The Role of Village Doctors in Residents’ Uptake of Eye Screening: Evidence from Ageing Residents in Rural China
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Sampling
2.3. Data Collection and Measurement
2.4. Ethical Approval
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Residents and Village Doctors
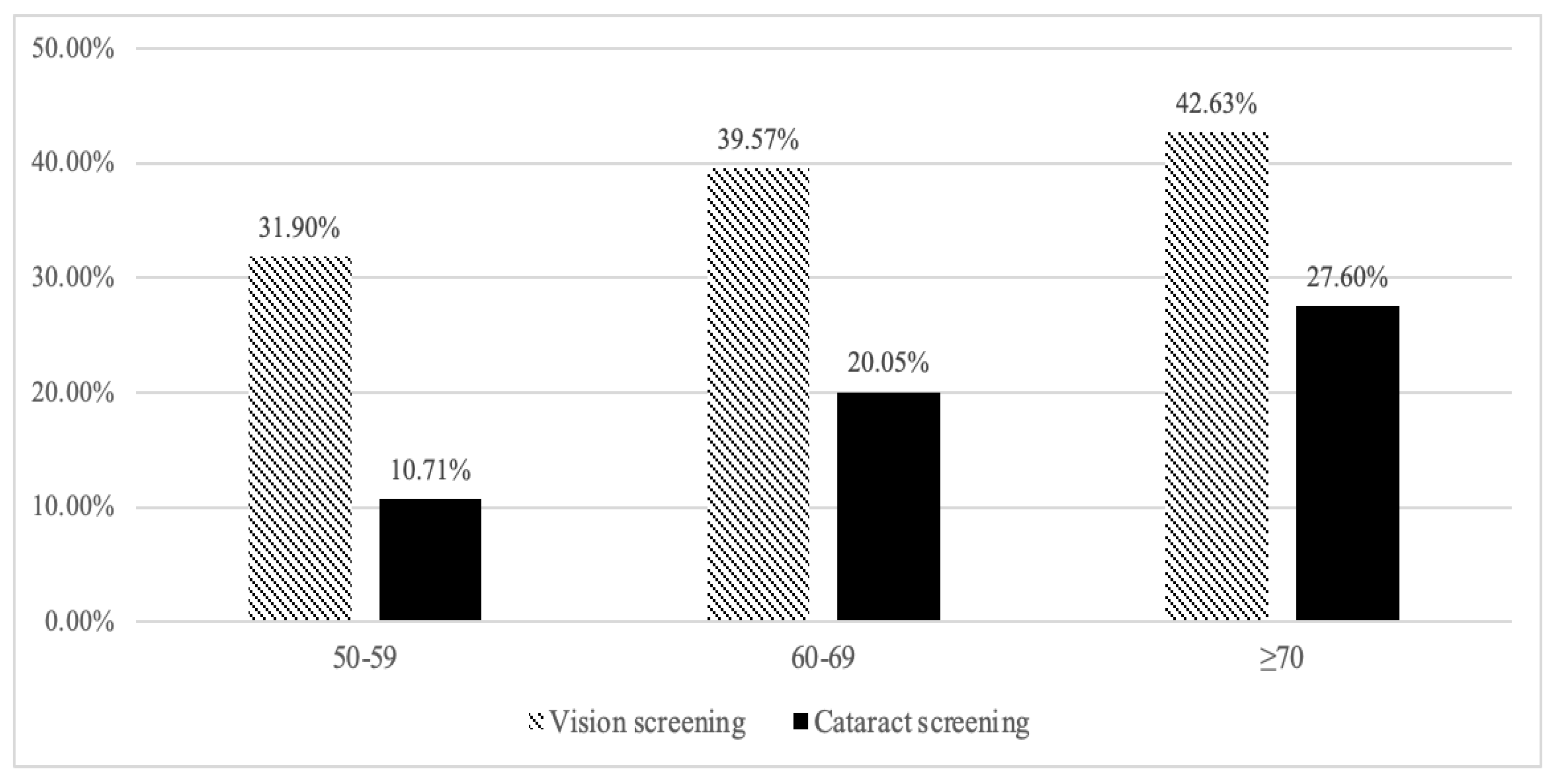
3.2. Uptake Rate of Residents’ Vision Screening and Cataract Screening
3.3. Determinants of Residents’ Uptake of Vision Screening
3.4. Determinants of Residents’ Uptake of Cataract Screening
3.5. Residents’ and Village Doctors’ Knowledge about Cataracts
3.6. Village Doctors’ Willingness and Attitude towards Providing Eye Screening Services
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Report on Vision; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-000857-0. [Google Scholar]
- Lewallen, S.; Tungpakorn, N.C.; Kim, S.-H.; Courtright, P. Progression of Eye Disease in “Cured” Leprosy Patients: Implications for Understanding the Pathophysiology of Ocular Disease and for Addressing Eyecare Needs. Br. J. Ophthalmol. 2000, 84, 817–821. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Taylor, H.R.; Anjou, M.D. Cataract Surgery and Indigenous Eye Care: A Review. Clin. Exp. Ophthalmol. 2020, 48, 512–516. [Google Scholar] [CrossRef]
- Asbell, P.A.; Dualan, I.; Mindel, J.; Brocks, D.; Ahmad, M.; Epstein, S. Age-Related Cataract. Lancet 2005, 365, 599–609. [Google Scholar] [CrossRef]
- Song, P.; Wang, H.; Theodoratou, E.; Chan, K.Y.; Rudan, I. The National and Subnational Prevalence of Cataract and Cataract Blindness in China: A Systematic Review and Meta-Analysis. J. Glob. Health 2018, 8, 010804. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.-F.; Liu, H.-R.; Zhang, Y.; Bai, W.-L.; Li, R.-Y.; Sun, R.-Z.; Wang, N.-L. Prevalence of Cataract and Cataract Surgery in Urban and Rural Chinese Populations over 50 Years Old: A Systematic Review and Meta-Analysis. Int. J. Ophthalmol. 2022, 15, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Zhu, J.; Zou, H.; He, X.; Zhao, R.; Lu, L. Analysis of Cataract Surgical Rate and Its Influencing Factors in Shanghai, China. Natl. Med. J. China 2013, 93, 3737. [Google Scholar] [CrossRef]
- Polack, S.; Kuper, H.; Mathenge, W.; Fletcher, A.; Foster, A. Cataract Visual Impairment and Quality of Life in a Kenyan Population. Br. J. Ophthalmol. 2007, 91, 927–932. [Google Scholar] [CrossRef]
- Polack, S.; Kuper, H.; Eusebio, C.; Mathenge, W.; Wadud, Z.; Foster, A. The Impact of Cataract on Time-Use: Results from a Population Based Case-Control Study in Kenya, the Philippines and Bangladesh. Ophthalmic Epidemiol. 2008, 15, 372–382. [Google Scholar] [CrossRef]
- He, M.; Wang, W.; Huang, W. Variations and Trends in Health Burden of Visual Impairment due to Cataract: A Global Analysis. Investig. Ophthalmol. Vis. Sci. 2017, 58, 4299–4306. [Google Scholar] [CrossRef]
- Arun, C.S.; Al-Bermani, A.; Stannard, K.; Taylor, R. Long-Term Impact of Retinal Screening on Significant Diabetes-Related Visual Impairment in the Working Age Population. Diabet. Med. 2009, 26, 489–492. [Google Scholar] [CrossRef]
- Burton, M.J.; Ramke, J.; Marques, A.P.; Bourne, R.R.A.; Congdon, N.; Jones, I.; Tong, B.A.M.A.; Arunga, S.; Bachani, D.; Bascaran, C.; et al. The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. Lancet Glob. Health 2021, 9, e489–e551. [Google Scholar] [CrossRef]
- Strahlman, E.; Ford, D.; Whelton, P.; Sommer, A. Vision Screening in a Primary Care Setting: A Missed Opportunity? Arch. Intern. Med. 1990, 150, 2159–2164. [Google Scholar] [CrossRef] [PubMed]
- Baruwa, E.; Tzu, J.; Congdon, N.; He, M.; Frick, K.D. Reversal in Gender Valuations of Cataract Surgery after the Implementation of Free Screening and Low-Priced High-Quality Surgery in a Rural Population of Southern China. Ophthalmic Epidemiol. 2008, 15, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zupan, N.J.; Shiyanbola, O.O.; Swearingen, R.; Carlson, J.N.; Jacobson, N.A.; Mahoney, J.E.; Klein, R.; Bjelland, T.D.; Smith, M.A. Factors Influencing Patient Adherence with Diabetic Eye Screening in Rural Communities: A Qualitative Study. PLoS ONE 2018, 13, e0206742. [Google Scholar] [CrossRef]
- Zhang, X.J.; Jhanji, V.; Leung, C.K.-S.; Li, E.Y.; Liu, Y.; Zheng, C.; Musch, D.C.; Chang, D.F.; Liang, Y.B.; Lam, D.S.C. Barriers for Poor Cataract Surgery Uptake among Patients with Operable Cataract in a Program of Outreach Screening and Low-Cost Surgery in Rural China. Ophthalmic Epidemiol. 2014, 21, 153–160. [Google Scholar] [CrossRef]
- Babiarz, K.S.; Yi, H.; Luo, R. Meeting the Health-Care Needs of the Rural Elderly: The Unique Role of Village Doctors. China World Econ. 2013, 21, 44–60. [Google Scholar] [CrossRef]
- Chen, Y.; Sylvia, S.; Wu, P.; Yi, H. Explaining the Declining Utilization of Village Clinics in Rural China over Time: A Decomposition Approach. Soc. Sci. Med. 2022, 301, 114978. [Google Scholar] [CrossRef]
- Li, T.; Lei, T.; Xie, Z.; Zhang, T. Determinants of Basic Public Health Services Provision by Village Doctors in China: Using Non-Communicable Diseases Management as an Example. BMC Health Serv. Res. 2016, 16, 42. [Google Scholar] [CrossRef]
- Yi, H.; Liu, H.; Wang, Z.; Xue, H.; Sylvia, S.; Shi, H.; Teuwen, D.E.; Han, Y.; Qin, J. The Competence of Village Clinicians in the Diagnosis and Management of Childhood Epilepsy in Southwestern China and Its Determinants: A Cross-Sectional Study. Lancet Reg. Health West. Pac. 2020, 3, 100031. [Google Scholar] [CrossRef]
- Sun, Y.; Mu, J.; Wang, D.W.; Ouyang, N.; Xing, L.; Guo, X.; Zhao, C.; Ren, G.; Ye, N.; Zhou, Y.; et al. A Village Doctor-Led Multifaceted Intervention for Blood Pressure Control in Rural China: An Open, Cluster Randomised Trial. Lancet 2022, 399, 1964–1975. [Google Scholar] [CrossRef]
- Xue, H.; Shi, Y.; Medina, A. Who Are Rural China’s Village Clinicians? China Agric. Econ. Rev. 2016, 8, 662–676. [Google Scholar] [CrossRef]
- National Health Commission of the People’s of Republic of China. 2021 Chinses Health Statistics Yearbook; China Union Medical University Press: Beijing, China, 2021; ISBN 978-7-5679-1835-1.
- Guo, W.; Sylvia, S.; Umble, K.; Chen, Y.; Zhang, X.; Yi, H. The Competence of Village Clinicians in the Diagnosis and Treatment of Heart Disease in Rural China: A Nationally Representative Assessment. Lancet Reg. Health West. Pac. 2020, 2, 100026. [Google Scholar] [CrossRef] [PubMed]
- Rao, S.; Xue, H.; Teuwen, D.E.; Shi, H.; Yi, H. Measurements of Quality of Village-Level Care and Patients’ Healthcare-Seeking Behaviors in Rural China. BMC Public Health 2021, 21, 1873. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Wang, H.; Yang, L.; Wang, H. Who Will Protect the Health of Rural Residents in China If Village Doctors Run Out? Aust. J. Prim. Health 2019, 25, 99–103. [Google Scholar] [CrossRef]
- China National Bureau of Statistics GDP per Capita in 2020. Available online: https://data.stats.gov.cn/search.htm?s=%E4%BA%BA%E5%9D%87GDP2020 (accessed on 6 September 2021).
- Camparini, M.; Cassinari, P.; Ferrigno, L.; Macaluso, C. ETDRS-Fast: Implementing Psychophysical Adaptive Methods to Standardized Visual Acuity Measurement with ETDRS Charts. Investig. Ophthalmol. Vis. Sci. 2001, 42, 1226–1231. [Google Scholar]
- Liu, Y.-C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef]
- Kuppala, J.; Falck, A.; Winblad, I.; Tuulonen, A. The Pyhäjärvi Cataract Study II. Criteria for Cataract Surgery. Acta Ophthalmol. 2012, 90, 327–333. [Google Scholar] [CrossRef]
- Alexander, R.L.; Miller, N.A.; Cotch, M.F.; Janiszewski, R. Factors That Influence the Receipt of Eye Care. Am. J. Health Behav. 2008, 32, 547–556. [Google Scholar] [CrossRef]
- Wang, D.; Ding, X.; He, M.; Yan, L.; Kuang, J.; Geng, Q.; Congdon, N. Use of Eye Care Services among Diabetic Patients in Urban and Rural China. Ophthalmology 2010, 117, 1755–1762. [Google Scholar] [CrossRef]
- Ehrlich, J.R.; Stagg, B.C.; Andrews, C.; Kumagai, A.; Musch, D.C. Vision Impairment and Receipt of Eye Care among Older Adults in Low- and Middle-Income Countries. JAMA Ophthalmol. 2019, 137, 146–158. [Google Scholar] [CrossRef]
- Anthony, O.; Ivy, O.; Maria, H.; Leticia, B.; Awedoba Albert, K. Eye Health Knowledge and Health-Seeking Behaviours in Ghana. Afr. Vis. Eye Health 2018, 77, 1–10. [Google Scholar] [CrossRef]
- Chen, T.; Jin, L.; Zhu, W.; Wang, C.; Zhang, G.; Wang, X.; Wang, J.; Yang, K.; Cochrane, G.M.; Lamoureux, E.L.; et al. Knowledge, Attitudes and Eye Health-Seeking Behaviours in a Population-Based Sample of People with Diabetes in Rural China. Br. J. Ophthalmol. 2021, 105, 806–811. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Lei, T.; Sun, F.; Xie, Z. Determinants of Village Doctors’ Job Satisfaction under China’s Health Sector Reform: A Cross-Sectional Mixed Methods Study. Int. J. Equity Health 2017, 16, 64. [Google Scholar] [CrossRef] [PubMed]
- Gu, L.; Zhu, R.; Li, Z.; Zhang, S.; Li, J.; Tian, D.; Sun, Z. Factors Associated with Rural Residents’ Contract Behavior with Village Doctors in Three Counties: A Cross-Sectional Study from China. Int. J. Environ. Res. Public Health 2020, 17, 8969. [Google Scholar] [CrossRef] [PubMed]
- De Souza, N.; Cui, Y.; Looi, S.; Paudel, P.; Shinde, L.; Kumar, K.; Berwal, R.; Wadhwa, R.; Daniel, V.; Flanagan, J.; et al. The Role of Optometrists in India: An Integral Part of an Eye Health Team. Indian J. Ophthalmol. 2012, 60, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Alshammari, F.; Shaikh, S.; Hussain, A.; Alafnan, A.; Almuzaini, I.; Alshammari, B. Public Awareness of Common Eye Diseases and the Role of Pharmacists in Raising This Awareness in Saudi Arabia: A Cross-Sectional Study. Healthcare 2021, 9, 692. [Google Scholar] [CrossRef]
- Briefing on the development of China Rural Eye Care Model. Available online: https://www.iapb.org/wp-content/uploads/07-Briefing-on-the-development-of-China-Rural-Eye-Care-Model-FHF.pdf (accessed on 7 June 2022).
- Ding, Y.; Smith, H.J.; Fei, Y.; Xu, B.; Nie, S.; Yan, W.; Diwan, V.K.; Sauerborn, R.; Dong, H. Factors Influencing the Provision of Public Health Services by Village Doctors in Hubei and Jiangxi Provinces, China. Bull. World Health Organ. 2013, 91, 64–69. [Google Scholar] [CrossRef]
- Zhao, X.; Liu, S.; Chen, Y.; Zhang, Q.; Wang, Y. Influential Factors of Burnout among Village Doctors in China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 2013. [Google Scholar] [CrossRef]

| Characteristics | N | Percent (%) |
|---|---|---|
| Characteristics of Residents (n = 1010) | ||
| Age (years) | ||
| 50–59 | 420 | 41.58 |
| 60–69 | 369 | 36.53 |
| ≥70 | 221 | 21.88 |
| Gender | ||
| Female | 604 | 59.80 |
| Male | 406 | 40.20 |
| Education status | ||
| No formal education | 444 | 43.96 |
| Primary education | 332 | 32.87 |
| Secondary education and above | 234 | 23.17 |
| Marital status | ||
| Do not have a spouse | 262 | 25.94 |
| Have a spouse | 748 | 74.06 |
| Live with at least one child | ||
| No | 556 | 55.05 |
| Yes | 454 | 44.95 |
| Annual household income (log), Mean (SD) | 1010 | 8.95 (1.14) |
| Visual acuity ≤ 0.3 in either eye | ||
| No | 663 | 65.64 |
| Yes | 347 | 34.36 |
| Characteristics of VDs (n = 35) | ||
| Age (years) of the VD | ||
| <45 | 13 | 37.14 |
| ≥45 | 22 | 62.86 |
| Gender of the VD | ||
| Female | 8 | 22.86 |
| Male | 27 | 77.14 |
| Education status of the VD | ||
| High school | 29 | 82.86 |
| College | 6 | 17.14 |
| Whether the VD lives in the village | ||
| No | 12 | 34.29 |
| Yes | 23 | 65.71 |
| Work experience (years) of the VD | ||
| <10 | 13 | 37.14 |
| ≥10 | 22 | 62.86 |
| More than half of work time spent on public health services last year | ||
| No | 8 | 22.86 |
| Yes | 27 | 77.14 |
| Service population | ||
| <2000 | 23 | 65.71 |
| ≥2000 | 12 | 34.29 |
| Service radius (KM) | ||
| <10 | 28 | 80.00 |
| ≥10 | 7 | 20.00 |
| Questions | Scoring Scheme | Correctly Answered by the Residents | Correctly Answered by the VD |
|---|---|---|---|
| N (%) | N (%) | ||
| 1. Should the elderly do regular cataract screening? | Yes = 1 mark | 807 (79.90) | 32 (91.43) |
| 2. Can cataracts be cured by surgery? | Yes = 1 mark | 757 (74.95) | 33 (94.29) |
| 3. Whether cataract surgery is safe? | Yes = 1 mark | 726 (71.88) | 34 (97.14) |
| 4. Whether cataract is a common disease for elders? | Yes = 1 mark | 702 (69.50) | 32 (91.43) |
| 5. Will cataract surgery improve eyesight? | Yes = 1 mark | 721 (71.39) | 34 (97.14) |
| 6. Can cataracts be cured with medications? | No = 1 mark | 485 (48.02) | 32 (91.43) |
| 7. Whether cataract surgery is covered by the New Cooperative Medical System? | Yes = 1 mark | 536 (54.06) | 35 (100.00) |
| 8. Should a patient delay cataract surgery before being blind? | No = 1 mark | 392 (38.81) | 31 (88.57) |
| Mean (SD) | - | 5.08 (1.91) | 6.94 (1.14) |
| Variables | Vision Screening (1) | Cataract Screening (2) | ||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Characteristics of residents (n = 1010) | ||||
| Age | ||||
| 50–59 (ref) | ||||
| 60–69 | 1.52 (1.00–2.33) | 0.051 | 1.84 (1.26–2.69) | 0.002 |
| ≥70 | 1.61 (0.97–2.69) | 0.063 | 2.19 (1.24–3.87) | 0.007 |
| Gender | ||||
| Female (ref) | ||||
| Male | 0.74 (0.53–1.04) | 0.079 | 0.83 (0.59–1.16) | 0.271 |
| Education status | ||||
| No formal education (ref) | ||||
| Primary education | 1.46 (0.91–2.33) | 0.116 | 0.81 (0.43–1.53) | 0.510 |
| Secondary education and above | 2.08 (1.35–3.19) | 0.001 | 1.56 (0.85–2.86) | 0.150 |
| Marital status | ||||
| Do not have a spouse (ref) | ||||
| Have a spouse | 0.97 (0.63–1.49) | 0.892 | 0.80 (0.53–1.18) | 0.248 |
| Live with a least one child | ||||
| No (ref) | ||||
| Yes | 0.82 (0.60–1.11) | 0.190 | 0.87 (0.58–1.30) | 0.491 |
| Annual household income (log) | 0.95 (0.84–1.07) | 0.379 | 0.92 (0.82–1.04) | 0.177 |
| Visual acuity ≤ 0.3 in either eye | ||||
| No (ref) | ||||
| Yes | 1.39 (1.02–1.90) | 0.036 | 2.08 (1.42–3.05) | 0.000 |
| Characteristics of VDs (n = 35) | ||||
| Age (years) of the VD | ||||
| <45 (ref) | ||||
| ≥45 | 1.45 (0.98–2.15) | 0.064 | 1.75 (1.24–2.47) | 0.001 |
| Gender of the VD | ||||
| Female (ref) | ||||
| Male | 1.20 (0.87–1.66) | 0.265 | 3.09 (2.15–4.43) | 0.000 |
| Education status of the VD | ||||
| High school (ref) | ||||
| College | 1.13 (0.56–2.31) | 0.728 | 1.20 (0.71–2.04) | 0.495 |
| Whether the VD lives in the village | ||||
| No (ref) | ||||
| Yes | 1.59 (0.94–2.70) | 0.086 | 1.17 (0.77–1.76) | 0.461 |
| Work experience (years) of the VD | ||||
| <10 (ref) | ||||
| ≥10 | 0.72 (0.41–1.27) | 0.259 | 0.65 (0.41–1.02) | 0.059 |
| More than half of work time spent on public health services last year | ||||
| No (ref) | ||||
| Yes | 1.94 (1.18–3.21) | 0.009 | 1.64 (1.10–2.44) | 0.015 |
| Service population | ||||
| <2000 (ref) | ||||
| ≥2000 | 0.61 (0.44–0.85) | 0.003 | 0.62 (0.44–0.87) | 0.006 |
| Service radius (KM) | ||||
| <10 (ref) | ||||
| ≥10 | 1.35 (0.86–2.12) | 0.196 | 0.76 (0.54–1.06) | 0.101 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Du, K.; Guan, H.; Ding, Y.; Zhang, Y.; Wang, D.; Wang, H. The Role of Village Doctors in Residents’ Uptake of Eye Screening: Evidence from Ageing Residents in Rural China. Healthcare 2022, 10, 1197. https://doi.org/10.3390/healthcare10071197
Huang J, Du K, Guan H, Ding Y, Zhang Y, Wang D, Wang H. The Role of Village Doctors in Residents’ Uptake of Eye Screening: Evidence from Ageing Residents in Rural China. Healthcare. 2022; 10(7):1197. https://doi.org/10.3390/healthcare10071197
Chicago/Turabian StyleHuang, Juerong, Kang Du, Hongyu Guan, Yuxiu Ding, Yunyun Zhang, Decai Wang, and Huan Wang. 2022. "The Role of Village Doctors in Residents’ Uptake of Eye Screening: Evidence from Ageing Residents in Rural China" Healthcare 10, no. 7: 1197. https://doi.org/10.3390/healthcare10071197
APA StyleHuang, J., Du, K., Guan, H., Ding, Y., Zhang, Y., Wang, D., & Wang, H. (2022). The Role of Village Doctors in Residents’ Uptake of Eye Screening: Evidence from Ageing Residents in Rural China. Healthcare, 10(7), 1197. https://doi.org/10.3390/healthcare10071197






