Abstract
Pregnancy is characterized by hormonal and physiological changes; some of these changes cause changes in sleep, presenting excessive sleep in early pregnancy due to the action of progesterone, and difficulty sleeping at the end of pregnancy due to weight gain and frequency of urination. Objective: to identify and systematize the evidence on the association between sleep quality and perinatal depression in pregnant and postpartum women. Methods: an integrative literature review was carried out with a search in the CINAHL, MEDLINE, and SCOPUS databases using the PRISMA flowchart. Results: Of the 92 articles, 10 studies were included according to the eligibility criteria. Results indicate that poor sleep quality during pregnancy is predictive of prenatal and postnatal depression. Sleep quality worsens with increasing gestational and maternal age. Conclusions: Sleep quality during pregnancy is associated with perinatal depression, a global public health problem with high prevalence. Due to its severe consequences for women, children, and families, perinatal depression needs to be identified early, preferably during pregnancy or soon after childbirth, justifying the priority of screening and prevention.
1. Introduction
Perinatal depression is a global public health problem with an estimated prevalence of 11.9% (95% CI, 11.4–12.5) according to a metaregression that included 96 studies [1]. Although the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) requires that the specifier “peripartum” in depression be necessary for depression to occur during pregnancy or in the first four weeks postpartum, most experts in the field still define postpartum depression as occurring at any time in the first postpartum year regardless of the time of onset [2]. Thus, perinatal depression is defined as depressive symptoms that occur during pregnancy and those that continue or start in the first year postpartum [2]. Depression in pregnancy is highly likely to persist after childbirth if it is not diagnosed and treated on time [3]. Mood changes characterize this depressive disorder, decreased self-esteem, concentration, energy, increased tension, agitation, pessimism, guilt, ideas of self-mutilation, sleep disturbances, and weight changes [4]. Perinatal depression profoundly impacts the mother, child, and the rest of the family. For example, it has a negative effect on the child’s neurocognitive development, mainly when maternal depression occurs during the first year of life [5]. In addition, the parents’ experience causes family fractures and frustration related to what they consider to be the ideal paternity [4]. Clinically, sleep quality may be associated with an increased risk of perinatal depression [6]. Poor sleep quality is frequent during the prenatal period. In a study with 2427 pregnant women that aimed to characterize their sleep patterns and sleep problems in all months of their pregnancy, 76% of the women had poor sleep quality during pregnancy [7]. However, because sleep difficulty is assumed to be a common and temporary complication in pregnancy, few studies have effectively investigated sleep quality during pregnancy and its consequences. Thus, the objective of the present review is to identify and systematize the evidence on the association between sleep quality and perinatal depression in pregnant and postpartum women.
2. Materials and Methods
The integrative literature review can contribute to the discipline of nursing, namely, to the development of theory and with direct applicability to health practice and policies. It enables the synthesis of generalized knowledge on a given topic, presenting different perspectives and consequently identifying knowledge gaps [8]. Thus, the integrative literature aims to synthesize the results of research or theory using narrative analysis [9]. Several methods have been developed to elaborate literature reviews, and they continue to evolve rigor to the complexity of conducting an exhaustive and complete review. Integrative reviews allow for broader research, with an assortment of purposes and the potential to comprehensively portray complex concepts, theories, or health problems relevant to Nursing [8]. This review was based on the methodology of Whittemore and Knafl [8], which is structured as follows: problem identification; elaboration of the review question, definition of the research strategy with the description of inclusion and exclusion criteria for studies, categorization of studies to be included in the review, data analysis, and knowledge synthesis. To synthesize the knowledge of this review, narrative analysis was performed [9].
2.1. Review Question
Considering the theme, the following review question was defined: what is the association between sleep quality and perinatal depression (O) in pregnant women and women in the postpartum period (P)?
Adapted from the PICO acronym, we used PO: P = population—pregnant women and women in the postpartum period; O = phenomenon outcome—sleep quality and perinatal depression.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria of the studies were: (1) studies that included pregnant participants and women in the postpartum period; (2) studies that included the sleep quality result measured by the Pittsburgh Sleep Quality Index and the assessment of depressive symptoms measured by the Edinburgh Postpartum Depression Scale, also admitting studies that included other measurement instruments as long as at least one of those was the Pittsburgh Sleep Quality Index or the Edinburgh Postpartum Depression Scale. As exclusion criteria, we defined: (1) studies whose participants were pregnant women with a depressive illness diagnosed before pregnancy, and (2) studies in which the exposure of interest was sleep respiratory pathology.
2.3. Search Strategy
A three-phase search was carried out: (1) a comprehensive and exploratory search on PubMed to identify evidence on the subject and consequently identify the most used terms for the further development of the search strategy; (2) an exhaustive search in the following databases (via the EBSCO service): Cumulative Index to Nursing and Allied Health Literature (CINAHL) Plus with Full Text, Medical Literature Analysis and Retrieval System Online (MEDLINE) with full Text, and SCOPUS; (3) the bibliographic references of the included studies were screened to identify possible studies of interest on athematic studies that were not screened in the performed search. The search formulas were adapted to each database as shown in Table 1. As limitations, we present the inclusion of studies that offered an available abstract in Portuguese and English, published between 2016 and 2021. and analyzed by peers.

Table 1.
Databases and research strategy.
2.4. Selection of Studies
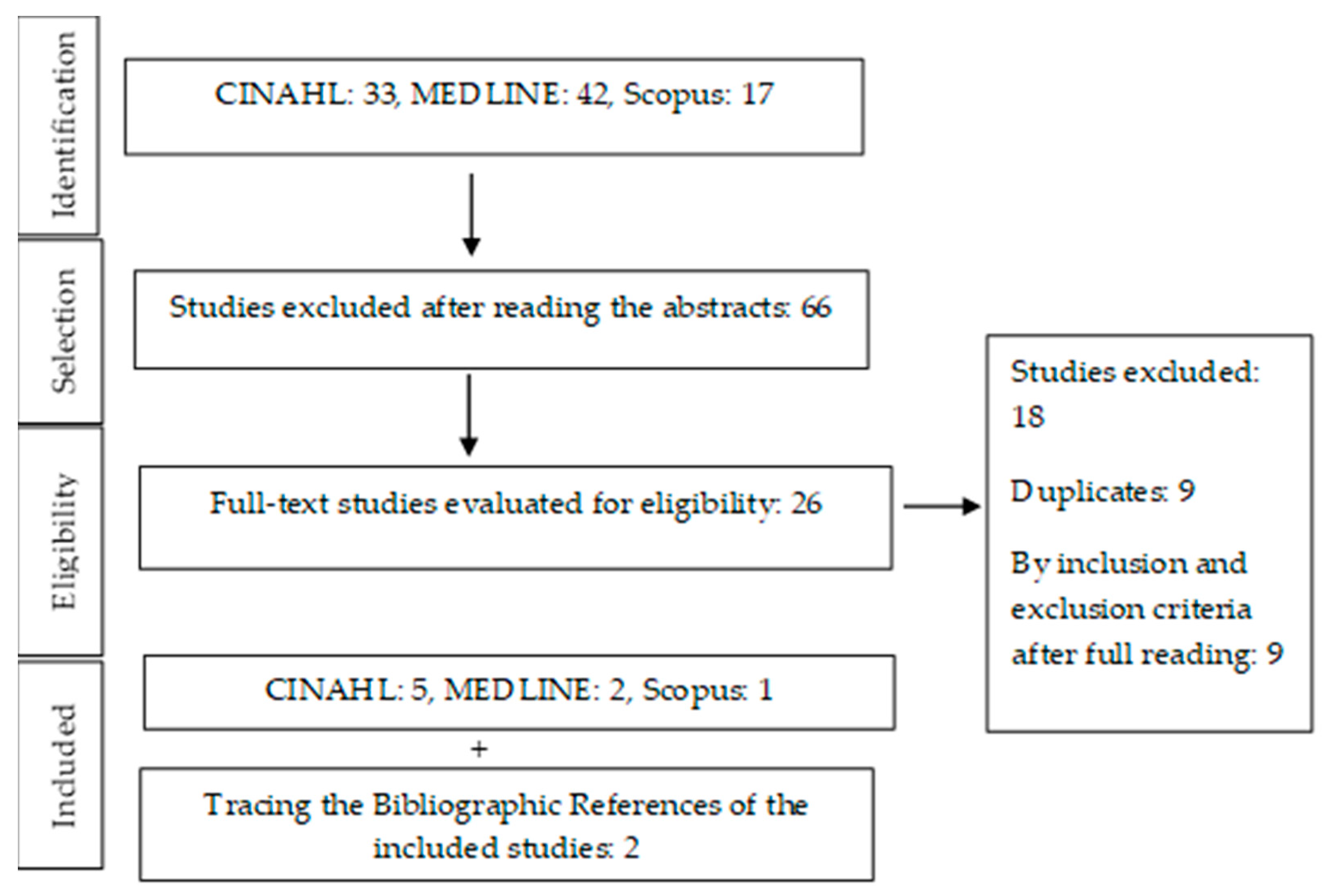
For the selection of studies, two reviewers read the titles and abstracts in an initial phase. These potentially relevant studies were then read in full, and selected according to the inclusion and exclusion criteria. In the absence of disagreement, including a third reviewer was unnecessary. The PRISMA flow diagram for determining articles for review is shown in Figure 1.
Figure 1.
PRISMA flow diagram for selecting articles for review.
2.5. Data Extraction
For data extraction, an instrument was built that addressed the following topics: title, author, and year; periodical; type of study and level of evidence; objective; and main results. In interpreting the results, similarities were identified, and a synthesis of knowledge was carried out considering the main results of the included studies that answered the review question.
2.6. Methodological Quality Assessment
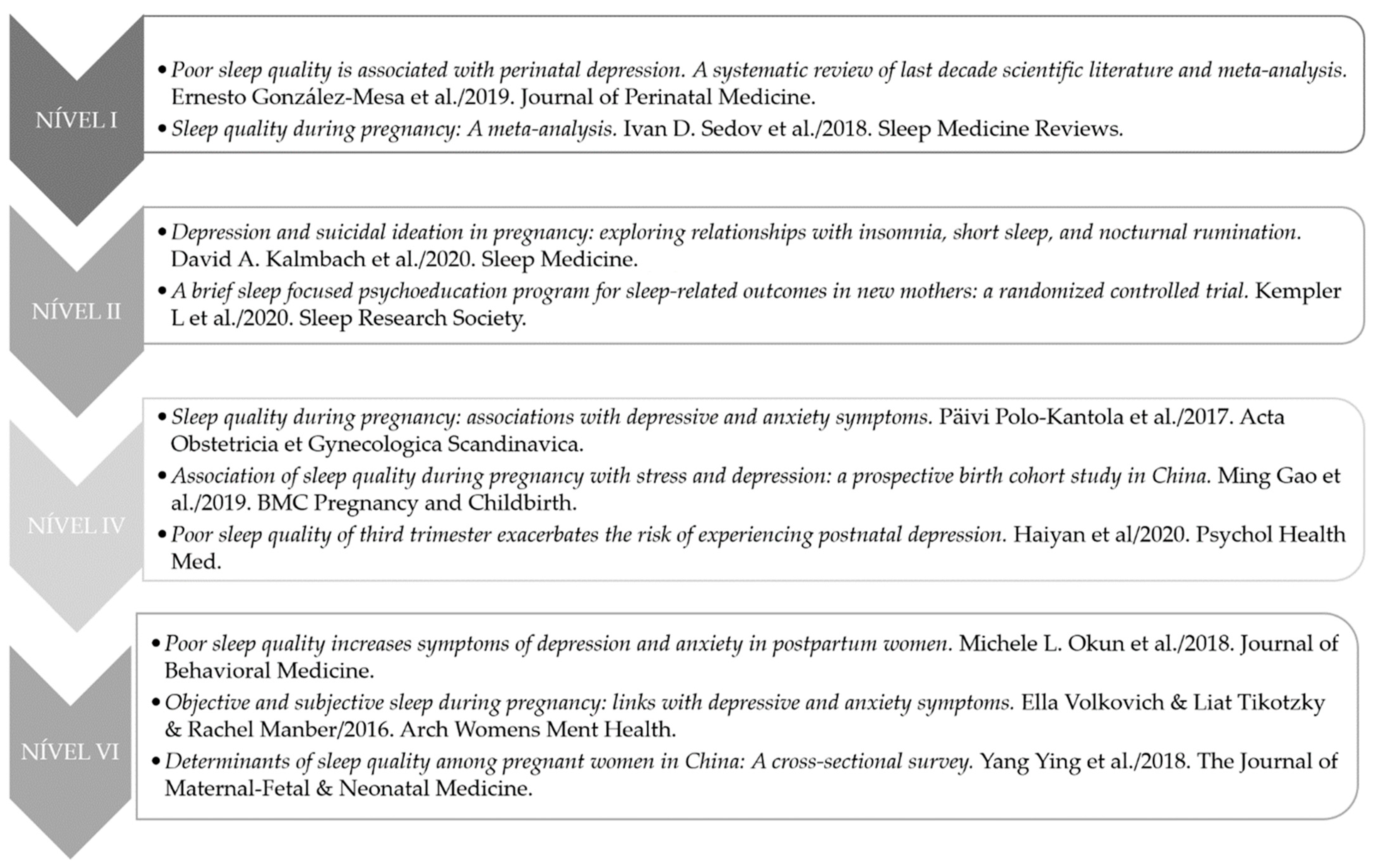
The selected articles were evaluated according to the level of evidence that they presented according to the hierarchical classification of evidence by Melnyk and Fineout-Overholt [10]: Level I—systematic review or meta-analysis; Level II—randomized controlled and well-delimited clinical trials; Level III—controlled clinical trials without randomization; Level IV—case–control studies and cohort studies; Level V—systematic, descriptive, and qualitative review studies; Level VI—descriptive or qualitative studies; Level VII—opinion of authorities and/or expert committee reports. Figure 2 shows the systematization of the included studies according to the hierarchical level of scientific evidence.
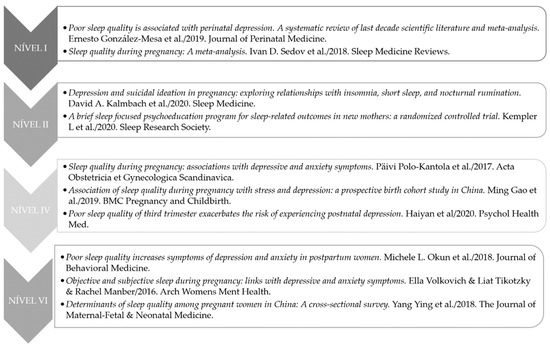
Figure 2.
Included studies according to the hierarchical level of scientific evidence [11,12,13,14,15,16,17,18,19,20].
3. Results
The main results extracted from the included studies in this integrative literature review are presented in Table 2.

Table 2.
Summary of the results of the included studies.
4. Discussion
One of the first questions that arise is the accuracy of the definition of sleep quality itself when assessing sleep quality. This is because there is, in fact, a set of indicators of good sleep, that is, a group of objectively identifiable indicators of sleep characteristics underlying its quality. However, there are also subjective sleep quality factors that greatly influence individual sleep satisfaction [11]. The present review found that the most frequently used instrument to assess sleep quality is the Pittsburgh/Pittsburgh Sleep Quality Index. Quality Index (PSQI). However, it may be necessary for the pregnant population to adjust the previously validated cutoff score (≥5) for the classification of poor sleep quality, and a higher score may be necessary to differentiate those who need further assessment and intervention. The physiological changes of pregnancy causing difficulty in sleeping complicate determining what pregnant women should expect regarding the need for additional assessment and treatment [12].
Poor sleep quality was significantly associated with increased symptoms of depression and anxiety [18]. Studies show that sleep quality during pregnancy is associated with prenatal stress and depression [11,13,15,21]. Pregnancy is described as stressful for many women, and stress-related disorders such as insomnia and depression are highly prevalent in this period [13]. Although insomnia is considered to be an independent disorder, insomnia and depression are associated during the perinatal period [22].
Sleep quality worsens with increasing gestational and maternal age [15,16,20]. An experimental study carried out on 267 pregnant women found that pregnant women from the second half of their pregnancy onwards had higher levels of insomnia, nocturnal rumination, depression, and suicidal tendencies [13]. Sleep quality worsens as the pregnancy progresses, worsening in the last trimester [15,20]. In addition, the quality of sleep declines with increasing age [22]. In one study, pregnant women aged 30 and over were found to experience poorer sleep quality than that of pregnant women under 30. Pregnant women aged 30 or over are also more likely to experience stress and depressive symptoms during pregnancy, which probably increases the risk of postpartum depression [16].
Results indicate that poor sleep quality is expected during pregnancy [19] and may be a vital intervention target, as disturbed sleep is predictive of postpartum depression and sleep disturbances [12,23]. The meta-analysis that quantified the prevalence of poor sleep quality during pregnancy concluded that it is necessary to identify women who need treatment, and to develop and provide evidence on appropriate interventions [12]. The poor quality of prenatal sleep seems to be related to the poor quality of postnatal sleep, which can consequently increase depressive symptoms after childbirth [17]. However, few studies report on the potential role of postnatal sleep quality, and its relationship with prenatal sleep and perinatal depression [17]. Thus, future investigations should compare sleep patterns in pregnancy, and after childbirth and perinatal depression. Further studies are also necessary to understand the efficiency of exercise programs specialized for postpartum women who may be vulnerable to depression, since exercises such as Pilates improve the quality of sleep in pregnant women [24]. Women undergoing treatment for insomnia during the third trimester of pregnancy reported less symptomatology of postpartum depression than those who did not receive treatment, thus suggesting a link between sleep quality during pregnancy and perinatal depression [25]. There are also studies on mobile phone use as a strategy for treating perinatal depressive symptoms [26], which could be an advantage for rural areas with less access to health services.
Depressed pregnant women are not only underdiagnosed but also reluctant to seek help. So, it is essential to identify variables that may reveal prenatal symptoms of depression, and this can be an effective strategy to signal women who need additional care throughout the perinatal period [22]. In addition, prenatal depression is a significant risk factor for postpartum depression [27]. The association between poor sleep quality and perinatal depression leads to clinical complications, so specialist nurses in the field of maternal and obstetric health, and obstetricians should identify sleep quality in routine prenatal tests performed, thus avoiding the development of mood pathologies [11,14]. The American College of Obstetricians and Gynecologists (ACOG) recommends screening for depression and anxiety symptoms at least once during pregnancy and postpartum [28]. The literature shows that, as pregnancy progresses, sleep-related problems such as insomnia, daytime sleepiness, and poor sleep quality increase [29]. Pregnant women experience stress, anxiety, and depressive symptoms rising from 24 weeks to postpartum [30]. During regular prenatal care, signs of insomnia, difficulty in managing mental stress, and excessive preoccupation with pregnancy should be ruled out to reduce the rates of clinical depression and suicidal ideation [13]. Several studies presented the nonuse of objective measures to assess sleep quality as a limitation, so whenever possible, actigraphy should be included in the methodology of future studies [13,15,16,17,18]. The very meaning of sleep quality is still difficult to understand by subjective measures of women’s sleep quality, which often only reflect individual satisfaction with sleep [31].
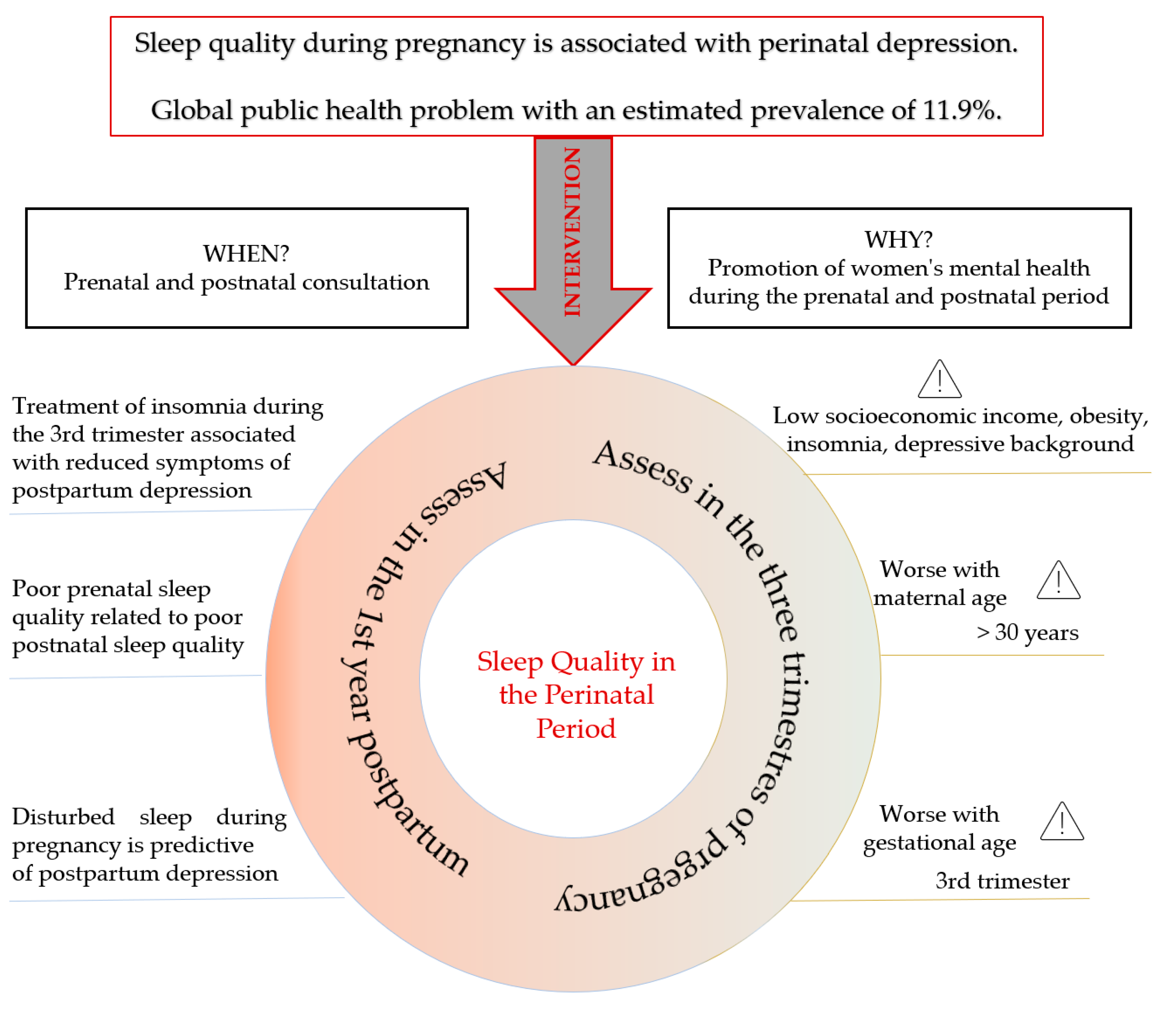
The present review has limitations: most of the included studies were carried out in China, which could bias the results for the culture and practices in that region of the globe. Multiculturalism influences sleep patterns, so the particularities of the target population to whom care is provided should be considered when extrapolating the results of this review. Two secondary studies were included that summarize many primary studies on the subject. For this reason, the primary studies that constituted these meta-analyses were not included in this review. On the basis of the interpretation and synthesis of the identified evidence, a construct is presented with the particularities to be considered during prenatal and postnatal evaluation by health professionals in maternal and obstetric health (Figure 3).
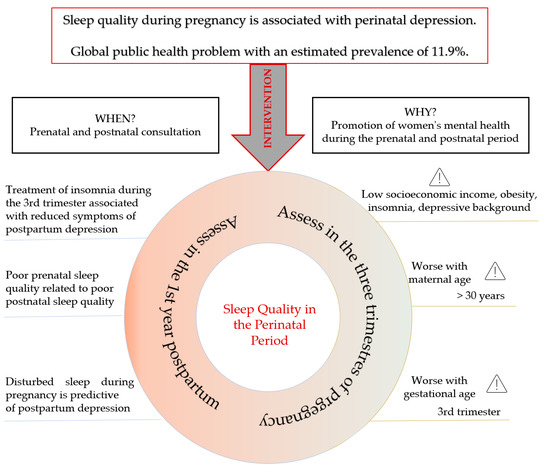
Figure 3.
Construct of the synthesis of evidence on the association between sleep quality and perinatal depression.
5. Conclusions
Due to its severe consequences for women, children, and families, perinatal depression needs to be identified early, preferably during pregnancy or soon after childbirth, justifying the priority of screening and prevention. This review found that the issue of sleep quality has been explored for its relevance as a protective factor for mental health. Regarding health and the implementation of good practices in detecting signs and situations of risk, it is essential to emphasize the relevance of interventions that promote mental health in pregnancy. During pregnancy, poor sleep quality increases the risk of perinatal depression, even controlling for risk factors such as psychological distress and stress. Treatments for prenatal sleep should be explored, such as stress reduction using mindfulness and/or psychoeducational programs.
Author Contributions
Conceptualization, A.F.P. and M.O.Z.; methodology, A.F.P. and M.O.Z.; formal analysis, A.F.P. and M.O.Z.; investigation, A.F.P. and M.O.Z.; data curation, A.F.P. and M.O.Z.; writing—original draft preparation, A.F.P. and M.O.Z.; writing—review and editing, A.F.P. and M.O.Z.; project administration, A.F.P. and M.O.Z.; Funding acquisition, M.O.Z. All authors have read and agreed to the published version of the manuscript.
Funding
The present publication was funded by Fundação Ciência e Tecnologia, IP national support through CHRC (UIDP/04923/2020).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Woody, C.A.; Ferrari, A.J.; Siskind, D.J.; Whiteford, H.A.; Harris, M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017, 219, 86–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stuart-Parrigon, K.; Stuart, S. Perinatal depression: An update and overview. Curr. Psychiatry Rep. 2014, 16, 468. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- General Directorate of Health [PT]. Directorate of Psychiatry and Mental Health Services. Mental Health Promotion in Pregnancy and Early Childhood: Guidance Manual for Health Professionals; General Directorate of Health: Lisbon, Portugal, 2005. [Google Scholar]
- Beestin, L.; Hugh-Jones, S.; Gough, B. The impact of maternal postnatal depression on men and their ways of fathering: An interpretive phenomenological analysis. Psychol. Health 2014, 29, 717–735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, L. The impact of postnatal depression on infant development. J. Child Psychol. Psychiatry 1992, 33, 543–561. [Google Scholar] [CrossRef]
- Palagini, L.; Gemignani, A.; Banti, S.; Manconi, M.; Mauri, M.; Riemann, D. Chronic sleep loss during pregnancy as a determinant of stress: Impact on pregnancy outcome. Sleep Med. 2014, 15, 853–859. [Google Scholar] [CrossRef]
- Mindell, J.A.; Cook, R.A.; Nikolovski, J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015, 16, 483–488. [Google Scholar] [CrossRef]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs. 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Whittemore, R.; Chao, A.; Jang, M.; Minges, K.E.; Park, C. Methods for knowledge synthesis: An overview. Heart Lung 2014, 43, 453–461. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Fineout-overholt, E. Evidence-Based Practice in Nursing & Healthcare. A Guide to Best Practice; Lippincot Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
- González-Mesa, E.; Cuenca-Marín, C.; Suarez-Arana, M.; Tripiana-Serrano, B.; Ibrahim-Díez, N.; Gonzalez-Cazorla, A.; Blasco-Alonso, M. Poor sleep quality is associated with perinatal depression. A systematic review of the last decade scientific literature and meta-analysis. J. Perinat. Med. 2019, 47, 689–703. [Google Scholar] [CrossRef]
- Sedov, I.D.; Cameron, E.E.; Madigan, S.; Tomfohr-Madsen, L.M. Sleep quality during pregnancy: A meta-analysis. Sleep Med. Rev. 2018, 38, 168–176. [Google Scholar] [CrossRef]
- Kalmbach, D.A.; Cheng, P.; Ong, J.C.; Ciesla, J.A.; Kingsberg, S.A.; Sangha, R.; Wanson, L.M.; O’Brien, L.M.; Roth, T.; Drake, C. Depression and suicidal ideation in pregnancy: Exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. 2020, 65, 62–73. [Google Scholar] [CrossRef] [PubMed]
- Kempler, L.; Sharpe, L.A.; Marshall, N.S.; Bartlett, D.J. A brief sleep focused psychoeducation program for sleep-related outcomes in new mothers: A randomized controlled trial. Sleep 2020, 43, zsaa101. [Google Scholar] [CrossRef] [PubMed]
- Polo-Kantola, P.; Aukia, L.; Karlsson, H.; Karlsson, L.; Paavonen, E.J. Sleep quality during pregnancy: Associations with depressive and anxiety symptoms. Acta Obstet. Gynecol. Scand. 2017, 96, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Hu, J.; Yang, L.; Ding, N.; Wei, X.; Li, L.; Liu, L.; Ma, Y.; Wen, D. Association of sleep quality during pregnancy with stress and depression: A prospective birth cohort study in China. BMC Pregnancy Childbirth 2019, 19, 444. [Google Scholar] [CrossRef] [Green Version]
- Zhou, H.; Li, W.; Ren, Y. Poor sleep quality of third trimester exacerbates the risk of experiencing postnatal depression. Psychol. Health Med. 2020, 25, 229–238. [Google Scholar] [CrossRef]
- Okun, M.L.; Mancuso, R.A.; Hobel, C.J.; Schetter, C.D.; Coussons-Read, M. Poor sleep quality increases symptoms of depression and anxiety in postpartum women. J. Behav. Med. 2018, 41, 703–710. [Google Scholar] [CrossRef]
- Volkovich, E.; Tikotzky, L.; Manber, R. Objective and subjective sleep during pregnancy: Links with depressive and anxiety symptoms. Arch. Womens Ment. Health 2016, 19, 173–181. [Google Scholar] [CrossRef]
- Yang, Y.; Mao, J.; Ye, Z.; Zeng, X.; Zhao, H.; Liu, Y.; Li, J.; Zheng, X. Determinants of sleep quality among pregnant women in China: A cross-sectional survey. J. Matern. Fetal Neonatal Med. 2018, 31, 2980–2985. [Google Scholar] [CrossRef]
- Eichler, J.; Schmidt, R.; Hiemisch, A.; Kiess, W.; Hilbert, A. Gestational weight gain, physical activity, sleep problems, substance use, and food intake as proximal risk factors of stress and depressive symptoms during pregnancy. BMC Pregnancy Childbirth 2019, 19, 175. [Google Scholar] [CrossRef] [Green Version]
- Osnes, R.S.; Eberhard-Gran, M.; Follestad, T.; Kallestad, H.; Morken, G.; Roaldset, J.O. Mid-Pregnancy Insomnia and its Association with Perinatal Depressive Symptoms: A prospective cohort study. Behav. Sleep Med. 2021, 19, 285–302. [Google Scholar] [CrossRef] [Green Version]
- Pietikäinen, J.T.; Polo-Kantola, P.; Pölkki, P.; Saarenpää-Heikkilä, O.; Paunio, T.; Paavonen, E.J. Sleeping problems during pregnancy-a risk factor for postnatal depression. Arch. Womens Ment. Health 2019, 22, 327–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hyun, A.-H.; Cho, J.-Y.; Koo, J.-H. Effect of Home-Based Tele-Pilates Intervention on Pregnant Women: A Pilot Study. Healthcare 2022, 10, 125. [Google Scholar] [CrossRef] [PubMed]
- Khazaie, H.; Ghadami, M.R.; Knight, D.C.; Emamian, F.; Tahmasian, M. Insomnia treatment in the third trimester of pregnancy reduces postpartum depression symptoms: A randomized clinical trial. Psychiatry Res. 2013, 210, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Dosani, A.; Arora, H.; Mazmudar, S. mHealth and Perinatal Depression in Low-and Middle-Income Countries: A Scoping Review of the Literature. Int. J. Environ. Res. Public Health 2020, 17, 7679. [Google Scholar] [CrossRef]
- Wisner, K.L.; Sit, D.K.Y.; McShea, M.C.; Rizzo, D.M.; Zoretich, R.A.; Hughes, C.L.; Eng, H.F.; Luther, J.F.; Wisniewski, S.; Costantino, M.L.; et al. Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum Women With Screen-Positive Depression Findings. JAMA Psychiatry 2013, 70, 490–498. [Google Scholar] [CrossRef]
- ACOG Committee. ACOG Committee Opinion No. 757: Screening for perinatal depression. Obstet. Gynecol. 2018, 132, e208–e212. [Google Scholar] [CrossRef]
- Warland, J.; Dorrian, J.; Morrison, J.L.; O’Brien, L.M. Maternal sleep during pregnancy and poor fetal outcomes: A scoping review of the literature with meta-analysis. Sleep Med. Rev. 2018, 41, 197–219. [Google Scholar] [CrossRef]
- Cheng, C.-Y.; Chou, Y.-H.; Chang, C.-H.; Liou, S.-R. Trends of Perinatal Stress, Anxiety, and Depression and Their Prediction on Postpartum Depression. Int. J. Environ. Res. Public Health 2021, 18, 9307. [Google Scholar] [CrossRef]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).