Novel Ultrasound-Guided Cervical Intervertebral Disc Injection of Platelet-Rich Plasma for Cervicodiscogenic Pain: A Case Report and Technical Note
Abstract
1. Introduction
2. Case Report
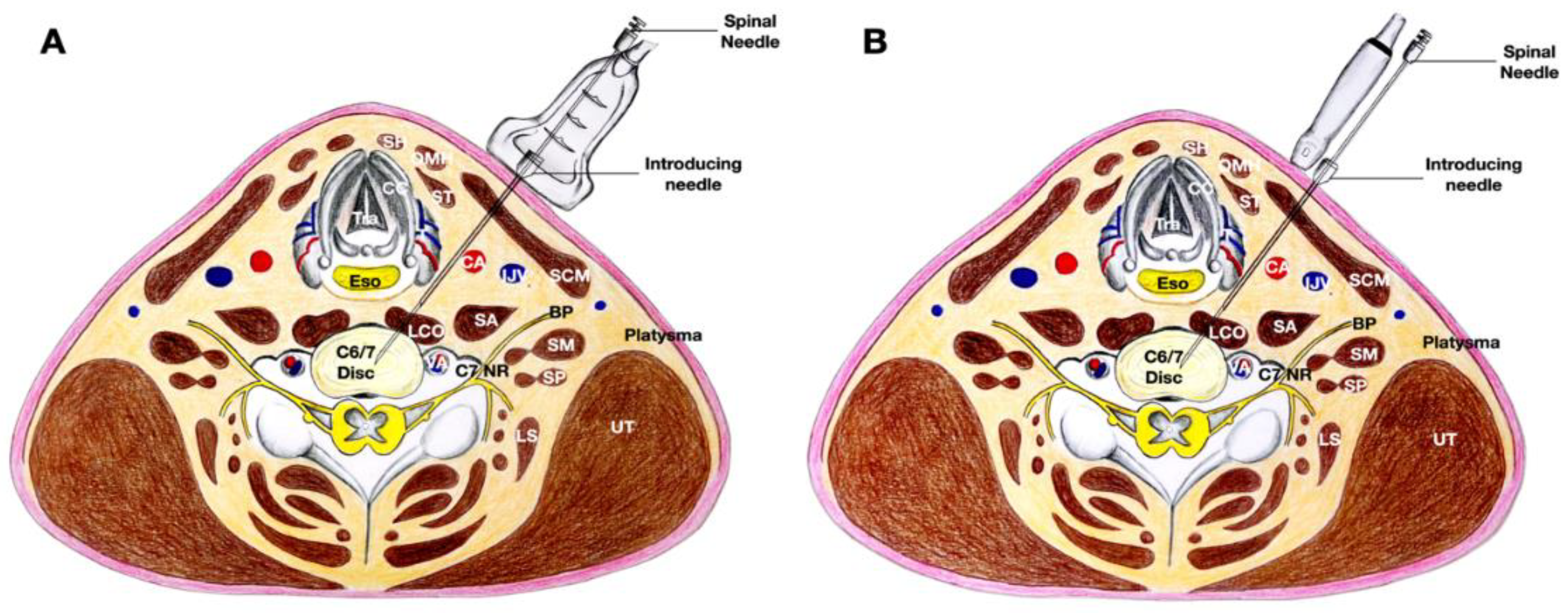
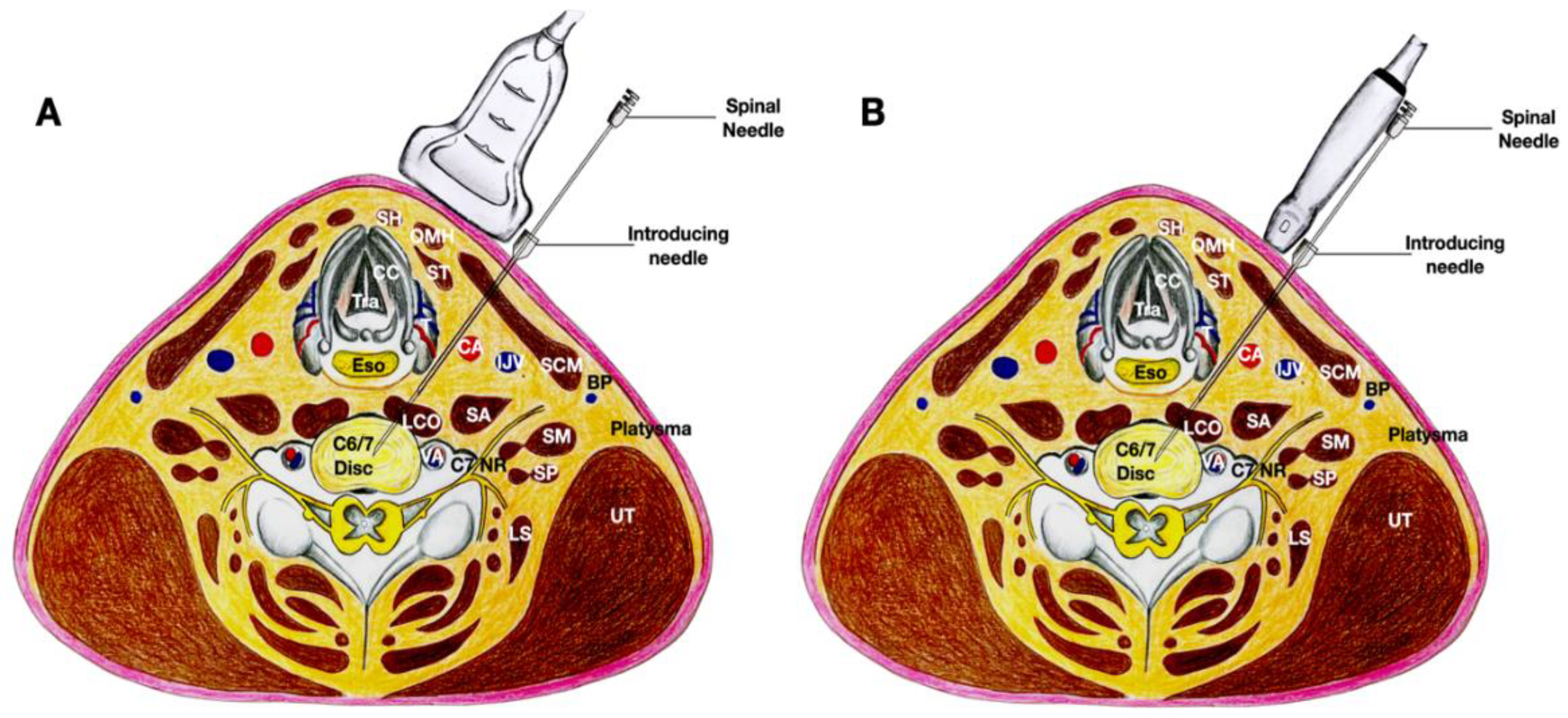
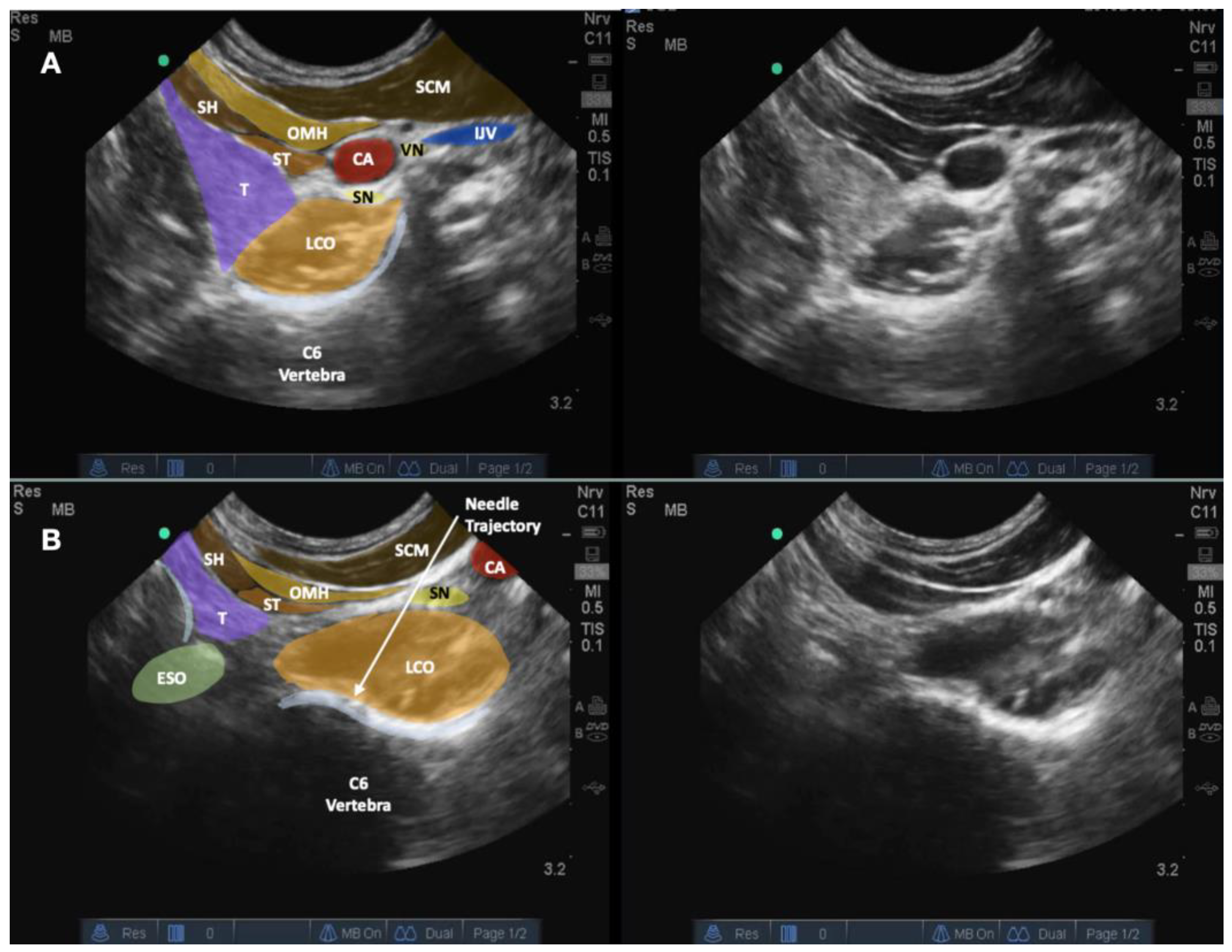
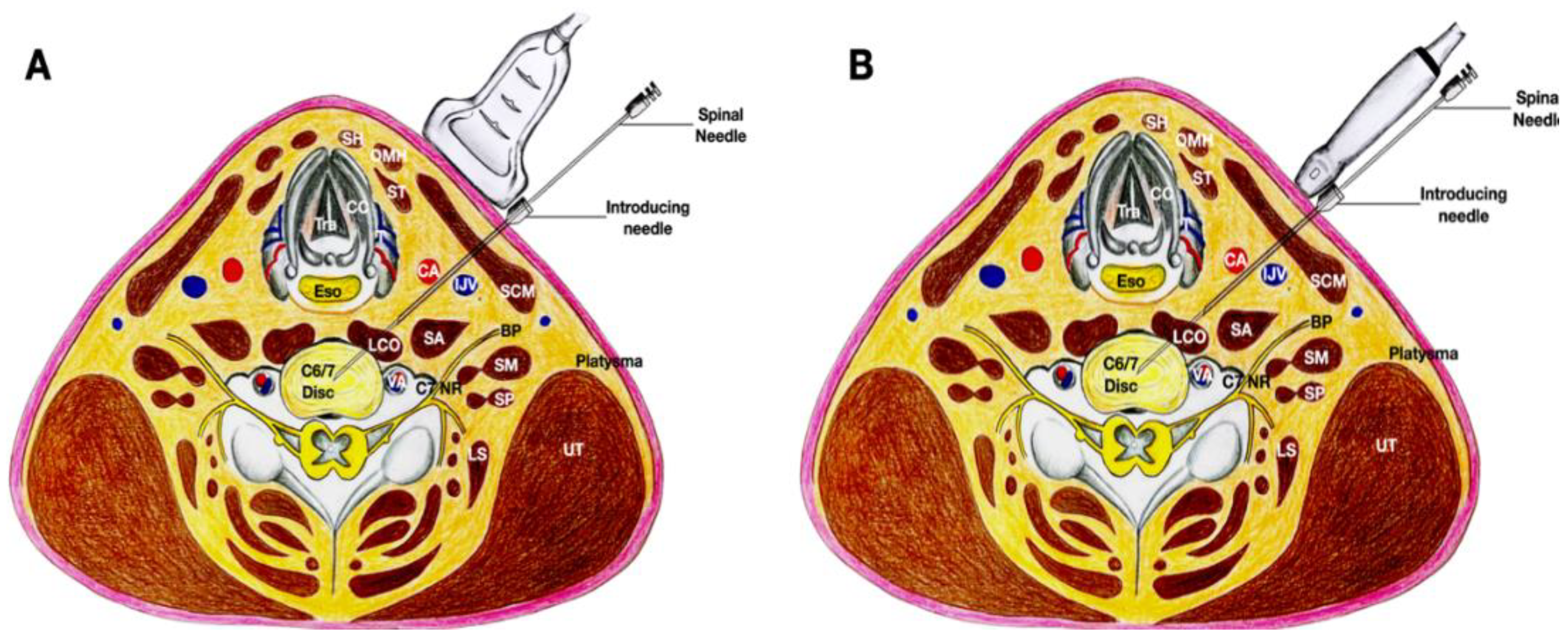
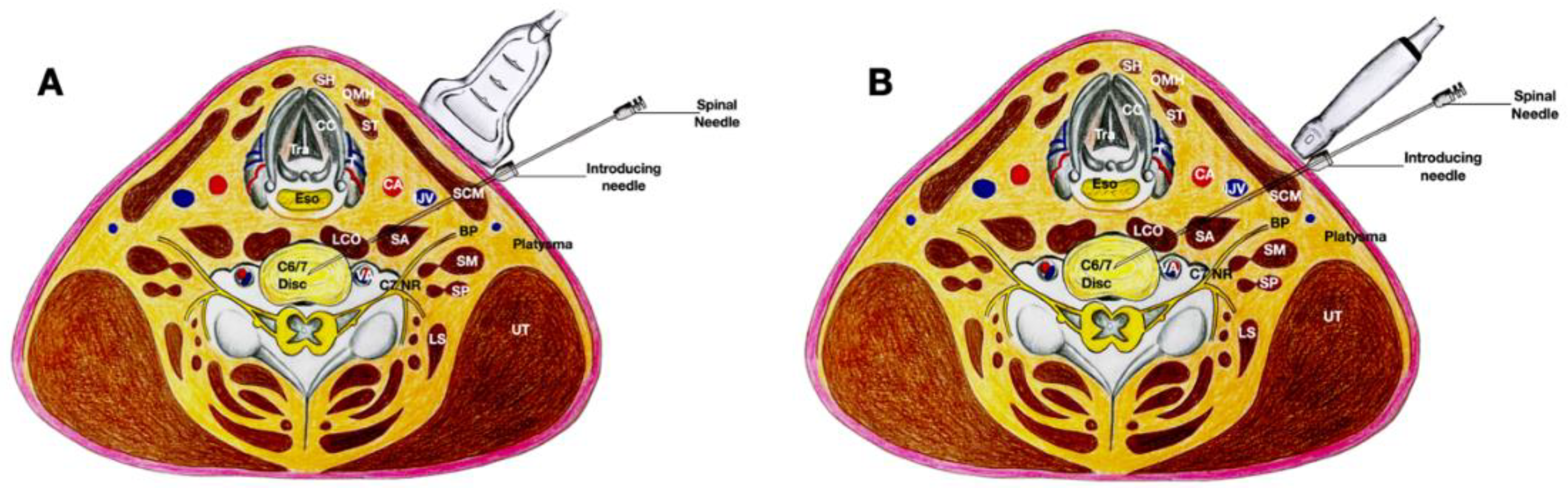
3. Technical Note
4. Results
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lam, K.H.S.; Hung, C.Y.; Wu, T.J. Ultrasound-Guided Cervical Intradiscal Injection with Platelet-Rich Plasma with Fluoroscopic Validation for the Treatment of Cervical Discogenic Pain: A Case Presentation and Technical Illustration. J. Pain Res. 2020, 13, 2125–2129. [Google Scholar] [CrossRef] [PubMed]
- Cloward, R.B. Cervical Discography. Acta Radiol. Diagn. 1963, 1, 675–688. [Google Scholar] [CrossRef] [PubMed]
- Cloward, R.B. Cervical diskography. A contribution to the etiology and mechanism of neck, shoulder and arm pain. Ann. Surg. 1959, 150, 1052–1064. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Ma, C.; Mai, M.; Li, G. Translation and validation study of Chinese versions of the neck disability index and the neck pain and disability scale. Spine 2010, 35, 1575–1579. [Google Scholar] [CrossRef] [PubMed]
- Maeda, M.; Maeda, N.; Masuda, K.; Nagano, T.; Tanaka, Y. Ultrasound-Guided Cervical Intervertebral Disc Injection without Fluoroscopy. J. Ultrasound Med. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Lam, S.K.H.; Reeves, K.D.; Cheng, A.L. Transition from deep regional blocks toward deep nerve hydrodissection in the upper body and torso: Method description and results from a retrospective chart review of the analgesic effect of 5% dextrose water as the primary hydrodissection injectate to enhance safety. Biomed. Res. Int. 2017, 2017, 7920438. [Google Scholar] [PubMed]
- Cameron, J.A.; Thielen, K.M. Autologous Platelet Rich Plasma for Neck and Lower Back Pain Secondary to Spinal Disc Herniation: Midterm Results. Arch. Med. 2017, 3, 10. [Google Scholar] [CrossRef][Green Version]
- Cheng, J.; Santiago, K.A.; Nguyen, J.T.; Solomon, J.L.; Lutz, G.E. Treatment of symptomatic degenerative intervertebral discs with autologous platelet-rich plasma: Follow-up at 5–9 years. Regen. Med. 2019, 14, 831–840. [Google Scholar] [CrossRef]
- Sharma, S.K.; Jones, J.O.; Zeballos, P.P.; Irwin, S.A.; Martin, T.W. The prevention of discitis during discography. Spine J. 2009, 9, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Guyer, R.D.; Ohnmeiss, D.D.; Vaccaro, A. Lumbar discography. Spine J. 2003, 3 (Suppl. S3), 11S–27S. [Google Scholar] [CrossRef]
- Lam, K.H.S.; Hung, C.Y.; Chiang, Y.P.; Onishi, K.; Su, D.C.J.; Clark, T.B.; Reeves, K.D. Ultrasound-Guided Nerve Hydrodissection for Pain Management: Rationale, Methods, Current Literature, and Theoretical Mechanisms. J. Pain Res. 2020, 13, 1957–1968. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lam, K.H.S.; Hung, C.-Y.; Wu, T.-J.; Chen, W.-H.; Ng, T.K.T.; Lin, J.-A.; Wu, Y.-T.; Lai, W.W. Novel Ultrasound-Guided Cervical Intervertebral Disc Injection of Platelet-Rich Plasma for Cervicodiscogenic Pain: A Case Report and Technical Note. Healthcare 2022, 10, 1427. https://doi.org/10.3390/healthcare10081427
Lam KHS, Hung C-Y, Wu T-J, Chen W-H, Ng TKT, Lin J-A, Wu Y-T, Lai WW. Novel Ultrasound-Guided Cervical Intervertebral Disc Injection of Platelet-Rich Plasma for Cervicodiscogenic Pain: A Case Report and Technical Note. Healthcare. 2022; 10(8):1427. https://doi.org/10.3390/healthcare10081427
Chicago/Turabian StyleLam, King Hei Stanley, Chen-Yu Hung, Tsung-Ju Wu, Wei-Hung Chen, Tony Kwun Tung Ng, Jui-An Lin, Yung-Tsan Wu, and Wai Wah Lai. 2022. "Novel Ultrasound-Guided Cervical Intervertebral Disc Injection of Platelet-Rich Plasma for Cervicodiscogenic Pain: A Case Report and Technical Note" Healthcare 10, no. 8: 1427. https://doi.org/10.3390/healthcare10081427
APA StyleLam, K. H. S., Hung, C.-Y., Wu, T.-J., Chen, W.-H., Ng, T. K. T., Lin, J.-A., Wu, Y.-T., & Lai, W. W. (2022). Novel Ultrasound-Guided Cervical Intervertebral Disc Injection of Platelet-Rich Plasma for Cervicodiscogenic Pain: A Case Report and Technical Note. Healthcare, 10(8), 1427. https://doi.org/10.3390/healthcare10081427






