Upper-Limb Robot-Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study
Abstract
:1. Introduction
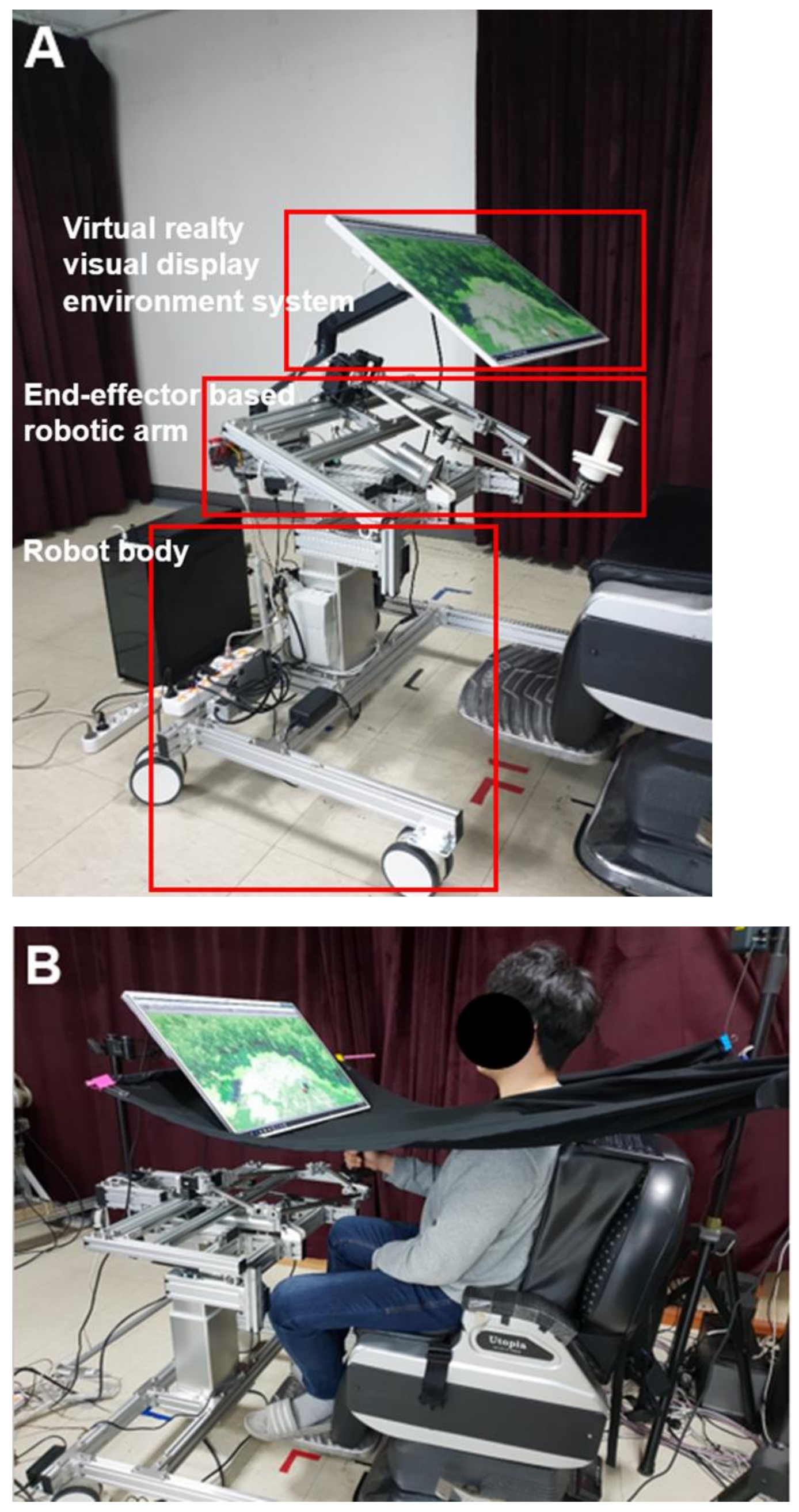
2. Materials and Methods
2.1. Subjects
2.2. Study Setting
2.3. Experimental Protocol
2.4. Evaluation Procedure
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. 2022. Available online: http://www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html (accessed on 11 June 2022).
- Dewald, J.P.; Beer, R.F. Abnormal joint torque patterns in the paretic upper limb of subjects with hemiparesis. Muscle Nerve Off. J. Am. Assoc. Electrodiagn. Med. 2001, 24, 273–283. [Google Scholar] [CrossRef]
- Hebert, D.; Lindsay, M.P.; McIntyre, A.; Kirton, A.; Rumney, P.G.; Bagg, S.; Bayley, M.; Dowlatshahi, D.; Dukelow, S.; Garnhum, M.; et al. Canadian stroke best practice recommendations: Stroke rehabilitation practice guidelines, update 2015. Int. J. Stroke 2016, 11, 459–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.Y.; Li, Y.; Lamontagne, A. The effects of error-augmentation versus error-reduction paradigms in robotic therapy to enhance upper extremity performance and recovery post-stroke: A systematic review. J. Neuroeng. Rehabil. 2018, 15, 1–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parker, V.M.; Wade, D.; Hewer, R.L. Loss of arm function after stroke: Measurement, frequency, and recovery. Int. Rehabil. Med. 1986, 8, 69–73. [Google Scholar] [CrossRef]
- Olsen, T.S. Arm and leg paresis as outcome predictors in stroke rehabilitation. Stroke 1990, 21, 247–251. [Google Scholar] [CrossRef] [Green Version]
- Abdollahi, F.; Abdollahi, F.; Rozario, S.V.; Kenyon, R.V.; Patton, J.L.; Case, E.; Kovic, M.; Listenberger, M. Arm control recovery enhanced by error augmentation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011. [Google Scholar]
- Norouzi-Gheidari, N.; Archambault, P.S.; Fung, J. Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: Systematic review and meta-analysis of the literature. J. Rehabil. Res. Dev. 2012, 49, 479–496. [Google Scholar] [CrossRef]
- Levin, M.F.; Kleim, J.A.; Wolf, S.L. What do motor “recovery” and “compensation” mean in patients following stroke? Neurorehabilit. Neural Repair. 2009, 23, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Maciejasz, P.; Eschweiler, J.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moggio, L.; de Sire, A.; Marotta, N.; Demeco, A.; Ammendolia, A. Exoskeleton versus end-effector robot-assisted therapy for finger-hand motor recovery in stroke survivors: Systematic review and meta-analysis. Top. Stroke Rehabil. 2021, 1–12. [Google Scholar] [CrossRef]
- Patton, J.L.; Stoykov, M.E.; Kovic, M.; Mussa-Ivaldi, F.A. Evaluation of robotic training forces that either enhance or reduce error in chronic hemiparetic stroke survivors. Exp. Brain Res. 2005, 168, 368–383. [Google Scholar] [CrossRef] [PubMed]
- Kao, P.-C.; Srivastava, S.; Agrawal, S.K.; Scholz, J.P. Effect of robotic performance-based error-augmentation versus error-reduction training on the gait of healthy individuals. Gait Posture 2013, 37, 113–120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozario, S.V.; Housman, S.; Kovic, M.; Kenyon, R.V.; Patton, J.L. Therapist-mediated post-stroke rehabilitation using haptic/graphic error augmentation. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009. [Google Scholar]
- Patton, J.L.; Kovic, M.; Mussa-Ivaldi, F.A. Custom-designed haptic training for restoring reaching ability to individuals with poststroke hemiparesis. J. Rehabil. Res. Dev. 2006, 43, 643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdollahi, F.; Case Lazarro, E.D.; Listenberger, M.; Kenyon, R.V.; Kovic, M.; Bogey, R.A.; Hedeker, D.; Jovanovic, B.D.; Patton, J.L. Error augmentation enhancing arm recovery in individuals with chronic stroke: A randomized crossover design. Neurorehabilit. Neural Repair 2014, 28, 120–128. [Google Scholar] [CrossRef]
- Kawato, M. Feedback-Error-Learning Neural Network for Supervised Motor Learning. In Advanced Neural Computers; Elsevier: Amsterdam, The Netherlands, 1990; pp. 365–372. [Google Scholar]
- Hsieh, Y.-W.; Lin, K.-C.; Wu, C.-Y.; Shih, T.-Y.; Li, M.-W.; Chen, C.-L. Comparison of proximal versus distal upper-limb robotic rehabilitation on motor performance after stroke: A cluster controlled trial. Sci. Rep. 2018, 8, 2091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, K.-H.; Song, W.-K. Effects of two different robot-assisted arm training on upper limb motor function and kinematics in chronic stroke survivors: A randomized controlled trial. Top. Stroke Rehabil. 2021, 28, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, J.; Bravo, G.; Hébert, R.; Dutil, É.; Mercier, L. Validation of the Box and Block Test as a measure of dexterity of elderly people: Reliability, validity, and norms studies. Arch. Phys. Med. Rehabil. 1994, 75, 751–755. [Google Scholar] [CrossRef]
- Yozbatiran, N.; Der-Yeghiaian, L.; Cramer, S.C. A Standardized Approach to Performing the Action Research Arm Test. Neurorehabilit. Neural Repair 2008, 22, 78–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hatem, S.M.; Saussez, G.; Della Faille, M.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [Green Version]
- Weber, L.M.; Stein, J. The use of robots in stroke rehabilitation: A narrative review. NeuroRehabilitation 2018, 43, 99–110. [Google Scholar] [CrossRef] [Green Version]
- Sage, G.H. Motor Learning and Control: A Neuropsychological Approach; Brown: Providence, RI, USA, 1984. [Google Scholar]
- Marchal-Crespo, L.; van Raai, M.; Rauter, G.; Wolf, P.; Riener, R. The effect of haptic guidance and visual feedback on learning a complex tennis task. Exp. Brain Res. 2013, 231, 277–291. [Google Scholar] [CrossRef] [Green Version]
- Marchal–Crespo, L.; Schneider, J.; Jaeger, L.; Riener, R. Learning a locomotor task: With or without errors? J. Neuroeng. Rehabil. 2014, 11, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schmidt, R.A.; Lee, T.D.; Winstein, C.; Wulf, G.; Zelaznik, H.N. Motor Control and Learning: A Behavioral Emphasis; Human kinetics: Champaign, IL, USA, 2018. [Google Scholar]
- Gilmore, P.E.; Spaulding, S.J. Motor control and motor learning: Implications for treatment of individuals post stroke. Phys. Occup. Ther. Geriatr. 2001, 20, 1–15. [Google Scholar] [CrossRef]
- Givon-Mayo, R.; Simons, E.; Ohry, A.; Karpin, H.; Israely, S.; Carmeli, E. A preliminary investigation of error enhancement of the velocity component in stroke patients’ reaching movements. Int. J. Ther. Rehabilitation 2014, 21, 160–168. [Google Scholar] [CrossRef]
- Liepert, J.; Bauder, H.; Miltner, W.H.R.; Taub, E.; Weiller, C. Treatment-Induced Cortical Reorganization After Stroke in Humans. Stroke 2000, 31, 1210–1216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Israely, S.; Carmeli, E. Error augmentation as a possible technique for improving upper extremity motor performance after a stroke—A systematic review. Top. Stroke Rehabil. 2016, 23, 116–125. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Mean ± SD or Number |
|---|---|
| Gender (male/female) | 20/7 |
| Paretic side (left/right) | 13/14 |
| Etiology (infarction/hemorrhage) | 16/11 |
| Brunnstrom stage (3/4/5/6) | 1/17/8/1 |
| MAS-UE (1/1+/2) | 6/16/5 |
| MRC-EF (3/4/5) | 5/8/14 |
| MRC-EE (3/4/5) | 5/7/15 |
| Age (years) | 54.51 ± 12.44 |
| Weight (kg) | 67.88 ± 11.54 |
| Height (cm) | 167.62 ± 7.31 |
| Onset duration (months) | 12.70 ± 5.78 |
| MMSE (scores) | 26.70 ± 3.97 |
| MBI (scores) | 90.33 ± 6.25 |
| Parameters | Pre-Intervention | Post-Intervention | ∆ Change | Z Values | p Values | |
|---|---|---|---|---|---|---|
| FMA | Total (max. 66) | 36.92 ± 13.62 | 38.55 ± 13.94 | 1.62 ± 1.88 | −3.562 | <0.000 |
| Proximal (max. 42) | 25.88 ± 7.74 | 27.11 ± 7.84 | 1.22 ± 1.64 | −3.203 | 0.001 | |
| Distal (max. 24) | 11.03 ± 7.61 | 11.29 ± 7.76 | 0.25 ± 1.58 | −0.962 | 0.336 | |
| BBT | 5.33 ± 7.65 | 5.92 ± 8.16 | 0.59 ± 1.42 | −2.032 | 0.042 | |
| ARAT (max. 57) | 16.96 ± 17.70 | 18.29 ± 17.14 | 1.33 ± 1.54 | −3.213 | 0.001 | |
| Parameters | Pre-Intervention | Post-Intervention | ∆ Change | Z Value | p Value | |
|---|---|---|---|---|---|---|
| Time (s) | IL | 3.94 ± 1.60 | 2.94 ± 1.08 | −0.99 ± 1.07 | −4.036 | <0.000 |
| Me | 4.17 ± 1.70 | 2.93 ± 0.92 | −1.24 ± 1.07 | −4.325 | <0.000 | |
| CL | 3.68 ± 1.43 | 3.00 ± 1.25 | −0.68 ± 1.06 | −3.099 | 0.002 | |
| Speed (cm/s) | IL | 6.26 ± 3.80 | 8.28 ± 4.14 | 2.02 ± 3.60 | −3.137 | 0.002 |
| Me | 6.76 ± 4.02 | 8.93 ± 4.80 | 2.16 ± 3.95 | −3.195 | 0.001 | |
| CL | 7.48 ± 5.55 | 9.98 ± 5.44 | 2.49 ± 4.15 | −3.243 | 0.001 | |
| Distance (cm) | IL | 15.09 ± 7.73 | 17.52 ± 7.27 | 2.42 ± 5.52 | −3.555 | <0.000 |
| Me | 17.00 ± 8.06 | 19.59 ± 7.98 | 2.58 ± 5.66 | −3.070 | 0.002 | |
| CL | 19.81 ± 11.47 | 22.46 ± 10.63 | 2.65 ± 6.85 | −3.559 | <0.000 | |
| CR | IL | 0.61 ± 0.17 | 0.71 ± 0.13 | 0.09 ± 0.13 | −2.246 | 0.025 |
| Me | 0.61 ± 0.18 | 0.70 ± 0.13 | 0.08 ± 0.15 | −1.970 | 0.049 | |
| CL | 0.61 ± 0.17 | 0.71 ± 0.12 | 0.09 ± 0.14 | −2.499 | 0.012 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, K.-H.; Hong, M.-R.; Song, W.-K. Upper-Limb Robot-Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study. Healthcare 2022, 10, 1186. https://doi.org/10.3390/healthcare10071186
Cho K-H, Hong M-R, Song W-K. Upper-Limb Robot-Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study. Healthcare. 2022; 10(7):1186. https://doi.org/10.3390/healthcare10071186
Chicago/Turabian StyleCho, Ki-Hun, Mi-Ran Hong, and Won-Kyung Song. 2022. "Upper-Limb Robot-Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study" Healthcare 10, no. 7: 1186. https://doi.org/10.3390/healthcare10071186
APA StyleCho, K.-H., Hong, M.-R., & Song, W.-K. (2022). Upper-Limb Robot-Assisted Therapy Based on Visual Error Augmentation in Virtual Reality for Motor Recovery and Kinematics after Chronic Hemiparetic Stroke: A Feasibility Study. Healthcare, 10(7), 1186. https://doi.org/10.3390/healthcare10071186






