Effects of Lighting Interventions to Improve Sleepiness in Night-Shift Workers: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Methods
2.2. Search Outcome
2.3. Quality Appraisal
2.4. Data Abstraction
2.5. Synthesis
3. Results
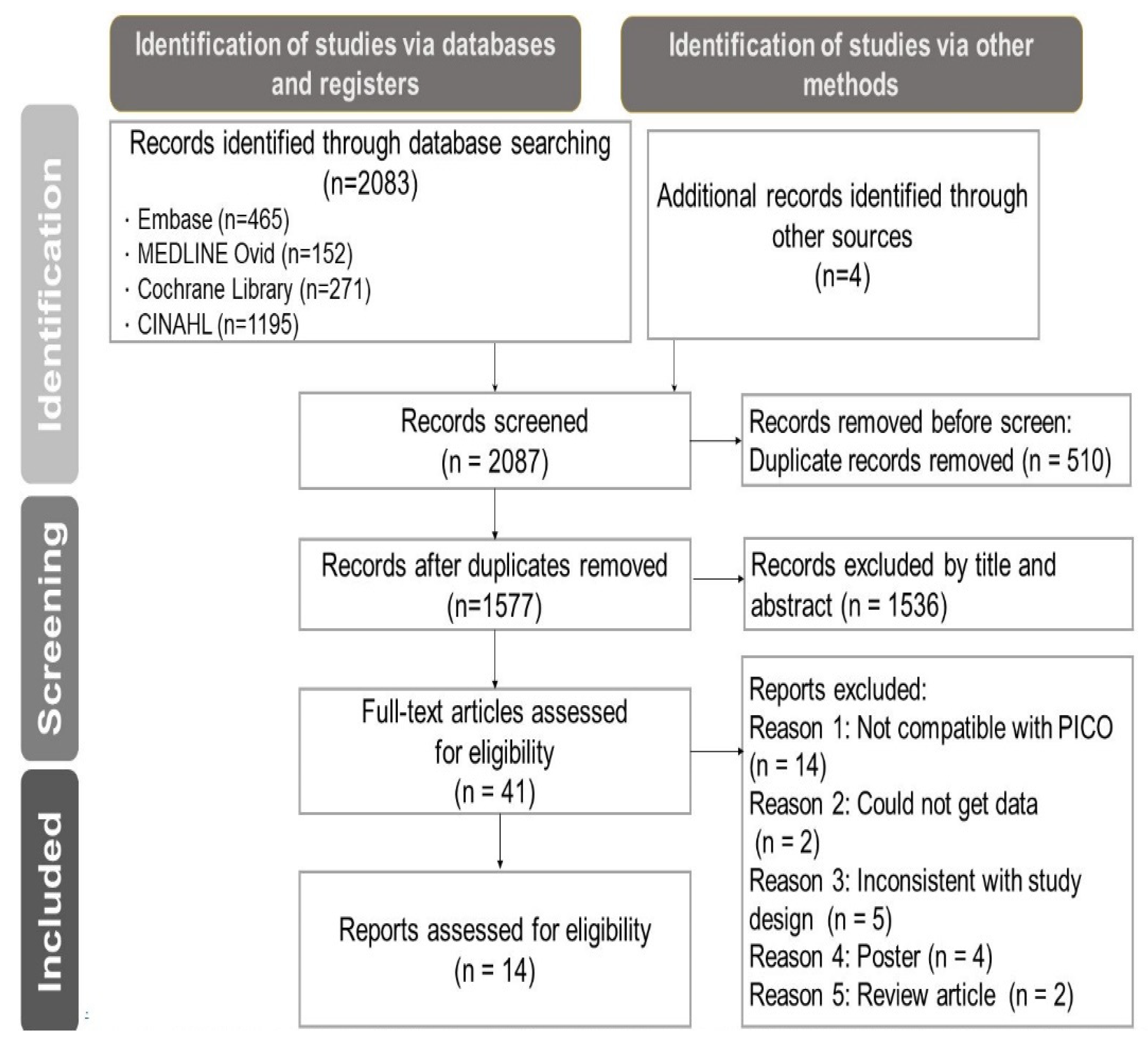
3.1. Selection of Studies
3.2. Description of the Included Studies
3.3. Risk of Bias and Sensitivity Analysis
3.4. Effects of Lighting Interventions in Improving Sleepiness
3.5. Subgroup Analyses
- Effects of lighting interventions on different groups in improving sleepiness
- Effects of color temperature in different spectral characteristics
4. Discussion
5. Limitations
6. Conclusions
7. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search Strategy | |
|---|---|---|
| Embase | 1. | (((“shift worker” OR “shift*work*” OR “in shift*” OR “Night Shift*” OR “irregular work*” OR “Rotating Shift Work” OR “a rotation system” OR “a relay system”) Near/4 (attendance OR work* OR laborer OR labourer OR job))):ti,ab,kw,de |
| 2. | “Shift worker”/exp | |
| 3. | (photograph* OR light* OR photoinduction* OR “photon radiation*” OR photoradiation*; OR optical* OR bright*):ti,ab,kw,de | |
| 4. | “light”/exp OR “photography”/exp | |
| 5. | (Sleepiness* OR drowsiness* OR somnolence* OR “Sleep disorder*” OR drows* OR “particularly in excess” OR vigilance* OR alertness OR “weather eye*” OR “look-out*” OR cognitive*):ti,ab,kw,de | |
| 6. | “Somnolence”/exp OR “Cognition”/exp | |
| 7. | (#1 OR #2) AND (#3 OR #4) AND (#5 OR #6) [embase]/lim | |
| MEDLINE (Ovid) | 1. | ((“shift worker” OR “shift*work*” OR “in shift*” OR “Night Shift*” OR “irregular work*” OR “Rotating Shift Work” OR “a rotation system” OR “a relay system”) Adj4 (attendance OR work* OR laborer OR labourer OR job)).mp |
| 2. | exp “Shift Work Schedule”/ | |
| 3. | (photograph* OR light* OR photoinduction* OR “photon radiation*” OR photoradiation* OR optical* OR bright*).mp | |
| 4. | exp “Light”/OR “light exposure”/OR “phototherapy”/ | |
| 5. | (Sleepiness* OR drowsiness* OR somnolence* OR Sleep disorder* OR drows* OR “particularly in excess” OR vigilance* OR alertness* OR “weather eye*” OR “look-out*” OR cognitive*).mp | |
| 6. | exp “Somnolence”/OR “Sleepiness”/OR “Cognition”/ | |
| 7. | (1 OR 2) AND (3 OR 4) AND (5 OR 6) | |
| CENTRAL | 1. | (((“shift worker” OR “shift*work*” OR “in shift*” OR “Night Shift*” OR “irregular work*” OR “Rotating Shift Work” OR “a rotation system” OR “a relay system”) Near/3 (attendance OR work* OR laborer OR labourer OR job))):ti,ab,kw |
| 2. | [mh “Shift Work Schedule”] | |
| 3. | (photograph* OR light* OR photoinduction* OR “photon radiation*” OR photoradiation* OR optical* OR bright*):ti,ab,kw | |
| 4. | [mh “Light”] OR [mh “phototherapy”] | |
| 5. | (Sleepiness* OR drowsiness* OR somnolence* OR “Sleep disorder*” OR drows* OR “particularly in excess” OR vigilance* OR alertness OR “weather eye*” OR “look-out*” OR cognitive*):ti,ab,kw | |
| 6. | [mh “Somnolence”] OR [mh “Sleepiness”] OR [mh “Cognition”] | |
| 7. | (#1 OR #2) AND (#3 OR #4 OR #5 OR #6) | |
| CINAHL | 1. | (((“shift worker” OR “shift*work*” OR “in shift*” OR “Night Shift*” OR “irregular work*” OR “Rotating Shift Work” OR “a rotation system” OR “a relay system”) N3 (attendance OR work* OR laborer OR labourer OR job))) |
| 2. | MH (“Shift Work Schedule+”) | |
| 3. | (photograph* OR light* OR photoinduction* OR “photon radiation*” OR photoradiation* OR optical* OR bright*) | |
| 4. | MH (“Light+”) OR MH(“Phototherapy+”) | |
| 5. | (Sleepiness* OR drowsiness* OR somnolence* OR Sleep disorder* OR drows* OR “particularly in excess” OR vigilance* OR alertness* OR “weather eye*” OR “look-out*” OR cognitive*) | |
| 6. | MH (“Somnolence+”) OR MH (“Sleepiness+”) OR MH (“Cognition+”) | |
| 7. | (S1 OR S2) AND (S3 OR S4 OR S5 OR S6) | |
| Google Scholar | 1. | ((shift worker OR night shift OR irregular work OR Rotating Shift Work OR a rotation system OR a relay system) AND (photograph OR light OR photoinduction OR photon radiation OR optical OR bright) AND (Sleepiness OR drowsiness OR somnolence OR vigilance OR alertness OR weather eye OR look-out OR cognitive)) |
References
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabilit. Nurs. 2014, 39, 1625. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMenamin, T.M. A time to work: Recent trends in shift work and flexible schedules. Mon. Lab. Rev. 2007, 130, 3–14. [Google Scholar]
- Ministry of Labor (2019, May). 108 Workers’ Living and Employment Situation Survey Report. Available online: https://statdb.mol.gov.tw/html/svy08/0823all.pdf (accessed on 5 March 2022).
- Wickwire, E.M.; Geiger-Brown, J.; Scharf, S.M.; Drake, C.L. Shift work and shift work sleep disorder: Clinical and organizational perspectives. Chest 2017, 151, 1156–1172. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Drake, C. Shift work disorder. Neurol. Clin. 2019, 37, 563–577. [Google Scholar] [CrossRef]
- Pandi-Perumal, S.R.; Srinivasan, V.; Maestroni, G.J.M.; Cardinali, D.P.; Poeggeler, B.; Hardeland, R. Melatonin: Nature’s most versatile biological signal? FEBS J. 2006, 273, 2813–2838. [Google Scholar] [CrossRef]
- Cipolla-Neto, J.; Amaral, F.G.D. Melatonin as a hormone: New physiological and clinical insights. Endocr. Rev. 2018, 39, 9901028. [Google Scholar] [CrossRef] [Green Version]
- Vanttola, P.; Puttonen, S.; Karhula, K.; Oksanen, T.; Harma, M. Prevalence of shift work disorder among hospital personnel: A cross sectional study using objective working hour data. J. Sleep Res. 2020, 29, e12906. [Google Scholar] [CrossRef] [PubMed]
- Selvi, K.S.; Jayabharathi, B.; Minisha, S.; Swratha, K.; Priya, M.V. Assessment of impact of shift work on health among staff nurses at SRM General Hospital, Kattankulathur. Int. J. Nurs. Educ. 2021, 13, 80–84. [Google Scholar] [CrossRef]
- Estryn-Béhar, M.; Van der Heijden, B.I.; NEXT Study Group. Effects of extended work shifts on employee fatigue, health, satisfaction, work/family balance, and patient safety. Work 2012, 41, 4283–4290. [Google Scholar] [CrossRef] [Green Version]
- Bjorvatn, B.; Pallesen, S.; Waage, S.; Thun, E.; Blytt, K.M. The effects of bright light treatment on subjective and objective sleepiness during three consecutive night shifts among hospital nurses A counter-balanced placebo-controlled crossover study. Scand. J. Work Environ. Health 2021, 47, 145–153. [Google Scholar] [CrossRef]
- Wahl, S.; Engelhardt, M.; Schaupp, P.; Lappe, C.; Ivanov, I.V. The inner clock-blue light sets the human rhythm. J. Biophotonics 2019, 12, e201900102. [Google Scholar] [CrossRef] [PubMed]
- Aarts, M.P.; Hartmeyer, S.L.; Morsink, K.; Kort, H.S.; de Kort, Y.A. Can special light glasses reduce sleepiness and improve sleep of nightshift workers? A placebo-controlled explorative field study. Clocks Sleep 2020, 2, 225–245. [Google Scholar] [CrossRef] [PubMed]
- Aemmi, S.Z.; Mohammadi, E.; Heidarian-Miri, H.; Fereidooni-Moghadam, M.; Boostani, H.; Zarea, K. The effectiveness of bright light exposure in shift-worker nurses: A systematic review and meta-analysis. Sleep Sci. 2020, 13, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Lam, C.; Chung, M.H. Dose–response effects of light therapy on sleepiness and circadian phase shift in shift workers: A meta-analysis and moderator analysis. Sci. Rep. 2021, 11, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Lowden, A.; Kecklund, G. Considerations on how to light the nightshift. Light. Res. Technol. 2021, 53, 437–452. [Google Scholar] [CrossRef]
- Souman, J.L.; Tinga, A.M.; Te Pas, S.F.; Van Ee, R.; Vlaskamp, B.N. Acute alerting effects of light: A systematic literature review. Behav. Brain Res. 2018, 337, 228–239. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- Amir-Behghadami, M.; Janati, A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg. Med. J. 2020, 37, 387. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane. 2022. Available online: www.training.cochrane.org/handbook (accessed on 2 April 2022).
- Cochrane Collaboration. Review Manager (RevMan) [Computer Program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. 2014. Available online: https://training.cochrane.org/online-learning/core-software/revman (accessed on 28 January 2022).
- Kakooei, H.; Zamanian Ardakani, Z.; Taghi Ayattollahi, M.; Karimian, M.; Nasl Saraji, G.; Akbar Owji, A. The effect of bright light on physiological circadian rhythms and subjective alertness of shift work nurses in Iran. Int. J. Occup. Saf. Ergon. 2010, 16, 477–485. [Google Scholar] [CrossRef]
- Hedges, L.V. Distribution theory for Glass’s estimator of effect size and related estimators. J. Educ. Stat. 1981, 6, 107–128. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef] [Green Version]
- Barger, L.K.; Sullivan, J.P.; Lockley, S.W.; Czeisler, C.A. Exposure to short wavelength-enriched white light and exercise improves alertness and performance in operational NASA flight controllers working overnight shifts. J. Occup. Environ. Med. 2020, 63, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Khammar, A.; Moghimian, M.; Ebrahimi, M.; Abbasi, M.; Baneshi, M.; Yari, A.; Hami, M.; Poursadeghiyan, M. Effects of bright light shock on sleepiness and adaptation among night workers of a hospital in Iran. Ann. Trop. Med. Public Health 2017, 10, 595–599. [Google Scholar] [CrossRef]
- Lowden, A.; Åkerstedt, T.; Wibom, R. Suppression of sleepiness and melatonin by bright light exposure during breaks in night work. J. Sleep Res. 2004, 13, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Sletten, T.L.; Ftouni, S.; Nicholas, C.L.; Magee, M.; Grunstein, R.R.; Ferguson, S.; Ferguson, S.; Kennaway, D.J.; O’Brien, D.; Lockley, S.W.; et al. Randomized controlled trial of the efficacy of a blue-enriched light intervention to improve alertness and performance in night shift workers. Occup. Environ. Med. 2017, 74, 792–801. [Google Scholar] [CrossRef]
- Sletten, T.L.; Raman, B.; Magee, M.; Ferguson, S.A.; Kennaway, D.J.; Grunstein, R.R.; Lockley, S.W.; Rajaratnam, S.M.W. A blue-enriched, increased intensity light intervention to improve alertness and performance in rotating night shift workers in an operational setting. Natl. Sci. Sleep 2021, 13, 647–657. [Google Scholar] [CrossRef]
- Sunde, E.; Mrdalj, J.; Pedersen, T.; Thun, E.; Bjorvatn, B.; Gronli, J.; Harris, A.; Waage, S.; Pallesen, S. Blue-enriched white light improves performance but not subjective alertness and circadian adaptation during three consecutive simulated night shifts. Front. Psychol. 2020, 11, 2172. [Google Scholar] [CrossRef]
- Song, Y.; Lv, X.; Qin, W.; Dang, W.; Chen, Z.; Nie, J.; Liu, B.; Dong, W. The effect of blue-enriched white light on cognitive performances and sleepiness of simulated shift workers: A randomized controlled trial. J. Occup. Environ. Med. 2021, 63, 752–759. [Google Scholar] [CrossRef]
- Griepentrog, J.E.; Labiner, H.E.; Gunn, S.R.; Rosengart, M.R. Bright environmental light improves the sleepiness of nightshift ICU nurses. Crit. Care 2018, 22, 295. [Google Scholar] [CrossRef] [Green Version]
- Sunde, E.; Pedersen, T.; Mrdalj, J.; Thun, E.; Gronli, J.; Harris, A.; Bjorvatn, B.; Waage, S.; Skene, J.D.; Pallesen, S. Role of nocturnal light intensity on adaptation to three consecutive night shifts: A counterbalanced crossover study. Occup. Environ. Med. 2020, 77, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Bjorvatn, B.; Pallesen, S. A practical approach to circadian rhythm sleep disorders. Sleep Med. Rev. 2009, 13, 47–60. [Google Scholar] [CrossRef]
- Comtet, H.; Geoffroy, P.A.; Kobayashi Frisk, M.; Hubbard, J.; Robin-Choteau, L.; Calvel, L.; Hugueny, L.; Viola, U.; Bourgin, P. Light therapy with boxes or glasses to counteract effects of acute sleep deprivation. Sci. Rep. 2019, 9, 18073. [Google Scholar] [CrossRef] [Green Version]
- Sadeghniiat-Haghighi, K.; Yazdi, Z.; Jahanihashemi, H.; Aminian, O. The effect of bright light on sleepiness among rapid-rotating 12-hour shift workers. Scand. J. Work Environ. Health 2011, 37, 77–79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenthal, R. The file drawer problem and tolerance for null results. Psychol. Bull. 1979, 86, 638. [Google Scholar] [CrossRef]
- Rodenbeck, A.; Wiater, A.; Neuwirth, M.; Özgüc, R. Effects of different light expositions on wakefulness, mood, and attention in shift workers: An ongoing field study in a morning and evening shift system. J. Sleep Res. 2018, 27. [Google Scholar] [CrossRef] [Green Version]
- Motamedzadeh, M.; Golmohammadi, R.; Kazemi, R.; Heidarimoghadam, R. The effect of blue-enriched white light on cognitive performances and sleepiness of night-shift workers: A field study. Physiol. Behav. 2017, 177, 208–214. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Smolensky, M.H.; Roth, T. Consequences of shift working on sleep duration, sleepiness, and sleep attacks. Chronobiol. Int. 2010, 27, 575–589. [Google Scholar] [CrossRef]
- Olson, J.A.; Artenie, D.Z.; Cyr, M.; Raz, A.; Lee, V. Developing a light-based intervention to reduce fatigue and improve sleep in rapidly rotating shift workers. Chronobiol. Int. 2020, 37, 573–591. [Google Scholar] [CrossRef]





| Author/ Year/Country | Study Design | Intervention Group (IG) | Control/Contrast Group (CG) | Population | Duration | Measurement Time Point | Outcomes and Measurement Tools |
|---|---|---|---|---|---|---|---|
| Lowden (2004) Sweden [28] | Crossover design | E: 2500 lux (5000 K) The workers were permitted two short breaks at night in the break room and light exposure time from nighttime 24:00–6:00 at any time the workers chose in the break room. In total, 67% of the workers chose between 3:00 and 4:00. Average exposure time length 20 ± 0.48 min. | 300 lux (3000 K) | Workers from a truck production plant 18 | 4 weeks | 24:00–6:00 q2h*2 check on every W1~W4 night | A significant interaction. Demonstrated a reduction in sleepiness in the BL condition, particularly on the first two nights at 4:00 and 6:00 h. KSS |
| Sadeghniiat-Haghighi (2011) Iran [37] | Crossover design | E: 2500 lux The light exposure occurred during two short breaks during the night shift. Each break was approximately 20 min long. The break time started at 24:30 and 2:30. | 300 lux | Workers from a ceramics factory 94 | 2 nights | 22:00, 24:00, 2:00, 4:00 check | Exposure to bright light might be effective in reducing the sleepiness of night workers. SSS |
| Sletten (2017) Australia [29] | RCT | E: 89 lux (17,000 K) Laboratory procedures for two consecutive night shifts at their usual occupation; workers remained in the laboratory from 17:30 to 8:30 for a simulated night shift. | 84 lux (4000 K) | Night-shift workers 71 | 2 nights | 23:00–7:00 q1h check | There were no differences between light conditions based on time into a shift, but blue-enriched light improved subjective sleepiness when light exposure coincided with the trough of the circadian rhythm. KSS |
| Comtet (2019) France [36] | Crossover design RCT | E: 2000 lux Health workers were given LED blue-enriched white light glasses at 5:00 for 30 min. | Dim light 8 lux | Health workers 18 | 3 nights | 5:00, 7:00, 8:00 check | Early morning light therapy under the condition of sleep loss may have broad practical applications to reduce sleepiness. KSS |
| Sunde, Pedersen (2020) Norway [34] | Crossover design | E: 900 lux (4000 K) The college students were given 3 nights of light exposure from 23:00 to 5:00. | 90 lux (4100 K) | College students simulating shift workers 27 | 3 nights | 23:30, 1:00, 2:30, 4:00,5:30 check | Bright light improved alertness. KSS |
| Barger (2020) USA [26] | RCT | E: 63 lux (8000 K) Subjects were given two 20 min breaks (11:00–3:30 and 3:30–8:00) and light exposure every night. | 63 lux (4100 K) | Flight controllers 12 | 5 nights | 11:00, 11:00–3:30, 3:30–8:00, 8:00 check | Short-wavelength light exposure was successful in improving alertness and performance. KSS |
| Sunde, Mrdalj (2020) Norway [31] | Crossover design RCT | E: 200 lux (7000 K) The college students were given exposure to polychromatic, blue-enriched white light from 23:00 to 5:00. | 200 lux (2500 K) | College students simulating shift workers 30 | 3 nights | 23:30, 1:00, 2:30, 4:00,5:30 check | 7000 K light was more beneficial compared to 2500 K for subjective alertness during night shifts. KSS |
| Song (2021) China [32] | RCT | E: 320 lux (6000 K) Subjects were exposed to blue light from 22:00–7:00. | 320 lux (3000 K) | College students simulating shift workers 48 | 1 night | 22:00–24:00, 2:00–4:00, 6:00–7:00 check | Exposure to blue-enriched white light could reduce sleepiness. KSS |
| Sletten (2021) Australia [30] | RCT | E: 106 lux (17,000 K) Laboratory procedures for two consecutive night shifts; workers remained at the laboratory from 17:30 h until 08:30 h for a simulated night shift at their usual occupation. | 43 lux (4000 K) | Night-shift workers 28 | 2 nights | 23:00–7:00 q1h check | Blue-enriched light improved subjective sleepiness when light exposure coincided with the trough of the circadian rhythm. KSS |
| Kakooei (2010) Iran [22] | Crossover design | E: 4500 lux (5000 K) Nurses were exposed to light intervention during two breaks (21:15–22:00 and 3:14–4:00). | 300 lux | Nurses from a hospital 34 | 3 nights | 19:00–16:00 q1h check | BL intervention improved alertness. KSS |
| Khammar (2017) Iran [27] | Crossover design RCT | E: 3500 lux (5000 K) The workers were exposed to full-spectrum light tubes at four breaks during the night shift (24:00, 2:00, 4:00, 6:00) in the break room. | Dim 400 lux | Hospital Workers 140 | 2 nights | 23:00–5:00 q2h check | Exposure to BL reduced shift workers’ sleepiness. KSS |
| Griepentrog (2018) USA [33] | Crossover design | E: 1500–2000 lux (3500–4100 K) Nurses were exposed to light intervention exposure from 19:00 to 5:00. | 300 lux | Nurses from a hospital 43 | 1 night | 5:00 check | BL intervention significantly reduced nurses’ sleepiness. SSS |
| Aarts (2020) The Netherlands [13] | Crossover design RCT | E: wear glasses FN (λ = 462 ± 10 nm, spectral irradiance of 22.36 µW/cm2/melanotic EDI of 114.38 lx at the cornea of the eyes) 4 × 15 min during nightshifts and for 30 min within 2 h after awakening. | LED 84 lux | Nurses from a hospital 23 | 3 nights | 24:00, 2:00, 4:00, 6:00, 8:00 q2h check | Wearing glasses as light intervention significantly reduced nurses’ sleepiness on the first night shift. KSS |
| Bjorvatn (2021) Norway [11] | Crossover design | E: BL 10,000 lux (4000 K) Nurses were exposed to light for 30 min at 2:00–3:00, 3:00–4:00, and 4:00–5:00. | Red dim light 100 lux | Nurses from a hospital 35 | 3 nights | 22:00–6:00 q2h check | No significant intervention effect was found for sleepiness. KSS |
| Subgroup | Effect Size | Heterogeneity | |||||
|---|---|---|---|---|---|---|---|
| Number of Studies | SMD | (95% CI) | p | χ2 | p | I2 (%) | |
| Characterization of group | |||||||
| Non-healthcare workers | 9 | −0.42 | −0.64, −0.21 | <0.0001 | 11.28 | =0.019 | 29 |
| Healthcare workers | 5 | −0.74 | −0.14, −0.07 | <0.03 | 40.16 | <0.00001 | 90 |
| Total between | 58.73 | <0.00001 | 78 | ||||
| Color temperature of light | |||||||
| ≥5000 K | 8 | −0.50 | −0.72, −0.28 | =0.0003 | 9.91 | =0.13 | 29 |
| <5000 K | 3 | −0.84 | −2.05, −0.38 | =0.18 | 33.91 | <0.00001 | 94 |
| Total between | 45.72 | <0.00001 | 78 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-J.; Huang, T.-Y.; Ou, S.-F.; Shiea, J.-T.; Lee, B.-O. Effects of Lighting Interventions to Improve Sleepiness in Night-Shift Workers: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 1390. https://doi.org/10.3390/healthcare10081390
Wu C-J, Huang T-Y, Ou S-F, Shiea J-T, Lee B-O. Effects of Lighting Interventions to Improve Sleepiness in Night-Shift Workers: A Systematic Review and Meta-Analysis. Healthcare. 2022; 10(8):1390. https://doi.org/10.3390/healthcare10081390
Chicago/Turabian StyleWu, Chi-Jen, Tai-Yang Huang, Su-Fei Ou, Jen-Taie Shiea, and Bih-O Lee. 2022. "Effects of Lighting Interventions to Improve Sleepiness in Night-Shift Workers: A Systematic Review and Meta-Analysis" Healthcare 10, no. 8: 1390. https://doi.org/10.3390/healthcare10081390
APA StyleWu, C.-J., Huang, T.-Y., Ou, S.-F., Shiea, J.-T., & Lee, B.-O. (2022). Effects of Lighting Interventions to Improve Sleepiness in Night-Shift Workers: A Systematic Review and Meta-Analysis. Healthcare, 10(8), 1390. https://doi.org/10.3390/healthcare10081390






