgery, PRP, corticosteroid injections, and the use of nonsteroidal anti-inflammatory drugs (NSAIDs). Two hundred sixteen RCTs of the respective SRs were examined. All the selected studies were approved by the ethical committee and the participants’ written informed consent was obtained. One of the 24 SRs analysed the efficacy of ultrasounds to treat LEP and comprised four RCTs [21]. Two reviews dealt with the use of splints in the case of elbow pain [22,24], whereas a 2004 Cochrane SR studied the effects of ESWT [26]. A 2004 review [31] analysed the efficacy of LLLT, and three SRs gathered the RCTs on therapeutic exercise [25,34,37,45]. Acupuncture in LEP treatment was studied in three SRs, including 16 RCTs of good methodological quality [23,38,40]. Two SRs collected RCTs that assessed the efficacy of manipulations in the case of LEP [27,42]. Within seven SRs, the authors pointed out a reduction of symptoms in subjects affected by LEP thanks to cortisone, botulinum, PRP injection, or the intake of NSAIDs [29,30,32,35,39,43]. Two SRs studied the most resolutive surgery techniques for LEP [33,41]. One study analysed the effect of trigger-point dry needling in subjects with LEP [44].
A total of over 20,000 patients were involved in the 227 RCTs analysed in this SR. For each study, the data linked to the terminology used to define the LEP and the inclusion criteria of the subjects were collected (symptom inception and clinical diagnostic tests). Details of the treatments and terminology adopted are described in Table 2.

Table 2.
Treatments and terminology used to define LEP.
3.3. Characteristics of the Included Studies
The oldest SR dated back to 1999 and analysed the effectiveness of US in LEP; the most recent SR was published in 2021 and collected the RCTs concerning the effectiveness of trigger-point dry needling in LEP [21,45]. The study by Bisset et al. collected the largest number of RCTs (24) and presented the largest number of selected subjects (1760) [27]. Butchbinder’s SR on the effectiveness of ESWT in the treatment of LEP selected only two high-quality RCTs [26].
Of 25 SRs, nine articles were related to a surgical or pharmacological approach (NSAIDs, corticosteroids, or PRP) in the case of LEP [28,29,30,32,33,35,36,39,43].
3.4. Risk of Bias of the Included Studies
Details of the RoBis of the included studies are presented in Table 3. Most items of the RoBis assessment tools used for the quality assessment were rated as low risk. Six SRs showed a low risk of bias in the items concerning the eligibility criteria, selection of studies, data collection, study appraisal, and synthesis [22,23,27,33,38,42]. Some SRs did not clearly describe the eligibility criteria based on the study characteristics and sources of information [26,30,37,39,43]. Items related to a low risk of bias in the selection of studies were lacking in seven SRs; in particular, problems were found concerning the research strategy used and the selection criteria [24,27,34,35,36,39,42]. Moreover, in four studies the item about the data collection and study appraisal was not completely described or had biases of assessment [26,29,37,41]. Synthesis and findings were evaluated. A high risk of bias in the synthesis and findings process was recorded in nine SRs, particularly in the presentation of the results and in the analysis of the selected studies [21,24,25,28,31,34,36,40,41,45].

Table 3.
RoBis, risk of bias for systematic reviews [18].
3.5. Summary of Findings
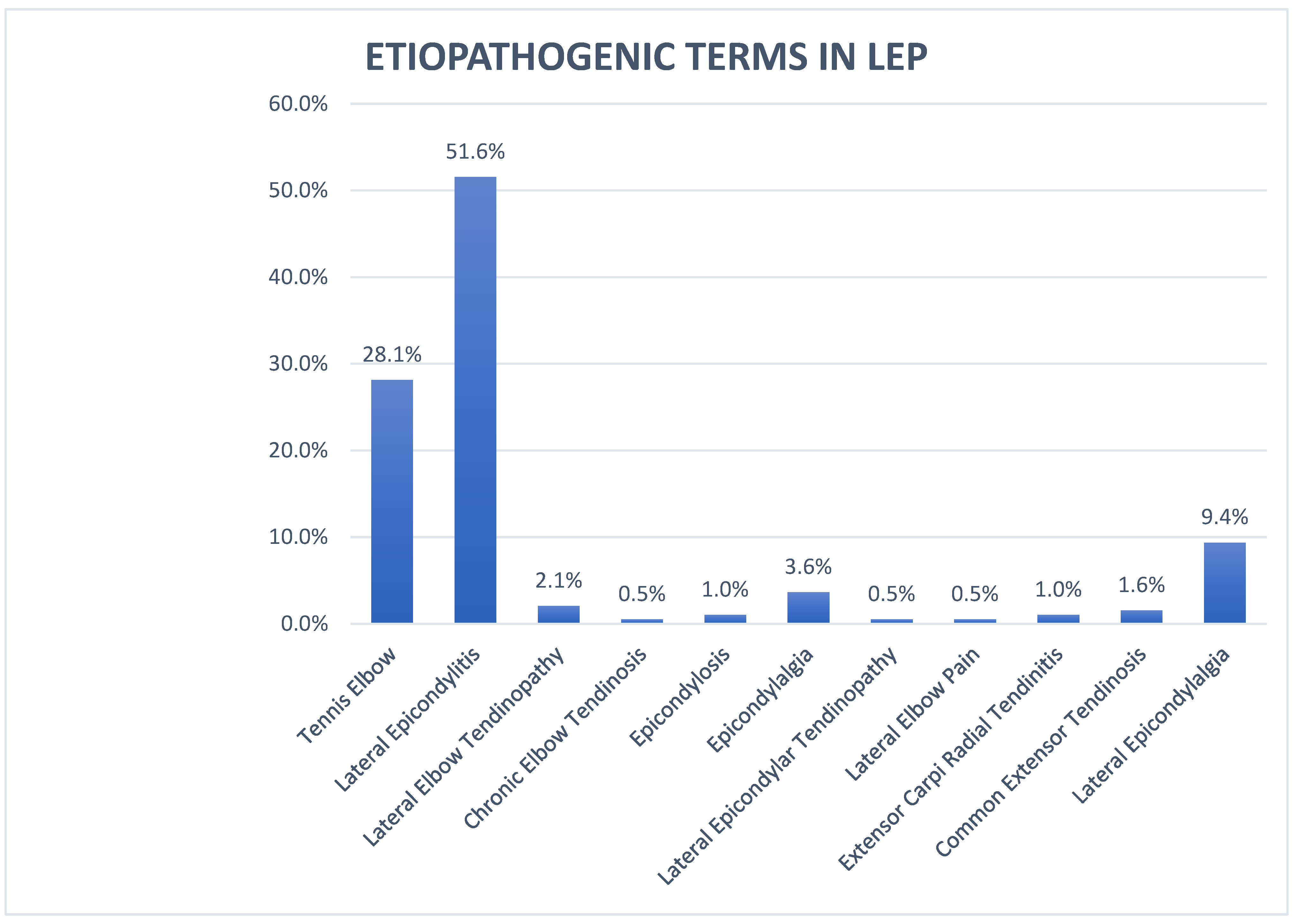
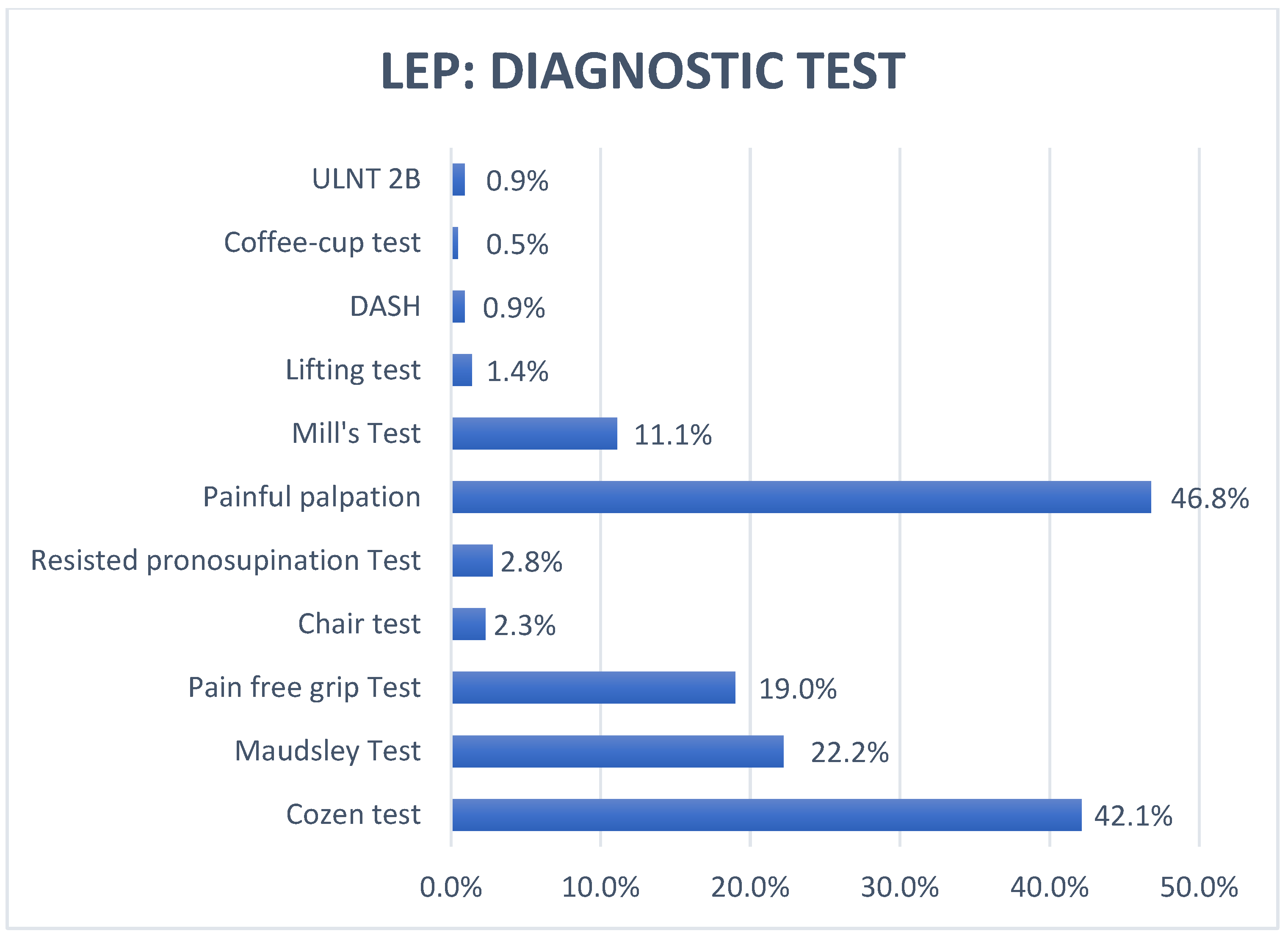
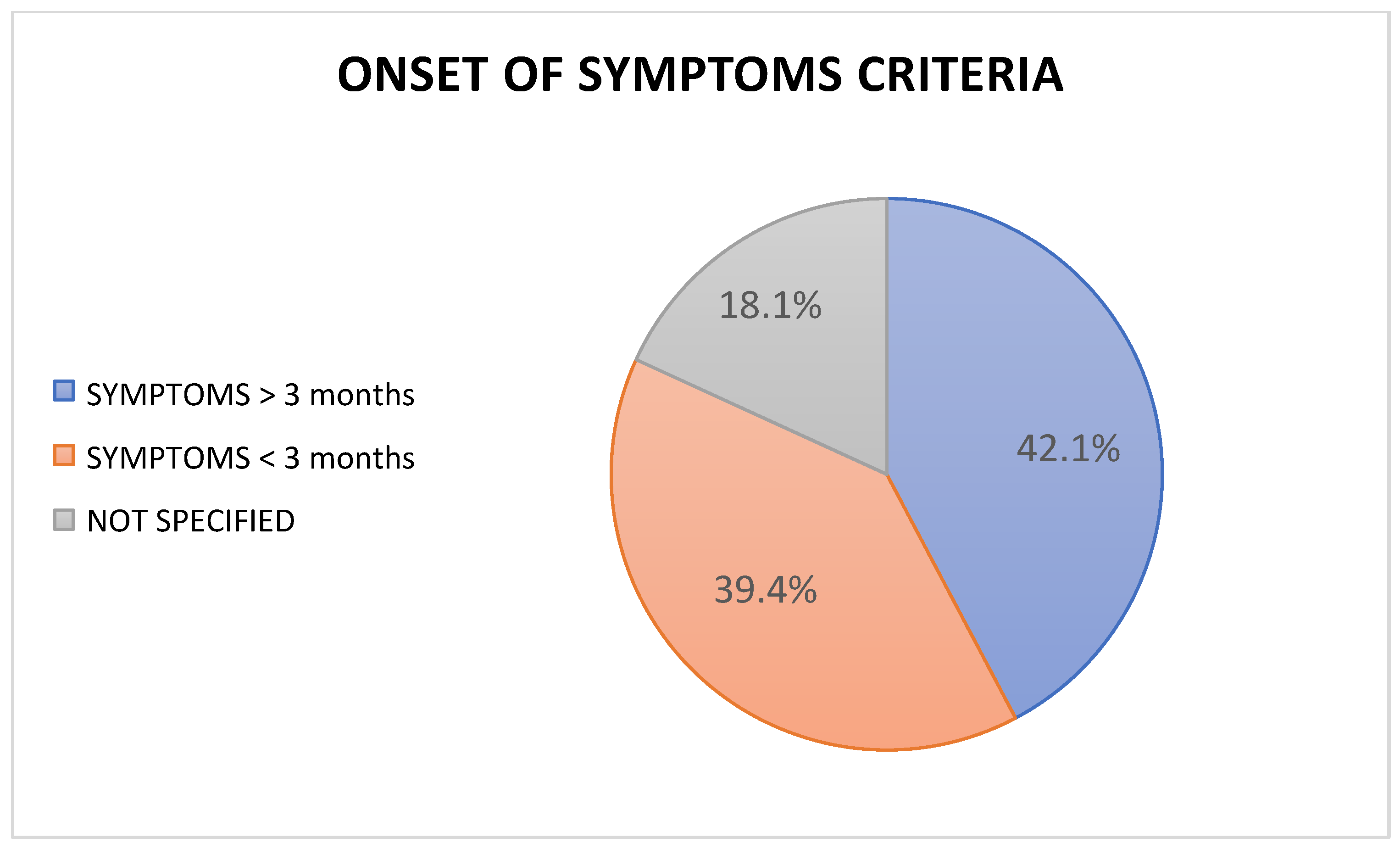
Results concerning the terminology, diagnostic test, and onset criteria of symptoms used in the selected articles are reported in Figure 2, Figure 3, and Figure 4.
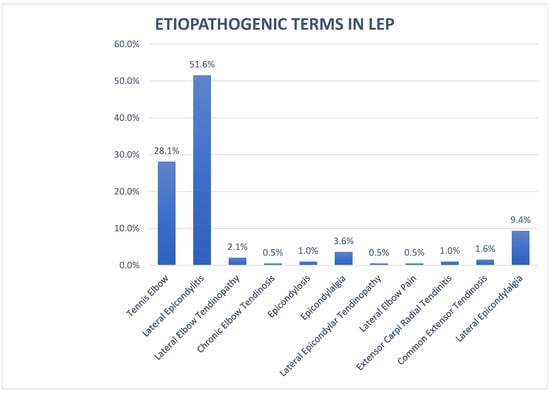
Figure 2.
Terminology for lateral elbow pain (LEP); legend: LEP—lateral elbow pain.
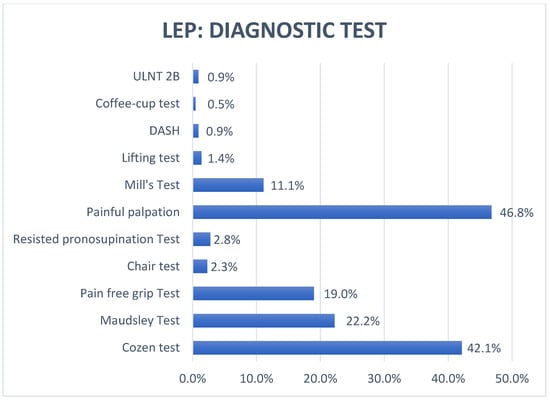
Figure 3.
Diagnostic test in lateral elbow pain (LEP); legend: ULNT—upper limp neural test; DASH—Disabilities of the Arm, Shoulder, and Hand; LEP—lateral elbow pain.
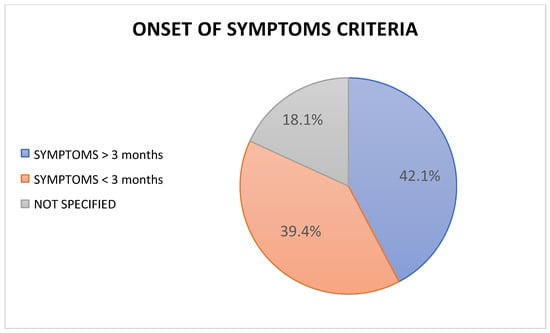
Figure 4.
Onset of symptom criteria for LEP reported in the selected studies.
3.6. Etiopathogenetic Terms in LEP
In the 25 SRs the symptomatology was described through the terms “tennis elbow”, “lateral epicondylitis”, “lateral elbow pain”, “lateral elbow tendinopathy”, “lateral epicondylalgia”, “epicondylosis” and “epicondilopathy” [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
In the 227 RCTs collected through the selection of the 24 SRs, 11 different terms were recorded describing the same LEP clinical condition. The most used term was “lateral epicondylitis” (51.6%), followed by “tennis elbow” (28.1%) and “lateral epicondylalgia” (9.4%). Further terms used to define LEP from an etiopathological point of view were “epicondylalgia” (3.6%), “epicondylosis” (1.0%) “lateral elbow tendinopathy” (2.1%), “chronic elbow tendinosis” (0.5%), “common extensor tendinosis” (1.6%), “lateral epicondylar tendinopathy” (0.5%), “extensor carpi radial tendinitis” (1.0%), and “lateral elbow pain” (0.5%) [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
Ninety-nine out of 227 articles used the term “lateral epicondylitis,” whereas 56 RCTs talked about “tennis elbow” and 18 about “lateral epicondylalgia.” Only one of the selected articles described the symptomatology as “lateral elbow pain” [33].
3.7. Including Criteria in LEP
Inclusion criteria of the subjects affected by LEP in the RCTs in the 25 SRs were examined. Painful palpation of the epicondyle turned out to be the most used clinical way to diagnose LEP (46.8%); however, more than half of the articles did not take it into account [24,25,27,29,30,31,34,35,36,43,44,45]. Considering the 227 RCTs, the Cozen test was one of the most recurring provocation tests in the literature (42.1%), whereas the Maudsley test appeared in 48 RCTs (22,2%). In 43 selected articles, the Cozen test was not combined with the Maudsley test to diagnose the presence of LEP [21,25,27,28,29,30,31,32,33,36,37,38,39,40,41,42,43]. The pain-free grip-strength test (PFGST) was used in 19% of the articles, meaning that this test was not considered throughout the diagnostic process in 168 out of 227 articles [21,22,24,25,26,27,28,29,31,33,34,35,36,37,38,41,45]. The Mill’s test was mentioned in 11.1% of the RCTs and was always combined with at least one other provocation test [21,26,28,30,31,32,34,36,37,38,39,42,43,44,45]. Further provocation tests were identified, among which were the chair test (2.3%), the resisted pronosupination test (2.8%), the lifting test (0.9%), and the coffee-cup test (0.3%). Two articles (1%) integrated the DASH scale (Disabilities of the Arm, Shoulder, and Hand) to diagnose LEP, although this tool is an upper-limb disability scale. The ULNT2B (upper limb neural tension test) was added in the diagnostic process only in two RCTs (0.6%) [21,44].
The onset timings of symptoms in the subjects selected by the 227 RCTs included in the SRs were collected. A total of 42.1% of the studies analysed patients that had been displaying symptoms for more than 3 months. A total of 89 articles (40.2%) included patients with LEP for less than 3 months. The remaining 39 articles did not describe a cut-off related to the timing of the symptoms’ onset [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44].
4. Discussion
The data collection of the terms used to give a more aetiologically correct meaning to a set of clear symptoms such as the ones associated with LEP showed a wide heterogeneity dictated both by a merely biomedical view of the musculoskeletal problem and by the habit of using a term that was first coined in 1883 and is still used to this day [46]. The term “tennis elbow” was used in 56 out of the 227 selected RCTs and, indeed, refers to pathology with a high incidence in tennis. However, it is well known that LEP mainly affects the working population category, especially those involved with heavy lifting and subtle movements of the upper limbs; the LEP incidence in tennis is rather low and affects mainly amateur tennis players [5,12,14,46].
Evaluation using the RoBis tool showed a low bias risk in most of the selected SRs [18,19]. The studies showed good methodological rigour from the point of view of the eligibility and selection criteria of the RCTs. In contrast, the synthesis of the studies was often difficult due to the heterogeneity of the outcomes and the evaluation criteria.
4.1. Terminology Variability in LEP
The term “lateral epicondylitis” was used in 51.6% of the articles and recalled the primarily inflammatory nature of LEP. After several histopathological studies on tendons, Khan et al. (2002) recommended opting for the term “tendinopathy” to describe the symptomatology more accurately [47]. Indeed, several authors underlined that LEP is not caused by an inflammatory component but by a degenerative tendon process in the following years [46,47,48].
According to these studies, terms such as “epicondylosis” (1.0%), “chronic elbow tendinosis” (0.5%), “common extensor tendinosis” (1.6%), “lateral epicondylar tendinopathy” (0.5%), and “extensor carpi radial tendinitis” (1.0%) should be abandoned because they are obsolete.
The term “tendinopathy,” in particular “lateral elbow tendinopathy” or “lateral epicondylar tendinopathy,” was mentioned in five articles (2.1% and 0.5%). It is worth noting that three of these RCTs were selected from an SR by Raman et al. (2012) that dealt with the therapeutic exercise’s efficacy in the treatment of LEP [34]. This link between exercise and tendinopathy is tightly connected to the cultural revolution in the rehabilitation in treating overload issues and tendinopathies. Several authors, such as Maffulli, Cook and afterwards Rio, were among the first to understand the importance of exercise in this kind of pathology [49,50,51].
Among the 227 selected RCTs, the term “lateral epicondylalgia” was included in 19 studies (9.4%). In an SR by Bisset et al. (2005), 28 RCTs were analysed that dealt with the most effective interventions in the case of “lateral epicondylalgia” [27]. This terminological and conceptual transition underlines the shift from the biomedical pathology to the musculoskeletal disorder related to the bio–psycho–social sphere [11,27,52].
4.2. Classification Based on Onset of Symptoms
The psycho–social sphere seems to have a key role in developing the central sensitisation (CS) phenomenon in subjects with LEP. The CS phenomenon is directly associated with the onset of a disturbance in the musculoskeletal structure (low-back pain, cervicogenic headache, LEP) and is more recurring in subjects showing symptoms for three months or more [53]. In the inclusion criteria of the 227 RCTs, only 42.1% of the studies included patients with symptoms lasting more than three months. That means that the remaining articles (39.4% with symptoms < 3 months and 18.1% with non-specified temporal criteria) structured the RCTs based on a group of patients that was not homogeneous for the symptoms’ onset, the related psychosocial associations, and, therefore, the presence or not of the CS phenomenon. That could have modified the response of some subjects to the proposed interventions, causing a background bias that invalidates the quality and the results of the study itself.
4.3. Diagnostic Test in LEP
The literature-based and clinical approach mainly uses provocation tests that exacerbate the epicondylar pain to diagnose in the case of suspected LEP.
In this SR, eight different provocation tests were identified (painful palpation, Cozen test, Maudsley test, chair test, resisted pronosupination test, Mill’s test, lifting test, coffee-cup test): Painful palpation of the epicondyle (46.8%), the Cozen test (42.1%), and the Maudsley test (22.2%) were the most mentioned ones in the 216 selected RCTs.
The Cozen and Maudsley tests are the only ones that were submitted to a primary study that calculated their psychometric values. In particular, these two tests showed high sensitivity values (Cozen test, 84%; Maudsley test, 88%) [18]. Furthermore, clustering these two tests might further increase their reliability. Literature about psychometric values of other tests is quite weak, so they should be studied further. The PFGST was administered in 19.0% of the cases and represents a valid instrument for the assessment of the load’s tolerance and the excitability of the elbow with a high reliability (ICC > 0.97) and a minimal clinical importance difference (MCID) of 7 kg, representing an 18% change of the mean normative value [27,45,54,55]. ULNT2B was proposed in two RCTs included to analyse the presence of an entrapment of the radial nerve at the level of Frohse’s arcade or inside of the brachioradial muscle [56,57]. In this regard, other tests have been proposed in the literature to evaluate the presence of peripheral nerve entrapment in LEP, such as the Rule-of-Nine test [58].
Most of the tests mentioned in the studies aim to elicit a symptom that recalls an insertional tendinopathy of the extensors of the wrist and fingers, but they do not allow for a differential diagnosis with other causes of LEP such as radial nerve entrapment and intra-articular pathology.
In fact, the studies showed that several cases of persistent LEP were related to a high incidence of intra-articular alterations caused by a condition of ligamentous micro-instability at the radial capitellum level. (S.M.I.L.E., symptomatic minor instability of the lateral elbow) [59,60]. Several cases of LEP revealed a ligamentous laxity of the radial component of the radial collateral ligament and/or of the radial annular ligament that lead to phenomena of synovitis and/or chondropathy at the radial capitellum level (CLAC lesion, “chondropathy of the lateral aspect of the capitellum”). From a diagnostic and prognostic point of view, it would be useful to start considering the intra-articular issue in the assessment of LEP to create a reliable and efficient procedural algorithm for identifying the main pain generator and for the treatment of this symptomatology. This kind of approach would allow for different management of cases of persistent LEP that have not shown improvement after the suggested rehabilitative treatment and that still show disability and restrictions in movement.
4.4. Lateral Elbow Disorders: A New Proposal
Following the previous paragraphs, we believe that the time has come to find, through a common language, a definition to better describe the disorders of the lateral part of the elbow. According to the authors, lateral elbow disorders (LEDs) seems the most appropriate term to describe them. Furthermore, we want to propose the use of more current tools for a clinical setting, capable of identifying specific subgroups of LEDs that (A) help to determine more carefully the description of signs and symptoms of patients suffering from lateral elbow pain, (B) respond to different prognosis and outcome times of the proposed treatments and their relative impact on the psycho–social aspects of the patient, and (C) in the presence of a high predominance of yellow flags, the patient should be monitored and educated, thus modifying any dysfunctional beliefs and overestimated expectations about elbow pain and reconceptualising, on a cognitive level, any fear, harm, and avoidance about elbow activity [61]. In this regard, we believe it is fundamental that the clinical framework follow a rational construct capable of:
- (1)
- Analysing any red flags to analyse the presence of situations that imply a non-musculoskeletal problem. In this case, the patient needs to be referred to the doctor for the most appropriate diagnostic investigations (screening for referral) [62,63,64,65];
- (2)
- Guiding the clinician in determining whether there is a structure predominantly involved in and responsible for the lateral musculoskeletal disorder of the elbow (muscle–tendon, joint, neural) capable of influencing the prognosis and the type of treatment (conservative and/or surgical); and
- (3)
- Recognising profiles of patients who, depending on the time of suffering, may present the risk of developing yellow flags capable of slowing down or altering the treatment process and/or deteriorating adherence to the therapeutic plan.
Following an evaluation algorithm proposed in a previous publication with the I-APPLEp algorithm [11], we believe that replacing the term “LEP” with “LEDs” is necessary. Our main goal is to describe and identify the lateral problems of the persistent-recalcitrant elbow—longer than three months—as an alternative to the old labels, among which are “epycondilitys,” “tennis elbow,” and “epycondilalgia.” Accordingly, we propose a modified version of the I-APPLE algorithm: LED-APP, the Lateral Elbow Disorders Approach (reported in Figure S1). It considers four possible subgroups of clinical pictures caused by three main anatomical complexes responsible for signs and symptoms, responding to different treatment principles and prognostic times. Namely, the algorithm includes the following as subgroups:
- -
- T-LED (Lateral Elbow Disorders—Tendinopathic Prevalence);
- -
- A-LED (Lateral Elbow Disorders—Arthropathic Prevalence);
- -
- N-LED (Lateral Elbow Disorders—Neuropathic Prevalence); and
- -
- M-LED (Lateral Elbow Disorders—Mixed Form).
The rationale for the new LED-APP assessment and treatment framework provides different steps of clinical assessment. In Clinical Assessment 1, we evaluate the involvement of the tendon component and the relative pain reported by the patient through the tendon load tests suggested by the literature as the most sensitive (rule out: Cozen test, Maudsley test, pain-free grip-strength test) [8,27]. The minimal clinical importance difference (MCID) of PFGS has been reported to be 7 kg in patients with LEP and represents an 18% change in the mean normative value of grip strength (38.4 kg) for men and women aged 40–50 years [27,45,54,55].
In case of positivity of these tests, we consider the clinical picture with tendinopathic prevalence (T-LED), and the treatment will be oriented towards desensitising pain with manual therapy and exercise and improving the load tolerance (load capacity) of the whole muscle–tendon system with progressive therapeutic exercise with a prognostic perspective of 4–6 weeks [66,67,68,69].
In case of failure of the conservative approach (NPRS <2 points, DASH <10 points, PRTEE <10 points), we consider it useful to refer patients to an orthopaedist. The main aim is to offer diagnostic imaging (Msk-US imaging, X-ray, MRI) and choose the most appropriate therapeutic path up to possible surgery [11]. In case of a negative Clinical Assessment 1, we will move on to Clinical Assessment 2, in which we evaluate whether the symptoms reported by the patient are attributable to joint pain through the direct provocation of the humero-radial joint structures with two provocative tests: SALT (supination antero-lateral pain test), proven to be sensitive and accurate for pictures of synovitis and anterior patolassity, and PEPPER (posterior elbow pain by palpation–extension of the radiocapitellar joint), proven to be sensitive and accurate for pictures of radial head chondropathy [70]. If these tests are positive (ad one of the two tests), the clinical picture will be considered a prevalent lateral elbow disorders (A-LED) with characteristics attributable to the clinical picture of SMILE (symptomatic minor instability of the lateral elbow) [59] and the treatment will be oriented to the protection of the joint component with the use of splints, braces and/or bandages, and manual therapy techniques of arthrokinematics [71] for pain control and intense therapeutic exercise with a prognostic outlook of 12–16 weeks [22,42,71]. In case of failure of the conservative approach (NPRS <2 points, DASH <10 points, PRTEE < 10 points), we consider it useful to refer patients to the orthopaedist. The main aim is to offer diagnostic imaging (Msk-US imaging, X-ray, MRI) and choose the most appropriate therapeutic path up to possible surgery [11].
In case of a negative Clinical Assessment 2, we will move on to Clinical Assessment 3, which assesses whether the patient’s symptoms are attributable to neural entrapment phenomena in Frohse’s arch (NIP syndrome or radial tunnel syndrome) or entrapment to the intermuscular septum between the extensor radial long carpus and the brachioradialis (Wartemberg syndrome) through clinical tests such as ULNT2b. If positive, proceed with two further tests: the Rule-of-Nines test and the Tinel test; in case of positivity to at least one of the two, the clinical picture will be considered a neural prevalence of lateral elbow disorder (N-LED) with the related sub-declinations. Thus, the treatment will include a manual therapy approach composed of neurodynamic and myofascial techniques associated with dynamic thermoplastic splints, ESWT, neurodynamic sliding or tensioning techniques, and dynamic stretching, with a prognostic perspective of (4) 8–12 weeks [72]. In case of failure of the conservative approach (NPRS <2 points, DASH <10 points, PRTEE <10 points), we consider it useful to refer patients to the orthopaedist. The main aim is to offer diagnostic imaging (Msk-US imaging, X-ray, MRI) and choose the most appropriate therapeutic path up to possible surgery [11].
In case of a negative Clinical Assessment 3, the signs and symptoms will be attributed to clinical pictures on a mixed basis (Mixed Form: M-LED), which should be approached and considered according to the clinical picture of reference. On the other hand, if the anamnestic collection and the description of the signs and/or symptoms are attributable to an uncommon specific problem, such as a possible expression of important and/or serious problems (e.g., trauma, fever, weight loss, infection, recent surgery, systemic disease, fracture, tumour), it is essential to refer back to the specialist for clinical and diagnostic study (screening for referral).
4.5. Limits
The SRs were selected through the RoBis tool to assess the risk of bias; this tool should not be used to generate a summary “quality score” because of the well-known problems associated with such scores. Therefore, the pooling of SR data does not present a cut-off for the quality screening of the articles. Inter review blindness was not maintained in the full-text analysis of the selected studies.
The authors are aware that the type of studies selected is not the best for evaluating a clinical condition’s taxonomy, classification, or diagnostic criteria. However, the choice to select systematic reviews of RCTs seemed a much more clinical and pragmatic choice to the authors. Since RCTs are the best studies to evaluate the best treatment, we started from this type of study to understand how these studies made diagnoses, which tests they relied on, and what they called these clinical conditions of LEP.
In future studies, this analysis of the literature could be helpful to analyse the reliability of clinical tests for patients with LEP and create a new algorithm of assessment and diagnosis. Lastly, quality studies to test its clinical efficacy are required to apply a structured and rigorous validation course.
4.6. Consistency
In the literature, to date, the terminological framework of this problem is confusing [73]. Therefore, there is a need for standard and internationally accepted definitions for LEP. LEP is defined as an overuse injury due to an unbalance between the resistance capacity of connective tissue and the biomechanical solicitations on the lateral aspect of the elbow [1,2,3,4,5,6,7,9]. Furthermore, pain is not the only symptom complained of by the patient, but is often associated with disabilities, functional impairments, and loss of social, sports, and work participation [9,10,11].
Therefore, in our view, a more suitable word may be “disorder” (lateral elbow disorders—LEDs), which better describes multifactorial conditions, which include, besides structural aspects, psychosocial elements often present in nonspecific painful disorders like LEP [5,6,9,10].
Our SR confirmed the findings for LEP, like in recent literature, which concluded that the evidence about the terminology of LEP is scarce and derived from studies not of good methodological quality [47,48,49,74,75]. This SR showed a quite high prevalence among studies of the term “LEP,” but this finding, albeit relative to a wider sample of patients, does not specifically include accurate reasons to adopt this term exclusively.
5. Conclusions
LEP includes a wide range of inflammatory and degenerative conditions affecting the muscles, tendons, ligaments, joints, peripheral nerves, and supporting blood vessels. These include clinical syndromes such as intra-articular and ligament disorders, tendinopathy, and peripheral nerve compression pathology.
In this SR, the terminological analysis of LEP that was carried out shows the need for “tidying up” within the wide range of terms and descriptions related to this symptomatology. The lack of clarity from a terminological point of view has led clinicians and researchers to define these symptoms with different terms, shifting from a traditional biomedical view to a biopsychosocial one, without determining a univocal term shared by everyone that could describe the pathology clearly and correctly. Furthermore, not even at the diagnostic level is there currently a validated and reliable cluster of tests in the literature that allows for the distinction between extra-articular-based symptomatology and an intra-articular-based one in a patient with LEP to define a suitable pathway of treatment.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10061095/s1, Figure S1: LED-APP: Framework of Lateral Elbow Disorders Approach.
Author Contributions
L.D.F. and S.V. conceived the study. S.V. and F.M. designed the study. All authors overviewed the data analysis and interpretation. L.D.F., S.V., and F.M. wrote the first draft of the paper. All authors contributed to the investigation and to the writing (review and editing). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Raw data are available upon request.
Acknowledgments
The authors would like to express their gratitude to Giacomo Rossettini, for his invaluable contribution to the critical revision of the manuscript for important intellectual content.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Literature search strategy.
Table A1.
Literature search strategy.
| The following databases were searched • Cochrane Library • Medline | ||
| Search engines used: • PubMed Clinical Queries—Systematic Reviews • Cochrane Review • Epistemonikos | ||
| Pubmed Clinical Queries Search Strategy Tennis elbow [MeSH Term] OR Tennis elbow OR Lateral epicondylitis OR Lateral epicondylalgia OR Lateral elbow tendinopathy | Cochrane Review Search Strategy Tennis elbow OR Lateral epicondylitis OR Lateral epicondylalgia OR Lateral elbow tendinopathy | Epistemonikos Search Strategy Tennis elbow OR Lateral epicondylitis OR Lateral epicondylalgia OR Lateral elbow tendinopathy |
References
- Verhaar, J.A. Tennis elbow. Anatomical, epidemiological and therapeutic aspects. Int. Orthop. 1994, 18, 263–267. [Google Scholar]
- Helliwell, P.S.; Bennett, R.M.; Littlejohn, G.; Muirden, K.D.; Wigley, R.D. Towards epidemiological criteria for soft-tissue disorders of the arm. Occup. Med. 2003, 53, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, P.G. The prevalence of humeral epicondylitis: A survey in general practice. J. R. Coll. Gen. Pract. 1986, 36, 464–465. [Google Scholar] [PubMed]
- Shiri, R.; Viikari-Juntura, E.; Varonen, H.; Heliövaara, M. Prevalence and Determinants of Lateral and Medial Epicondylitis: A Population Study. Am. J. Epidemiol. 2006, 164, 1065–1074. [Google Scholar] [CrossRef] [PubMed]
- De Smedt, T.; de Jong, A.; Van Leemput, W.; Lieven, D.; Van Glabbeek, F. Lateral epicondylitis in tennis: Update on aetiology, biomechanics and treatment. Br. J. Sports Med. 2007, 41, 816–819. [Google Scholar] [CrossRef] [PubMed]
- Waugh, E.J.; Jaglal, S.B.; Davis, A.M.; Tomlinson, G.; Verrier, M.C. Factors associated with prognosis of lateral epicondylitis after 8 weeks of physical therapy. Arch. Phys. Med. Rehabil. 2004, 85, 308–318. [Google Scholar] [CrossRef]
- Coombes, B.K.; Bisset, L.; Vicenzino, B. Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All. J. Orthop. Sports Phys. Ther. 2015, 45, 938–949. [Google Scholar] [CrossRef]
- Saroja, G.; Aseer, P.A.L.; Venkata Sai, P.M. Diagnostic accuracy of provocative tests in lateral epicondylitis. Int. J. Physiother. Res. 2014, 2, 815–823. [Google Scholar] [CrossRef]
- Taylor, S.A.; Hannafin, J.A. Evaluation and Management of Elbow Tendinopathy. Sports Health A Multidiscip. Approach 2012, 4, 384–393. [Google Scholar] [CrossRef]
- Herquelot, E.; Bodin, J.; Roquelaure, Y.; Ha, C.; Leclerc, A.; Goldberg, M.; Descatha, A. Work-related risk factors for lateral epicondylitis and other cause of elbow pain in the working population. Am. J. Ind. Med. 2013, 56, 400–409. [Google Scholar] [CrossRef]
- Di Filippo, L.; Pennella, D.; Maselli, F.; Arrigoni, P. Research proposal of a new clinic model for the interpretation of Lateral Elbow Pain: Is it time to change? Muscle Ligaments Tendons J. 2020, 10, 57–66. [Google Scholar] [CrossRef]
- Walz, D.M.; Newman, J.S.; Konin, G.P.; Ross, G. Epicondylitis: Pathogenesis, Imaging, and Treatment. RadioGraphics 2010, 30, 167–184. [Google Scholar] [CrossRef]
- Karanasios, S.; Korakakis, V.; Moutzouri, M.; Drakonaki, E.; Koci, K.; Pantazopoulou, V.; Tsepis, E.; Gioftsos, G. Diagnostic accuracy of examination tests for lateral elbow tendinopathy (LET)—A systematic review. J. Hand Ther. 2021, in press. [Google Scholar] [CrossRef]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Hunt, H.; Pollock, A.; Campbell, P.; Estcourt, L.; Brunton, G. An introduction to overviews of reviews: Planning a relevant research question and objective for an overview. Syst. Rev. 2018, 7, 39. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interven-tions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Whiting, P.; Savović, J.; Higgins, J.P.T.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R.; ROBIS Group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef]
- Banzi, R.; Cinquini, M.; Gonzalez-Lorenzo, M.; Pecoraro, V.; Capobussi, M.; Minozzi, S. Quality assessment versus risk of bias in systematic reviews: AMSTAR and ROBIS had similar reliability but differed in their construct and applicability. J. Clin. Epidemiol. 2018, 99, 24–32. [Google Scholar] [CrossRef]
- Altman, D.G. Practical Statistics for Medical Research, 1st ed.; Chapman and Hall: London, UK, 1991. [Google Scholar]
- Van der Windt, D.A.; van der Heijden, G.J.; van den Berg, S.G.; Ter Riet, G.; de Winter, A.F.; Bouter, L.M. Ultrasound therapy for musculoskeletal disorders: A systematic review. Pain 1999, 81, 257–271. [Google Scholar] [CrossRef]
- Struijs, P.A.; Smidt, N.; Arola, H.; Van Dijk, C.N.; Buchbinder, R.; Assendelft, W.J. Orthotic devices for tennis elbow: A systematic review. Br. J. Gen. Pr. 2001, 51, 924–929. [Google Scholar]
- Green, S.; Buchbinder, R.; Barnsley, L.; Hall, S.; White, M.; Smidt, N.; Assendelft, W.J. Acupuncture for lateral elbow pain. Cochrane Database Syst. Rev. 2002, 2013, CD003527. [Google Scholar] [CrossRef]
- Borkholder, C.D.; Hill, V.A.; Fess, E.E. The efficacy of splinting for lateral epicondylitis: A systematic review. J. Hand Ther. 2004, 17, 181–199. [Google Scholar] [CrossRef]
- Trudel, D.; Duley, J.; Zastrow, I.; Kerr, E.W.; Davidson, R.; MacDermid, J.C. Rehabilitation for patients with lateral epicondylitis: A systematic review. J. Hand Ther. 2004, 17, 243–266. [Google Scholar] [CrossRef]
- Buchbinder, R.; Green, S.; Youd, J.M.; Assendelft, W.J.; Barnsley, L.; Smidt, N. Shock wave therapy for lateral elbow pain. Cochrane Database Syst. Rev. 2005, 23, 411–414. [Google Scholar] [CrossRef]
- Bisset, L.; Paungmali, A.; Vicenzino, B.; Beller, E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br. J. Sports Med. 2005, 39, 411–422. [Google Scholar] [CrossRef]
- Herd, C.R.; Meserve, B.B. A Systematic Review of the Effectiveness of Manipulative Therapy in Treating Lateral Epicondylalgia. J. Man. Manip. Ther. 2008, 16, 225–237. [Google Scholar] [CrossRef]
- Barr, S.; Cerisola, F.L.; Blanchard, V. Effectiveness of corticosteroid injections compared with physiotherapeutic interventions for lateral epicondylitis: A systematic review. Physiotherapy 2009, 95, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Coombes, B.K.; Bisset, L.; Vicenzino, B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: A systematic review of randomised controlled trials. Lancet 2010, 376, 1751–1767. [Google Scholar] [CrossRef]
- Tumilty, S.; Munn, J.; McDonough, S.; Hurley, D.A.; Basford, J.R.; Baxter, G.D. Low Level Laser Treatment of Tendinopathy: A Systematic Review with Meta-analysis. Photomed. Laser Surg. 2010, 28, 3–16. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, L.; Bannuru, R.R.; Severin, M.; Harvey, W. Injection of botulinum toxin for treatment of chronic lateral epi-condylitis: Systematic review and meta-analysis. Semin. Arthritis Rheum. 2011, 40, 532–538. [Google Scholar] [CrossRef]
- Buchbinder, R.; Johnston, R.V.; Barnsley, L.; Assendelft, W.J.; Bell, S.N.; Smidt, N. Surgery for lateral elbow pain. Cochrane Database Syst. Rev. 2011, 2011, CD003525. [Google Scholar] [CrossRef]
- Raman, J.; MacDermid, J.C.; Grewal, R. Effectiveness of Different Methods of Resistance Exercises in Lateral Epicondylosis—A Systematic Review. J. Hand Ther. 2012, 25, 5–26. [Google Scholar] [CrossRef]
- Ahmad, Z.; Brooks, R.; Kang, S.-N.; Weaver, H.; Nunney, I.; Tytherleigh-Strong, G.; Rushton, N. The Effect of Platelet-Rich Plasma on Clinical Outcomes in Lateral Epicondylitis. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 1851–1862. [Google Scholar] [CrossRef] [PubMed]
- Pattanittum, P.; Turner, T.; Green, S.; Buchbinder, R. Non-steroidal anti-inflammatory drugs (NSAIDs) for treating lateral elbow pain in adults. Cochrane Database Syst. Rev. 2013, 2013, CD003686. [Google Scholar] [CrossRef]
- Cullinane, F.L.; Boocock, M.G.; Trevelyan, F.C. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin. Rehabil. 2014, 28, 3–19. [Google Scholar] [CrossRef]
- Tang, H.; Fan, H.; Chen, J.; Yang, M.; Yi, X.; Dai, G.; Chen, J.; Tang, L.; Rong, H.; Wu, J.; et al. Acupuncture for Lateral Epicondylitis: A Systematic Review. Evidence-Based Complement. Altern. Med. 2015, 2015, 861849. [Google Scholar] [CrossRef]
- Tsikopoulos, K.; Tsikopoulos, A.; Natsis, K. Autologous whole blood or corticosteroid injections for the treatment of epi-condylopathy and plantar fasciopathy? A systematic review and meta-analysis of randomized controlled trials. Phys. Ther. Sport 2016, 22, 114–122. [Google Scholar] [CrossRef]
- Mattie, R.; Wong, J.; McCormick, Z.; Yu, S.; Saltychev, M.; Laimi, K. Percutaneous Needle Tenotomy for the Treatment of Lateral Epicondylitis: A Systematic Review of the Literature. PM R 2017, 9, 603–611. [Google Scholar] [CrossRef]
- Burn, M.B.; Mitchell, R.J.; Liberman, S.R.; Lintner, D.M.; Harris, J.D.; McCulloch, P.C. Open, Arthroscopic, and Percutaneous Surgical Treatment of Lateral Epicondylitis: A Systematic Review. Hand 2017, 13, 264–274. [Google Scholar] [CrossRef]
- Lucado, A.M.; Dale, R.B.; Vincent, J.; Day, J.M. Do joint mobilizations assist in the recovery of lateral elbow tendinopathy? A systematic review and meta-analysis. J. Hand Ther. 2018, 32, 262–276. [Google Scholar] [CrossRef]
- Lin, Y.-C.; Wu, W.-T.; Hsu, Y.-C.; Han, D.-S.; Chang, K.-V. Comparative effectiveness of botulinum toxin versus non-surgical treatments for treating lateral epicondylitis: A systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 131–145. [Google Scholar] [CrossRef] [PubMed]
- Navarro-Santana, M.J.; Sanchez-Infante, J.; Gómez-Chiguano, G.F.; Cleland, J.A.; López-De-Uralde-Villanueva, I.; Fernández-De-Las-Peñas, C.; Manzano, G.P. Effects of trigger point dry needling on lateral epicondylalgia of musculoskeletal origin: A systematic review and meta-analysis. Clin. Rehabil. 2020, 34, 1327–1340. [Google Scholar] [CrossRef] [PubMed]
- Karanasios, S.; Korakakis, V.; Whiteley, R.; Vasilogeorgis, I.; Woodbridge, S.; Gioftsos, G. Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: A systematic review and meta-analysis of 2123 subjects in 30 trials. Br. J. Sports Med. 2020, 55, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Major, H.P. Lawn-tennis Elbow. BMJ 1883, 2, 557. [Google Scholar]
- Khan, K.M.; Cook, J.L.; Kannus, P.; Maffulli, N.; Bonar, S.F. Time to abandon the ‘tendinitis’ myth. BMJ 2002, 324, 626–627. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, J.T.; Baptista, J.S.; Vaz, M. Incidence and prevalence of upper-limb work related musculoskeletal disorders: A systematic review. Work 2015, 51, 635–644. [Google Scholar] [CrossRef]
- Maffulli, N.; Testa, V.; Capasso, G.; Ewen, S.W.; Sullo, A.; Benazzo, F.; King, J.B. Similar Histopathological Picture in Males with Achilles and Patellar Tendinopathy. Med. Sci. Sports Exerc. 2004, 36, 1470–1475. [Google Scholar] [CrossRef]
- Cook, J.L.; Purdam, C.R. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br. J. Sports Med. 2009, 43, 409–416. [Google Scholar] [CrossRef]
- Rio, E.; Kidgell, D.; Moseley, L.; Gaida, J.; Docking, S.; Purdam, C.; Cook, J. Tendon neuroplastic training: Changing the way we think about tendon rehabilitation: A narrative review. Br. J. Sports Med. 2015, 50, 209–215. [Google Scholar] [CrossRef]
- Coombes, B.K.; Bisset, L.; Vicenzino, B. A new integrative model of lateral epicondylalgia. Br. J. Sports Med. 2009, 43, 252–258. [Google Scholar] [CrossRef]
- Fernandez-Carnero, J.; Fernandez-de-Las-Penas, C.; de la Llave-Rincon, A.I.; Ge, H.-Y.; Arendt-Nielsen, L. Widespread mechanical pain hypersensitivity as sign of central sensitization in unilateral epicondylalgia: A blinded, controlled study. Clin. J. Pain 2009, 25, 555–561. [Google Scholar] [CrossRef]
- Kim, J.K.; Park, M.G.; Shin, S.J. What is the Minimum Clinically Important Difference in Grip Strength? Clin. Orthop. Relat. Res. 2014, 472, 2536–2541. [Google Scholar] [CrossRef]
- Lim, E.C.W. Pain Free Grip Strength test. J. Physiother. 2013, 59, 59. [Google Scholar] [CrossRef]
- Vicenzino, B.; Paungmali, A.; Buratowski, S.; Wright, A. Specific manipulative therapy treatment for chronic lateral epicon-dylalgia produces uniquely characteristic hypoalgesia. Man Ther. 2001, 6, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Drechsler, W.; Knarr, J.F.; Snyder-Mackler, L. A Comparison of Two Treatment Regimens for Lateral Epicondylitis: A Randomized Trial of Clinical Interventions. J. Sport Rehabil. 1997, 6, 226–234. [Google Scholar] [CrossRef]
- Moradi, A.; Ebrahimzadeh, M.H.; Jupiter, J.B. Radial Tunnel Syndrome, Diagnostic and Treatment Dilemma. Arch. Bone Jt. Surg. 2015, 3, 156–162. [Google Scholar]
- Arrigoni, P.; Cucchi, D.; D’Ambrosi, R.; Butt, U.; Safran, M.R.; Denard, P.; Randelli, P. Intra-articular findings in symptomatic minor instability of the lateral elbow (SMILE). Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2255–2263. [Google Scholar] [CrossRef]
- Kniesel, B.; Huth, J.; Bauer, G.; Mauch, F. Systematic diagnosis and therapy of lateral elbow pain with emphasis on elbow instability. Arch. Orthop. Trauma. Surg. 2014, 134, 1641–1647. [Google Scholar] [CrossRef]
- Vlaeyen, J.; Morley, S.; Linton, S.; Boersma, K.; De Jong, J. Pain-Related Fear: Exposure-Based Treatment for Chronic Pain; IASP Press: Washington, DC, USA, 2012. [Google Scholar]
- Pennella, D.; Giagio, S.; Maselli, F.; Fiorentino, F.; Brindisino, F. Red flags useful to screen for gastrointestinal and hepatic diseases in patients with shoulder pain: A scoping review. Musculoskelet. Care 2022. [Google Scholar]
- Maselli, F.; Palladino, M.; Barbari, V.; Storari, L.; Rossettini, G.; Testa, M. The diagnostic value of Red Flags in thoracolumbar pain: A systematic review. Disabil. Rehabil. 2020, 44, 1190–1206. [Google Scholar] [CrossRef] [PubMed]
- Maselli, F.; Testa, M. Superficial peroneal nerve schwannoma presenting as lumbar radicular syndrome in a non-competitive runner. J. Back Musculoskelet. Rehabil. 2019, 32, 361–365. [Google Scholar] [CrossRef]
- Mourad, F.; Maselli, F.; Patuzzo, A.; Siracusa, A.; Di Filippo, L.; Dunning, J.; de Las Peñas, C.F. Osteocohondritis dissecans of the radial head in a young athlete: A case report. Int. J. Sports Phys. Ther. 2018, 13, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Bialosky, J.E.; Bishop, M.D.; Price, D.D.; Robinson, M.E.; George, S.Z. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Man. Ther. 2009, 14, 531–538. [Google Scholar] [CrossRef]
- Zusman, M. The Modernisation of Manipulative Therapy. Int. J. Clin. Med. 2011, 2, 644–649. [Google Scholar] [CrossRef]
- Bishop, M.D.; Torres-Cueco, R.; Gay, C.W.; Lluch-Girbes, E.; Beneciuk, J.M.; Bialosky, J.E. What effect can manual therapy have on a patient’s pain experience? Pain Manag. 2015, 5, 455–464. [Google Scholar] [CrossRef]
- Rio, E.; Moseley, L.; Purdam, C.; Samiric, T.; Kidgell, D.; Pearce, A.J.; Jaberzadeh, S.; Cook, J. The pain of tendinopathy: Physiological or pathophysiological? Sports Med. 2014, 44, 9–23. [Google Scholar] [CrossRef]
- Arrigoni, P.; Cucchi, D.; Menon, A.; Randelli, P. It’s time to change perspective! New diagnostic tools for lateral elbow pain. Musculoskelet. Surg. 2017, 101, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Hing, W.; Hall, T.; Rivett, D.; Vicenzino, B.; Mulligan, B. The Mulligan Concept of Manual Therapy, 1st ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Bula-Oyola, E.; Belda-Lois, J.-M.; Porcar-Seder, R.; Page, A. Effectiveness of electrophysical modalities in the rehabilitation of radial, ulnar, and median neuropathies. PLoS ONE 2021, 16, e0248484. [Google Scholar] [CrossRef]
- Boyer, M.I.; Hastings, H., II. Lateral tennis elbow: Is there any science out there? J. Shoulder Elbow Surg. 1999, 8, 481–491. [Google Scholar] [CrossRef]
- Nimgade, A.; Sullivan, M.; Goldman, R. Physiotherapy, Steroid Injections, or Rest for Lateral Epicondylosis? What the Evidence Suggests. Pain Pr. 2005, 5, 203–215. [Google Scholar] [CrossRef]
- Nirschl, R.P.; Ashman, E.S. Elbow tendinopathy: Tennis elbow. Clin. Sports Med. 2003, 22, 813–836. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).