Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Evidence Synthesis
3. Results
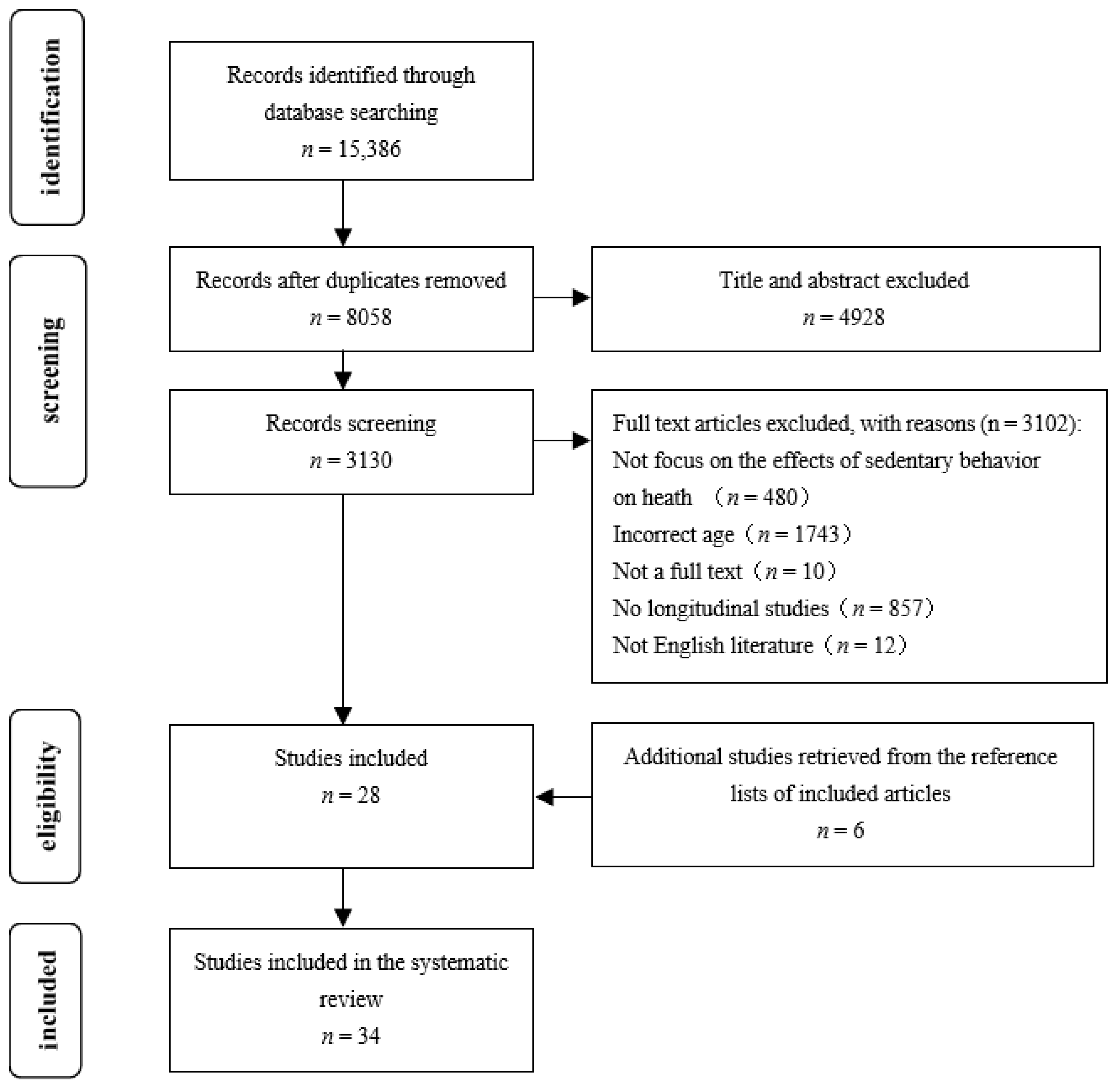
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.3. Methodological Quality
3.4. Summary of Results
3.4.1. Sedentary Behavior: Adiposity Indicators
3.4.2. Sedentary Behavior: Physical Fitness
3.4.3. Sedentary Behavior: Metabolic Syndrome/Cardiovascular Disease Risk Factors
3.4.4. Sedentary Behavior: Cognitive Function
3.4.5. Sedentary Behavior: Emotional Disorder
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pate, R.R.; O’Neill, J.R.; Lobelo, F. The evolving definition of “sedentary”. Exerc. Sport Sci. Rev. 2008, 36, 173–178. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; ISBN 978-92-4-001512-8. [Google Scholar]
- Owen, N.; Healy, G.N.; Dempsey, P.C.; Salmon, J.; Timperio, A.; Clark, B.K.; Goode, A.D.; Koorts, H.; Ridgers, N.D.; Hadgraft, N.T.; et al. Sedentary behavior and public health: Integrating the evidence and identifying potential solutions. Annu. Rev. Public Health 2020, 41, 265–287. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.; Liu, B.; Sun, Y.; Snetselaar, L.G.; Wallace, R.B.; Bao, W. Trends in adherence to the physical activity guidelines for americans for aerobic activity and time spent on sedentary behavior among US adults, 2007 to 2016. JAMA Netw. Open 2019, 2, e197597. [Google Scholar] [CrossRef]
- Bluearth Move More, Sit Less. 2019. Available online: https://www.movemoresitless.org.au/ (accessed on 5 July 2022).
- Loyen, A.; Clarke-Cornwell, A.M.; Anderssen, S.A.; Hagströmer, M.; Sardinha, L.B.; Sundquist, K.; Ekelund, U.; Steene-Johannessen, J.; Baptista, F.; Hansen, B.H.; et al. Sedentary time and physical activity surveillance through accelerometer pooling in four european countries. Sports Med. 2017, 47, 1421–1435. [Google Scholar] [CrossRef]
- Must, A.; Tybor, D.J. Physical activity and sedentary behavior: A review of longitudinal studies of weight and adiposity in youth. Int. J. Obes. 2005, 29, S84–S96. [Google Scholar] [CrossRef] [PubMed]
- Mansoubi, M.; Pearson, N.; Biddle, S.J.H.; Clemes, S. The relationship between sedentary behaviour and physical activity in adults: A systematic review. Prev. Med. 2014, 69, 28–35. [Google Scholar] [CrossRef]
- Vaara, J.P.; Vasankari, T.; Wyss, T.; Pihlainen, K.; Ojanen, T.; Raitanen, J.; Vähä-Ypyä, H.; Kyröläinen, H. Device-based measures of sedentary time and physical activity are associated with physical fitness and body fat content. Front. Sports Act. Living 2020, 2, 587789. [Google Scholar] [CrossRef]
- Hoang, T.D.; Reis, J.; Zhu, N.; Jacobs, D.R.; Launer, L.J.; Whitmer, R.A.; Sidney, S.; Yaffe, K. Effect of early adult patterns of physical activity and television viewing on midlife cognitive function. JAMA Psychiatry 2016, 73, 73–79. [Google Scholar] [CrossRef]
- Thomée, S.; Härenstam, A.; Hagberg, M. Computer use and stress, sleep disturbances, and symptoms of depression among young adults–a prospective cohort study. BMC Psychiatry 2012, 12, 176. [Google Scholar] [CrossRef]
- Staiano, A.E.; Martin, C.K.; Champagne, C.M.; Rood, J.C.; Katzmarzyk, P.T. Sedentary time, physical activity, and adiposity in a longitudinal cohort of nonobese young adults. Am. J. Clin. Nutr. 2018, 108, 946–952. [Google Scholar] [CrossRef]
- Carter, S.E.; Draijer, R.; Thompson, A.; Thijssen, D.H.J.; Hopkins, N.D. Relationship between sedentary behavior and physical activity at work and cognition and mood. J. Phys. Act. Health 2020, 17, 1140–1152. [Google Scholar] [CrossRef]
- Proper, K.I.; Singh, A.S.; van Mechelen, W.; Chinapaw, M.J.M. Sedentary behaviors and health outcomes among adults. Am. J. Prev. Med. 2011, 40, 174–182. [Google Scholar] [CrossRef]
- Thorp, A.A.; Owen, N.; Neuhaus, M.; Dunstan, D.W. Sedentary behaviors and subsequent health outcomes in adults. Am. J. Prev. Med. 2011, 41, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Freed, G.L.; Davis, M.M.; Singer, D.; Prosser, L.A. Valuing health at different ages: Evidence from a nationally representative survey in the US. Appl. Health Econ. Health Policy 2011, 9, 149–156. [Google Scholar] [CrossRef]
- Zoer, I.; Ruitenburg, M.M.; Botje, D.; Frings-Dresen, M.H.W.; Sluiter, J.K. The associations between psychosocial workload and mental health complaints in different age groups. Ergonomics 2011, 54, 943–952. [Google Scholar] [CrossRef] [PubMed]
- Settersten, R.A., Jr.; Ottusch, T.M.; Schneider, B. Becoming adult: Meanings of markers to adulthood. In Emerging Trends in the Social and Behavioral Sciences; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015; pp. 1–16. ISBN 978-1-118-90077-2. [Google Scholar]
- Lysberg, F.; Innstrand, S.T.; Cvancarova Småstuen, M.; Lysberg, C.; Høie, M.M.; Espnes, G.A. Age groups changes in self-rated health: A prospective longitudinal study over a 20-year period using health survey of north trøndelag data. Scand. J. Public Health 2021, 49, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, R.D.; Weinberger, A.H.; Kim, J.H.; Wu, M.; Galea, S. Trends in anxiety among adults in the united states, 2008–2018: Rapid increases among young adults. J. Psychiatr. Res. 2020, 130, 441–446. [Google Scholar] [CrossRef]
- Coggon, D.; Rose, G.; Barker, D.J.P. Epidemiology for the Uninitiated, 5th ed.; BMJ Publishing Group: London, UK, 2003; ISBN 0-7279-1604-1. [Google Scholar]
- Belur, J.; Tompson, L.; Thornton, A.; Simon, M. Interrater Reliability in Systematic Review Methodology: Exploring Variation in Coder Decision-Making. Sociol. Methods Res. 2021, 50, 837–865. [Google Scholar] [CrossRef]
- Tooth, L. Quality of reporting of observational longitudinal research. Am. J. Epidemiol. 2005, 161, 280–288. [Google Scholar] [CrossRef]
- Hayden, J.A.; Côté, P.; Bombardier, C. Evaluation of the quality of prognosis studies in systematic reviews. Ann. Intern. Med. 2006, 144, 427. [Google Scholar] [CrossRef]
- Singh, A.S.; Mulder, C.; Twisk, J.W.R.; Van Mechelen, W.; Chinapaw, M.J.M. Tracking of childhood overweight into adulthood: A systematic review of the literature. Obes. Rev. 2008, 9, 474–488. [Google Scholar] [CrossRef]
- van Ekris, E.; Altenburg, T.M.; Singh, A.S.; Proper, K.I.; Heymans, M.W.; Chinapaw, M.J.M. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 833–849. [Google Scholar] [CrossRef]
- Teychenne, M.; Stephens, L.D.; Costigan, S.A.; Olstad, D.L.; Stubbs, B.; Turner, A.I. The association between sedentary behaviour and indicators of stress: A systematic review. BMC Public Health 2019, 19, 1357. [Google Scholar] [CrossRef]
- Ki, M.; Pouliou, T.; Li, L.; Power, C. Physical (in) activity over 20 y in adulthood: Associations with adult lipid levels in the 1958 british birth cohort. Atherosclerosis 2011, 219, 361–367. [Google Scholar] [CrossRef] [PubMed]
- van de Laar, R.J.; Stehouwer, C.D.; Prins, M.H.; van Mechelen, W.; Twisk, J.W.; Ferreira, I. Self-reported time spent watching television is associated with arterial stiffness in young adults: The amsterdam growth and health longitudinal study. Br. J. Sports Med. 2014, 48, 256–264. [Google Scholar] [CrossRef]
- Lyden, K.; Keadle, S.K.; Staudenmayer, J.; Braun, B.; Freedson, P.S. Discrete features of sedentary behavior impact cardiometabolic risk factors. Med. Sci. Sports Exerc. 2015, 47, 1079–1086. [Google Scholar] [CrossRef]
- Pouliou, T.; Ki, M.; Law, C.; Li, L.; Power, C. Physical activity and sedentary behaviour at different life stages and adult blood pressure in the 1958 british cohort. J. Hypertens. 2012, 30, 275–283. [Google Scholar] [CrossRef]
- Altenburg, T.M.; Rotteveel, J.; Serné, E.H.; Chinapaw, M.J. Effects of multiple sedentary days on metabolic risk factors in free-living conditions: Lessons learned and future recommendations. Front. Physiol. 2016, 7, 616. [Google Scholar] [CrossRef] [PubMed]
- Drenowatz, C.; DeMello, M.M.; Shook, R.P.; Hand, G.A.; Burgess, S.; Blair, S.N. The association between sedentary behaviors during weekdays and weekend with change in body composition in young adults. AIMS Public Health 2016, 3, 375–388. [Google Scholar] [CrossRef] [PubMed]
- DeMello, M.M.; Pinto, B.M.; Dunsiger, S.I.; Shook, R.P.; Burgess, S.; Hand, G.A.; Blair, S.N. Reciprocal relationship between sedentary behavior and mood in young adults over one-year duration. Ment. Health Phys. Act. 2018, 14, 157–162. [Google Scholar] [CrossRef]
- Cleland, V.J.; Patterson, K.; Breslin, M.; Schmidt, M.D.; Dwyer, T.; Venn, A.J. Longitudinal associations between TV viewing and BMI not explained by the “mindless eating” or “physical activity displacement” hypotheses among adults. BMC Public Health 2018, 18, 797. [Google Scholar] [CrossRef]
- Whitaker, K.M.; Pettee Gabriel, K.; Buman, M.P.; Pereira, M.A.; Jacobs, D.R.; Reis, J.P.; Gibbs, B.B.; Carnethon, M.R.; Staudenmayer, J.; Sidney, S.; et al. Associations of accelerometer-measured sedentary time and physical activity with prospectively assessed cardiometabolic risk factors: The CARDIA study. J. Am. Heart Assoc. 2019, 8, e010212. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.G.C.d.; Silva, I.C.M.d.; Ekelund, U.; Brage, S.; Ong, K.K.; De Lucia Rolfe, E.; Lima, N.P.; Silva, S.G.d.; França, G.V.A.d.; Horta, B.L. Associations of physical activity and sedentary time with body composition in brazilian young adults. Sci. Rep. 2019, 9, 5444. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Hamer, M.; Mishra, G.D. Early adulthood television viewing and cardiometabolic risk profiles in early middle age: Results from a population, prospective cohort study. Diabetologia 2012, 55, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Pavey, T.G.; Brown, W.J. Sitting time and depression in young women over 12-years: The effect of physical activity. J. Sci. Med. Sport 2019, 22, 1125–1131. [Google Scholar] [CrossRef]
- Ellingson, L.D.; Meyer, J.D.; Shook, R.P.; Dixon, P.M.; Hand, G.A.; Wirth, M.D.; Paluch, A.E.; Burgess, S.; Hebert, J.R.; Blair, S.N. Changes in sedentary time are associated with changes in mental wellbeing over 1 year in young adults. Prev. Med. Rep. 2018, 11, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Uddin, R.; Burton, N.W.; Khan, A. Combined effects of physical inactivity and sedentary behaviour on psychological distress among university-based young adults: A one-year prospective study. Psychiatr. Q. 2020, 91, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Fujii, Y.; Yamamoto, R.; Shinzawa, M.; Kimura, Y.; Aoki, K.; Tomi, R.; Ozaki, S.; Yoshimura, R.; Taneike, M.; Nakanishi, K.; et al. Occupational sedentary behavior and prediction of proteinuria in young to middle-aged adults: A retrospective cohort study. J. Nephrol. 2021, 34, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Vieira, N.F.L.; Bueno, N.B.; Silva, S.M.; Lins, I.L.; Albuquerque, F.C.; Macêna, M.L.; Silva-Júnior, A.E.; Pureza, I.M.; Clemente, A.G.; Florêncio, T.T. Sitting/lying time is associated with waist-to-hip increase but not with body weight increase or blood cardiovascular risk factors changes in adult women living in social vulnerability: A 2-year longitudinal study. Am. J. Hum. Biol. 2020, 32, e23372. [Google Scholar] [CrossRef] [PubMed]
- Mars, B.; Gunnell, D.; Biddle, L.; Kidger, J.; Moran, P.; Winstone, L.; Heron, J. Prospective associations between internet use and poor mental health: A population-based study. PLoS ONE 2020, 15, e0235889. [Google Scholar] [CrossRef] [PubMed]
- Thomée, S.; Eklöf, M.; Gustafsson, E.; Nilsson, R.; Hagberg, M. Prevalence of perceived stress, symptoms of depression and sleep disturbances in relation to information and communication technology (ICT) use among young adults–an explorative prospective study. Comput. Hum. Behav. 2007, 23, 1300–1321. [Google Scholar] [CrossRef]
- Endrighi, R.; Steptoe, A.; Hamer, M. The effect of experimentally induced sedentariness on mood and psychobiological responses to mental stress. Br. J. Psychiatry 2016, 208, 245–251. [Google Scholar] [CrossRef]
- Jeffery, R.W.; French, S.A. Epidemic obesity in the united states: Are fast foods and television viewing contributing? Am. J. Public Health 1998, 88, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Brown, W. Who does not gain weight? prevalence and predictors of weight maintenance in young women. Int. J. Obes. Relat. Metab. Disord. 2003, 26, 1570–1578. [Google Scholar] [CrossRef]
- Hancox, R.J.; Milne, B.J.; Poulton, R. Association between child and adolescent television viewing and adult health: A longitudinal birth cohort study. Lancet 2004, 364, 257–262. [Google Scholar] [CrossRef]
- Viner, R.M.; Cole, T.J. Television viewing in early childhood predicts adult body mass index. J. Pediatr. 2005, 147, 429–435. [Google Scholar] [CrossRef]
- Boone, J.E.; Gordon-Larsen, P.; Adair, L.S.; Popkin, B.M. Screen time and physical activity during adolescence: Longitudinal effects on obesity in young adulthood. Int. J. Behav. Nutr. Phys. Act. 2007, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Beunza, J.J.; Martínez-González, M.A.; Ebrahim, S.; Bes-Rastrollo, M.; Núñez, J.; Martínez, J.A.; Alonso, A. Sedentary behaviors and the risk of incident hypertension: The SUN cohort. Am. J. Hypertens. 2007, 20, 1156–1162. [Google Scholar] [CrossRef]
- Landhuis, C.E.; Poulton, R.; Welch, D.; Hancox, R.J. Programming obesity and poor fitness: The long-term impact of childhood television. Obesity 2008, 16, 1457–1459. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.J.; Manor, O.; Power, C. Television viewing and obesity: A prospective study in the 1958 british birth cohort. Eur. J. Clin. Nutr. 2008, 62, 1355–1363. [Google Scholar] [CrossRef] [PubMed]
- Crawford, D.; Jeffery, R.; French, S. Television viewing, physical inactivity and obesity. Int. J. Obes. 1999, 23, 437–440. [Google Scholar] [CrossRef]
- Primack, B.A.; Shensa, A.; Sidani, J.E.; Escobar-Viera, C.G.; Fine, M.J. Temporal associations between social media use and depression. Am. J. Prev. Med. 2021, 60, 179–188. [Google Scholar] [CrossRef]
- Hung, S.-P.; Chen, C.-Y.; Guo, F.-R.; Chang, C.-I.; Jan, C.-F. Combine body mass index and body fat percentage measures to improve the accuracy of obesity screening in young adults. Obes. Res. Clin. Pract. 2017, 11, 11–18. [Google Scholar] [CrossRef]
- Adedia, D.; Boakye, A.; Mensah, D.; Lokpo, S.; Afeke, I.; Duedu, K. Comparative assessment of methods for determining adiposity and a model for obesity index. bioRxiv 2019, 6, 710970. [Google Scholar] [CrossRef]
- Whitaker, K.M.; Pereira, M.A.; Jacobs, D.R.; Sidney, S.; Odegaard, A.O. Sedentary behavior, physical activity, and abdominal adipose tissue deposition. Med. Sci. Sports Exerc. 2017, 49, 450–458. [Google Scholar] [CrossRef]
- Carter, S.; Hartman, Y.; Holder, S.; Thijssen, D.H.; Hopkins, N.D. Sedentary behavior and cardiovascular disease risk: Mediating mechanisms. Exerc. Sport. Sci. Rev. 2017, 45, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Vella, C.A.; Taylor, K.; Nelson, M.C. Associations of leisure screen time with cardiometabolic biomarkers in college-aged adults. J. Behav Med. 2020, 43, 1014–1025. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, B.B.; Naquin, M.R.; Sirikul, B.; Kraemer, R.R. Five Weeks of Aquatic-Calisthenic High Intensity Interval Training Improves Cardiorespiratory Fitness and Body Composition in Sedentary Young Adults. J. Sports Sci. Med. 2020, 19, 187–194. [Google Scholar] [PubMed]
- Lepp, A.; Barkley, J.E.; Sanders, G.J.; Rebold, M.; Gates, P. The relationship between cell phone use, physical and sedentary activity, and cardiorespiratory fitness in a sample of U.S. college students. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 79. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Tian, X.Y.; Sun, F.H.; Huang, W.Y.; Sheridan, S.; Wu, Y.; Wong, S.H.-S. Associations of sedentary patterns with cardiometabolic biomarkers in physically active young males. Med. Sci. Sports Exerc. 2021, 53, 838–844. [Google Scholar] [CrossRef]
- Dumuid, D.; Pedišić, Ž.; Stanford, T.E.; Martín-Fernández, J.-A.; Hron, K.; Maher, C.A.; Lewis, L.K.; Olds, T. The compositional isotemporal substitution model: A method for estimating changes in a health outcome for reallocation of time between sleep, physical activity and sedentary behaviour. Stat. Methods Med. Res. 2019, 28, 846–857. [Google Scholar] [CrossRef] [PubMed]
- Hartanto, A.; Yong, J.C.; Toh, W.X.; Lee, S.T.H.; Tng, G.Y.Q.; Tov, W. Cognitive, social, emotional, and subjective health benefits of computer use in adults: A 9-year longitudinal study from the Midlife in the United States (MIDUS). Comput. Hum. Behav. 2020, 104, 106179. [Google Scholar] [CrossRef]
- Tun, P.A.; Lachman, M.E. The association between computer use and cognition across adulthood: Use it so you won’t lose it? Psychol. Aging 2010, 25, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Fancourt, D.; Steptoe, A. Television viewing and cognitive decline in older age: Findings from the english longitudinal study of ageing. Sci. Rep. 2019, 9, 2851. [Google Scholar] [CrossRef]
- Hallgren, M.; Owen, N.; Stubbs, B.; Zeebari, Z.; Vancampfort, D.; Schuch, F.; Bellocco, R.; Dunstan, D.; Trolle Lagerros, Y. Passive and mentally-active sedentary behaviors and incident major depressive disorder: A 13-year cohort study. J. Affect. Disord. 2018, 241, 579–585. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, A.G.; Spence, J.C.; Carson, V.; Connor Gorber, S.; Dillman, C.; Janssen, I.; Kho, M.E.; Stearns, J.A.; Timmons, B.W.; Tremblay, M.S. Systematic review of sedentary behaviour and health indicators in the early years (aged 0-4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 753–772. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S.; et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
| Study (Year) | Country | Sample | Follow-Up Duration | Type of Sedentary Behavior (and Measure) | Type of Health Outcome (and Measure) | Variables Controlled in Analysis | Statistical Analysis | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Ki et al., 2011 [28] | United Kingdom | n = 7824, aged 23 years, male 50.2%, female 49.8% | 22 years | TV viewing (EPAQ-2) | HDL-cholesterol, and triglycerides (non-fasting venous blood samples) | Smoking, alcohol drink, diet, sedentary behavior, activity, BMI, long-term limiting illness, birth weight | Linear regression | TV viewing and HDL cholesterol: β = −0.02, p < 0.001 TV viewing and triglycerides: β = 0.026, p < 0.01 |
| Thomée et al., 2012 [11] | Sweden | n = 4163, aged 20–24 years, male 35%, female 65% | 1 year | Computer use (self-report questionnaires) | Stress and symptoms of depression (Prime-MD) | Status, educational level, occupation | Cox regression | Computer use and stress: PR = 1.7 (95%CI, 1.23, 2.25) Computer use and symptoms of depression: PR = 1.9 (95%CI, 1.17, 3.03) |
| Van de Laar et al., 2014 [29] | The Nether lands | n = 373, aged 32 years, male 47.5%, female 52.5% | 4 years | Television time (self-report questionnaires) | Cardiovascular risk factors (ultrasound scanner) | Gender, body height, alcohol consumption and smoking behavior, daily energy intake, physical activity | Generalized estimating equations | Television time and cardiovascular risk factors: triglycerides: β = 0.078 (0.008, 0.148), p < 0.05 Total-to-HDL cholesterol ratio: β = 0.066 (0.007, 0.125), p < 0.05 mean arterial pressure: β = 0.078 (0.007, 0.148), p < 0.05 |
| Lyden et al., 2015 [30] | USA | n = 10, mean age 25.2 ± 5.7 years, male 40%, female 60% | 7 days | Sitting (accelerometers) | Markers of cardiometabolic risk (oral glucose tolerance test) | MVPA | Linear regression | Sitting and plasma insulin: β = 0.91, p < 0.01 Sitting and glucose: β = 0.39, p = 0.16 |
| Pouliou et al., 2012 [31] | United Kingdom | n = 9927, aged 23 years, male 46.7%, female 53.3% | 22 years | TV viewing (EPAQ) | Blood pressure (digital oscillometer sphygmomanometer) | Birth-weight, smoking, alcohol, diet, social class, and pre-existing medical condition | Logistic regression | TV viewing and blood pressure in men: OR = 1.06 (1.00, 1.12) TV viewing and blood pressure in women: OR = 1.01 (0.94, 1.09) |
| Altenburg et al., 2016 [32] | The Nether lands | n = 7, aged 18–23 years, male | 6 days | Sitting time (accelerometers) | Glucose, C-peptide, and triglycerides (blood sample) | LPA time | Generalized estimating equations | Sitting time and metabolic risk factors [β (90%CI)]: C-peptide: 0.11(0.002, 0.22), p < 0.01 glucose and triglycerides were not significantly different |
| Drenowatz et al., 2016 [33] | USA | n = 332, mean age 23.7 ± 3.7 years, male 50%, female 50% | 1 year | Sedentary time (accelerometers) | BMI (kg/m2) Body fat percentage (fat mass/body weight) | Age, baseline sedentary time, baseline body composition, MVPA | Linear regression | Sedentary time and BMI [β]: −0.074, p > 0.05 Sedentary time and body fat percentage [β]: 0.062, p < 0.05 |
| Hoang et al., 2016 [10] | USA | n = 3247, mean age 25.1 ± 3.6 years, male 43.5%, female 56.5% | 25 years | Television viewing (asked) | Cognitive function (DSST, Stroop test, RAVLT) | Age, race, sex, educational level, smoking, BMI, and hypertension | Logistic regression | Television viewing and cognitive function DSST: OR = 1.64 (1.21, 2.33) Stroop: OR = 1.56 (1.13, 2.14) RAVLT: OR = 1.14 (0.86, 1.53) |
| DeMello et al., 2018 [34] | USA | n = 430, mean age 27.66 ± 3.78 years, male 49.5%, female 50.5% | 1 year | Sedentary behavior (accelerometers) | Mood (profile of mood state) | Perceived stress, age, BMI and gender, employment, PA, and total stressful life events | Cross-lagged, autoregressive clustered model | Sedentary behavior and worse mood: β = 0.20, p = 0.01 |
| Cleland et al., 2018 [35] | Australia | n = 1068, mean age 31.5 years, male 35.95%, female 64.05% | 5 years | TV viewing (Self-report questionnaires) | BMI (kg/m2) | Gender, age, highest level of education, marital status, employment status, occupation, number of children, and current smoking | Linear regression | TV viewing and BMI [β (95%CI)]: >1 h increase (hours/week): 0.41 (0.03, 0.78) |
| Staiano et al., 2018 [12] | United Kingdom | n = 71, mean age 26.9 ± 4.5 years, male 44%, female 56% | 2 years | Sedentary time (accelerometers) | Adiposity (whole-body DXA) | Age, gender, energy intake | Linear regression | Sedentary behavior was not significantly associated with any adiposity indicators (p > 0.05) |
| Whitaker et al., 2019 [36] | USA | n = 1922, aged 18–30 years, male 41.6%, female 58.4% | 10 years | Sedentary time (accelerometers) | Cardiometabolic risk factors (fasting venous blood samples) | Sex, race, age, education, employment status, health insurance, self-reported medication uses for blood pressure, cholesterol, or diabetes mellitus, smoking status, alcohol consumption, BMI | Linear correlations | Sedentary time and Cardiometabolic risk factors [R]: 0.070, p < 0.05 |
| Silva et al., 2019 [37] | Brazil | n = 3206, mean age 30.2 years, male 49.6%, female 50.4% | 13 years | Sedentary time (IPAQ-L) | Waist circumference (Bod POD Scale) | Sex, family income at birth, maternal schooling at birth, maternal skin color, birth weight, socioeconomic status, achieved schooling, smoking and daily energy intake | Linear regression | Sedentary time and waist circumference: [β (95%CI)]: 1.05 (0.16, 0.012) p < 0.001 |
| Stamatakis et al., 2012 [38] | United Kingdom | n = 5972, aged 23 years, male 49.3%, female 50.7% | 11 years | TV viewing (interview) | cardiometabolic risk factor (non-fasting blood samples) | Sex, smoking, alcohol, CVD medication social class, MVPA and TV viewing times | Linear regression | TV viewing and cardiometabolic risk: β = 0.048 (−0.012, 0.107), p = 0.071 |
| Pavey et al., 2019 [39] | Australia | n = 6205, mean age 24.6 ± 1.5 years, female | 12 years | Sitting time (asked) | Depression (CESD-10) | Area of residence, education, marital status, number of children, smoking status, alcohol status, BMI, chronic conditions | Generalized estimating equation | Sitting time and depression [OR (95%CI)]: Sitting time ≥10 h/day: 1.41 (1.12–1.77) |
| Ellingson et al., 2018 [40] | USA | n = 271 mean age 27.8 ± 3.7 years, male 51%, female 49% | 1 year | Total time spent ≤1.5 METs while awake (Accelerometers) | Mood (profile of mood states) Stress (Perceived Stress Scale) | Age, sex, race, education | Linear regression | Sedentary behavior and total mood disorder: β = 0.23, p = 0.001 Sedentary behavior and stress: β = 0.20, p = 0.006 |
| Carter et al., 2020 [13] | USA | n = 75, mean age 33.6 ± 10.4 years male 44%, female 56% | 1 year | Sedentary behavior (accelerometers) | Mood (PNANS, Bond–Lader); Cognitive (Stroop, ANT, N-Back Tasks) | Age, sex | Linear regression | Sedentary behavior was not significantly associated with cognitive function and mood (p > 0.05) |
| Uddin et al., 2020 [41] | Australia | n = 395, mean age 20.7 ± 1.35 years, male 55%, female 45% | 1 year | Sedentary behavior (GPAQ) | Psychological distress (Kessler Psychological Distress) | Age, gender, marital status, BMI, education, occupation, income, television (TV) in bedroom, perceived health, sleep difficulties, smoking, diet | Generalized Estimating Equations | Sedentary behavior was not significantly associated with psychological distress (p = 0.638) |
| Fujii et al., 2020 [42] | Japan | n = 10,212, mean age 34 years, male 48.8%, female 51.2% | 4.8 years | Sedentary behavior (asked) | Proteinuria (dipstick test) | Age, sex, smoking status, sleep duration, BMI, systolic blood pressure, sedentary workers, television viewing, exercise, cardiovascular diseases | Cox regression | Sedentary behavior and proteinuria: HR = 1.35, (1.11–1.63) |
| Vaara et al., 2020 [9] | Finland | n = 415, mean age 26 ± 7 years, male | 7 days | ≤1.5 METs (accelerometers) | Body fat content (bioelectrical impedance method) Physical fitness (indirect graded cycle ergometer test and muscular fitness tests) | Age and smoking | Linear regression | Sedentary behavior and cardiorespiratory fitness and muscular fitness: β = −0.245 (−0.338; −0.152), β = −0.193 (−0.287; −0.099) Sedentary behavior and body fat content: β = 0.42, p < 0.001) |
| Vieira et al., 2020 [43] | Brazil | n = 34, mean age 31.85 years, female | 2 years | Sitting/lying time (accelerometers) | Body weight (electronic scale) WHR (waist/hip) blood cardiovascular (fasting blood sample) | Age, schooling, number of children, marital status, tobacco status, alcohol user, unemployment, per capita income | Multivariable mixed models | Sitting/lying time was associated with an increase in WHR, but not in body weight or blood cardiovascular risk factors. |
| Mars et al., 2020 [44] | United Kingdom | n = 1431, mean age 18.2 ± 0.5 years, male 62.6%, female 37.4% | 3 years | Internet use (asked) | Depression (sMFQ) Anxiety (GAD-7) | Earlier mental health problems | Logistic regression | Internet use and anxiety: OR = 1.00 (0.99, 1.02), p = 0.310 |
| Thomée et al., 2007 [45] | Sweden | n = 1127, aged 18–25, male 51.9% female 48.1% | 1 year | Computer/ Internet use (self-report questionnaires) | Stress, depression, anxiety (Prime-MD) | Age, sex, social position | Crude prevalence ratios | Overall computer or internet use and stress (95%CI): 1.02 (0.60,1.75); Depression: 1.02 (0.60,1.75); anxiety: 0.62 (0.36, 1.05); |
| Endrighi et al., 2016 [46] | United Kingdom | n = 43, aged 18–35 years, male 55.8%, female 44.2% | 4 weeks | Sedentary time (accelerometers) | Psychological distress (GHQ-28) Mood (POMS-SF) | MVPA | Linear regression | No significant associations emerged between GHQ scores and changes in sedentary time (β = 0.08, p = 0.62) Sedentary time was significantly associated with the POMS negative mood score (β = 0.32, p = 0.03) |
| Jeffery et al., 1998 [47] | USA | n = 1059, mean aged 34 years, male 18.7%, female, 81.3% | 1 year | Television viewing (self-report questionnaires) | BMI (kg/m2) | Age, education, baseline smoking, baseline body mass index, energy intake, physical activity. | Linear regression | Significant positive relationship between hours of TV viewing and change in body mass index in high-income women (β = 0.30; 0.02, 0.58) |
| Ball et al., 2003 [48] | Australia | n = 8726, aged 18–23, women | 4 years | Sitting time (self-report questionnaires) | Body weight (BMI) | Occupation, student status, marital status, parity and new mothers | ANOVA | Compared with the ‘low sitting’ group, the women who reported moderate or high sitting time were less likely to be in the weight maintainers. |
| Hancox et al., 2004 [49] | New Zealand | n = 980, birth cohort. boy 48%, girl 52% | 26 years | Television viewing (self-report questionnaires) | Cardiometabolic risk (fasting blood samples) | Sex, bodyweight, physical activity | Linear regression | TV viewing time is a significant predictor of elevated cholesterol (mmol/L) at age 26 years: β (SE) = 0.09 (0.04) p = 0.0383 No significant association with blood pressure |
| Viner et al., 2005 [50] | United Kingdom | n = 8158, birth cohort, male, 48.7%, female 51.3% | 5, 10, and 30 years | Television viewing (self-report questionnaires) | BMI (Self-report) | Gender, birth weight, social class, educational status | Linear regression | β (95% CI) on weekends = 0.04 (0.03, 0.06), p < 0.001; β (95% CI) on weekdays = 0.03 (0.01, 0.05), p = 0.001 |
| Boone et al., 2016 [51] | USA | n = 9605, mean aged 21.4 years, male 50.8%, female 49.2% | 6 years | Screen time (self-report questionnaires) | Obesity (BMI) | Age, race/ethnicity, household income, and highest parental education | Logistic regression | Screen time hours had a stronger influence on incident obesity in females [OR (95% CI): OR 4 vs. 40 h = 0.58 (0.43, 0.80)] than males [OR (95% CI): OR 4 vs. 40 h = 0.78 (0.61, 0.99)] |
| Beunza et al., 2007 [52] | Spain | n = 6742, Mean age 33.3 years, male 38.2%, female 61.8% | Mean 40 months | TV viewing, computer use, driving, sleeping (self-report questionnaires) | Hypertension (Follow-up questionnaires) | Age, gender, BMI, physical activity, family history of hypertension, hypercholesterolemia, smoking status, intake of sodium alcohol, low-fat dairy, fruit, vegetable, and olive oil | Cox regression | HR (95% CI) for incident hypertension and total sedentary behavior <14.2 h/day = 1.00 (ref) >21 h/day = 1.48 (1.01, 2.18) |
| Landhuis et al., 2008 [53] | New Zealand | n = 1037, Born April 1972–March 1973, male 51.6%, female 48.4% | 27 years | Television viewing (asked) | Fitness (cycle ergometer) obesity (BMI ≥ 30 kg/m2) | Childhood socioeconomic status, early BMI, and parental BMI | Logistic regression | Childhood viewing predicted both adult obesity (OR 95%CI = 1.30; 1.07, 1.58) and adult poor fitness (OR 95%CI = 1.41; 1.17, 1.69). |
| Parsons et al., 2008 [54] | United Kingdom | n = 11,301, birth cohort, male 50.7%, female 49.3% | 16, 23, and 33 years | Television viewing (self-report questionnaires) | BMI and central adiposity (Calculated and indexed by waist and hip circumferences) | Maternal BMI, social class, puberty status, physical activity, alcohol consumption, smoking status, healthy eating score | Linear regression | TV viewing at 23 years was significantly associated with waist–hip ratio at age 45 years: ≥5 times a week = 0.006 (men), 0.004 (women) |
| Crawford et al., 1999 [55] | Australia | n = 881, mean aged 34.3 years, male 20%, female 80% | 3 years | Television viewing (self-report questionnaires) | BMI (kg/m2) | Dietary, age, education, smoking, baseline BMI | Linear regression | There were no significant relationships between change in BMI and TV viewing |
| Primack et al., 2021 [56] | USA | n = 990, mean age 27.0 ± 2.7 years, male 45.9%, female 55.1% | 6 months | Social media use (asked) | Depression (Questionnaire) | Age, sex, race and ethnicity, educational level, household income, relationship status, living situation, and adverse childhood experiences | Logistic regression | Social media use and depression: OR = 1.04 (0.78, 1.38) |
| Reference | Source Population | Recruitment | Participation Rate | Description Baseline Sample | Numbers at Follow-Up | Follow-up Duration | Response rate at Follow-Up | Not-Selective non-Response | Measure SB | SB Measured before Health Outcome | Measure Health Outcome | Appropriate Statistical Model | Cases at Least 10 Times | Point Estimates and Measures of Variability | No Selective Reporting of Results | Total | Percentage ‘+’ |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carter et al., 2020 [13] | + | ? | + | + | + | + | + | − | + | + | − | + | − | + | + | 11 | 73 |
| Whitaker et al., 2019 [36] | + | + | – | + | + | + | − | − | + | + | ? | + | + | + | + | 11 | 73 |
| Ki et al., 2011 [28] | + | ? | + | + | ? | + | + | − | − | + | + | + | + | + | − | 10 | 67 |
| Stamatakis et al., 2012 [38] | + | ? | + | + | ? | + | − | + | − | + | + | + | + | + | − | 10 | 67 |
| Drenowatz et al., 2016 [33] | + | ? | – | + | + | + | − | + | + | + | ? | + | + | + | − | 10 | 67 |
| Uddin et al., 2020 [41] | + | ? | + | + | + | + | − | + | − | + | − | + | + | + | − | 10 | 67 |
| Beunza et al., 2007 [52] | + | + | – | + | − | + | + | − | − | + | − | + | + | + | + | 10 | 67 |
| Silva et al., 2019 [37] | + | ? | + | ? | + | + | − | − | − | + | − | + | + | + | + | 9 | 60 |
| Pouliou et al., 2012 [31] | + | ? | + | + | ? | + | − | − | − | + | + | + | + | + | − | 9 | 60 |
| Cleland et al., 2018 [35] | + | ? | – | + | + | + | − | + | − | + | − | + | − | + | + | 9 | 60 |
| Vaara et al., 2020 [9] | + | ? | + | + | ? | + | − | − | + | + | ? | + | + | + | − | 9 | 60 |
| Ellingson et al., 2018 [40] | + | ? | – | + | − | + | − | − | + | + | − | + | + | + | + | 9 | 60 |
| Altenburg et al., 2016 [32] | + | ? | – | + | + | + | − | − | + | + | ? | + | − | + | + | 9 | 60 |
| Fujii et al., 2021 [42] | – | ? | – | + | ? | + | + | − | − | + | ? | + | + | + | + | 8 | 53 |
| Mars et al., 2020 [44] | + | ? | + | ? | + | + | − | − | − | + | − | + | + | + | − | 8 | 53 |
| Hoang et al., 2016 [10] | + | ? | – | + | − | + | − | + | − | − | + | + | + | + | − | 8 | 53 |
| Thomée et al., 2012 [45] | + | + | – | ? | + | + | − | − | − | + | − | + | + | + | − | 8 | 53 |
| DeMello et al., 2018 [34] | + | ? | – | + | + | + | − | − | + | − | − | + | + | + | − | 8 | 53 |
| Pavey et al., 2019 [39] | + | ? | – | + | − | + | − | − | − | + | − | + | + | − | + | 7 | 47 |
| Primack et al., 2021 [56] | – | ? | + | + | ? | + | − | − | − | + | − | + | + | + | − | 7 | 47 |
| Staiano et al., 2018 [12] | – | ? | – | + | − | + | − | − | + | + | − | + | − | + | + | 7 | 47 |
| Van de Laar et al., 2014 [29] | + | ? | – | + | ? | + | − | − | − | + | − | + | + | + | − | 7 | 47 |
| Lyden et al., 2015 [30] | – | – | – | ? | − | + | + | − | + | + | ? | + | − | + | + | 7 | 47 |
| Hancox et al., 2004 [49] | + | ? | + | − | + | + | + | ? | − | − | ? | + | − | + | − | 7 | 47 |
| Endrighi et al., 2016 [46] | + | - | – | ? | − | + | − | − | + | + | − | + | ? | + | − | 6 | 40 |
| Parsons et al., 2008 [54] | + | - | + | ? | ? | + | ? | − | − | + | − | + | − | + | − | 6 | 40 |
| Landhuis et al., 2008 [53] | + | - | + | − | − | + | + | − | − | − | − | + | − | + | − | 6 | 40 |
| Thomée et al., 2007 [45] | + | ? | – | − | + | + | − | − | − | + | − | + | − | + | − | 6 | 40 |
| Vieira et al., 2020 [43] | – | ? | – | + | + | + | − | + | + | − | ? | + | − | − | − | 6 | 40 |
| Boone et al., 2016 [51] | - | – | – | + | − | + | + | − | − | + | − | + | − | + | − | 6 | 40 |
| Ball et al., 2003 [48] | + | ? | – | + | − | + | − | − | − | + | − | − | − | + | − | 5 | 33 |
| Viner et al., 2005 [50] | + | ? | – | ? | + | + | − | − | − | − | − | + | − | + | − | 5 | 33 |
| Jeffery et al., 1998 [47] | – | ? | – | + | − | + | − | − | − | − | − | + | − | + | − | 4 | 27 |
| Crawford et al., 1999 [55] | – | ? | – | ? | − | + | − | − | − | − | − | + | − | + | − | 3 | 20 |
| Health Indicator | Association | Studies (Primary Author, Publication Year) | Association (%) | Evidence |
|---|---|---|---|---|
| Adiposity indicators | + | Vaara et al., 2020 [9] a; Jeffery et al., 1998 [47] b; Viner et al., 2005 [50] b; Parsons et al., 2008 [54] b; Ball et al., 2003 [48] b; Boone et al., 2016 [51] b; Landhuis et al., 2008 [53] b | 7/12 58.3% | Insufficient |
| 0 | Silva et al., 2019 [37] a; Drenowatz et al., 2016 [33] a; Cleland et al., 2018 [35] a; Staiano et al., 2018 [12] b; Crawford et al., 1999 [55] b | 5/12 41.7% | ||
| Physical fitness | − | Vaara et al., 2020 [9] a; Landhuis et al., 2008 [53] b | 2/2 100% | Moderate |
| Metabolic syndrome/ cardiovascular disease risk factors | + | Whitaker et al., 2019 [36] a; Fujii et al., 2021 [42] a; van de Laar et al., 2014 [29] b; Ki et al., 2011 [28] a; Hancox et al., 2004 [49] b | 5/11 45.4% | Insufficient |
| 0 | Pouliou et al., 2012 [31] a; Beunza et al., 2007 [52] a; Altenburg et al., 2016 [32] a; Stamatakis et al., 2012 [38] a; Lyden et al., 2015 [30] b; Vieira et al., 2020 [43] b | 6/11 54.6% | ||
| Cognitive function | − | Hoang et al., 2016 [10] a | 1/2 50% | Insufficient |
| 0 | Carter et al., 2020 [13] a | 1/2 50% | ||
| Emotional disorder | + | Ellingson et al., 2018 [40] a; DeMello et al., 2018 [34] a; Pavey et al., 2019 [39] b; Primack et al., 2021 [56] b | 4/10 40% | Insufficient |
| 0 | Carter et al., 2020 [13] a; Uddin et al., 2020 [41] a; Mars et al., 2020 [44] a; Thomée et al., 2012 [11] a; Endrighi et al., 2016 [46] b, Thomée et al., 2007 [45] b | 6/10 60% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Liu, Y.; Zhou, Y. Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies. Healthcare 2022, 10, 1480. https://doi.org/10.3390/healthcare10081480
Huang Z, Liu Y, Zhou Y. Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies. Healthcare. 2022; 10(8):1480. https://doi.org/10.3390/healthcare10081480
Chicago/Turabian StyleHuang, Zan, Yanjie Liu, and Yulan Zhou. 2022. "Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies" Healthcare 10, no. 8: 1480. https://doi.org/10.3390/healthcare10081480
APA StyleHuang, Z., Liu, Y., & Zhou, Y. (2022). Sedentary Behaviors and Health Outcomes among Young Adults: A Systematic Review of Longitudinal Studies. Healthcare, 10(8), 1480. https://doi.org/10.3390/healthcare10081480





