CT-Based Radiomic Analysis May Predict Bacteriological Features of Infected Intraperitoneal Fluid Collections after Gastric Cancer Surgery
Abstract
:1. Introduction
2. Materials and Methods
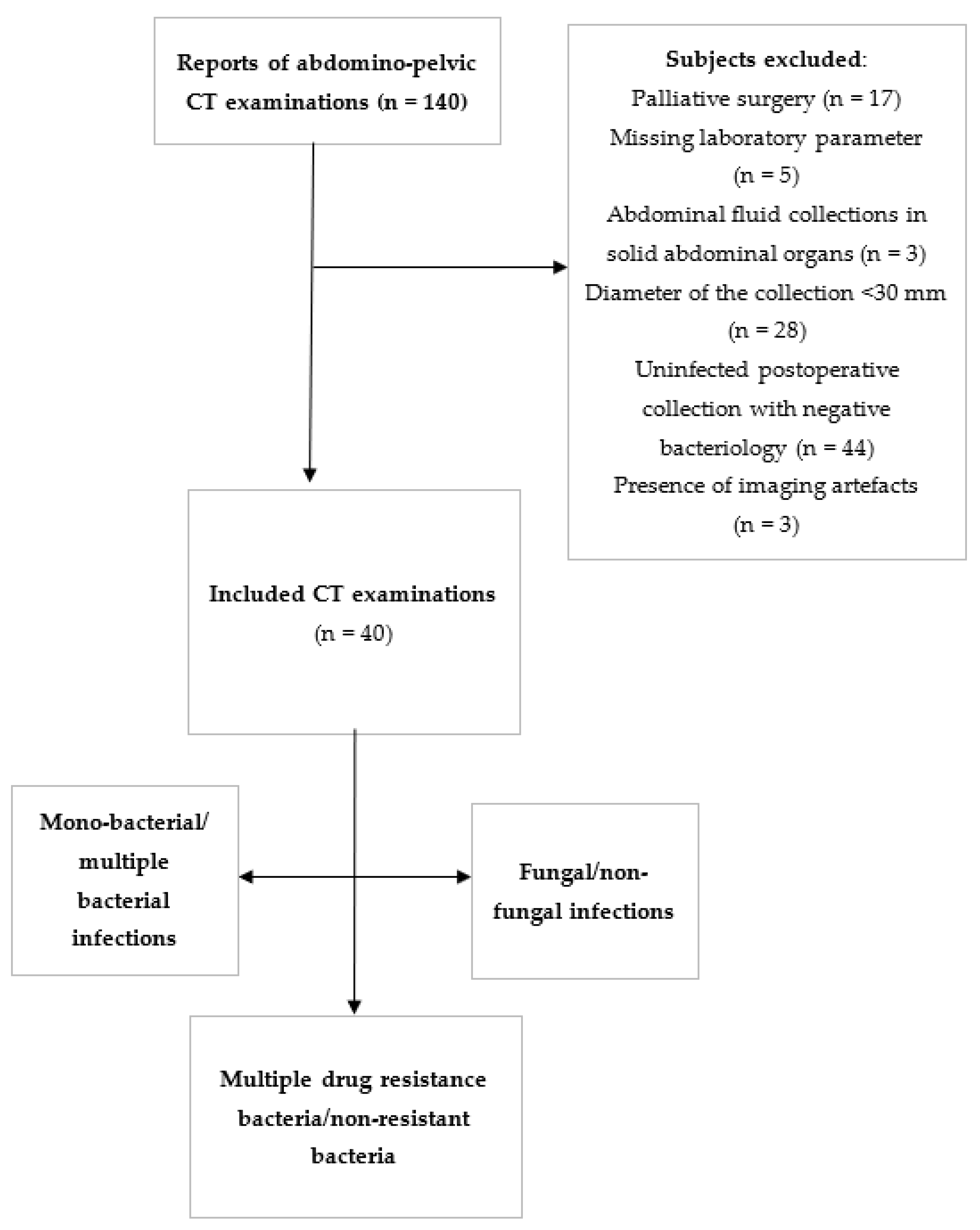
2.1. Patients
2.2. Reference Standard
2.3. Image Acquisition
2.4. Image Interpretation
2.5. Texture Analysis
2.5.1. Image Pre-Processing and Segmentation
2.5.2. Feature Extraction
2.5.3. Feature Selection
2.5.4. Class Prediction
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zimmerman, L.H.; Tyburski, J.G.; Glowniak, J.; Singla, R.; Lavery, T.; Nailor, M.; Stassinopoulus, J.; Hong, K.; Barshikar, S.; Dolman, H.S.; et al. Impact of evaluating antibiotic concentrations in abdominal abscesses percutaneously drained. Am. J. Surg. 2011, 201, 348. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.P.; Condon, R.E. Peritonitis and intraabdom-inal abscesses. In Principles of Surgery, 5th ed.; Schwartz, S.I., Ed.; McGraw-Hill: New York, NY, USA, 1989; pp. 1479–1489. [Google Scholar]
- Lorber, B.; Swenson, R.M. The bacteriology of intra-ab-dominal infections. Surg. Clin. N. Am. 1975, 55, 1349–1354. [Google Scholar] [CrossRef]
- Sirine, K.R. Diagnosis and treatment of intra-abdominal abscesses. Surg. Infect. 2000, 1, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Halber, M.D.; Daffner, R.H.; Morgan, C.L.; Trought, W.S.; Thompson, W.M.; Rice, R.P.; Korobkin, M. Intraabdominal abscess: Current concepts in radiologic evaluation. AJR Am. J. Roentgenol. 1979, 133, 9–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haaga, J.R.; Alfidi, R.J.; Havrilla, T.R.; Cooperman, A.M.; Seidelmann, F.E.; Reich, N.E.; Weinstein, A.J.; Meaney, T.F. CT detection and aspiration of abdominal abscesses. AJR Am. J. Roentgenol. 1977, 128, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Jaques, P.; Mauro, M.; Safrit, H.; Yankaskas, B.; Piggott, B. CT features of intraabdominal abscesses: Prediction of successful percutaneous drainage. AJR Am. J. Roentgenol. 1986, 146, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.M.; Sirlin, C.B.; Pinto, P.S.; Jeffrey, R.B.; Stella, D.L.; Casola, G. Disproportionate fat stranding: A helpful CT sign in patients with acute abdominal pain. Radiographics 2004, 24, 703. [Google Scholar] [CrossRef]
- Gnannt, R.; Fischer, M.A.; Baechler, T.; Clavien, P.A.; Karlo, C.; Seifert, B.; Lesurtel, M.; Alkadhi, H. Distinguishing infected from noninfected abdominal fluid collections after surgery: An imaging, clinical, and laboratory-based scoring system. Investig. Radiol. 2015, 50, 17–23. [Google Scholar] [CrossRef] [Green Version]
- Howard, R.J.; Simmons, R.L. (Eds.) Peritonitis and other intraabdominal infections. In Surgical Infectious Diseases; Appleton & Lange: Norwalk, CT, USA, 1988; p. 605. [Google Scholar]
- Vipond, M.N.; Whawell, S.A.; Thompson, J.N.; Dudley, H.A. Effect of experimental peritonitis and ischaemia on peritoneal fibrinolytic activity. Eur. J. Surg. 1994, 160, 471–477. [Google Scholar]
- Thompson, J.N.; Paterson-Brown, S.; Harbourne, T.; Whawell, S.A.; Kalodiki, E.; Dudley, H.A. Reduced human peritoneal plasminogen activating activity: Possible mechanism of adhesion formation. Br. J. Surg. 1989, 76, 382–384. [Google Scholar] [CrossRef]
- Allen, B.C.; Barnhart, H.; Bashir, M.; Nieman, C.; Breault, S.; Jafe, T.A. Diagnostic accuracy of intra-abdominal fuid collection characterization in the era of multidetector computed tomography. Am. Surg. 2012, 78, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Radosa, C.G.; Radosa, J.C.; Laniado, M.; Brandt, J.; Streitzig, J.; Seppelt, D.; Volk, A.; Plodeck, V.; Kühn, J.P.; Hoffmann, R.T. Infected versus sterile abdominal fluid collections in postoperative CT: A scoring system based on clinical and imaging findings. Abdom. Radiol. 2020, 45, 2871–2878. [Google Scholar] [CrossRef] [PubMed]
- Skusa, C.; Skusa, R.; Wohlfarth, M.; Warnke, P.; Podbielski, A.; Bath, K.; Grob, J.; Schafmayer, C.; Frickmann, H.; Weber, M.A.; et al. Imaging and Clinical Parameters for Distinction between Infected and Non-Infected Fluid Collections in CT: Prospective Study Using Extended Microbiological Approach. Diagnostics 2022, 12, 493. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.L.; Xia, H.H.X.; Zhu, S.L. Ascitic Fluid Analysis in the Dif-ferential Diagnosis of Ascites: Focus on Cirrhotic Ascites. J. Clin. Transl. Hepatol. 2014, 2, 58–64. [Google Scholar] [PubMed] [Green Version]
- Lupean, R.A.; Ștefan, P.A.; Oancea, M.D.; Măluțan, A.M.; Lebovici, A.; Pușcaș, M.E.; Csutak, C.; Mihu, C.M. Computer Tomography in the Diagnosis of Ovarian Cysts: The Role of Fluid Attenuation Values. Healthcare 2020, 14, 398. [Google Scholar] [CrossRef]
- Lupean, R.A.; Ștefan, P.A.; Lebovici, A.; Csutak, C.; Rusu, G.M.; Mihu, C.M. Differentiation of Endometriomas from Hemorrhagic cysts at Magnetic Resonance: The Role of Quantitative Signal Intensity Measurements. Curr. Med. Imaging 2020, 17, 524–531. [Google Scholar] [CrossRef]
- Lebovici, A.; Csutak, C.; Popa, P.; Crisan, N.; Suciu, M.; Feciche, M.; Andraș, I.; Ștefan, P.-A.; Feier, D. Magnetic resonance imaging characteristics of chronic prostatitis in patients under the age of 50: Is it more than the eye can see? Acta Radiol. 2021, 839–846. [Google Scholar] [CrossRef]
- Van Timmeren, J.E.; Cester, D.; Tanadini-Lang, S.; Alkadhi, H.; Baessler, B. Radiomics in medical imaging—“how-to” guide and critical reflection. Insights Imaging 2020, 11, 91. [Google Scholar] [CrossRef]
- Csutak, C.; Ștefan, P.A.; Lenghel, L.M.; Moroșanu, C.O.; Lupean, R.-A.; Șimonca, L.; Mihu, C.M.; Lebovici, A. Differentiating High-Grade Gliomas from Brain Metastases at Magnetic Resonance: The Role of Texture Analysis of the Peritumoral Zone. Brain Sci. 2020, 10, 638. [Google Scholar] [CrossRef]
- Mannil, M.; Von Spiczak, J.; Manka, R.; Alkadhi, H. Texture Analysis and Machine Learning for Detecting Myocardial Infarction in Noncontrast Low-Dose Computed Tomography. Investig. Radiol. 2018, 53, 338–343. [Google Scholar] [CrossRef]
- Montravers, P.; Dupont, H.; Leone, M.; Constantin, J.M.; Mertes, P.M.; Laterre, P.F.; Société française d’anesthésie et de réanimation (Sfar); Société de réanimation de langue française (SRLF); Misset, B.; Société de pathologie infectieuse de langue française (SPILF); et al. Guidelines for management of intra-abdominal infections. Anaesth. Crit. Care Pain Med. 2015, 34, 117–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dupont, H.; Bourichon, A.; Paugam-Burtz, C.; Mantz, J.; Desmonts, J.M. Can yeast isolation in peritoneal fluid be predicted in intensive care unit patients with peritonitis? Crit. Care Med. 2003, 31, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Winn, W. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1997; p. 2Y110. [Google Scholar]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mărginean, L.; Ștefan, P.A.; Lebovici, A.; Opincariu, I.; Csutak, C.; Lupean, R.A.; Coroian, P.A.; Suciu, B.A. CT in the Differentiation of Gliomas from Brain Metastases: The Radiomics Analysis of the Peritumoral Zone. Brain Sci. 2022, 12, 109. [Google Scholar] [CrossRef]
- Lupean, R.A.; Ștefan, P.A.; Csutak, C.; Lebovici, A.; Măluțan, A.M.; Buiga, R.; Melincovici, C.S.; Mihu, C.M. Differentiation of Endometriomas from Ovarian Hemorrhagic Cysts at Magnetic Resonance: The Role of Texture Analysis. Medicina 2020, 56, 487. [Google Scholar] [CrossRef]
- Ardakani, A.A.; Rasekhi, A.; Mohammadi, A.; Motevalian, E.; Najafabad, B.K. Differentiation between metastatic and tumour-free cervical lymph nodes in patients with papillary thyroid carcinoma by grey-scale sonographic texture analysis. Pol. J. Radiol. 2018, 83, e37–e46. [Google Scholar] [CrossRef]
- Ștefan, P.A.; Lupean, R.A.; Mihu, C.M.; Lebovici, A.; Oancea, M.D.; Hîțu, L.; Duma, D.; Csutak, C. Ultrasonography in the Diagnosis of Adnexal Lesions: The Role of Texture Analysis. Diagnostics 2021, 11, 812. [Google Scholar] [CrossRef]
- Lupean, R.A.; Ștefan, P.A.; Feier, D.S.; Csutak, C.; Ganeshan, B.; Lebovici, A.; Petresc, B.; Mihu, C.M. Radiomic Analysis of MRI Images is Instrumental to the Stratification of Ovarian Cysts. J. Pers. Med. 2020, 10, 127. [Google Scholar] [CrossRef]
- Vaishali, D.; Ramesh, R.; Anita, C. 2D autoregressive model for texture analysis and synthesis. In Proceedings of the 2014 International Conference on Communication and Signal Processing, Bangkok, Thailand, 10–12 October 2014; pp. 1135–1139. [Google Scholar]
- Ha, S.; Choi, H.; Cheon, G.J.; Kang, K.W.; Chung, J.K.; Kim, E.E.; Lee, D.S. Autoclustering of Non-small Cell Lung Carcinoma Subtypes on (18)F-FDG PET Using Texture Analysis: A Preliminary Result. Nucl. Med. Mol. Imaging 2014, 48, 278–286. [Google Scholar] [CrossRef] [Green Version]
- Mital, D.P.; Leng, G.W. An Autoregressive Approach to Surface Texture Analysis. Int. J. Pattern Recognit. Artif. Intell. 1994, 8, 845–857. [Google Scholar] [CrossRef]
- Abbadeni, N. Perceptual meaning of the estimated parameters of the autoregressive model. In Proceedings of the IEEE International Conference on Image Processing, Genoa, Italy, 11–14 September 2005; p. III-1164. [Google Scholar]
- O’Byrne, M.; Schoefs, F.; Ghosh, B.; Pakrashi, V. Texture Analysis based Detection and Classification of Surface Features on Ageing Infrastructure Elements. In Proceedings of the Bridge and Concrete Research in Ireland, Dublin, Ireland, 6 September 2012; pp. 271–275. [Google Scholar]
- Sullivan, A.; Edlund, C.; Nord, C.E. Effect of antimicrobial agents on the ecological balance of human microflora. Lancet Infect. Dis. 2001, 1, 101–114. [Google Scholar] [CrossRef]
- Brook, I. Microbiology of polymicrobial abscesses and implications for therapy. J. Antimicrob. Chemother. 2002, 50, 805–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bartlett, J.G. Intra-abdominal sepsis. Med. Clin. N. Am. 1995, 79, 599–617. [Google Scholar] [CrossRef]
- Broche, A.; Tellado, J. Defense mechanisms of the peritoneal cavity. Curr. Opin. Crit. Care 2001, 7, 105–116. [Google Scholar] [CrossRef]
- Onderdonk, A.; Weinstein, W.; Sullivan, N.; Bartlett, J.; Gobach, S. Experimental intraabdominal abscesses in rats: Quantitative bacteriology of infected animals. Infect. Immun. 1974, 10, 1256–1259. [Google Scholar] [CrossRef] [Green Version]
- Duerden, I. Virulence factors in anaerobes. Clin. Infect. Dis. 1994, 18, 253–259. [Google Scholar] [CrossRef]
- Incoronato, M.; Aiello, M.; Infante, T.; Cavaliere, C.; Grimaldi, A.M.; Mirabelli, P.; Monti, S.; Salvatore, M. Radiogenomic analysis of oncological data: A technical survey. Int. J. Mol. Sci. 2017, 18, 805. [Google Scholar] [CrossRef] [Green Version]
- Ștefan, P.A.; Lebovici, A.; Csutak, C.; Mihu, C.M. Computer Tomography in the Diagnosis of Ascites: The Role of Fluid Attenuation Values. Curr. Med. Imaging 2021, 17, 390–395. [Google Scholar] [CrossRef]
- Ștefan, P.A.; Csutak, C.; Lebovici, A.; Rusu, G.M.; Mihu, C.M. Diffusion-Weighted Magnetic Resonance Imaging as a Noninvasive Parameter for Differentiating Benign and Malignant Intraperitoneal Collections. Medicina 2020, 56, 217. [Google Scholar] [CrossRef]
- Csutak, C.; Ștefan, P.A.; Lupean, R.A.; Lenghel, L.M.; Mihu, C.M.; Lebovici, A. Computed tomography in the diagnosis of intraperitoneal effusions: The role of texture analysis. Bosn. J. Basic Med. Sci. 2021, 21, 488–494. [Google Scholar] [CrossRef]
- Stefan, P.A.; Puscas, M.E.; Csuak, C.; Lebovici, A.; Petresc, B.; Lupean, R.; Mihu, C.M. The utility of texture-based classification of different types of ascites on magnetic resonance. J. BUON 2020, 25, 1237–1244. [Google Scholar]
- Just, N. Improving tumour heterogeneity MRI assessment with histo-grams. Br. J. Cancer 2014, 111, 2205–2213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puia, V.R.; Puia, A.; Fetti, A.C.; Stefan, P.A.; Valean, D.; Herdean, A.; Rusu, I.; Vasile, T.; Lebovici, A.; Al-Hajjar, N. Computed Tomography for the Diagnosis of Intraperitoneal Infected Fluid Collections after Surgery for Gastric Cancer. Role of Texture Analysis. J. Gastrointestin Liver Dis. 2022, 31, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Meyer, H.J.; Schnarkowski, B.; Leonhardi, J.; Mehdorn, M.; Ebel, S.; Goessmann, H.; Denecke, T. CT Texture analysis and CT scores for characterization of fluid collections. BMC Med. Imaging 2021, 21, 187. [Google Scholar] [CrossRef] [PubMed]
- Ordonez, A.A.; Jain, S.K. Pathogen-specific Bacterial Imaging in Nuclear Medicine. Semin. Nucl. Med. 2018, 48, 182–194. [Google Scholar] [CrossRef]


| Parameters | Class | Computational Variations | Computation Method |
|---|---|---|---|
| Teta 1–4, Sigma | ARM | - | - |
| GrNonZeros, percentage of pixels with nonzero gradient, GrMean, GrVariance, GrSkewness, GrKurtosis | AR | - | 4 bits/pixel |
| Perc.01–99%, Skewness, Kurtosis, Variance, Mean | Histogram | - | - |
| GLevNonU, LngREmph, RLNonUni, ShrtREmp, Fraction | RLM | 4 directions | 6 bits/pixel |
| InvDfMom, SumAverg, SumVarnc, SumEntrp, Entropy, DifVarnc, DifEntrp, AngScMom, Contrast, Correlat, SumOfSqs | COM | 4 directions | 6 bits/pixel; 5 between-pixel distances |
| WavEn | WT | 4 frequency bands | 5 scales |
| Fungal vs. Non-Fungal | Fungal | Non-Fungal | p-Value | ||
| Median | IQR | Median | IQR | ||
| ATeta3 | 0.23 | 0.18–0.43 | 0.42 | 0.36–0.52 | 0.02 |
| ATeta4 | 0.05 | 0.01–0.16 | −0.009 | −011–0.04 | 0.02 |
| CZ1D6Contrast | 0.34 | 0.14–2.6 | 0.87 | 0.10–8.53 | 0.43 |
| CN2D6Correlat | 0.09 | 0.06–0.15 | 0.04 | −0.002–0.12 | 0.10 |
| RND6RLNonUni | 140.61 | 59.45–653.45 | 498.60 | 38.69–1580.42 | 0.37 |
| CH4D6Correlat | 0.07 | 0.04–0.13 | 0.07 | 0.004–0.10 | 0.40 |
| GD4Skewness | 1.17 | 0.28–1.34 | 0.36 | 0.11–2.02 | 0.49 |
| CV1D6Contrast | 0.32 | 0.13–1.97 | 0.68 | 0.08–7.11 | 0.49 |
| RVD6RLNonUni | 95.78 | 43.84–571.62 | 506.96 | 22.78–1450.85 | 0.43 |
| CH1D6AngScMom | 0.35 | 0.13–0.73 | 0.19 | 0.01–0.80 | 0.40 |
| Mono vs. Multiple-bacterial | Monobacterial | Multiple-bacterial | p-value | ||
| Median | IQR | Median | IQR | ||
| CN5D6Correlat | 0.08 | 0.02–0.15 | 0.01 | −0.03–0.06 | 0.04 |
| ATeta2 | −0.18 | −0.25–0.01 | −0.15 | −0.28–−0.03 | 0.75 |
| CN2D6AngScMom | 0.11 | 0.04–0.30 | 0.04 | −0.003–0.08 | 0.03 |
| WavEnHL_s-2 | 0.47 | 0.13–3.02 | 0.74 | 0.16–16.06 | 0.34 |
| RVD6LngREmph | 27.84 | 3.75–539.08 | 9.43 | 1.62–61.38 | 0.13 |
| CH1D6Contrast | 0.23 | 0.05–1.31 | 0.40 | 0.12–5.99 | 0.19 |
| RZD6GLevNonU | 223.30 | 117.44–505.92 | 169.84 | 90.70–228.98 | 0.25 |
| RHD6LngREmph | 35.00 | 4.31–513.91 | 11.68 | 1.69–89.29 | 0.15 |
| ATeta4 | −0.02 | −0.12–0.04 | 0.03 | 0.01–0.14 | 0.12 |
| Perc01 | 1001.5 | 113.5–1019.5 | 90.00 | 78.00–994.25 | 0.02 |
| Multi vs. Non-Multiresistant | Multiresistant | Non-Multiresistant | p-value | ||
| Median | IQR | Median | IQR | ||
| RND6GLevNonU | 187.76 | 120.15–384.61 | 157.79 | 100.10–212.03 | 0.29 |
| CH1D6DifVarnc | 1.33 | 0.13–2.35 | 0.26 | 0.06–1.31 | 0.24 |
| GD4Kurtosis | 0.26 | −1.08–0.50 | 0.19 | −0.44–12.85 | 0.47 |
| RHD6GLevNonU | 165.87 | 91.77–369.11 | 131.18 | 89.00–184.78 | 0.24 |
| ATeta1 | 0.51 | 0.33–0.58 | 0.59 | 0.36–0.69 | 0.34 |
| CN5D6Correlat | 0.01 | −0.02–0.05 | 0.03 | −0.01–0.09 | 0.43 |
| WavEnLL_s-1 | 10,243.16 | 4182.69–12,237.74 | 10398 | 4286.96–16013.20 | 0.37 |
| CN4D6Correlat | 0.04 | −0.04–0.06 | 0.03 | 0.00–0.09 | 0.53 |
| Kurtosis | 0.47 | 0.21–1.25 | 0.73 | 0.24–4.71 | 0.47 |
| CN2D6Contrast | 0.04 | 0.00–0.07 | 0.07 | 0.04–0.21 | 0.04 |
| Parameter | Sign.lvl. | AUC | J | Cut-Off | Se (%) | Sp |
|---|---|---|---|---|---|---|
| Fungi vs. non-fungi | ||||||
| ATeta3 | 0.0137 | 0.765 (0.564–0.906) | 0.5556 | ≤0.23 | 55.5 (21.2–86.3) | 100 (81.5–100) |
| ATeta4 | 0.003 | 0.772 (0.571–0.91) | 0.5 | >−0.024 | 100 (66.4–100) | 50 (26–74) |
| Combined Teta model | <0.0001 | 0.877 (0.717–1) | 0.72 | >0.49 | 77.78 (40.0–97.2) | 94.44 (72.7–99.9) |
| Mono vs. poli microbian | ||||||
| CN2D6AngScMom | 0.0129 | 0.757 (0.541–0.907) | 0.44 | >0.05 | 80 (44.4–97.5) | 64.29 (35.1–87.2) |
| Multirezistent vs. non multi | ||||||
| CN2D6Contrast | 0.0173 | 0.74 (0.528–0.893) | 0.5 | ≤0.098 | 100 (75.3–100) | 50 (21.1–78.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Puia, V.R.; Lupean, R.A.; Ștefan, P.A.; Fetti, A.C.; Vălean, D.; Zaharie, F.; Rusu, I.; Ciobanu, L.; Al-Hajjar, N. CT-Based Radiomic Analysis May Predict Bacteriological Features of Infected Intraperitoneal Fluid Collections after Gastric Cancer Surgery. Healthcare 2022, 10, 1280. https://doi.org/10.3390/healthcare10071280
Puia VR, Lupean RA, Ștefan PA, Fetti AC, Vălean D, Zaharie F, Rusu I, Ciobanu L, Al-Hajjar N. CT-Based Radiomic Analysis May Predict Bacteriological Features of Infected Intraperitoneal Fluid Collections after Gastric Cancer Surgery. Healthcare. 2022; 10(7):1280. https://doi.org/10.3390/healthcare10071280
Chicago/Turabian StylePuia, Vlad Radu, Roxana Adelina Lupean, Paul Andrei Ștefan, Alin Cornel Fetti, Dan Vălean, Florin Zaharie, Ioana Rusu, Lidia Ciobanu, and Nadim Al-Hajjar. 2022. "CT-Based Radiomic Analysis May Predict Bacteriological Features of Infected Intraperitoneal Fluid Collections after Gastric Cancer Surgery" Healthcare 10, no. 7: 1280. https://doi.org/10.3390/healthcare10071280







