Effectiveness of Digital Flipped Learning Evidence-Based Practice on Nurses’ Knowledge, Attitude, and Practice: A Quasi-Experimental Trial
Abstract
:1. Introduction
2. Literatures Review
3. Methods
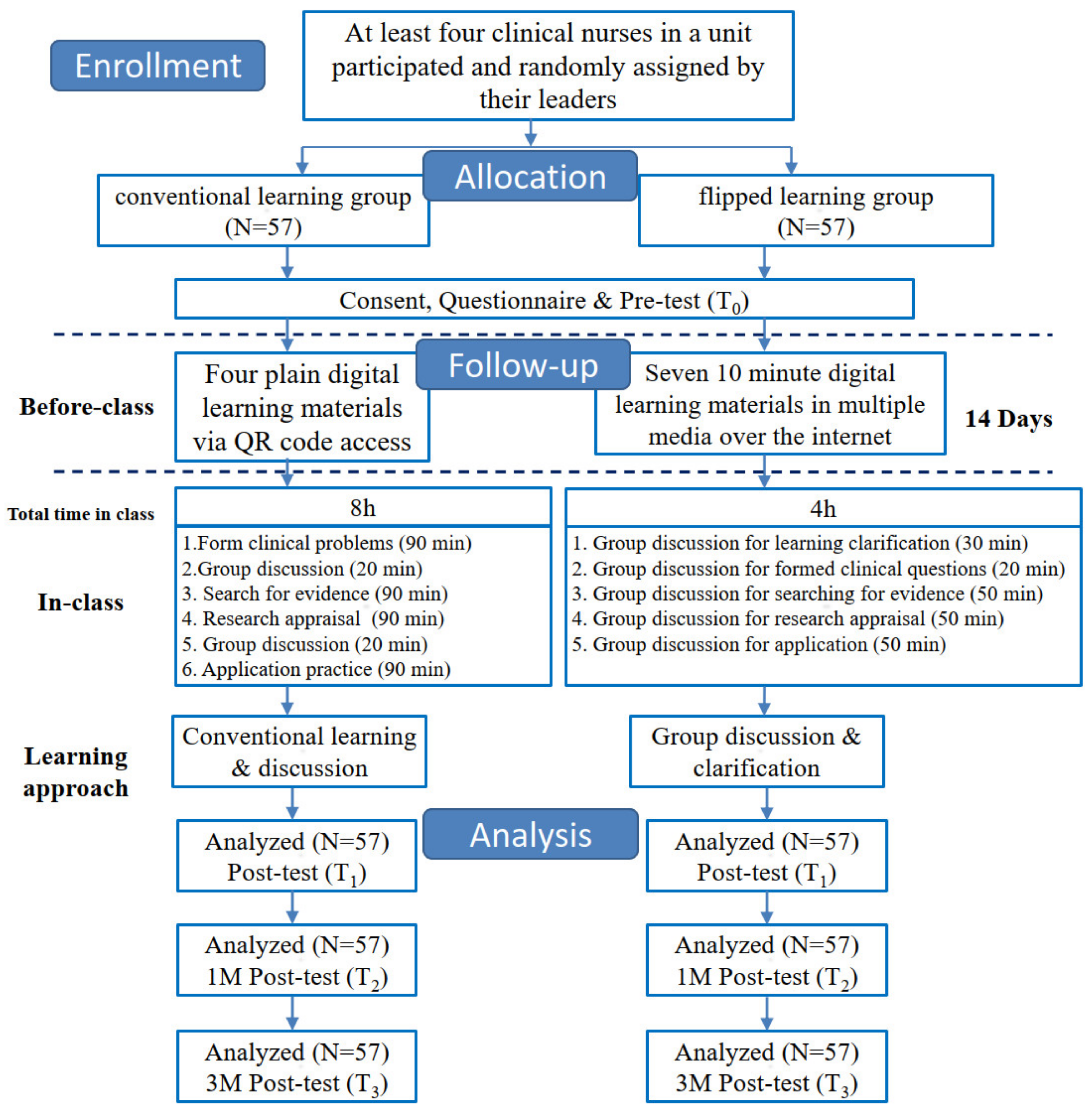
3.1. Study Design
3.2. Participants
3.3. Intervention
3.3.1. Interventions: Flipped Learning
3.3.2. Interventions: Conventional Learning
3.4. Outcome Measures
3.5. Instruments
3.6. Data Collection
3.7. Data Analysis
4. Results
4.1. Comparison of Homogeneity in Demographic Variables between the Two Groups
4.2. Comparison of the Knowledge, Attitude, and Practice in the Two Groups
4.3. Effusiveness of Intervention on Participants’ Knowledge, Attitude, and Practice of EBP
4.4. Satisfaction of the Intervention in the Two Groups
5. Discussion
5.1. Knowledge of EBP
5.2. Attitude to EBP
5.3. Practice of EBP
5.4. Satisfaction
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Fineout-Overholt, E.; Melnyk, B.M.; Schultz, A. Transforming health care from the inside out: Advancing evidence-based practice in the 21st century. J. Prof. Nurs. 2005, 21, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Fineout-Overholt, E.; Stetler, C.; Allan, J. Outcomes and implementation strategies from the first US evidence-based practice leadership summit. Worldviews Evid.-Based Nurs. 2005, 2, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Jalali-Nia, S.F.; Salsali, M.; Dehghan-Nayeri, N.; Ebadi, A. Effect of evidence-based education on Iranian nursing students’ knowledge and attitude. Nurs. Health Sci. 2011, 13, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Brown, C.E.; Ecoff, L.; Davidson, J.E.; Gallo, A.; Klimpel, K.; Wickline, M.A. Regional evidence-based practice fellowship program: Impact on evidence-based practice implementation and barriers. Clin. Nurs. Res. 2013, 22, 51–69. [Google Scholar] [CrossRef] [PubMed]
- Levin, R.F.; Fineout-Overholt, E.; Melnyk, B.M.; Barnes, M.; Vetter, M.J. Fostering evidence-based practice to improve nurse and cost outcomes in a community health setting: A pilot test of the advancing research and clinical practice through close collaboration model. Nurs. Adm. Q. 2011, 35, 21–33. [Google Scholar] [CrossRef]
- Varnell, G.; Haas, B.; Duke, G.; Hudson, K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid.-Based Nurs. 2008, 5, 172–181. [Google Scholar] [CrossRef]
- Courey, T.; Benson-Soros, J.; Deemer, K.; Zeller, R.A. The missing link: Information literacy and evidence-based practice as a new challenge for nurse educators. Nurs. Educ. Perspect. 2006, 27, 320–323. [Google Scholar]
- Penz, K.; D’Arcy, C.; Stewart, N.; Kosteniuk, J.; Morgan, D.; Smith, B. Barriers to participation in continuing education activities among rural and remote nurses. J. Contin. Educ. Nurs. 2007, 38, 58–66. [Google Scholar] [CrossRef]
- Weng, Y.H.; Chen, C.; Kuo, K.N.; Yang, C.Y.; Lo, H.L.; Chen, K.H.; Chiu, Y.W. Implementation of Evidence-Based Practice in Relation to a Clinical Nursing Ladder System: A National Survey in Taiwan. Worldviews Evid.-Based Nurs. 2015, 12, 22–30. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; Perillo, S.; Brown, T. What are the factors of organisational culture in health care settings that act as barriers to the implementation of evidence-based practice? A scoping review. Nurse Educ. Today 2015, 35, e34–e41. [Google Scholar] [CrossRef]
- Chan, E.Y.; Glass, G.F.; Phang, K.N. Evaluation of a Hospital-Based Nursing Research and Evidence-Based Practice Mentorship Program on Improving Nurses’ Knowledge, Attitudes, and Evidence-Based Practice. J. Contin. Educ. Nurs. 2020, 51, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Bazargani, H.; Tabrizi, J.S.; Azami-Aghdash, S. Barriers to evidence-based medicine: A systematic review. J. Eval. Clin. Pract. 2014, 20, 793–802. [Google Scholar] [CrossRef] [PubMed]
- McCutcheon, K.; Lohan, M.; Traynor, M.; Martin, D. A systematic review evaluating the impact of online or blended learning vs. face-to-face learning of clinical skills in undergraduate nurse education. J. Adv. Nurs. 2015, 71, 255–270. [Google Scholar] [CrossRef]
- Hart, P.; Eaton, L.; Buckner, M.; Morrow, B.N.; Barrett, D.T.; Fraser, D.D.; Hooks, D.; Sharrer, R.L. Effectiveness of a Computer-Based Educational Program on Nurses’ Knowledge, Attitude, and Skill Level Related to Evidence-Based Practice. Worldviews Evid.-Based Nurs. 2008, 5, 75–84. [Google Scholar] [CrossRef]
- Pérez-Campos, M.A.; Sánchez-García, I.; Pancorbo-Hidalgo, P.L. Knowledge, Attitude and Use of Evidence-Based Practice among nurses active on the Internet. Investig. Educ. Enfermería 2014, 32, 451–460. [Google Scholar] [CrossRef] [Green Version]
- Chu, T.-L.; Wang, J.; Monrouxe, L.; Sung, Y.-C.; Kuo, C.-l.; Ho, L.-H.; Lin, Y.-E. The effects of the flipped classroom in teaching evidence based nursing: A quasi-experimental study. PLoS ONE 2019, 14, e0210606. [Google Scholar] [CrossRef] [PubMed]
- Koota, E.; Kääriäinen, M.; Kyngäs, H.; Lääperi, M.; Melender, H.L. Effectiveness of evidence-based practice (ebp) education on emergency nurses’ ebp attitudes, knowledge, self-efficacy, skills, and behavior: A randomized controlled trial. Worldviews Evid.-Based Nurs. 2021, 18, 23–32. [Google Scholar] [CrossRef]
- Bergmann, J.; Sams, A. Flip your Classroom: Reach Every Student in Every Class Every Day; International Society for Technology in Education: Eugene, OR, USA, 2012. [Google Scholar]
- McDonald, K.; Smith, C.M. The flipped classroom for professional development: Part I. Benefits and strategies. J. Contin. Educ. Nurs. 2013, 44, 437–438. [Google Scholar] [CrossRef]
- Santos, M.C. Nurses’ barriers to learning: An integrative review. J. Nurses Prof. Dev. 2012, 28, 182–185. [Google Scholar] [CrossRef]
- Hessler, K.L. Nursing education: Flipping the classroom. Nurse Pract. 2016, 41, 17–27. [Google Scholar] [CrossRef]
- Onda, M.; Takagaki, N. Approach to Evidence-based Medicine Exercises Using Flipped Teaching: Introductory Education for Clinical Practice for 4th-Year Pharmacy Students. Yakugaku Zasshi J. Pharm. Soc. Jpn. 2018, 138, 645–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilboy, M.B.; Heinerichs, S.; Pazzaglia, G. Enhancing student engagement using the flipped classroom. J. Nutr. Educ. Behav. 2015, 47, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Hwang, G.-J.; Chen, P.-Y. Effects of a collective problem-solving promotion-based flipped classroom on students’ learning performances and interactive patterns. Interact. Learn. Environ. 2019, 1–16. [Google Scholar] [CrossRef]
- Hwang, G.-J.; Wu, P.-H.; Chen, C.-C. An online game approach for improving students’ learning performance in web-based problem-solving activities. Comput. Educ. 2012, 59, 1246–1256. [Google Scholar] [CrossRef]
- Jones-Bonofiglio, K.D.; Willett, T.; Ng, S. An evaluation of flipped e-learning experiences. Med. Teach. 2018, 40, 953–961. [Google Scholar] [CrossRef]
- Kuo, F.-R.; Hwang, G.-J.; Lee, C.-C. A hybrid approach to promoting students’ web-based problem-solving competence and learning attitude. Comput. Educ. 2012, 58, 351–364. [Google Scholar] [CrossRef]
- Kumaravel, B.; Hearn, J.H.; Jahangiri, L.; Pollard, R.; Stocker, C.J.; Nunan, D. A systematic review and taxonomy of tools for evaluating evidence-based medicine teaching in medical education. Syst. Rev. 2020, 9, 91. [Google Scholar] [CrossRef]
- Häggman-Laitila, A.; Mattila, L.R.; Melender, H.L. Educational interventions on evidence-based nursing in clinical practice: A systematic review with qualitative analysis. Nurse Educ. Today 2016, 43, 50–59. [Google Scholar] [CrossRef]
- Lee, C.-Y.; Wang, W.-F.; Chang, Y.-J. The Effects of Evidence-Based Nursing Training Program on Nurses’ Knowledge, Attitude, and Behavior. New Taipei J. Nurs. 2011, 13, 19–31. [Google Scholar] [CrossRef]
- Rose Bovino, L.; Aquila, A.M.; Bartos, S.; McCurry, T.; Cunningham, C.E.; Lane, T.; Rogucki, N.; DosSantos, J.; Moody, D.; Mealia-Ospina, K.; et al. A Cross-sectional Study on Evidence-Based Nursing Practice in the Contemporary Hospital Setting: Implications for Nurses in Professional Development. J. Nurses Prof. Dev. 2017, 33, 64–69. [Google Scholar] [CrossRef]
- Salah, M.m.A.; Abu-Moghli, F.A. Perceived Knowledge, Attitudes, and Implementation of Evidence-Based Practice Among Jordanian Nurses in Critical Care Units. Dimens. Crit. Care Nurs. 2020, 39, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Moore, L. Effectiveness of an Online Educational Module in Improving Evidence-Based Practice Skills of Practicing Registered Nurses. Worldviews Evid.-Based Nurs. 2017, 14, 358–366. [Google Scholar] [CrossRef] [PubMed]
- van der Goot, W.E.; Keers, J.C.; Kuipers, R.; Nieweg, R.M.B.; de Groot, M. The effect of a multifaceted evidence-based practice programme for nurses on knowledge, skills, attitudes, and perceived barriers: A cohort study. Nurse Educ. Today 2018, 63, 6–11. [Google Scholar] [CrossRef]
- Moye, J.J.; Dugger, W.E., Jr.; Starkweather, K.N. Is “Learning by Doing” Important? A Study of Doing-Based Learning. Technol. Eng. Teach. 2014, 74, 22–28. [Google Scholar]
- Chung, C.-J.; Lai, C.-L.; Hwang, G.-J. Roles and research trends of flipped classrooms in nursing education: A review of academic publications from 2010 to 2017. Interact. Learn. Environ. 2019, 29, 883–904. [Google Scholar] [CrossRef]
- Hwang, G.-J.; Lai, C.-L.; Wang, S.-Y. Seamless flipped learning: A mobile technology-enhanced flipped classroom with effective learning strategies. J. Comput. Educ. 2015, 2, 449–473. [Google Scholar] [CrossRef]
- ten Cate, O. What happens to the student? The neglected variable in educational outcome research. Adv. Health Sci. Educ. 2001, 6, 81–88. [Google Scholar] [CrossRef]
- Hampton, D.C.; Keys, Y. Generation Z students: Will they change our nursing classrooms. J. Nurs. Educ. Pract. 2017, 7, 111–115. [Google Scholar] [CrossRef] [Green Version]



| CL (n = 57) | FL (n = 57) | |||
|---|---|---|---|---|
| Variable | n (%) | n (%) | t/X2 | p |
| Age (years), mean (SD) | 32.54 (8.84) | 33.84 (7.53) | −0.84 | 0.401 |
| Sex | 0.65 | >0.999 | ||
| Female | 55 (96.49) | 54 (94.74) | ||
| Male | 2 (3.51) | 3 (5.26) | ||
| Education level | 0.04 | >0.999 | ||
| Diploma | 20 (35.09) | 19 (33.33) | ||
| College and above | 37 (64.91) | 38 (66.67) | ||
| a Career ladder | 8.98 | 0.000 | ||
| N–N1 | 36 (63.16) | 20 (35.09) | ||
| N2–N4 | 21 (36.84) | 37 (64.91) | ||
| Working years | 12.93 | 0.000 | ||
| 5 and under 5 | 29 (50.88) | 14 (24.56) | ||
| 6–10 | 6 (10.53) | 14 (24.56) | ||
| 11–15 | 7 (12.28) | 17 (29.82) | ||
| 16 and above | 15 (26.32) | 12 (21.05) | ||
| English proficiency | 1.00 | 0.422 | ||
| Acceptable to good and above | 16 (28.07) | 21 (36.84) | ||
| Unacceptable | 41 (71.93) | 36 (63.16) | ||
| Daily working hours | 1.55 | 0.465 | ||
| 8 | 5 (8.77) | 6 (10.53) | ||
| 8–9 | 42 (73.68) | 36 (63.16) | ||
| 9–10 | 10 (17.54) | 15 (26.32) | ||
| Work unit | 0.78 | 0.851 | ||
| Medical, obstetrics and gynecology, pediatrics | 16 (28.07) | 19 (33.33) | ||
| Surgical and operation room | 8 (14.04) | 9 (15.79) | ||
| b Others | 19 (33.33) | 15 (26.32) | ||
| Intensive care unit | 14 (24.56) | 14 (24.56) | ||
| Workload perception | 0.16 | 0.832 | ||
| Stressful and incompetent | 16 (28.07) | 18 (31.58) | ||
| Competent | 41 (71.93) | 39 (68.42) | ||
| Participation motivation | 0.36 | 0.833 | ||
| Interest and self−professional growth | 24 (42.11) | 21 (36.84) | ||
| Unit assigned | 26 (45.61) | 29 (50.88) | ||
| Work required | 7 (12.28) | 7 (12.28) | ||
| Experienced literature seeking | 0.14 | 0.700 | ||
| Yes | 26 (45.61) | 28 (49.12) | ||
| No | 31 (54.39) | 29 (50.88) | ||
| Experienced critical appraisal | 0.00 | >0.999 | ||
| Yes | 29 (50.88) | 29 (50.88) | ||
| No | 28 (49.12) | 28 (49.12) | ||
| Experienced critical appraisal in a team | 0.14 | 0.851 | ||
| Yes | 24 (42.11) | 26 (45.61) | ||
| No | 33 (57.89) | 31 (54.39) | ||
| Experienced learning through EBP | 0.14 | 0.852 | ||
| Yes | 32 (56.14) | 30 (52.63) | ||
| No | 25 (43.86) | 27 (47.37) |
| CL Group (n = 57) | FL Group (n = 57) | Between Two Groups | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item | T0 | T1 | T2 | T3 | pA | T0 | T1 | T2 | T3 | pB | pC | pD | pE | pF |
| Mean (SD) | p-Value | Mean (SD) | p-Value | p-Value | ||||||||||
| K | 8.11 (0.95) | 8.61 (0.92) | 8.39 (0.88) | 7.80 (0.95) | 0.000 *** | 8.37 (0.97) | 8.61 (1.03) | 8.44 (1.17) | 8.48 (1.05) | 0.040 * | 0.153 | 1.000 | 0.702 | 0.001 ** |
| A | 31.49 (3.67) | 33.61 (4.04) | 33.93 (3.98) | 33.40 (4.14) | 0.000 ** | 30.67 (3.25) | 34.04 (3.92) | 32.61 (3.68) | 32.74 (3.85) | 0.000 *** | 0.213 | 0.517 | 0.010 ** | 0.372 |
| P | 27.07 (7.02) | 34.14 (7.79) | 33.47 (7.73) | 35.90 (8.08) | 0.000 *** | 27.88 (6.25) | 33.77 (6.59) | 34.82 (6.49) | 33.89 (6.19) | 0.000 *** | 0.573 | 0.792 | 0.153 | 0.160 |
| Model 1 | Model 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | 95% CI | p | Estimate | SE | 95% CI | p | |
| Knowledge | ||||||||
| Group (FL vs. CL) | −0.21 | 0.14 | −0.49, 0.07 | 0.13 | −0.24 | 0.18 | −0.60, 0.12 | 0.19 |
| Test (Time) | ||||||||
| T1 vs. T0 | 0.38 | 0.08 | 0.22, 0.54 | <0.0001 | −0.02 | 0.26 | −0.53, 0.50 | 0.95 |
| T2 vs. T0 | 0.18 | 0.10 | −0.02, 0.37 | 0.08 | −0.04 | 0.33 | −0.80, 0.52 | 0.68 |
| T3 vs. T0 | −0.10 | 0.11 | −0.30, 0.11 | 0.36 | 0.52 | 0.30 | −0.06, 1.10 | 0.08 |
| Group × Test | ||||||||
| T1 vs. T0 | 0.26 | 0.16 | −0.05, 0.58 | 0.10 | ||||
| T2 vs. T0 | 0.21 | 0.20 | −0.18, 0.60 | 0.29 | ||||
| T3 vs. T0 | −0.41 | 0.21 | −0.82, −0.002 | 0.049 | ||||
| Attitude | ||||||||
| Group (FL vs. CL) | 0.70 | 0.50 | −0.28, 1.69 | 0.16 | 0.93 | 0.66 | −0.37, 2.23 | 0.16 |
| Test | ||||||||
| T1 vs. T0 | 2.75 | 0.46 | 1.84, 3.65 | <0.0001 | 4.61 | 1.43 | 1.82, 7.41 | 0.001 |
| T2 vs. T0 | 2.19 | 0.42 | 1.38, 3.01 | <0.0001 | 1.46 | 1.44 | −1.36, 4.27 | 0.31 |
| T3 vs. T0 | 1.99 | 0.41 | 1.18, 2.79 | <0.0001 | 2.20 | 1.43 | −0.61, 5.01 | 0.13 |
| Group × Test | ||||||||
| T1 vs. T0 | −1.25 | 0.91 | −3.04, 0.54 | 0.17 | ||||
| T2 vs. T0 | 0.49 | 0.83 | −1.14, 2.12 | 0.56 | ||||
| T3 vs. T0 | −0.14 | 0.82 | −1.75, 1.47 | 0.86 | ||||
| Practice | ||||||||
| Group (FL vs. CL) | 0.22 | 0.89 | −1.53, 1.96 | 0.81 | −0.58 | 1.27 | −3.06, 1.91 | 0.65 |
| Test | ||||||||
| T1 vs. T0 | 6.48 | 0.92 | 4.67, 8.29 | <0.0001 | 4.72 | 2.76 | −0.69, 10.1 | 0.09 |
| T2 vs. T0 | 6.68 | 0.76 | 5.19, 8.16 | <0.0001 | 7.49 | 2.01 | 3.55, 11.4 | 0.0002 |
| T3 vs. T0 | 7.41 | 0.78 | 5.89, 8.93 | <0.0001 | 3.20 | 2.05 | −0.81, 7.21 | 0.01 |
| Group × Test | ||||||||
| T1 vs. T0 | 1.18 | 1.85 | −2.44, 4.79 | 0.52 | ||||
| T2 vs. T0 | −0.54 | 1.52 | −3.52, 2.43 | 0.72 | ||||
| T3 vs. T0 | 2.80 | 1.52 | −0.18, 5.79 | 0.07 | ||||
| Item | CL (n = 57) | FL (n = 57) | p |
|---|---|---|---|
| Mean (SD) | |||
| 1. I could understand EBP through the course content. | 3.75 (1.15) | 4.46 (0.66) | <0.000 *** |
| 2. I learned how to ask a clinical question. | 3.82 (1.04) | 4.42 (0.53) | <0.000 *** |
| 3. The course strengthens my ability to search for the empirical literature. | 3.82 (1.02) | 4.46 (0.50) | <0.000 *** |
| 4. The course improved my ability to critique the literature. | 3.84 (1.01) | 4.44 (0.50) | <0.000 *** |
| 5. I could apply EBP in clinical care. | 3.84 (1.01) | 4.39 (0.56) | 0.001 ** |
| 6. The course enhanced my confidence in the instructor in the clinical application of evidence-based nursing. | 3.84 (1.01) | 4.42 (0.57) | <0.000 *** |
| 7. The case discussion helped me understand EBP. | 3.88 (1.05) | 4.44 (0.50) | <0.000 *** |
| 8. Practical experience improved my ability to search for empirical literature. | 3.96 (0.96) | 4.44 (0.50) | 0.001 ** |
| 9. Group discussions enhanced my ability to critique the literature. | 3.86 (0.97) | 4.40 (0.49) | <0.000 *** |
| 10. The workshop helped me complete the EBP 5As and apply them to clinical care. | 3.88 (0.98) | 4.35 (0.52) | 0.002 * |
| Total score | 38.49 (0.99) | 44.24 (0.60) | 0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chao, W.-Y.; Huang, L.-C.; Hung, H.-C.; Hung, S.-C.; Chuang, T.-F.; Yeh, L.-Y.; Tseng, H.-C. Effectiveness of Digital Flipped Learning Evidence-Based Practice on Nurses’ Knowledge, Attitude, and Practice: A Quasi-Experimental Trial. Healthcare 2022, 10, 1257. https://doi.org/10.3390/healthcare10071257
Chao W-Y, Huang L-C, Hung H-C, Hung S-C, Chuang T-F, Yeh L-Y, Tseng H-C. Effectiveness of Digital Flipped Learning Evidence-Based Practice on Nurses’ Knowledge, Attitude, and Practice: A Quasi-Experimental Trial. Healthcare. 2022; 10(7):1257. https://doi.org/10.3390/healthcare10071257
Chicago/Turabian StyleChao, Wen-Yi, Li-Chi Huang, Hung-Chang Hung, Shih-Chang Hung, Tzung-Fang Chuang, Li-Yueh Yeh, and Hui-Chen Tseng. 2022. "Effectiveness of Digital Flipped Learning Evidence-Based Practice on Nurses’ Knowledge, Attitude, and Practice: A Quasi-Experimental Trial" Healthcare 10, no. 7: 1257. https://doi.org/10.3390/healthcare10071257
APA StyleChao, W.-Y., Huang, L.-C., Hung, H.-C., Hung, S.-C., Chuang, T.-F., Yeh, L.-Y., & Tseng, H.-C. (2022). Effectiveness of Digital Flipped Learning Evidence-Based Practice on Nurses’ Knowledge, Attitude, and Practice: A Quasi-Experimental Trial. Healthcare, 10(7), 1257. https://doi.org/10.3390/healthcare10071257






