The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review
Abstract
:1. Introduction
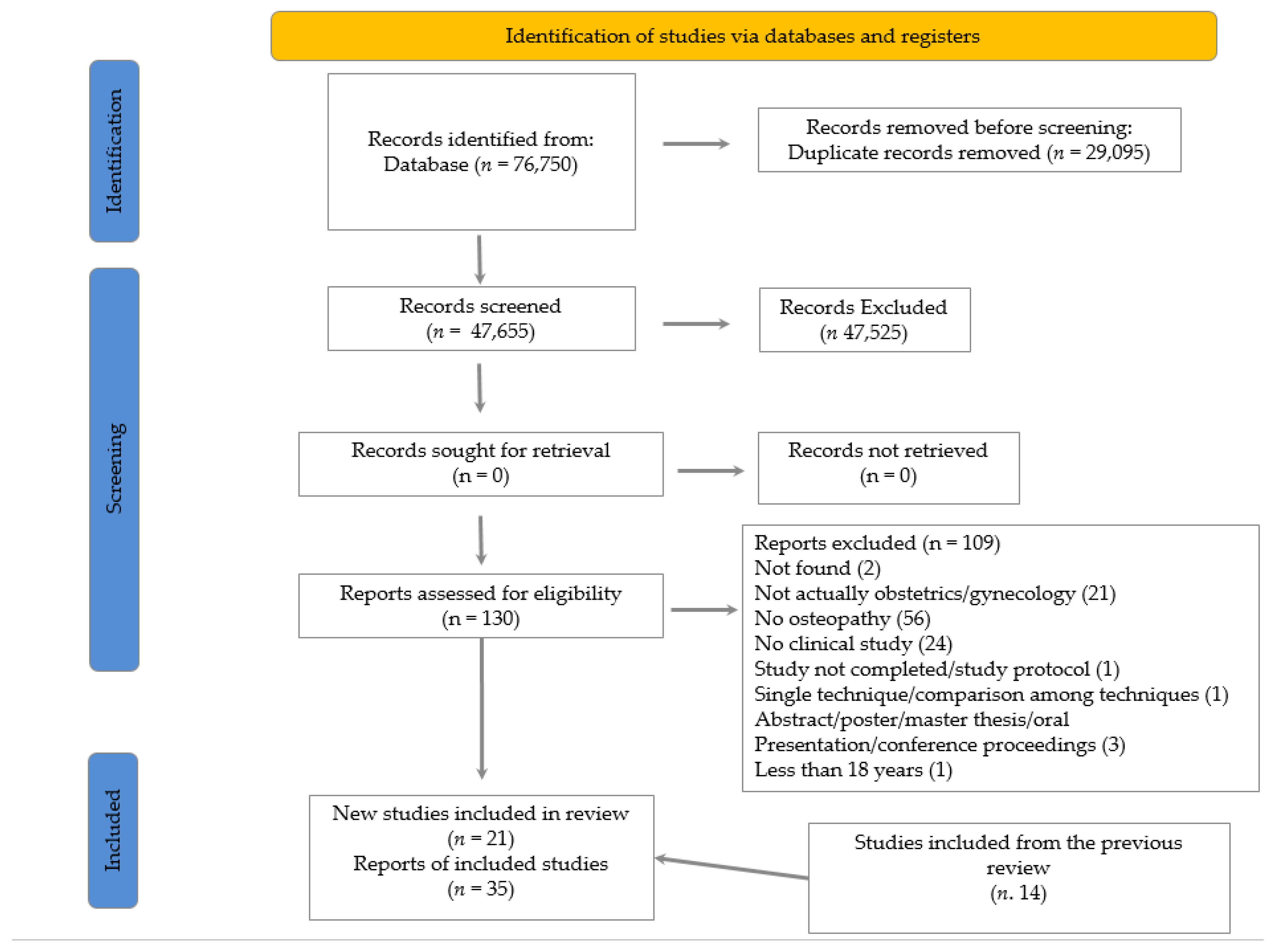
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Items
2.4. Selection Process
2.5. Data Extraction
2.6. Data Analysis
2.7. Differences with the Previous Review
3. Results
3.1. Pregnancy
3.2. Labour
3.3. Postpartum
3.4. Pelvic Pain
3.5. Vulvodynia
3.6. Endometriosis
3.7. Dysmenorrhea
3.8. Polycystic Ovary Syndrome (PCOS)
3.9. Menopause
3.10. Somatic Dysfunction and Characteristics of the Treatment Session
3.11. Side Effects and Health Economics
3.12. Quality Assessment
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tramontano, M.; Pagnotta, S.; Lunghi, C.; Manzo, C.; Manzo, F.; Consolo, S.; Manzo, V. Assessment and Management of Somatic Dysfunctions in Patients With Patellofemoral Pain Syndrome. J. Osteopat. Med. 2020, 120, 165–173. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems; World Health Organization: Geneve, Switzerland, 2019. [Google Scholar]
- American Association of Colleges of Osteopathic Medicine. Educational Council on Osteopathic Principles. In Glossary of Osteopathic Terminology; American Association of Colleges of Osteopathic Medicine: Bethesda, MD, USA, 2017; Available online: https://www.aacom.org/docs/default-source/insideome/got2011ed.pdf (accessed on 1 April 2022).
- Morin, C.; Gaboury, I. Osteopathic empirical research: A bibliometric analysis from 1966 to 2018. BMC Complement. Med. Ther. 2021, 21, 196. [Google Scholar] [CrossRef]
- Farra, F.D.; Risio, R.G.; Vismara, L.; Bergna, A. Effectiveness of osteopathic interventions in chronic non-specific low back pain: A systematic review and meta-analysis. Complement. Ther. Med. 2020, 56, 102616. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Consorti, G.; Morone, G.; Lunghi, C. Vertigo and Balance Disorders–The Role of Osteopathic Manipulative Treatment: A Systematic Review. Complement. Med. Res. 2020, 28, 368–377. [Google Scholar] [CrossRef]
- Tassorelli, C.; Tramontano, M.; Berlangieri, M.; Schweiger, V.; D’Ippolito, M.; Palmerini, V.; Bonazza, S.; Rosa, R.; Cerbo, R.; Buzzi, M.G. Assessing and treating primary headaches and cranio-facial pain in patients undergoing rehabilitation for neurological diseases. J. Headache Pain 2017, 18, 99. [Google Scholar] [CrossRef]
- Cerritelli, F.; Ruffini, N.; Lacorte, E.; Vanacore, N. Osteopathic manipulative treatment in neurological diseases: Systematic review of the literature. J. Neurol. Sci. 2016, 369, 333–341. [Google Scholar] [CrossRef]
- Tamburella, F.; Piras, F.; Piras, F.; Spanò, B.; Tramontano, M.; Gili, T. Cerebral Perfusion Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Front. Physiol. 2019, 10, 403. [Google Scholar] [CrossRef] [PubMed]
- Tramontano, M.; Cerritelli, F.; Piras, F.; Spanò, B.; Tamburella, F.; Piras, F.; Caltagirone, C.; Gili, T. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020, 10, 969. [Google Scholar] [CrossRef]
- Cerritelli, F.; Chiacchiaretta, P.; Gambi, F.; Perrucci, M.G.; Barassi, G.; Visciano, C.; Bellomo, R.G.; Saggini, R.; Ferretti, A. Effect of manual approaches with osteopathic modality on brain correlates of interoception: An fMRI study. Sci. Rep. 2020, 10, 3214. [Google Scholar] [CrossRef]
- Ponzo, V.; Cinnera, A.M.; Mommo, F.; Caltagirone, C.; Koch, G.; Tramontano, M. Osteopathic Manipulative Therapy Potentiates Motor Cortical Plasticity. J. Am. Osteopat. Assoc. 2018, 118, 396–402. [Google Scholar] [CrossRef]
- Baroni, F.; Tramontano, M.; Barsotti, N.; Chiera, M.; Lanaro, D.; Lunghi, C. Osteopathic structure/function models renovation for a person-centered approach: A narrative review and integrative hypothesis. J. Complement. Integr. Med. 2021. [Google Scholar] [CrossRef]
- Huang, G.; Le, A.-L.; Goddard, Y.; James, D.; Thavorn, K.; Payne, M.; Chen, I. A Systematic Review of the Cost of Chronic Pelvic Pain in Women. J. Obstet. Gynaecol. Can. 2021, 44, 286–293.e3. [Google Scholar] [CrossRef] [PubMed]
- Genario, R.; Morello, E.; Bueno, A.A.; Santos, H.O. The usefulness of melatonin in the field of obstetrics and gynecology. Pharmacol. Res. 2019, 147, 104337. [Google Scholar] [CrossRef] [PubMed]
- Ruffini, N.; D’Alessandro, G.; Cardinali, L.; Frondaroli, F.; Cerritelli, F. Osteopathic manipulative treatment in gynecology and obstetrics: A systematic review. Complement. Ther. Med. 2016, 26, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Baroni, F.; Ruffini, N.; D’Alessandro, G.; Consorti, G.; Lunghi, C. The role of touch in osteopathic practice: A narrative review and integrative hypothesis. Complement. Ther. Clin. Pract. 2020, 42, 101277. [Google Scholar] [CrossRef]
- Tramontano, M.; Tamburella, F.; Farra, F.D.; Bergna, A.; Lunghi, C.; Innocenti, M.; Cavera, F.; Savini, F.; Manzo, V.; D’Alessandro, G. International Overview of Somatic Dysfunction Assessment and Treatment in Osteopathic Research: A Scoping Review. Healthcare 2021, 10, 28. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- D’Alessandro, G.; Ruffini, N.; Iacopini, A.; Annoni, M.; Kossowsky, J.; Cerritelli, F. Overcoming placebo-related challenges in manual therapy trials: The ‘whats and hows’ and the ‘touch equality assumption’ proposals. Int. J. Osteopat. Med. 2021, 42, 5–10. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic Reviews of Etiology and Risk. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar]
- The Cochrane Collaboration. Review Manager (RevMan) [Computer Program],Version 5.4. 2020. [Google Scholar]
- Schreiber, C. Osteopathie bei Low Back Pain in der Schwangerschaft–eine Fallstudie. Osteopat. Med. 2017, 18, 10–14. [Google Scholar] [CrossRef]
- Russo, G.; Remonato, A.; Remonato, R.; Zanier, E. Hypnosis and Osteopathic Manipulative Treatment for Visual Disorders during Pregnancy: A Case Report. Adv. Mind. Body. Med. 2017, 31, 23–27. [Google Scholar] [PubMed]
- Urbanek, B. Osteopathic Care of a Twin Risk Pregnancy: Case Study. J. Spine 2015, 4, 254. [Google Scholar] [CrossRef]
- Hensel, K.L.; Buchanan, S.; Brown, S.K.; Rodriguez, M.; Cruser, D.A. Pregnancy Research on Osteopathic Manipulation Optimizing Treatment Effects: The PROMOTE study. Am. J. Obstet. Gynecol. 2014, 212, 108.e1–108.e9. [Google Scholar] [CrossRef] [PubMed]
- Hensel, K.L.; Roane, B.M.; Chaphekar, A.V.; Smith-Barbaro, P. PROMOTE Study: Safety of Osteopathic Manipulative Treatment during the Third Trimester by Labor and Delivery Outcomes. J. Osteopat. Med. 2016, 116, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Hensel, K.L.; Roane, B.M. Does Compression of the Fourth Ventricle Cause Preterm Labor? Analysis of Data from the PROMOTE Study. J. Osteopat. Med. 2019, 119, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Martingano, D.; Ho, S.; Rogoff, S.; Chang, G.; Aglialoro, G.C. Effect of Osteopathic Obstetrical Management on the Duration of Labor in the Inpatient Setting: A Prospective Study and Literature Review. J. Osteopat. Med. 2019, 119, 371–378. [Google Scholar] [CrossRef]
- Schwerla, F.; Rother, K.; Rother, D.; Ruetz, M.; Resch, K.-L. Osteopathic Manipulative Therapy in Women With Postpartum Low Back Pain and Disability: A Pragmatic Randomized Controlled Trial. J. Osteopat. Med. 2015, 115, 416–425. [Google Scholar] [CrossRef]
- Kirk, B.; Elliott-Burke, T. The effect of visceral manipulation on Diastasis Recti Abdominis (DRA): A case series. J. Bodyw. Mov. Ther. 2020, 26, 471–480. [Google Scholar] [CrossRef]
- Origo, D.; Tarantino, A. Osteopathic manipulative treatment in pudendal neuralgia: A case report. J. Bodyw. Mov. Ther. 2018, 23, 247–250. [Google Scholar] [CrossRef]
- Giovanis, A.; Zeszutek, S. Somatic Dysfunctions of Hip and Pelvis Overlooked in a Case of Vulvodynia. J. Osteopat. Med. 2020, 120, 792–795. [Google Scholar] [CrossRef] [PubMed]
- Daraï, C.; Bendifallah, S.; Foulot, H.; Ballester, M.; Chabbert-Buffet, N.; Daraï, E. Intérêt clinique du traitement ostéopathique chez les patientes ayant une endométriose colorectale: Classification fondée sur les symptômes et la qualité de vie. Gynécologie Obs. Fertil. Sénologie. 2017, 45, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Daraï, C.; Deboute, O.; Zacharopoulou, C.; Laas, E.; Canlorbe, G.; Belghiti, J.; Zilberman, S.; Ballester, M.; Daraï, E. Impact of osteopathic manipulative therapy on quality of life of patients with deep infiltrating endometriosis with colorectal involvement: Results of a pilot study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 188, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Sillem, M.; Juhasz-Böss, I.; Klausmeier, I.; Mechsner, S.; Siedentopf, F.; Solomayer, E. Osteopathy for Endometriosis and Chronic Pelvic Pain–a Pilot Study. Geburtshilfe Frauenheilkd. 2016, 76, 960–963. [Google Scholar] [CrossRef]
- Ott, S. Osteopathische Ansätze bei Endometriose. Osteopat. Med. 2017, 18, 4–9. [Google Scholar] [CrossRef]
- Goyal, K.; Narkeesh, K.; Samuel, A.J.; Sharma, S.; Chatterjee, S.; Arumugam, N. The effectiveness of osteopathic manipulative treatment in an abnormal uterine bleeding related pain and health related quality of life (HR-QoL)–A case report. J. Bodyw. Mov. Ther. 2016, 21, 569–573. [Google Scholar] [CrossRef]
- Matsushita, S.; Wong, B.; Kanumalla, R.; Goldstein, L. Osteopathic Manipulative Treatment and Psychosocial Management of Dysmenorrhea. J. Osteopat. Med. 2020, 120, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Origo, D.; Piloni, S.; Tarantino, A.G. Secondary dysmenorrhea and dyspareunia associated with pelvic girdle dysfunction: A case report and review of literature. J. Bodyw. Mov. Ther. 2021, 27, 165–168. [Google Scholar] [CrossRef]
- Schwerla, F.; Wirthwein, P.; Rütz, M.; Resch, K.-L. Osteopathic treatment in patients with primary dysmenorrhoea: A randomised controlled trial. Int. J. Osteopat. Med. 2014, 17, 222–231. [Google Scholar] [CrossRef]
- Davis, S.E.; Hendryx, J.; Menezes, C.; Bouwer, S.; Menezes, H.; Patel, V.; Smith, C.A.B.; Speelman, D.L. Weekly Osteopathic Manipulative Treatment to Improve Measures of Sympathetic Tone in Women With Polycystic Ovary Syndrome: A Randomized, Controlled Pilot Study. J. Osteopat. Med. 2020, 120, 310–321. [Google Scholar] [CrossRef]
- Noccioli, G. Randomized clinical trial on the effects of osteopathic treatment in menopausal women. G. Ital. Ostet. Ginecol. 2014, 36, 339–341. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Aryal, S. Prevention of Progressive Back-Specific Dysfunction during Pregnancy: An Assessment of Osteopathic Manual Treatment Based on Cochrane Back Review Group Criteria. J. Osteopat. Med. 2013, 113, 728–736. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Buchanan, S.; Hensel, K.L.; King, H.H.; Fulda, K.G.; Stoll, S.T. Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: A randomized controlled trial. Am. J. Obstet. Gynecol. 2010, 202, 43.e1–43.e8. [Google Scholar] [CrossRef]
- Guthrie, R.A.; Martin, R.H. Effect of pressure applied to the upper thoracic (placebo) versus lumbar areas (osteo-pathic manipulative treatment) for inhibition of lumbar myalgia during labor. J. Am. Osteopath. Assoc. 1982, 82, 247–251. [Google Scholar] [CrossRef]
- Smallwood, C.R.; Borgerding, C.J.; Cox, M.S.; Berkowitz, M.R. Osteopathic manipulative treatment (OMT) during labor facilitates a natural, drug-free childbirth for a primigravida patient: A case report. Int. J. Osteopat. Med. 2013, 16, 170–177. [Google Scholar] [CrossRef]
- Kermorgant, G. Osteopathie und Unfruchtbarkeit. Osteopat. Med. 2013, 14, 7–9. [Google Scholar] [CrossRef]
- Kramp, M.E. Combined manual therapy techniques for the treatment of women with infertility: A case series. J. Am. Osteopat. Assoc. 2012, 112, 680–684. [Google Scholar]
- Grimaldi, M. Le périnée douloureux sous toutes ses formes. Apport de la médecine manuelle et ostéopathie. J. Gynecol. Obs. Biol. Reprod 2008, 37, 449–456. [Google Scholar] [CrossRef]
- Cleary, C.; Fox, J.P. Menopausal symptoms: An osteopathic investigation. Complement. Ther. Med. 1994, 2, 181–186. [Google Scholar] [CrossRef]
- Molins-Cubero, S.; Rodríguez-Blanco, C.; Oliva-Pascual-Vaca, Á.; Heredia-Rizo, A.M.; Boscá-Gandía, J.J.; Ricard, F. Changes in Pain Perception after Pelvis Manipulation in Women with Primary Dysmenorrhea: A Randomized Controlled Trial. Pain Med. 2014, 15, 1455–1463. [Google Scholar] [CrossRef]
- Elden, H.; Ostgaard, H.-C.; Glantz, A.; Marciniak, P.; Linnér, A.-C.; Olsén, M.F. Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: A multicenter, single blind, randomized controlled trial. Acta Obstet. Gynecol. Scand. 2013, 92, 775–782. [Google Scholar] [CrossRef]
- King, H.H.; A Tettambel, M.; Lockwood, M.D.; Johnson, K.H.; A Arsenault, D.; Quist, R. Osteopathic manipulative treatment in prenatal care: A retrospective case control design study. J. Am. Osteopat. Assoc. 2003, 103, 577–582. [Google Scholar]
- Hensel, K.L.; Pacchia, C.F.; Smith, M.L. Acute improvement in hemodynamic control after osteopathic manipulative treatment in the third trimester of pregnancy. Complement. Ther. Med. 2013, 21, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Gitlin, R.S.; Wolf, D.L. Uterine contractions following osteopathic cranial manipulation—A pilot study. J. Am. Osteopath. Assoc. 1992, 92, 1183. [Google Scholar]
- Vernon, H.; MacAdam, K.; Marshall, V.; Pion, M.; Sadowska, M. Validation of a Sham Manipulative Procedure for the Cervical Spine for Use in Clinical Trials. J. Manip. Physiol. Ther. 2005, 28, 662–666. [Google Scholar] [CrossRef] [PubMed]
- Hancock, M.J.; Maher, C.G.; Latimer, J.; McAuley, J.H. Selecting an appropriate placebo for a trial of spinal manipulative therapy. Aust. J. Physiother. 2006, 52, 135–138. [Google Scholar] [CrossRef]
- Henley, C.E.; Wilson, T.E. Use of Beat-to-Beat Cardiovascular Variability Data to Determine the Validity of Sham Therapy as the Placebo Control in Osteopathic Manipulative Medicine Research. J. Osteopat. Med. 2014, 114, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Cerritelli, F.; Verzella, M.; Cicchitti, L.; D’Alessandro, G.; Vanacore, N. The paradox of sham therapy and placebo effect in osteopathy. Medicine 2016, 95, e4728. [Google Scholar] [CrossRef]


| Type of Study | New Studies Included in Current Review (N.) | Studies Included in the Previous Review (N.) | Total of Studies (N.) |
|---|---|---|---|
| Case report | 9 | 2 | 11 |
| Case series | 1 | 2 | 3 |
| Pilot prospective observational study | 2 | \ | 2 |
| Pilot study | 1 | \ | 1 |
| Prospective cohort study | 1 | \ | 1 |
| RCT | 7 | 6 | 13 |
| Controlled before–after study | \ | 1 | 1 |
| Controlled prospective study | \ | 1 | 1 |
| Observational Retrospective study | \ | 1 | 1 |
| Retrospective case-control | \ | 1 | 1 |
| Type of Clinical Condition | New Studies Included in This Review (N.) | Studies Included in the Previous Review (N.) | Total Studies (N.) |
|---|---|---|---|
| Pelvic pain | 1 | 1 | 2 |
| Vulvodynia | 1 | / | 1 |
| Dysmenorrhea | 3 | 2 | 5 |
| Endometriosis | 5 | / | 5 |
| PCOS | 1 | / | 1 |
| Infertility | / | 2 | 2 |
| Pregnancy | 4 | 5 | 9 |
| Labour | 3 | 3 | 6 |
| Post-partum | 2 | / | 2 |
| Menopause | 1 | 1 | 2 |
| Guthrie 1982 [48] | Cleary 1994 [58] | Licciardone 2010 [59] | Licciardone2013 [56] | Hensel 2013 [60] | Elden 2013 [53] | Molins-Cubero 2014 [61] | Schwerla 2014 [45] | Noccioli 2014 [47] | Hensel 2015 [30] | Schwerla 2015 [34] | Hensel 2016 [31] | Hensel 2019 [32] | Davis 2020 [46] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Review | Old | Old | Old | Old | Old | Old | Old | New | New | New | New | New | New | New |
| RoB, 2011 | High | Low/ Moderate | Moderate | High | Unclear | Low | Low | NA | NA | NA | NA | NA | NA | NA |
| RoB, 2019 | Some concerns | Low | Some concerns | Low | High | Low | Low | Low | Low | Low | Low | Low | High | Low |
| Score for Each Question | Tot. | Overall Judgement | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |||
| King et al., 2003 [57] | 2 | 1 | 0 | 2 | 0 | 2 | 2 | 0 | 1 | 2 | 1 | 2 | 15 | Moderate |
| Grimaldi et al., 2008 [49] | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | NA | NA | NA | NA | 8 | Poor |
| Kramp et al., 2012 [55] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | NA | NA | NA | NA | 14 | Moderate |
| Schorpp et al., 2013 [50] | 2 | 1 | 2 | 1 | 0 | 2 | 2 | 0 | NA | NA | NA | NA | 10 | Moderate |
| Kermorgant et al. 2013 [51] | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | NA | NA | NA | NA | 13 | Moderate |
| Noccioli et al., 2014 [47] | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 1 | 1 | 2 | 2 | 1 | 16 | Moderate |
| Darai et al., 2015 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | 0 | NA | NA | NA | NA | 7 | Poor |
| Sillem et al., 2016 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | NA | NA | NA | NA | 4 | Poor |
| Darai et al., 2017 [38] | 2 | 2 | 2 | 2 | 0 | 0 | 1 | 0 | NA | NA | NA | NA | 9 | Moderate |
| Martingano et al., 2019 [33] | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 21 | Moderate |
| Kirk et al., 2021 [35] | 2 | 2 | 2 | 2 | 1 | 0 | 0 | 0 | NA | NA | NA | NA | 9 | Moderate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruffini, N.; D’Alessandro, G.; Pimpinella, A.; Galli, M.; Galeotti, T.; Cerritelli, F.; Tramontano, M. The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review. Healthcare 2022, 10, 1566. https://doi.org/10.3390/healthcare10081566
Ruffini N, D’Alessandro G, Pimpinella A, Galli M, Galeotti T, Cerritelli F, Tramontano M. The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review. Healthcare. 2022; 10(8):1566. https://doi.org/10.3390/healthcare10081566
Chicago/Turabian StyleRuffini, Nuria, Giandomenico D’Alessandro, Annalisa Pimpinella, Matteo Galli, Tiziana Galeotti, Francesco Cerritelli, and Marco Tramontano. 2022. "The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review" Healthcare 10, no. 8: 1566. https://doi.org/10.3390/healthcare10081566
APA StyleRuffini, N., D’Alessandro, G., Pimpinella, A., Galli, M., Galeotti, T., Cerritelli, F., & Tramontano, M. (2022). The Role of Osteopathic Care in Gynaecology and Obstetrics: An Updated Systematic Review. Healthcare, 10(8), 1566. https://doi.org/10.3390/healthcare10081566






