Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial
Abstract
:1. Introduction
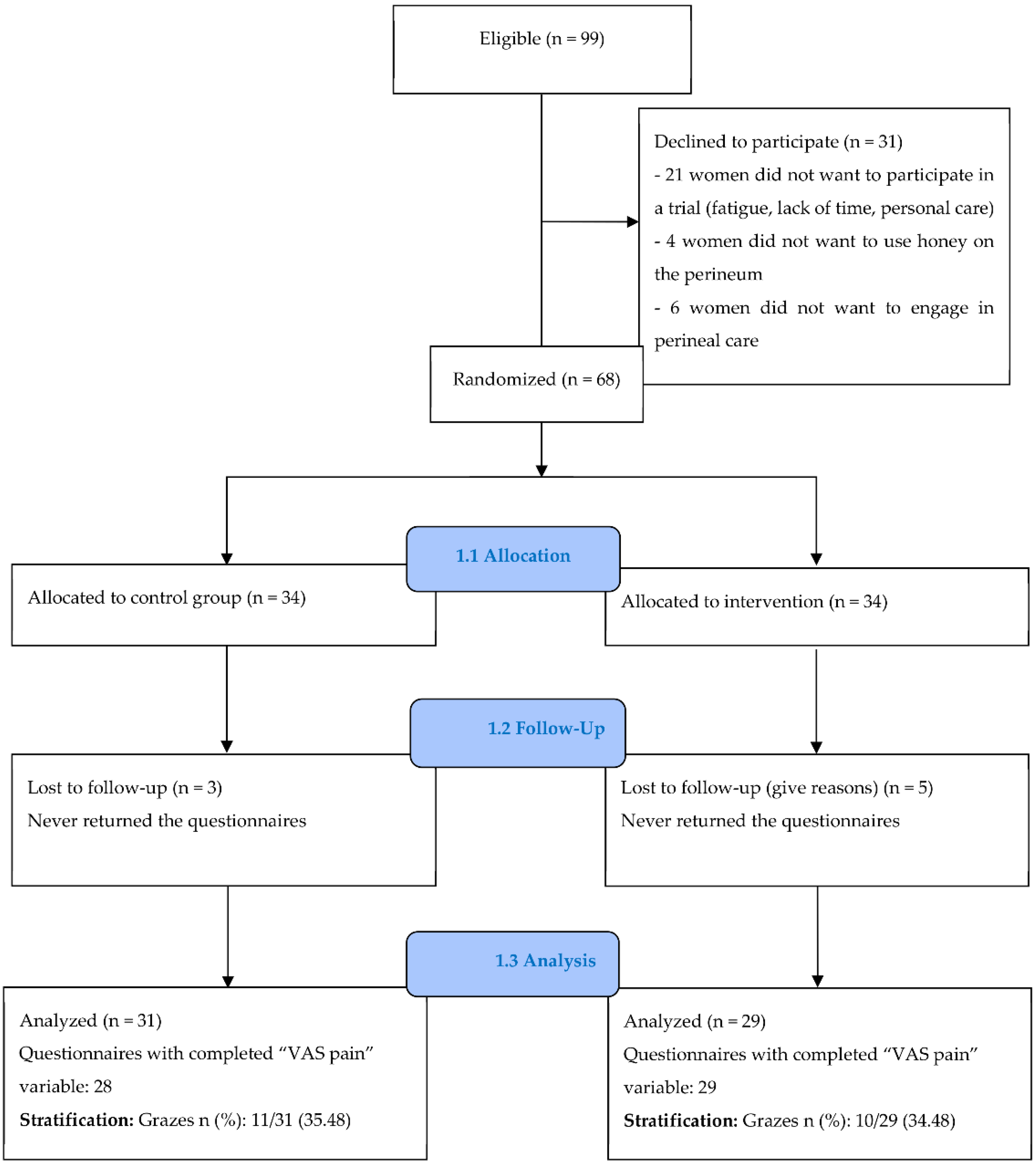
2. Materials and Methods
2.1. Trial Design and Setting
2.2. Sample Size
2.3. Participants and Recruitment Procedure
2.4. Interventions
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics of Participants
3.2. Comparison of the Primary and Secondary Outcomes between Groups
3.3. Compliance and Satisfaction with the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jansson, M.H.; Franzén, K.; Hiyoshi, A.; Tegerstedt, G.; Dahlgren, H.; Nilsson, K. Risk Factors for Perineal and Vaginal Tears in Primiparous Women—The Prospective POPRACT-Cohort Study. BMC Pregnancy Childbirth 2020, 20, 749. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.A.; Price, N.; Simonite, V.; Burns, E.E. Incidence of and Risk Factors for Perineal Trauma: A Prospective Observational Study. BMC Pregnancy Childbirth 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Desseauve, D.; Proust, S.; Carlier-Guerin, C.; Rutten, C.; Pierre, F.; Fritel, X. Evaluation of Long-Term Pelvic Floor Symptoms after an Obstetric Anal Sphincter Injury (OASI) at Least One Year after Delivery: A Retrospective Cohort Study of 159 Cases. Gynécol. Obs. Fertil. 2016, 44, 385–390. [Google Scholar] [CrossRef]
- Elharmeel, S.M.; Chaudhary, Y.; Tan, S.; Scheermeyer, E.; Hanafy, A.; van Driel, M.L. Surgical Repair of Spontaneous Perineal Tears That Occur during Childbirth versus No Intervention. Cochrane Database Syst. Rev. 2011, 8, CD008534. [Google Scholar] [CrossRef]
- Webb, S.; Sherburn, M.; Ismail, K.M.K. Managing Perineal Trauma after Childbirth. BMJ 2014, 349, g6829. [Google Scholar] [CrossRef]
- Macarthur, A.J.; Macarthur, C. Incidence, Severity, and Determinants of Perineal Pain after Vaginal Delivery: A Prospective Cohort Study. Am. J. Obstet. Gynecol. 2004, 191, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, A.J.; Ramsay, I.N. The Psychosocial Impact of Urinary Incontinence in Women. Obstet. Gynaecol. 2011, 13, 143–148. [Google Scholar] [CrossRef]
- Skinner, E.M.; Barnett, B.; Dietz, H.P. Psychological Consequences of Pelvic Floor Trauma Following Vaginal Birth: A Qualitative Study from Two Australian Tertiary Maternity Units. Arch. Womens Ment. Health 2018, 21, 341–351. [Google Scholar] [CrossRef]
- Sénat, M.-V.; Sentilhes, L.; Battut, A.; Benhamou, D.; Bydlowski, S.; Chantry, A.; Deffieux, X.; Diers, F.; Doret, M.; Ducroux-Schouwey, C.; et al. Post-Partum: Recommandations Pour La Pratique Clinique—Texte Court. Rev. Sage Femme 2016, 15, 30–40. [Google Scholar] [CrossRef]
- Panchaud, A.; Rothuizen, L.; Buclin, T.; Fischer, C. Médicaments et Allaitement: Quelques Éléments à Considérer Avant de Les Juger Incompatibles. Rev. Med. Suisse 2008, 4, 540–545. [Google Scholar] [PubMed]
- Jull, A.B.; Cullum, N.; Dumville, J.C.; Westby, M.J.; Deshpande, S.; Walker, N. Honey as a Topical Treatment for Wounds. In The Cochrane Library; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015. [Google Scholar] [CrossRef]
- Molan, P.; Rhodes, T. Honey: A Biologic Wound Dressing. Wounds Compend. Clin. Res. Pract. 2015, 27, 141–151. [Google Scholar]
- Lavaf, M.; Simbar, M.; Mojab, F.; Alavi Majd, H.; Samimi, M. Comparison of Honey and Phenytoin (PHT) Cream Effects on Intensity of Pain and Episiotomy Wound Healing in Nulliparous Women. J. Complement. Integr. Med. 2017, 15. [Google Scholar] [CrossRef] [PubMed]
- Manjula, P.; Anitha, C.R.; Ranjani, P. Effectiveness of Honey Versus Betadine on Episiotomy Wound Healing. Manag. J. Nurs. 2012, 2, 32–37. [Google Scholar]
- Sheikhan, F.; Jahdi, F.; Khoei, E.M.; Shamsalizadeh, N.; Sheikhan, M.; Haghani, H. Episiotomy Pain Relief: Use of Lavender Oil Essence in Primiparous Iranian Women. Complement. Ther. Clin. Pract. 2012, 18, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.F.; Bjerre, E.; Hansen, M.D.; Hilden, J.; Landler, N.E.; Tendal, B.; Hróbjartsson, A. Pain Relief That Matters to Patients: Systematic Review of Empirical Studies Assessing the Minimum Clinically Important Difference in Acute Pain. BMC Med. 2017, 15, 35. [Google Scholar] [CrossRef]
- Amorim Francisco, A.; Junqueira Vasconcellos de Oliveira, S.M.; Barbosa da Silva, F.M.; Bick, D.; Gonzalez Riesco, M.L. Women’s Experiences of Perineal Pain during the Immediate Postnatal Period: A Cross-Sectional Study in Brazil. Midwifery 2011, 27, e254–e259. [Google Scholar] [CrossRef]
- Alvarenga, M.B.; de Oliveira, S.M.J.V.; Francisco, A.A.; da Silva, F.M.B.; Sousa, M.; Nobre, M.R. Effect of Low-Level Laser Therapy on Pain and Perineal Healing after Episiotomy: A Triple-Blind Randomized Controlled Trial. Lasers Surg. Med. 2017, 49, 181–188. [Google Scholar] [CrossRef]
- Sealed Envelope. Power Calculator for Continuous Outcome Superiority Trial. Available online: https://www.sealedenvelope.com/power/continuous-superiority/ (accessed on 27 March 2018).
- Haelle, T. ACOG: New Recommandations on Obstetric Lacerations. Medscape. 2016. Available online: https://www.medscape.com/viewarticle/865296 (accessed on 27 March 2018).
- Marshall, J.; Raynor, M. Myles Textbook for Midwives, 16th ed.; Churchill Livingstone: London, UK, 2014. [Google Scholar]
- Meaume, S.; Dereure, O.; Téot, L. Plaies et Cicatrisations; Masson: Paris, France, 2005. [Google Scholar]
- Laubscher, A.; Dayer, P. Tableau Materiel de Pansement. Available online: https://www.hug.ch/sites/interhug/files/technique_soins/pdf/tableau_materiel_pansement.pdf (accessed on 20 January 2021).
- Carter, D.A.; Blair, S.E.; Cokcetin, N.N.; Bouzo, D.; Brooks, P.; Schothauer, R.; Harry, E.J. Therapeutic Manuka Honey: No Longer So Alternative. Front. Microbiol. 2016, 7, 569. [Google Scholar] [CrossRef] [PubMed]
- The Joanna Briggs Instutite. The Use of Medical-Grade Honey in Wound Care. Wound Pract. Res. 2011, 19, 171–173. [Google Scholar]
- Gardénal, M. Le Miel de Manuka: Ce Miel qui Soigne Antibactérien, Antibiotique, Anti Inflammatoire, Cicatrisant, quels Sont les Secrets des Propriétés Exceptionnelles de ce Miel Unique au Monde? Déliver: Toulon, France, 2013. [Google Scholar]
- Hôpitaux Universiraires de Genève. Home—Pharmacie à Genève aux HUG. Available online: https://pharmacie.hug.ch/ (accessed on 9 January 2021).
- Marquié, L.; Duarte, L.-R.; Mauriès, V.; Izard, P.; Pouymayou, J. Les caractéristiques psychométriques du Questionnaire de douleur de Saint-Antoine en consultation d’algologie chez les personnes atteintes de cancer. Douleur Analgésie 2008, 21, 52–61. [Google Scholar] [CrossRef]
- Melzack, R. The Short-Form McGill Pain Questionnaire. Pain 1987, 30, 191–197. [Google Scholar] [CrossRef]
- Shirvani, M.A.; Nikpour, M.; Azadbakht, M.; Banihosseini, S.Z.; Zanjani, R. The Effect of Honey Gel on Cesarean Incision Pain: A Triple Blind Clinical Trial. Afr. J. Pharm. Pharmacol. 2013, 7, 19–24. [Google Scholar] [CrossRef]
- Dufour, J.; Santagata, M. Les Effets du Miel Sur la Cicatrice de Césarienne—Travail de Bachelor. Available online: http://doc.rero.ch/record/305329 (accessed on 20 January 2021).
- Heidari, T.; Roozbahani, N.; Amiri Farahani, L.; Attarha, M.; Akbari Torkestani, N.; Jamilian, M.; Bekhradi, R. Does Iranian Astragalus Gossypinus Honey Assist in Healing Caesarean Wounds and Scars? Eur. J. Integr. Med. 2013, 5, 226–233. [Google Scholar] [CrossRef]
- Magalon, G.; Vanwijck, R. Guide Des Plaies. Du Pansement à La Chirurgie; John Libbey Eurotext: Paris, France, 2003. [Google Scholar]
- Manresa, M.; Pereda, A.; Bataller, E.; Terre-Rull, C.; Ismail, K.M.; Webb, S.S. Incidence of Perineal Pain and Dyspareunia Following Spontaneous Vaginal Birth: A Systematic Review and Meta-Analysis. Int. Urogynecol. J. 2019, 30, 853–868. [Google Scholar] [CrossRef]
- Carr, A.C. Therapeutic Properties of New Zealand and Australian Tea Trees (Leptospermum and Melaleuca). N. Z. Pharm. 1998, 18. [Google Scholar]
- Moroni, C.; Laurent, B. Influence de La Douleur Sur La Cognition. Psychol. Neuropsychiatr. Vieil. 2006, 4, 21–30. [Google Scholar] [PubMed]
- Seridi, H.B.; Beauquier-Maccotta, B. Les troubles du sommeil pendant la grossesse et pendant le post-partum (revue de la littérature). Ann. Méd. Psychol. Rev. Psychiatr. 2019, 177, 655–662. [Google Scholar] [CrossRef]
- Kettle, C.; Dowswell, T.; Ismail, K.M. Continuous and Interrupted Suturing Techniques for Repair of Episiotomy or Second-Degree Tears. Cochrane Database Syst. Rev. 2012, 11, CD000947. [Google Scholar] [CrossRef] [PubMed]

| Control (n = 31) | Intervention (n = 29) | Total (n = 60) | ||
|---|---|---|---|---|
| Mean age (SD) | 33.80 (5.04) | 33.31 (4.31) | 33.57 (4.67) | |
| Mean BMI (SD) | 23.54 (3.87) | 24.07 (3.74) | 23.80 (3.79) | |
| Education n (%) | Primary school | 2/31 (6.45) | 3/29 (10.34) | 5/60 (8.33) |
| Secondary school | 4/31 (12.90) | 2/29 (6.90) | 6/60 (10.00) | |
| Apprenticeship | 7/31 (22.58) | 4/29 (13.79) | 11/60 (18.33) | |
| University | 18/31 (58.67) | 20/29 (68.97) | 38/60 (63.33) | |
| Tobacco use n (%) | 4/31 (12.90) | 3/29 (10.34) | 7/60 (11.67) | |
| Diabetes 1 n (%) | 0/31 (0.00) | 4/29 (13.79) | 4/60 (6.67) | |
| Gestation n (%) | 1st | 13/31 (41.94) | 12/29 (41.38) | 25/60 (41.67) |
| ≥2 | 18/31 (58.06) | 17/29 (58.62) | 35/60 (58.33) | |
| Parity n (%) | 1st | 17/31 (54.84) | 14/29 (48.28) | 31/60 (51.67) |
| ≥2 | 14/31 (45.16) | 15/29 (51.72) | 29/60 (48.33) | |
| Personal treatment 2 n (%) | 4/31 (87.10) | 4/29 (86.21) | 8/60 (13.33) | |
| Mode of birth n (%) | Spontaneous 3 | 23/31 (74.19) | 22/29 (75.86) | 45/60 (75.00) |
| Instrumental 4 | 8/31 (25.81) | 7/29 (24.14) | 15/60 (25.00) | |
| Anesthesia n (%) | Epidural | 25/31 (80.65) | 19/29 (65.52) | 44/60 (73.33) |
| Local | 6/31 (19.35) | 10/29 (34.48) | 16/60 (26.67) | |
| Perineal tears n (%) | 1st degree | 12/31 (38.71) | 13/29 (44.83 | 25/60 (41.67) |
| 2nd degree | 15/31 (48.39) | 10/29 (34.48) | 25/60 (41.67) | |
| Episiotomy | 4/31 (12.90) | 6/29 (20.69) | 10 /60 (16.67) | |
| Grazes n (%) | 11/31 (35.48) | 10/29 (34.48) | 21/60 (35.00) | |
| Mean neonate weight gr (SD) | 3285 (570) | 3357 (350) | 3320 (474) | |
| Control (n= 31) | Intervention (n = 29) | Chi 2 | |
|---|---|---|---|
| Not at all n (%) | 0 (0.00) | 0 (0.00) | |
| A little n (%) | 6 (19.35) | 6 (20.69) | |
| I do not know n (%) | 8 (25.81) | 13 (44.83) | 0.33 |
| A lot n (%) | 14 (45.16) | 7 (24.14) | |
| Very much n (%) | 3 (9.68) | 3 (10.34) |
| Day 1 | Day 4 | |||||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | p-Value | Control | Intervention | p-Value | |||
| VAS perineal pain | Mean VAS pain (SD) | 3.38 (2.14) (n = 29) | 3.34 (2.35) (n = 29) | 0.65 | 2.28 (1.96) (n = 28) | 1.41 (1.49) (n = 29) | 0.09 | |
| Mean without grazes (SD) | 3.61 (2.36) (n = 18) | 3.76 (2.48) (n = 19) | 0.87 | 1.84 (1.67) (n = 18) | 1.5 1.77) (n = 19) | 0.57 | ||
| Mean with grazes (SD) | 3.02 (1.78) (n = 11) | 2.53 (1.96) (n = 10) | 0.50 | 3.08 (2.26) (n = 10) | 1.15 (0.78) (n = 10) | 0.054 | ||
| p-value | 0.49 | 0.22 | - | 0.49 | 0.22 | - | ||
| QDSA | Likert QDSA | No pain n (%) | 2/31 (6.45) | 1/29 (3.45) | 0.95 | 5/30 (16.67) | 6/29 (20.69) | 0.44 |
| Mild n (%) | 9/31 (29.03) | 8/29 (27.59) | 12/30 (40.00) | 15/29 (51.72) | ||||
| Discomforting n (%) | 15/31 (48.39) | 15/29 (51.72) | 12/30 (40.00) | 7/29 (24.14) | ||||
| Distressing n (%) | 5/31 (16.13) | 5/29 (17.24) | 0/30 (0.00) | 1/29 (3.45) | ||||
| Horrible n (%) | 0/31 (0.00) | 0/29 (0.00) | 1/30 (3.33) | 0/29 (0.00) | ||||
| Excruciating n (%) | 0/31 (0.00) | 0/29 (0.00) | 0/30 (0.00) | 0/29 (0.00) | ||||
| Sensory category | Mean intensity score (SD) | 6.07 (4.55) | 6.41 (4.19) | 0.64 | 4.10 (4.40) | 2.93 (2.83) | 0.44 | |
| Mean number of words chosen (SD) | 3.53 (2.24) | 3.79 (2.01) | 0.63 | 2.6 (2.08) | 2.17 (1.65) | 0.47 | ||
| Affective category | Mean intensity score (SD) | 2.57 (3.56) | 3.14 (3.54) | 0.30 | 2.2 (3.86) | 1.0 (1.89) | 0.20 | |
| Mean number of words chosen (SD) | 1.53 (2.03) | 2.28 (2.28) | 0.14 | 1.47 (2.24) | 0.86 (1.51) | 0.24 | ||
| Total | Mean intensity score (SD) | 8.63 (7.64) | 9.55 (7.03) | 0.42 | 6.3 (7.94) | 3.93 (3.90) | 0.46 | |
| Mean number of words chosen (SD) | 5.07 (3.92) | 6.07 (3.96) | 0.33 | 4.07 (4.01) | 3.03 (2.85) | 0.34 | ||
| Pain relief drugs use | Women who used pain relief drugs n (%) | 26/31 (83.87) | 23/29 (79.31) | 0.75 | 17/31 (54.84) | 13/28 (46.43) | 0.61 | |
| Mean paracetamol use in mg (SD) | 1466.67 (1224.28) | 1535.71 (1393.96) | 0.94 | 866.67 (1129.03) | 611.11 (923.34) | 0.50 | ||
| Mean ibuprofen use in mg (SD) | 646.67 (537.38) | 707.14 (614.59) | 0.79 | 466.67 (539.05) | 192.59 (339.60) | 0.049 | ||
| VAS urinary burning | Mean VAS urinary burning (SD) | 2.42 (2.18) (n = 29) | 2.64 (2.52) (n = 28) | 0.99 | 1.73 (2.07) (n = 29) | 1.32 (1.93) (n = 28) | 0.31 | |
| Mean without grazes (SD) | 2.23 (2.41) (n = 18) | 2.50 (2.69) (n = 18) | 0.94 | 1.14 (1.52) (n = 18) | 1.39 (2.22) (n = 18) | 0.94 | ||
| Mean with grazes (SD) | 2.73 (1.80) (n = 11) | 2.88 (2.29) (n = 10) | 0.97 | 2.69 (2.55) (n = 11) | 1.19 (1.34) (n = 10) | 0.12 | ||
| p-value | 0.29 | 0.45 | - | 0.03 | 0.71 | - | ||
| Day 1 | Day 4 | |||
|---|---|---|---|---|
| Degree of Satisfaction | n = 29 | n = 28 | ||
| Not at all n (%) | 0/29 (0.00) | 2/29 (6.90) | 0/28 (0.00) | 2/28 (7.14) |
| A little satisfied n (%) | 0/29 (0.00) | 0/28 (0.00) | ||
| Somewhat satisfied n (%) | 2/29 (6.90) | 2/28 (7.14) | ||
| Satisfied n (%) | 18/29 (62.07) | 27/29 (93.10) | 11/28 (39.29) | 26/28 (92.86) |
| Very satisfied n (%) | 9/29 (31.03) | 15/28 (53.57) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerosa, D.; Santagata, M.; Martinez de Tejada, B.; Guittier, M.-J. Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial. Healthcare 2022, 10, 1515. https://doi.org/10.3390/healthcare10081515
Gerosa D, Santagata M, Martinez de Tejada B, Guittier M-J. Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial. Healthcare. 2022; 10(8):1515. https://doi.org/10.3390/healthcare10081515
Chicago/Turabian StyleGerosa, Désirée, Marika Santagata, Begoña Martinez de Tejada, and Marie-Julia Guittier. 2022. "Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial" Healthcare 10, no. 8: 1515. https://doi.org/10.3390/healthcare10081515
APA StyleGerosa, D., Santagata, M., Martinez de Tejada, B., & Guittier, M.-J. (2022). Application of Honey to Reduce Perineal Laceration Pain during the Postpartum Period: A Randomized Controlled Trial. Healthcare, 10(8), 1515. https://doi.org/10.3390/healthcare10081515






