Patient Judgement of Change with Elective Surgery Correlates with Patient Reported Outcomes and Quality of Life
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection and Sample Size
2.3. Outcome Measures
2.4. Statistical Analysis
3. Results
4. Discussion
Implications for Practice
- When collecting PROMs with surgical patients, it is acceptable to use a single “judgement of change” recall question completed by patients one week after the surgery, to measure their views on the amount of change experienced
- Before and after elective surgery, it may not be essential to administer both a quality of recovery PROM and a quality of life PROM, as they are closely correlated
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Glouberman, S. PROMs: A critical step, but only one of many. Healthc. Pap. 2012, 11, 29. [Google Scholar] [CrossRef] [PubMed]
- Ishaque, S.; Karnon, J.; Chen, G.; Nair, R.; Salter, A.B. A systematic review of randomised controlled trials evaluating the use of patient-reported outcome measures (PROMs). Qual. Life Res. 2019, 28, 567–592. [Google Scholar] [CrossRef] [PubMed]
- Field, J.; Holmes, M.M.; Newell, D. PROMs data: Can it be used to make decisions for individual patients? A narrative review. Patient Relat. Outcome Meas. 2019, 10, 233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, H.; Butow, P.; Dhillon, H.; Sundaresan, P. A review of the barriers to using Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs) in routine cancer care. J. Med. Radiat. Sci. 2021, 68, 186–195. [Google Scholar] [CrossRef]
- Grocott, M.P. Monitoring surgical outcomes: How and why? Curr. Anaesth. Crit. Care 2010, 21, 129–136. [Google Scholar] [CrossRef]
- Morris, M.; Brusco, N.; Woods, J.; Myles, P.S.; Hodge, A.; Jones, C.; Lloyd, D.; Rovtar, V.; Clifford, A.; Atkinson, V. Protocol for implementation of the ‘AusPROM’recommendations for elective surgery patients: A mixed-methods cohort study. BMJ Open 2021, 11, e049937. [Google Scholar] [CrossRef]
- Kwong, E.; Neuburger, J.; Black, N. Agreement between retrospectively and contemporaneously collected patient-reported outcome measures (PROMs) in hip and knee replacement patients. Qual. Life Res. 2018, 27, 1845–1854. [Google Scholar] [CrossRef] [Green Version]
- Australian Commission on Safety and Quality in Health Care. Selecting PROMs. Available online: https://wwwsafetyandqualitygovau/list-generic-proms (accessed on 15 January 2022).
- Van der Willik, E.M.; Terwee, C.B.; Bos, W.J.W.; Hemmelder, M.H.; Jager, K.J.; Zoccali, C.; Dekker, F.W.; Meuleman, Y. Patient-reported outcome measures (PROMs): Making sense of individual PROM scores and changes in PROM scores over time. Nephrology 2021, 26, 391–399. [Google Scholar] [CrossRef]
- Macchiarola, L.; Pirone, M.; Grassi, A.; Pizza, N.; Trisolino, G.; Stilli, S.; Zaffagnini, S. High recall bias in retrospective assessment of the pediatric International Knee Documentation Committee Questionnaire (Pedi-IKDC) in children with knee pathologies. Knee Surg. Sports Traumatol. Arthrosc. 2022. [Google Scholar] [CrossRef]
- McCann, A.C.; Phillips, K.M.; Trope, M.; Caradonna, D.S.; Gray, S.T.; Sedaghat, A.R. Characterising the potential for recall bias in anchor-based MCID calculation of patient-reported outcome measures for chronic rhinosinusitis. Clin. Otolaryngol. 2020, 45, 768–774. [Google Scholar] [CrossRef]
- Zini, M.; Banfi, G. A Narrative Literature Review of Bias in Collecting Patient Reported Outcomes Measures (PROMs). Int. J. Environ. Res. Public Health 2021, 18, 12445. [Google Scholar] [CrossRef] [PubMed]
- EuroQOL. EQ-5D. 2020. Available online: https://euroqol.org/ (accessed on 15 January 2022).
- Marti, C.; Hensler, S.; Herren, D.B.; Niedermann, K.; Marks, M. Measurement properties of the EuroQoL EQ-5D-5L to assess quality of life in patients undergoing carpal tunnel release. J. Hand Surg. 2016, 41, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.R.; Patel, R.C.; Singleton, G.F.; Moonesinghe, S.R. Patient-reported outcomes for ambulatory surgery. Curr. Opin. Anesthesiol. 2020, 33, 768–773. [Google Scholar] [CrossRef]
- Brusco, N.K.; Watts, J.J.; Shields, N.; Taylor, N.F. Are weekend inpatient rehabilitation services value for money? An economic evaluation alongside a randomized controlled trial with a 30 day follow up. BMC Med. 2014, 12, 89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brusco, N.K.; Watts, J.J.; Shields, N.; Taylor, N.F. Is cost effectiveness sustained after weekend inpatient rehabilitation? 12 month follow up from a randomized controlled trial. BMC Health Serv. Res. 2015, 15, 165. [Google Scholar] [CrossRef] [Green Version]
- Kleif, J.; Waage, J.; Christensen, K.B.; Gögenur, I. Systematic review of the QoR-15 score, a patient-reported outcome measure measuring quality of recovery after surgery and anaesthesia. Br. J. Anaesth. 2018, 120, 28–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stark, P.A.; Myles, P.S.; Burke, J.A. Development and Psychometric Evaluation of a Postoperative Quality of Recovery ScoreThe QoR-15. J. Am. Soc. Anesthesiol. 2013, 118, 1332–1340. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gagnier, J.J.; Lai, J.; Mokkink, L.B.; Terwee, C.B. COSMIN reporting guideline for studies on measurement properties of patient-reported outcome measures. Qual. Life Res. 2021, 30, 2197–2218. [Google Scholar] [CrossRef] [PubMed]
- Clinical & Translational Science Institute. Sample Size Calculators for Designing Clinical Research. Available online: https://sample-size.net/correlation-sample-size/ (accessed on 3 May 2022).
- Chen, P.; Lin, K.-C.; Liing, R.-J.; Wu, C.-Y.; Chen, C.-L.; Chang, K.-C. Validity, responsiveness, and minimal clinically important difference of EQ-5D-5L in stroke patients undergoing rehabilitation. Qual. Life Res. 2016, 25, 1585–1596. [Google Scholar] [CrossRef] [PubMed]
- Golicki, D.; Niewada, M.; Buczek, J.; Karlińska, A.; Kobayashi, A.; Janssen, M.F.; Pickard, A.S. Validity of EQ-5D-5L in stroke. Qual. Life Res. 2015, 24, 845–850. [Google Scholar] [CrossRef] [Green Version]
- Mulhern, B.; Feng, Y.; Shah, K.; Janssen, M.F.; Herdman, M.; van Hout, B.; Devlin, N. Comparing the UK EQ-5D-3L and English EQ-5D-5L value sets. Pharmacoeconomics 2018, 36, 699–713. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.S.; Notz, W.I.; Flinger, M.A. The Basic Practice of Statistics, 6th ed.; WH Freeman: New York, NY, USA, 2013; Volume 2. [Google Scholar]
- IBM. SPSS Statistics, 21.0; IBM: Chicago, IL, USA, 2012. [Google Scholar]
- Murphy, M.; Hollinghurst, S.; Salisbury, C. Identification, description and appraisal of generic PROMs for primary care: A systematic review. BMC Fam. Pract. 2018, 19, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stirling Bryan, J.D.; Davis, J.; Broesch, J.; Doyle-Waters, M.M.; Lewis, S.; Mcgrail, K.; McGregor, M.J.; Murphy, J.M.; Sawatzky, R. Choosing your partner for the PROM: A review of evidence on patient-reported outcome measures for use in primary and community care. Healthc. Policy 2014, 10, 38. [Google Scholar]
- Myles, P.S. More than just morbidity and mortality—Quality of recovery and long-term functional recovery after surgery. Anaesthesia 2020, 75 (Suppl. 1), e143–e150. [Google Scholar] [CrossRef] [PubMed]
- Kwong, E.; Black, N. Retrospectively patient-reported pre-event health status showed strong association and agreement with contemporaneous reports. J. Clin. Epidemiol. 2017, 81, 22–32. [Google Scholar] [CrossRef] [Green Version]
- Kwong, E.; Black, N. Feasibility of collecting retrospective patient reported outcome measures (PROMs) in emergency hospital admissions. J. Patient-Rep. Outcomes 2018, 2, 1–11. [Google Scholar] [CrossRef]
- Kwong, E.; Neuburger, J.; Black, N. Can patient reported outcomes measures (PROMs) be used in emergency admissions? Comparison of retrospective and contemporaneous PROMs after hip and knee replacement: A cohort study. Lancet 2017, 390, S55. [Google Scholar] [CrossRef]
- McCaffrey, N.; Kaambwa, B.; Currow, D.C.; Ratcliffe, J. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Health Qual. Life Outcomes 2016, 14, 133. [Google Scholar] [CrossRef] [Green Version]
- Reeve, B.B.; Wyrwich, K.W.; Wu, A.W.; Velikova, G.; Terwee, C.B.; Snyder, C.F.; Schwartz, C.; Revicki, D.A.; Moinpour, C.M.; McLeod, L.; et al. ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual. Life Res. 2013, 22, 1889–1905. [Google Scholar] [CrossRef]


| Survey I n = 1135 | Survey II n = 1698 | Survey III n = 1344 | ||
|---|---|---|---|---|
| Email response rate | Sent | 6263 | 9615 | 9612 |
| Responses | 1063 | 1449 | 1197 | |
| Response Rate | 17.0% | 15.1% | 12.5% | |
| Short Message Service (SMS) response rate | Sent | 114 | 740 | 740 |
| Responses | 72 | 249 | 147 | |
| Response Rate | 63.2% | 33.6% | 19.9% | |
| Overall responses rate | Sent | 6377 | 10,355 | 10,352 |
| Responses | 1135 | 1698 | 1344 | |
| Response Rate | 17.8% | 16.4% | 13.0% | |
| Age range | 18–40, 244 (21.5%) 41–64, 490 (43.2%) 65–74, 274 (24.2%) 75–84, 119 (10.5%) 85+, 6 (0.5%) | 18–40, 307 (18.1%) 41–64, 785 (46.4%) 65–74, 417 (24.6%) 75–84, 177 (10.5%) 85+, 7 (0.4%) | 18–40, 212 (15.8%) 41–64, 613 (45.6%) 65–74, 357 (26.6%) 75–84, 154 (11.5%) 85+, 7 (0.5%) | |
| Gender, female | 673 (59.4%) | 945 (55.8%) | 733 (54.6%) | |
| Day surgery | 253 (47.3%) | 938 (55.5%) | 732 (54.6%) | |
| Survey I | Survey II | Survey III | Mean Difference (95% CI, p Value) | |||
|---|---|---|---|---|---|---|
| Survey II Minus Survey I | Survey III Minus Survey II | Survey III Minus Survey I | ||||
| QoR-15 * | ||||||
| Overnight stay admissions | 122.93 (SD 19.54; n = 188) | 110.94 (SD 23.05; n = 540) | 124.52 (SD 20.59; n = 473) | −12.00 (−15.69 to −8.31; p < 0.001) | 13.59 (10.88 to 16.30; p < 0.001) | 1.59 (−1.84 to 5.03; p = 0.363) |
| Day admissions | 126.41 (SD 16.82; n = 165) | 120.37 (SD 21.52; n = 633) | 128.63 (SD 20.02; n = 497) | −6.04 (−9.60 to −2.50; p = 0.001) | 8.26 (5.81 to 10.72; p < 0.001) | 2.23 (−1.18 to 5.63; p = 0.199) |
| Combined overnight and day admissions | 124.40 (SD 19.02; n = 738) | 116.08 (SD 22.70; n = 1,178) | 126.57 (SD 20.43; n = 973) | −8.31 (−10.28 to −6.35; p < 0.001) | 10.49 (8.64 to 12.33; p < 0.001) | 2.18 (0.28 to 4.07; p = 0.025) |
| EQ-5D # | ||||||
| Overnight stay admissions | 0.634 (SD 0.295; n = 9) | 0.616 (SD 0.260; n = 55) | 0.735 (SD 0.205; n = 60) | −0.018 (−0.208 to 0.172; p = 0.851) | 0.118 (0.032 to 0.204; p = 0.007) | 0.078 (−0.055 to 0.256; p = 0.201) |
| Day admissions | 0.823 (SD 0.145; n = 12) | 0.694 (SD 0.177; n = 123) | 0.767 (SD 0.218; n = 79) | −0.129 (−0.234 to −0.024; p = 0.016) | 0.073 (0.018 to 0.128; p = 0.010) | −0.056 (−0.185 to 0.074; p = 0.394) |
| Combined overnight and day admissions | 0.738 (SD 0.233; n = 84) | 0.670 (SD 0.209; n = 178) | 0.753 (SD 0.211; n = 140) | −0.068 (−0.124 to −0.011; p = 0.019) | 0.083 (0.036 to 0.130; p = 0.001) | 0.015 (−0.044 to 0.075; p = 0.615) |
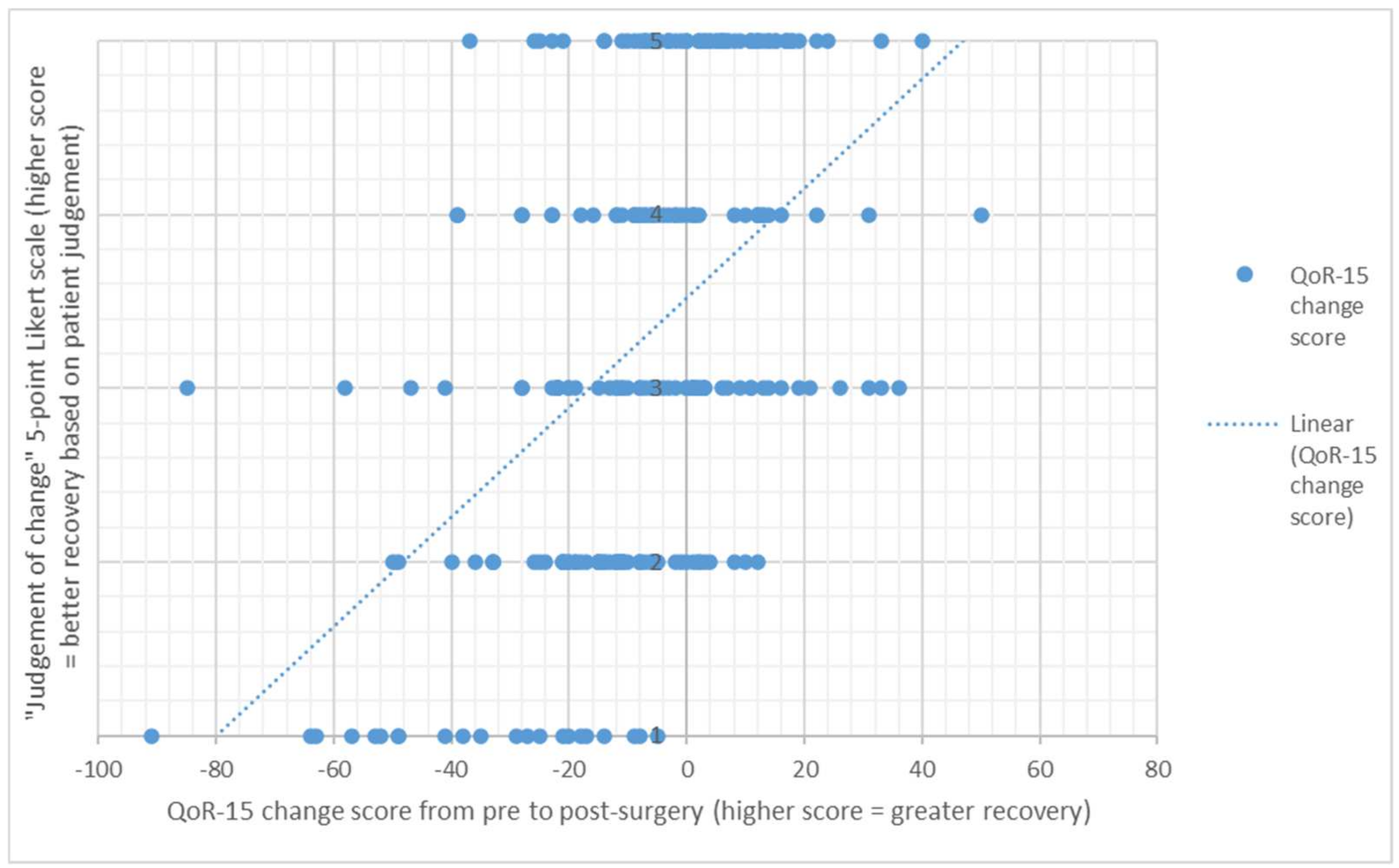
| Likert Scale | From Pre to One Week Post-Surgery | From Pre to Four Weeks Post-Surgery | ||
|---|---|---|---|---|
| Number | Mean (SD) | Number | Mean (SD) | |
| 1 = Worse | 23 | −38.7 (25.9) | 9 | −21.7 (24.8) |
| 2 = A little worse | 59 | −13.6 (12.9) | 15 | −12.5 (16.5) |
| 3 = Much the same | 57 | −5.7 (21.2) | 57 | −2.1 (21.5) |
| 4 = A little better | 44 | −2.8 (16.9) | 38 | 0.1 (15.1) |
| 5 = Better | 64 | 2.9 (13.9) | 122 | 8.2 (18.2) |
| Number | Correlation Coefficient # | p Value | |
|---|---|---|---|
| EQ-5D: Personal Care, and QoR-15: Personal toilet and hygiene | 412 | −0.414 | p < 0.001 |
| EQ-5D: Usual Activities, and QoR-15: Usual Activities | 401 | −0.717 | p < 0.001 |
| EQ-5D: Pain, and QoR-15: Moderate Pain | 404 | −0.677 | p < 0.001 |
| EQ-5D: Pain, and QoR-15: Severe Pain | 400 | −0.660 | p < 0.001 |
| EQ-5D: Anxiety/Depression, and QoR-15: Worried or Anxious | 398 | −0.718 | p < 0.001 |
| EQ-5D: Anxiety/Depression, and QoR-15: Sad or Depressed | 398 | −0.766 | p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Morris, M.E.; Atkinson, V.; Woods, J.; Myles, P.S.; Hodge, A.; Jones, C.H.; Lloyd, D.; Rovtar, V.; Clifford, A.M.; Brusco, N.K. Patient Judgement of Change with Elective Surgery Correlates with Patient Reported Outcomes and Quality of Life. Healthcare 2022, 10, 999. https://doi.org/10.3390/healthcare10060999
Morris ME, Atkinson V, Woods J, Myles PS, Hodge A, Jones CH, Lloyd D, Rovtar V, Clifford AM, Brusco NK. Patient Judgement of Change with Elective Surgery Correlates with Patient Reported Outcomes and Quality of Life. Healthcare. 2022; 10(6):999. https://doi.org/10.3390/healthcare10060999
Chicago/Turabian StyleMorris, Meg E., Victoria Atkinson, Jeffrey Woods, Paul S. Myles, Anita Hodge, Cathy H. Jones, Damien Lloyd, Vincent Rovtar, Amanda M. Clifford, and Natasha K. Brusco. 2022. "Patient Judgement of Change with Elective Surgery Correlates with Patient Reported Outcomes and Quality of Life" Healthcare 10, no. 6: 999. https://doi.org/10.3390/healthcare10060999
APA StyleMorris, M. E., Atkinson, V., Woods, J., Myles, P. S., Hodge, A., Jones, C. H., Lloyd, D., Rovtar, V., Clifford, A. M., & Brusco, N. K. (2022). Patient Judgement of Change with Elective Surgery Correlates with Patient Reported Outcomes and Quality of Life. Healthcare, 10(6), 999. https://doi.org/10.3390/healthcare10060999







