Characteristics of Biomechanical and Physical Function According to Symptomatic and Asymptomatic Acetabular Impingement Syndrome in Young Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Participants
2.3. Subjective Hip Score
2.4. Range of Motion
2.5. Y-Balance Test
2.6. Isokinetic Hip Strength
2.7. Data Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Subjective Hip Score
3.3. Range of Motion
3.4. Dynamic Balance
3.5. Isokinetic Hip Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ng, K.G.; Jeffers, J.R.; Beaulé, P.E. Hip joint capsular anatomy, mechanics, and surgical management. J. Bone Jt. Surg. Am. 2019, 101, 2141–2151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jamari, J.; Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Prakoso, A.T.; Basri, H.; van der Heide, E. Computational Contact Pressure Prediction of CoCrMo, SS 316L and Ti6Al4V Femoral Head against UHMWPE Acetabular Cup under Gait Cycle. J. Funct. Biomater. 2022, 13, 64. [Google Scholar] [CrossRef] [PubMed]
- Schmaranzer, F.; Kheterpal, A.B.; Bredella, M.A. Best practices: Hip femoroacetabular impingement. AJR Am. J. Roentgenol. 2021, 216, 585–598. [Google Scholar] [CrossRef] [PubMed]
- Trigg, S.D.; Schroeder, J.D.; Hulsopple, C. Femoroacetabular impingement syndrome. Curr. Sports Med. Rep. 2020, 19, 360–366. [Google Scholar] [CrossRef]
- Heimer, C.Y.; Wu, C.H.; Perka, C.; Hardt, S.; Göhler, F.; Winkler, T.; Bäcker, H.C. The Impact of Hip Dysplasia on CAM Impingement. J. Pers. Med. 2022, 12, 1129. [Google Scholar] [CrossRef]
- Hale, R.F.; Melugin, H.P.; Zhou, J.; LaPrade, M.D.; Bernard, C.; Leland, D.; Levy, B.A.; Krych, A.J. Incidence of femoroacetabular impingement and surgical management trends over time. Am. J. Sports Med. 2021, 49, 35–41. [Google Scholar] [CrossRef]
- Han, J.; Won, S.-H.; Kim, J.-T.; Hahn, M.-H.; Won, Y.-Y. Prevalence of cam deformity with associated femoroacetabular impingement syndrome in hip joint computed tomography of asymptomatic adults. Hip Pelvis 2018, 30, 5–11. [Google Scholar] [CrossRef] [Green Version]
- Morales-Avalos, R.; Tapia-Náñez, A.; Simental-Mendía, M.; Elizondo-Riojas, G.; Morcos-Sandino, M.; Tey-Pons, M.; Peña-Martínez, V.M.; Barrera, F.J.; Guzman-Lopez, S.; Elizondo-Omaña, R.E. Prevalence of Morphological Variations Associated With Femoroacetabular Impingement According to Age and Sex: A Study of 1878 Asymptomatic Hips in Nonprofessional Athletes. Orthop. J. Sports Med. 2021, 9, 2325967120977892–2325967120977905. [Google Scholar] [CrossRef]
- Melugin, H.P.; Hale, R.F.; Zhou, J.; LaPrade, M.; Bernard, C.; Leland, D.; Levy, B.A.; Krych, A.J. Risk factors for long-term hip osteoarthritis in patients with femoroacetabular impingement without surgical intervention. Am. J. Sports Med. 2020, 48, 2881–2886. [Google Scholar] [CrossRef]
- Li, A.E.; Jawetz, S.T.; Greditzer, H.G.; Burge, A.J.; Nawabi, D.H.; Potter, H.G. MRI for the preoperative evaluation of femoroacetabular impingement. Insights Imaging 2016, 7, 187–198. [Google Scholar] [CrossRef] [Green Version]
- Sogbein, O.A.; Shah, A.; Kay, J.; Memon, M.; Simunovic, N.; Belzile, E.L.; Ayeni, O.R. Predictors of outcomes after hip arthroscopic surgery for femoroacetabular impingement: A systematic review. Orthop. J. Sports Med. 2019, 7, 2325967119848982–2325967119849000. [Google Scholar] [CrossRef]
- Dwyer, T.; Whelan, D.; Shah, P.S.; Ajrawat, P.; Hoit, G.; Chahal, J. Operative versus nonoperative treatment of femoroacetabular impingement syndrome: A meta-analysis of short-term outcomes. Arthroscopy 2020, 36, 263–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunt, D.; Prather, H.; Hayes, M.H.; Clohisy, J.C. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PMR 2012, 4, 479–487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monn, S.; Maffiuletti, N.A.; Bizzini, M.; Sutter, R.; Naal, F.D.; Leunig, M.; Casartelli, N.C. Mid-term outcomes of exercise therapy for the non-surgical management of femoroacetabular impingement syndrome: Are short-term effects persisting? Phys. Ther. Sport 2022, 55, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Müller-Torrente, A.; Puig-Torregrosa, J.; Montero-Navarro, S.; Sanz-Reig, J.; Morera-Balaguer, J.; Más-Martínez, J.; Sánchez-Mas, J.; Botella-Rico, J.M. Benefits of a specific and supervised rehabilitation program in femoroacetabular impingement patients undergoing hip arthroscopy: A randomized control trial. J. Clin. Med. 2021, 10, 3125. [Google Scholar] [CrossRef] [PubMed]
- Frasson, V.B.; Vaz, M.A.; Morales, A.B.; Torresan, A.; Telöken, M.A.; Gusmão, P.D.F.; Crestani, M.V.; Baroni, B.M. Hip muscle weakness and reduced joint range of motion in patients with femoroacetabular impingement syndrome: A case-control study. Braz. J. Phys. Ther. 2020, 24, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.-C.; Karlsson, H. The star excursion balance test: Criterion and divergent validity on patients with femoral acetabular impingement. Man. Ther. 2016, 26, 104–109. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- O’Brien, M.; Bourne, M.N.; Heerey, J.; Timmins, R.G.; Pizzari, T. A novel device to assess hip strength: Concurrent validity and normative values in male athletes. Phys. Ther. Sport 2019, 35, 63–68. [Google Scholar] [CrossRef] [Green Version]
- Tak, I.; Tijssen, M.; Schamp, T.; Sierevelt, I.; Thorborg, K.; Kerkhoffs, G.; Stubbe, J.; Van Beijsterveldt, A.-M.; Haverkamp, D. The Dutch Hip and Groin Outcome Score: Cross-cultural adaptation and validation according to the COSMIN checklist. J. Orthop. Sports Phys. Ther. 2018, 48, 299–306. [Google Scholar] [CrossRef]
- Powden, C.J.; Dodds, T.K.; Gabriel, E.H. The reliability of the star excursion balance test and lower quarter Y-balance test in healthy adults: A systematic review. Int. J. Sports Phys. Ther. 2019, 14, 683–694. [Google Scholar] [CrossRef] [PubMed]
- Zapparoli, F.Y.; Riberto, M. Isokinetic evaluation of the hip flexor and extensor muscles: A systematic review. J. Sport Rehabil. 2017, 26, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Serong, S.; Fickert, S.; Niemeyer, P.; Banke, I.J.; Goronzy, J.; Sobau, C.; Zinser, W.; Landgraeber, S. Outcome-affecting parameters of hip arthroscopy for femoroacetabular impingement with concomitant cartilage damage—data analysis from the German cartilage registry. J. Clin. Med. 2022, 11, 1532. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Bedi, A.; Fu, F.; Karlsson, J.; Ayeni, O.R.; Bhandari, M. New perspectives on femoroacetabular impingement syndrome. Nat. Rev. Rheumatol. 2016, 12, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Siebenrock, K.-A.; Ferner, F.; Noble, P.; Santore, R.; Werlen, S.; Mamisch, T.C. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin. Orthop. Relat. Res. 2011, 469, 3229–3240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polat, G.; Şahin, K.; Arzu, U.; Kendirci, A.Ş.; Aşık, M. Prevalence of asymptomatic femoroacetabular impingement in Turkey; cross sectional study. Acta Orthop. Traumatol. Turcica 2018, 52, 49–53. [Google Scholar] [CrossRef]
- Ishøi, L.; Thorborg, K.; Ørum, M.G.; Kemp, J.L.; Reiman, M.P.; Hölmich, P. How many patients achieve an acceptable symptom state after hip arthroscopy for femoroacetabular impingement syndrome? A cross-sectional study including pass cutoff values for the HAGOS and iHOT-33. Orthop. J. Sports Med. 2021, 9, 2325967121995267–2325967121995275. [Google Scholar] [CrossRef]
- Pålsson, A.; Kostogiannis, I.; Ageberg, E. Combining results from hip impingement and range of motion tests can increase diagnostic accuracy in patients with FAI syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 3382–3392. [Google Scholar] [CrossRef] [Green Version]
- Diamond, L.E.; Dobson, F.L.; Bennell, K.L.; Wrigley, T.V.; Hodges, P.W.; Hinman, R.S. Physical impairments and activity limitations in people with femoroacetabular impingement: A systematic review. Br. J. Sports Med. 2015, 49, 230–242. [Google Scholar] [CrossRef] [Green Version]
- Freke, M.; Kemp, J.L.; Svege, I.; Risberg, M.A.; Semciw, A.I.; Crossley, K.M. Physical impairments in symptomatic femoroacetabular impingement: A systematic review of the evidence. Br. J. Sports Med. 2016, 50, 1180. [Google Scholar] [CrossRef]
- Naili, J.E.; Stålman, A.; Valentin, A.; Skorpil, M.; Weidenhielm, L. Hip joint range of motion is restricted by pain rather than mechanical impingement in individuals with femoroacetabular impingement syndrome. Arch. Orthop. Trauma Surg. 2022, 142, 1985–1994. [Google Scholar] [CrossRef] [PubMed]
- Hatton, A.L.; Kemp, J.L.; Brauer, S.G.; Clark, R.A.; Crossley, K.M. Impairment of dynamic Single-Leg balance performance in individuals with hip chondropathy. Arthritis Care Res. 2014, 66, 709–716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Picorelli, A.M.; Hatton, A.L.; Gane, E.M.; Smith, M.D. Balance performance in older adults with hip osteoarthritis: A systematic review. Gait Posture 2018, 65, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Hartigan, D.E.; Perets, I.; Meghpara, M.B.; Mohr, M.R.; Close, M.R.; Yuen, L.C.; Domb, B.G. Biomechanics, anatomy, pathology, imaging and clinical evaluation of the acetabular labrum: Current concepts. J. ISAKOS 2018, 3, 148–154. [Google Scholar] [CrossRef]
- Frank, J.M.; Harris, J.D.; Erickson, B.J.; Slikker III, W.; Bush-Joseph, C.A.; Salata, M.J.; Nho, S.J. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: A systematic review. Arthroscopy 2015, 31, 1199–1204. [Google Scholar] [CrossRef]
- Ng, K.G.; Mantovani, G.; Modenese, L.; Beaulé, P.E.; Lamontagne, M. Altered walking and muscle patterns reduce hip contact forces in individuals with symptomatic cam femoroacetabular impingement. Am. J. Sports Med. 2018, 46, 2615–2623. [Google Scholar] [CrossRef]
- Spiker, A.M.; Kraszewski, A.P.; Maak, T.G.; Nwachukwu, B.U.; Backus, S.I.; Hillstrom, H.J.; Kelly, B.T.; Ranawat, A.S. Dynamic Assessment of Femoroacetabular Impingement Syndrome Hips. Arthroscopy 2022, 38, 404–416. [Google Scholar] [CrossRef]
- Kierkegaard, S.; Mechlenburg, I.; Lund, B.; Søballe, K.; Dalgas, U. Impaired hip muscle strength in patients with femoroacetabular impingement syndrome. J. Sci. Med. Sport 2017, 20, 1062–1067. [Google Scholar] [CrossRef]
- Casartelli, N.; Maffiuletti, N.; Item-Glatthorn, J.; Staehli, S.; Bizzini, M.; Impellizzeri, F.; Leunig, M. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthr. Cartil. 2011, 19, 816–821. [Google Scholar] [CrossRef] [Green Version]
- Diamond, L.E.; Wrigley, T.V.; Hinman, R.S.; Hodges, P.W.; O’Donnell, J.; Takla, A.; Bennell, K.L. Isometric and isokinetic hip strength and agonist/antagonist ratios in symptomatic femoroacetabular impingement. J. Sci. Med. Sport 2016, 19, 696–701. [Google Scholar] [CrossRef]
- Heuck, A.; Dienst, M.; Glaser, C. Femoroazetabuläres Impingement–Update 2019. Der Radiol. 2019, 59, 242–256. [Google Scholar] [CrossRef] [PubMed]



| Variables | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Healthy (n = 52) | FAIasym (n = 51) | FAIsym (n = 52) | p-Value | Healthy (n = 51) | FAIasym (n = 52) | FAIsym (n = 49) | p-Value | |
| Age, years | 28.4 ± 3.3 | 27.2 ± 4.5 | 28.5 ± 3.6 | 0.241 | 27.1 ± 4.5 | 26.2 ± 3.3 | 26.7 ± 3.4 | 0.457 |
| Height, cm | 176.5 ± 4.5 | 177.4 ± 4.6 | 176.3 ± 3.3 | 0.563 | 166.3 ± 3.2 | 167.0 ± 3.2 | 165.4 ± 4.2 | 0.410 |
| Weight, kg | 70.3 ± 5.4 | 69.7 ± 5.3 | 71.7 ± 4.5 | 0.674 | 58.7 ± 6.6 | 59.3 ± 7.4 | 57.3 ± 6.5 | 0.419 |
| BMI, kg/m2 | 22.7 ± 3.7 | 22.3 ± 3.7 | 23.1 ± 3.8 | 0.301 | 21.4 ± 2.3 | 21.5 ± 3.5 | 21.2 ± 3.3 | 0.386 |
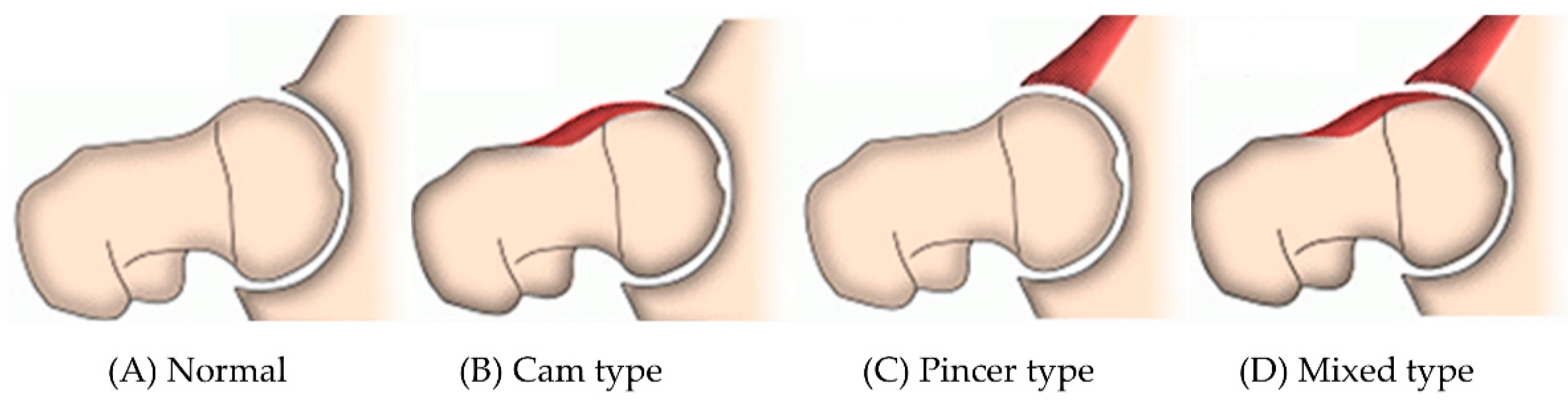
| Cam type | – | 21 (41.2%) | 22 (42.3%) | 0.360 | – | 23 (44.2%) | 20 (40.8%) | 0.312 |
| Pincer type | – | 17 (33.3%) | 14 (26.9%) | – | 16 (30.8%) | 15 (30.6%) | ||
| Mixed type | – | 13 (25.5%) | 16 (30.8%) | – | 13 (25.0%) | 14 (28.6%) | ||
| HAGOS | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Healthy | FAIasym | FAIsym | p-Value | Healthy | FAIasym | FAIsym | p-Value | |
| Symptoms | 91.3 ± 3.8 | 85.2 ± 7.5 | 55.4 ± 18.5 b,c | <0.001 | 93.5 ± 2.2 | 86.6 ± 8.7 | 64.5 ± 17.5 b,c | <0.001 |
| Pain | 93.2 ± 4.6 | 90.5 ± 8.4 | 61.3 ± 23.3 b,c | <0.001 | 90.6 ± 2.4 | 88.4 ± 9.5 | 53.4 ± 16.7 b,c | <0.001 |
| ADL | 92.4 ± 4.3 | 90.7 ± 6.2 | 56.6 ± 19.8 b,c | <0.001 | 90.8 ± 2.2 | 88.7 ± 7.8 | 58.7 ± 21.4 b,c | <0.001 |
| Sport and recreation | 89.6 ± 5.7 | 85.8 ± 8.8 | 38.1 ± 21.9 b,c | <0.001 | 88.3 ± 4.6 | 85.1 ± 7.9 | 44.2 ± 13.7 b,c | <0.001 |
| Physical activity | 93.2 ± 2.1 | 87.9 ± 8.0 | 40.8 ± 26.0 b,c | <0.001 | 89.9 ± 3.8 | 87.8 ± 8.0 | 38.9 ± 18.2 b,c | <0.001 |
| Quality of life | 91.6 ± 3.2 | 86.6 ± 5.6 | 43.4 ± 26.4 b,c | <0.001 | 91.2 ± 3.9 | 85.4 ± 8.4 | 61.5 ± 14.8 b,c | <0.001 |
| HAGOS total score | 91.7 ± 4.2 | 87.2 ± 7.4 | 49.9 ± 22.2 b,c | <0.001 | 91.7 ± 2.4 | 86.2 ± 8.2 | 53.9 ± 17.3 b,c | <0.001 |
| ROM, Degree | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Healthy | FAIasym | FAIsym | p-Value | Healthy | FAIasym | FAIsym | p-Value | |
| Flexion | 130.0 ± 12.6 | 126.6 ± 14.3 | 108.6 ± 20.7 b,c | 0.021 | 138.3 ± 14.7 | 132.5 ± 15.5 | 109.3 ± 18.3 | 0.004 |
| Extension | 13.4 ± 3.4 | 12.3 ± 3.2 | 13.1 ± 3.2 | 0.385 | 15.2 ± 5.4 | 14.8 ± 5.3 | 15.2 ± 5.5 | 0.320 |
| Adduction | 22.6 ± 3.8 | 21.9 ± 3.8 | 19.7 ± 6.2 b,c | 0.016 | 24.7 ± 6.2 | 22.5 ± 6.8 | 20.6 ± 8.6 b,c | 0.003 |
| Abduction | 39.8 ± 5.2 | 38.5 ± 6.0 | 38.3 ± 6.7 | 0.127 | 44.4 ± 9.1 | 42.3 ± 9.5 | 41.7 ± 8.7 | 0.358 |
| Internal rotation | 43.4 ± 5.9 | 40.2 ± 7.4 | 35.6 ± 5.1 b,c | 0.004 | 48.3 ± 7.8 | 45.8 ± 8.3 | 38.8 ± 8.8 b,c | 0.012 |
| External rotation | 49.3 ± 5.3 | 42.9 ± 5.2 | 28.2 ± 6.6 b,c | <0.001 | 53.8 ± 8.3 | 47.3 ± 10.7 | 33.5 ± 9.5 b,c | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, J.; Kim, Y.; Choi, M.; Zhang, C. Characteristics of Biomechanical and Physical Function According to Symptomatic and Asymptomatic Acetabular Impingement Syndrome in Young Adults. Healthcare 2022, 10, 1484. https://doi.org/10.3390/healthcare10081484
Zhang J, Kim Y, Choi M, Zhang C. Characteristics of Biomechanical and Physical Function According to Symptomatic and Asymptomatic Acetabular Impingement Syndrome in Young Adults. Healthcare. 2022; 10(8):1484. https://doi.org/10.3390/healthcare10081484
Chicago/Turabian StyleZhang, Junyong, Yonghwan Kim, Moonyoung Choi, and Cong Zhang. 2022. "Characteristics of Biomechanical and Physical Function According to Symptomatic and Asymptomatic Acetabular Impingement Syndrome in Young Adults" Healthcare 10, no. 8: 1484. https://doi.org/10.3390/healthcare10081484






