Abstract
Much work has focused on the development of instruments that measure the quality of care, but few studies have been published for staff assessment of the quality of care provided by inpatient psychiatric care. Therefore, an instrument is needed to measure the quality of care from the perspective of facility staff. The aim of the present study was to evaluate the psychometric properties and factor structure of the Quality in Psychiatric Care-Inpatient Staff (QPC-IPS) instrument. A sample of 104 staff at seven wards in four regions in Sweden completed the QPC-IPS, which consists of 30 items covering six dimensions of quality. Confirmatory factor analysis confirmed the proposed six factor structure of the QPC-IPS. Internal consistency for the full QPC-IPS was adequate, but poor for some of the dimensions. Staff ratings of the quality of care were generally high. The highest rating was for the Support dimension and the lowest for the Secure environment dimension.
1. Introduction
Quality of care is a topic relevant in health management, research, and clinical practice. In psychiatric care, the interest in issues of quality-of-care measurements has been growing [1]. The use of well-constructed measurement instruments with high levels of reliability and validity is an effective way to measure the quality of care [2], and their use is fundamental for improving the quality of psychiatric care and finding out where changes are needed [3].
Patients’ experiences of quality of care have for many years been deemed to be an important measure of quality of care [3]. The assessment of the staff’s judgement of the quality of care can also provide useful data for improving and developing the care and its efficacy. This data is important as it reflects the views of the staff providing the care, which is a significant indicator when measuring its quality [4].
Extensive work has been focused on developing quality of care measuring instruments in the health care services [5]. In spite of this, less has been published on how staff experience the quality of psychiatric inpatient care. In a systematic review of the psychometric properties of instruments measuring quality of care in psychiatric care, Sanchez-Balcells et al. [6] found only five measurements for staff/management, and of these, only three were for inpatient care, namely for management [7], for nursing staff and patients [8] and for forensic inpatient care staff [9]. Only one of these instruments measured how staff experience the quality of inpatient care, but this instrument was for forensic inpatient care staff. In order to systematically assess the quality of care from the perspective of the staff, valid standardised measurements are needed that can aid comparative benchmarking both nationally and internationally. Such measurements can also identify incongruence between the views of patients and staff on the quality of care [10], as evidence shows that understandings and perspectives on efforts can vary between the two groups [11]. Hence, both perspectives are needed to obtain a more complete assessment [6].
Instruments measuring quality of care should have a clear conceptualisation of what quality of care is [12]. As quality of care is context specific [13], measuring instruments should also be designed for the services where they are to be used [14]. The Quality in Psychiatric Care-Inpatient (QPC-IP) instrument was developed from a definition of quality of care, psychometrically tested, context specific and is frequently used for measuring quality of care from the patients’ perspective [15]. Recently, the Quality in Psychiatric Care-Inpatient Staff (QPC-IPS) instrument was developed for measuring staff perceptions of the quality of care with the same items as the QPC-IP, providing the possibility of comparing the two perspectives on the ratings for quality of care. Still, little is known about how staff and patients sharing the same ward perceive the quality of care. One reason can be the lack of a single instrument that covers the same dimensions of quality of care for both the patients and staff [16]. When a new instrument is developed, it is necessary to develop, refine and establish its psychometric properties [17]. Therefore, the aim of the present study is to evaluate the psychometric properties and factor structure of the Quality in Psychiatric Care-Inpatient Staff (QPC-IPS) instrument.
2. Materials and Methods
2.1. Design
The study has a cross-sectional design.
2.2. Participants and Procedures
A sample of 104 staff at seven wards in four regions in Sweden completed the QPC-IPS. Data collection took place during six months in 2019. Inclusion criteria for participants encompassed: (1) permanent employees or locum tenens in psychiatric inpatient care and (2) having worked for at least three months in psychiatric inpatient care. The invitation to participate was handled by a contact person (mostly the head of the ward) who orally and in writing informed the staff about the aim of the study. All participants were informed that their participation was voluntary, that their answers would be anonymised and that they could withdraw at any time. Those who agreed to participate gave their oral consent and were requested to complete the QPC-IPS instrument anonymously.
2.3. The QPC-IPS Instrument
The QPC, short for Quality in Psychiatric Care, is a self-reported and multidimensional instrument developed for patients’ perceptions of quality of care [16] and adapted to six patient versions for diverse mental health contexts. Each patient version has a common core with context-specific items [18] and a staff version with the same dimensions and items. Currently, the instrument for the inpatient care staff (QPC-IPS) in Indonesian and Spanish [19,20] and forensic inpatient care staff in Swedish and Danish (QPC-FIPS) [9,21] have been psychometrically evaluated.
In this study, staff perceptions were measured with the Swedish QPC-IPS, short for Quality in Psychiatric Care-Inpatient staff. The QPC-IPS starts with a number of background questions concerning demography and general relevant information, followed by 30 items divided into six quality dimensions: Encounter (8 items), Participation (8 items), Discharge (4 items), Support (4 items), Secluded environment (3 items), and Secure environment (3 items). Each item describes perceptions of the provided quality of care and consists of a statement on quality of care (e.g., "I experience that the patients are involved in decisions about their care") rated on a 4-point Likert type scale, ranging from 1 = totally disagree to 4 = totally agree with an additional non-applicable response alternative. An open question at the end invites further comments on the quality of care.
2.4. Data Analysis
To compute descriptive statistics, we used the statistical software package SPSS version 22 (IBM Corp., Armonk, NY, USA). To assess the scales, we used Cronbach’s alpha [22] with Nunnally and Bernstein’s [23] 0.70 criterion for adequate homogeneity. Confirmatory factor analysis (CFA) was performed using LISREL 8.8, Scientific Software International: Chicago, IL, USA [24] with generally weighted least-squares estimation on the asymptotic covariance matrices. The PRELIS program [25] obtained polychoric and polyserial correlation matrices and the weighted least squares method using the asymptotic covariance matrix estimated the parameters. The Satorra–Bentler scaled chi-square (S-Bχ2) test [26] was used because the data were ordinal (i.e., 4-point Likert scale).
Confirmatory factor analysis was used to test whether the factor structure, i.e., the construct validity of the QPC-IPS is consistent with that of the OPQ-IP, serving as an a priori model. Thus, items 7, 10, 11, 12, 15, 18, 20 and 25 were assumed to represent Encounter; items 1, 5, 6, 13, 14, 27, 29 and 30 represent Participation; items 8, 16, 17 and 21 represent Discharge; items 19, 22, 23 and 24 represent Support; items 3, 26, and 28 represent Secluded environment; and items 2, 4 and 9 represent Secure environment.
In addition to the Satorra–Bentler scaled chi-square (S-Bχ2), we used the root mean square error of approximation (RMSEA), the standardised root mean square residual (SRMR), and the comparative fit index (CFI) to evaluate the adequacy of the a priori model [27]. Values lower than 0.08 and 0.05 for the RMSEA, equal to or lower than 0.10 and 0.08 for the SRMR, and equal to or greater than 0.90 and 0.95 for the CFI were considered to constitute an adequate and excellent level of goodness of fit, respectively [28].
3. Results
3.1. Sample Description
The sample consisted of 104 staff (81 women and 23 men) aged between 22 and 67 years (mean = 46.8, SD = 14.2), of which 71 (68%) were nursing assistants, 28 (27%) were licensed nurses, and the remaining 5 (5%) were psychiatrists, counsellors or care assistants. Of the staff, 100 (96%) were Swedish and the remaining 4 (4%) were from other European countries. The staff had worked at the ward for on average 7.7 years (range 0–43 years) and most of them—68 (65%)—worked daytime, 20 (19%) worked a combination of day- and night-time, and 14 (14%) worked night-time only.
3.2. Factor Structure of the QPC-IPS
The CFA performed on the model representing the QPC-IP factor structure showed a significant chi square (S-Bχ2 = 517.67, df = 390, p < 0.001), CFI = 0.98, RMSEA = 0.056 (CI = 0.043–0.069) with a Close Fit (RMSEA < 0.05) p = 0.21, and SRMR = 0.092. This result indicated an adequate to excellent fit. Hence, the model was regarded an acceptable representation of the proposed factor structure of the QPC-IPS. All loadings were significant (p < 0.05).
3.3. Internal Consistency
The internal consistency of the QPC-IPS was adequate with a Cronbach α of 0.94 for the full questionnaire as well as for the individual factors Encounter (α = 0.90), Participation (α = 0.87), Discharge (α = 0.82), Secure environment (α = 0.76), and Support (α =0.75). Less than adequate consistency was, however, found for Secluded environment (α = 0.65).
3.4. Test Retest
Forty staff completed the QPC-IPS twice and test-retest analyses demonstrated excellent retest reliability for the full QPC-IPS, and adequate to excellent retest reliability for the specific dimensions, with Participation receiving the highest and Secluded environment the lowest retest reliability (Table 1).

Table 1.
Test-retest statistics for the QPC-IPS among staff in inpatient psychiatric care at Time 1 (T1) and Time 2 (T2) × months later.
3.5. Description of Staff View of Inpatient Quality of Care
The mean and standard deviations for the QPC-IPS items are given in Table 2.

Table 2.
Summary statistics for the QPC-IPS.
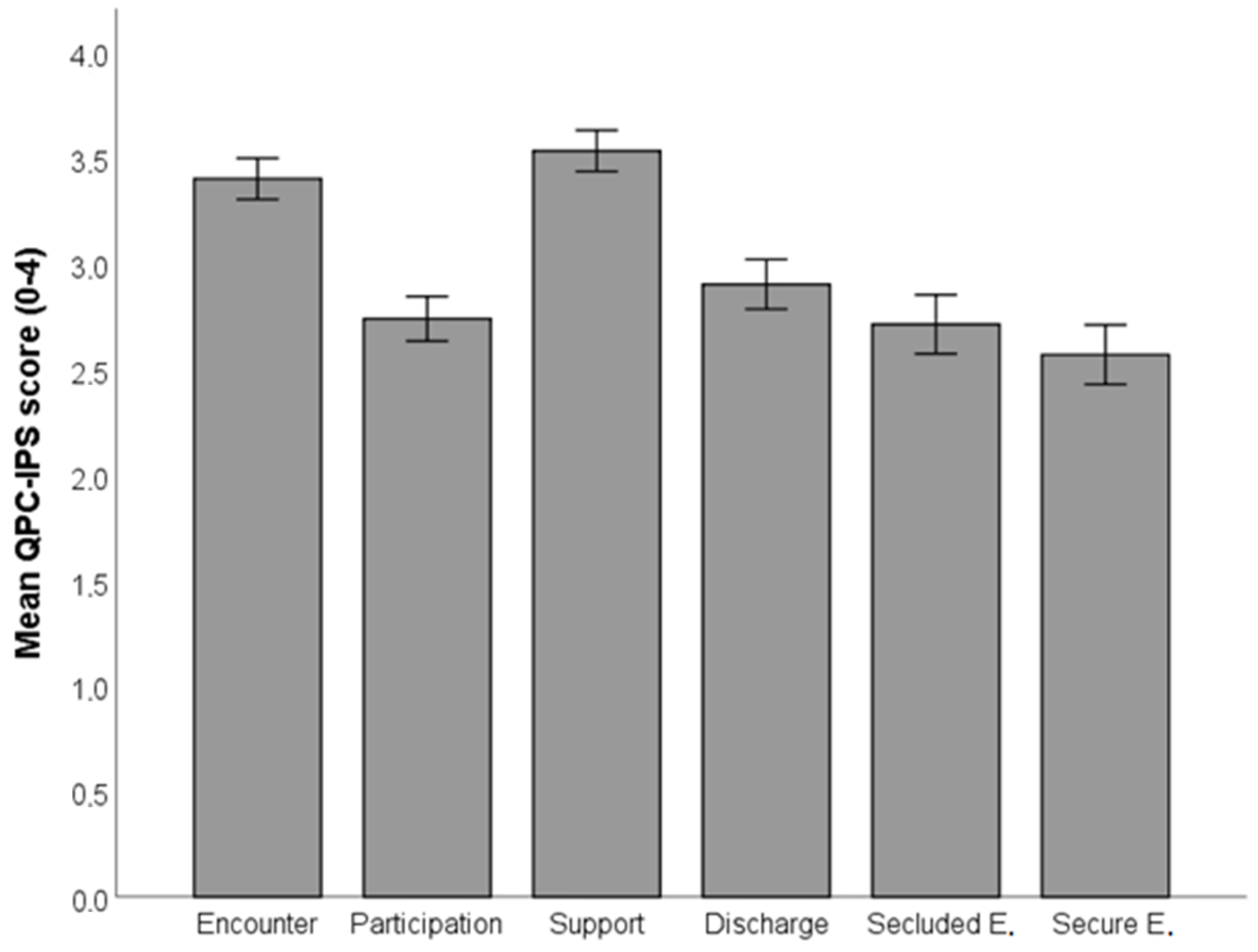
As shown in Figure 1, and supported by dependent t-tests, the perceived quality of Support was significantly greater than the perceived quality of the second-ranked dimension, Encounter (t(103) = 3.46, p < 0.001), which in turn was perceived as significantly greater than Discharge (t(103) = 9.90, p < 0.001). Discharge was perceived as greater than Participation (t(103) = 3.49, p < 0.001), which, however, was not perceived as significantly greater than Secluded environment, which in turn was significantly larger than Secure environment (t(103) = 2.14, p = 0.035).
Figure 1.
Mean QPC-IPS scores for each QPC-IPS dimension.
As shown in Table 3, all correlations among the QPC-IPS dimensions were significantly correlated with coefficients demonstrating moderate to strong relationships.

Table 3.
Correlation coefficients for the QPC-IPS dimensions among staff in inpatient psychiatric care.
4. Discussion
Measuring quality of care is a step towards improving psychiatric inpatient care but it has been held back by a lack of psychometrically tested instruments for measuring staff perception of the quality of care provided. Therefore, the aim of the present study was to evaluate the psychometric properties and factor structure of the QPC-IPS. The findings demonstrate that the QPC-IPS is a valid and reliable instrument for measuring staff perceptions of the quality of care in psychiatric inpatient care. The CFA showed that the factor structure of the QPC-IPS was equivalent with that of the patients’ version (QPC-IP) [15], demonstrating its construct validity. Thus, both patients and staff in inpatient psychiatric care have a similar view of the quality of care concept expressed in the QPC instruments.
Even though the aim of the study was to evaluate the psychometric properties and factor structure of the QPC-IPS, it is worth noting that the staff in this study perceived the quality of care in general as high: 88.4% had a mean score greater than 2.5, which is the centre of the rating scale used in QPC-IPS. This is in line with other studies using the QPC instruments in various psychiatric cultures and contexts, for example, Denmark [21], Indonesia [19] and Spain [20]. The highest rating in the present study was in the dimension of Support, which is in line with previous studies on staff in inpatient care [19,20]. The findings from the current study may indicate that staff were aware of the patients’ shame and guilt and sought to prevent these feelings in their treatment. This finding also indicates that the staff prevents situations where the patient becomes a threat to themselves and others. This is strange and may be contradictory, as the lowest rating was in the Secure environment dimension. This finding highlights that staff did not experience the care environment as safe and that the patients did not feel secure among their fellow patients. This is in line with previous studies on perceptions of quality among staff in forensic inpatient care in both Sweden [9] and Denmark [21] as well as in other studies regarding safety in psychiatric inpatient wards [29,30]. It seems that staff in inpatient care, regardless of context, perceived the ward environment as unsafe. Maybe this can be explained by the occurrence of violence, mainly verbal and sometimes also physical, in psychiatric care [31]. Regardless, staff should create a secure foundation for patients in inpatient care [32] and the safety of both patients and staff is an important aspect of the quality of care [31]. In addition, nurses are expected to apply research evidence in practice to improve both the quality of care and safety on the ward [33], as they are key personnel in the delivery of health care [34]. Thibaut et al. [35] conclude in a systematic review that patient safety in inpatient psychiatric care is under-researched, therefore more research is needed in this area.
4.1. Limitations
Some limitations of the study must be mentioned. Only 104 staff agreed to participate in this study. The general rule of thumb [36] suggests a minimum of 150 respondents when the instrument consists of 30 items. On the other hand, finding participants for questionnaire-based studies is a general problem [37]. In this study, it was not possible to analyse the dropouts because of the incomplete registration of “missing staff” at the wards.
4.2. Implications for Practice
The QPC-IPS is an adequate instrument for measuring quality of care from the staff’s perspective and can be used as a tool in daily work. This is important information as staff, especially nurses, are crucial in the process of implementing measurements.
Generally, the scores for the different dimensions indicated where improvements may be required, and the QPC-IPS can be used as a local, regional and national self-rating instrument. The awareness of the staff’s low ratings for the quality of care regarding the dimension Secure environment can be used to manage and support quality of care improvement.
5. Conclusions
The 30-item QPC-IPS is a psychometrically adequate instrument and is an easy, time-efficient, inexpensive and quick way to evaluate quality of care. QPC-IPS can be used as a tool to motivate care staff to continually and systematically improve the care provided. The low rating in the dimension Secure environment is a challenge for nursing staff as well as other staff and management to improve. In addition, the instrument can with advantage be used with the patient version (QPC-IP) [15] to achieve an overall picture of the quality of care. As Shannon, Mitchell, and Cain [38] state, both perspectives are needed. Therefore, further research should compare both the patients’ and the staff’s ratings of quality of care. So far, QPC-IPS is available, apart from Swedish, in two languages—Indonesian [19] and Spanish [20]—which allows for international comparisons of quality of care.
Author Contributions
All authors have contributed significantly and are in agreement on the content of the manuscript. Conceptualization, A.S. and L.-O.L.; methodology, A.S. and L.-O.L.; software, L.-O.L.; validation, A.S. and L.-O.L.; formal analysis, L.-O.L.; investigation, A.S. and L.-O.L.; resources, A.S. and L.-O.L.; data curation, A.S. and L.-O.L.; writing—original draft preparation, A.S. and L.-O.L.; writing—review and editing, A.S. and L.-O.L.; visualization, A.S. and L.-O.L.; supervision, A.S. and L.-O.L.; project administration, A.S.; funding acquisition, A.S. and L.-O.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by grants from The Fund for Rehabilitation and Medical Research (Fonden för Rehabilitering och Medicin) (reference number 18RS2843), and the Region Örebro County Research Committee (Forskningskommittén i Region Örebro län), Sweden (reference number OLL-811421). This research received no specific grants from any funding agency in the public, commercial or not-for-profit sectors.
Institutional Review Board Statement
This study was designed in accordance with ethical principles for medical research involving human subjects by the guidelines of the Declaration of Helsinki [39]. The study was approved by the Regional Research Ethics Committee in Uppsala, Sweden (reference number 2018/186).
Informed Consent Statements
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Data available on request from authors. The data that support the findings of this study are available from the corresponding author upon reasonable request and in accordance with ethical approval.
Acknowledgments
We would like to thank Daniel Pichler, Nicholas Ståhl and Ulf Johansson at the University Health Care Research Center, Örebro, Sweden for administrative assistance.
Conflicts of Interest
The authors declare no conflict of interest with respect to the research, authorship and/or publication of this article.
References
- Parameswaran, S.G.; Spaeth–Rublee, B.; Pincus, H.A. Measuring the quality of mental health care: Consensus perspectives from selected industrialized countries. Adm. Policy Ment. Health 2015, 42, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Konderding, U. Which kind of psychometrics is adequate for patient satisfaction questionnaires? Patient Prefer. Adherence 2016, 10, 2083–2090. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.E.; Tsugawa, Y.; Figueroa, J.F.; Jha, A.K. Association between the Centers for Medicare and Medicaid Services hospital star rating and patient outcomes. JAMA Intern. Med. 2016, 176, 848–850. [Google Scholar] [CrossRef] [PubMed]
- Arnetz, B.B. Staff perception of the impact of health care transformation on quality of care. Int. J. Qual. Health Care 1999, 11, 345–351. [Google Scholar] [CrossRef]
- Farr, M.; Cressey, P. Understanding staff perspectives of quality of care in practice in healthcare. BMC Health Serv. Res. 2015, 15, 123. [Google Scholar] [CrossRef]
- Sanchez-Balcells, S.; Callarisa Roca, M.; Rodriguez-Zunino, N.; Puig-Llobert, M.; Lluch-Canut, M.-T.; Roldan-Merino, J.F. Psychometric properties of instruments measuring quality and satisfaction in mental health: A systematic review. J. Adv. Nurs. 2018, 74, 2497–2510. [Google Scholar] [CrossRef]
- Delaney, K.R.; Johnson, M.E.; Fogg, L. Development and testing of the combined assessment of psychiatric environments. A patient-centered quality measure for inpatient psychiatric treatment. J. Am. Psychiatr. Nurses Assoc. 2015, 21, 134–147. [Google Scholar] [CrossRef]
- Danielson, C.K.; Borckardt, J.J.; Grubaugh, A.L.; Pelic, C.G.; Hardesty, S.J.; Frueh, B.C. Quantifying staff and patient perceptions of quality of care improvements in the psychiatric inpatient setting: Preliminary psychometrics of a new measure. Psychol. Serv. 2008, 5, 1–10. [Google Scholar] [CrossRef]
- Schröder, A.; Lundqvist, L.-O. The Quality in Psychiatric Care–Forensic In-Patient Staff (QPC-FIPS) instrument: Psychometric properties and staff views of the quality of forensic psychiatric services in Sweden. Open J. Nurs. 2013, 3, 330–341. [Google Scholar] [CrossRef][Green Version]
- Luther, L.; Fukui, S.; Garabrant, J.M.; Rollins, A.L.; Morse, G.; Henry, N.; Shimp, D.; Gearhart, T.; Salyers, M. Measuring quality of care in community mental health: Validation of concordant clinician and client quality-of-care scales. J. Behav. Health Serv. Res. 2019, 46, 64–79. [Google Scholar] [CrossRef]
- Granger, B.B.; Sandelowski, M.; Tahshjain, H.; Swedberg, K.; Ekman, I. A qualitative descriptive study of the work of adherence to chronic heart failure regimen: Patient and physician perspectives. J. Cardiovasc. Nurs. 2009, 24, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Sitzia, J.; Wood, N. Patient satisfaction: A review of issues and concepts. Soc. Sci. Med. 1997, 45, 1829–1843. [Google Scholar] [CrossRef]
- Boyer, L.; Baumstarck-Barrau, K.; Cano, N.; Zendjidjian, X.; Belzeaux, R.; Limousin, S.; Magalon, D.; Samuelian, J.C.; Lancon, C.; Auquier, P. Assessment of psychiatric inpatient satisfaction: A systematic review of self-reported instruments. Eur. Psychiatry 2009, 24, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Shiva, A.; Haden, S.C.; Brooks, J. Psychiatric civil and forensic inpatient satisfaction with care: The impact of provider and recipient characteristics. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 979–987. [Google Scholar] [CrossRef]
- Schröder, A.; Wilde-Larsson, B.; Ahlström, G.; Lundqvist, L.-O. Psychometric properties of the instrument Quality in Psychiatric Care and descriptions of quality of care among in-patients. Int. Health Care Qual. Assur. 2010, 23, 554–570. [Google Scholar] [CrossRef]
- Lundqvist, L.-O.; Schröder, A. Patient and staff views of quality in forensic psychiatric in-patient care. J. Forensic Nurs. 2015, 11, 51–58. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A practical guide to their development and use, 2nd ed.; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Lundqvist, L.-O.; Suryani; Anna, N.; Rafiyah, I.; Schröder, A. Indonesian adaptation of the Quality in Psychiatric Care–In-patient (QPC-IP) instrument: Psychometric properties and factor structure. Asian J. Psychiatr. 2018, 34, 1–5. [Google Scholar] [CrossRef]
- Lundqvist, L.-O.; Suryani; Hermiati, D.; Sutini, T.; Schröder, A. A psychometric evaluation of the Indonesian version of the Quality in Psychiatric Care–Inpatient Staff (QPC-IPS) instrument. Asian J. Psychiatr. 2019, 46, 29–33. [Google Scholar] [CrossRef]
- Sanchez-Balcells, S.; Lundqvist, L.-O.; Roldan-Merino, J.F.; Lluch-Canut, M.-T.; Calarisa Roca, M.; Rodriguez Zunino, N.; Tomas Jimenez, M.; Schröder, A.; Puig-Llobet, M. A Spanish adaptation of the Quality in Psychiatric Care–Inpatient Staff (QPC-IPS) instrument: Psychometric properties and factor structure. An. Sist. Sanit. Navar. 2020, 43, 307–321. [Google Scholar]
- Lundqvist, L.-O.; Riiskjaer, E.; Lorentzen, K.; Schröder, A. Factor structure and psychometric properties of the Danish adaptation of the Quality in Psychiatric Care–Forensic In-patient Staff (QPC-FIPS). Open J. Nurs. 2014, 4, 878–885. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw–Hill: New York, NY, USA, 1994. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: User’s Reference Guide, 2nd ed.; Scientific Software International: Chicago, IL, USA, 1996. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. PRELIS—A Program for Multivariate Data Screening and Data Summarization. A Preprocessor for LISREL, 2nd ed.; Scientific Software Inc.: Chicago, IL, USA, 1988. [Google Scholar]
- Satorra, A.; Bentler, P.M. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika 2001, 66, 507–514. [Google Scholar] [CrossRef]
- Cangur, S.; Ercan, I. Comparison of model fit indices used in structural equation modeling under multivariate normality. J. Mod. App. Stat. Methods 2015, 14, 52–167. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Jones, J.; Nolan, P.; Bowers, L.; Simpson, A.; Hackney, D.; Bhui, K. Psychiatric wards: Places of safety? J. Psychiatr. Ment. Health Nurs. 2010, 17, 124–130. [Google Scholar] [CrossRef]
- Stenhouse, R.C. “Safe enough in here?”: Patients’ expecations and experinces of feeling safe in an acute psychiatric inpatient ward. J. Clin. Nurs. 2013, 22, 3109–3119. [Google Scholar] [CrossRef] [PubMed]
- Samartzis, L.; Talias, M.A. Assessing and improving the quality in mental health services. Int. J. Environ. Res. Public Health 2020, 17, 249. [Google Scholar] [CrossRef]
- Pelto-Piri, V.; Wallsten, T.; Hylén, U.; Nikban, I.; Kjellin, L. Feeling safe or unsafe in the psychiatric inpatient care, a hospital-based qualitative interview study with inpatients in Sweden. Int. J. Ment. Health Syst. 2019, 13, 23. [Google Scholar] [CrossRef]
- Melnyk, B.; Gallagher-Ford, L.; Long, L.E.; Fineout-Overholt, E. The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews Evid.-Based Nurs. 2014, 11, 5–15. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidus, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef]
- Tibaut, B.; Dewa, L.H.; Ramtale, S.C.; D’Lima, D.; Adam, S.; Ashrafian, H.; Darzi, A.; Archer, S. Patient safety in inpatient mental health settings: A systematic review. BMJ Open 2019, 9, e030230. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F.; Anderson, R.E.; Tatham, R.L.; Black, W.C. Multivariate Data Analysis with Readings; Prentice Hall: Hoboken, NJ, USA, 1995. [Google Scholar]
- Rindfuss, R.R.; Choe, M.K.; Tsuya, N.O.; Bumpass, L.L.; Tamaki, E. Do low survey response rates bias results? Evidence from Japan. Demogr. Res. 2015, 32, 797–828. [Google Scholar] [CrossRef]
- Shannon, S.E.; Mitchell, P.H.; Cain, K.C. Patients, nurses, and physicians have differing views of quality of critical care. J. Nurs. Scholarsh. 2002, 34, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, B.; Dunn, L. The declaration of Helsinki on medical research involving human subjects: A review of seventh revision. J. Nepal Health Res. Counc. 2019, 17, 548–552. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).