Leveraging mHealth and Wearable Sensors to Manage Alcohol Use Disorders: A Systematic Literature Review
Abstract
:1. Rationale
2. Objectives
3. Methods
3.1. Eligibility Criteria
3.2. Information Sources
3.3. Search Strategy
3.4. Selection Process
3.5. Data Collection Process
3.6. Data Items
3.7. Study Risk of Bias Assessment
3.8. Effect Measures
3.9. Synthesis Methods
3.10. Reporting Bias Assessment
3.11. Additional Analyses and Certainty Assessment
4. Results
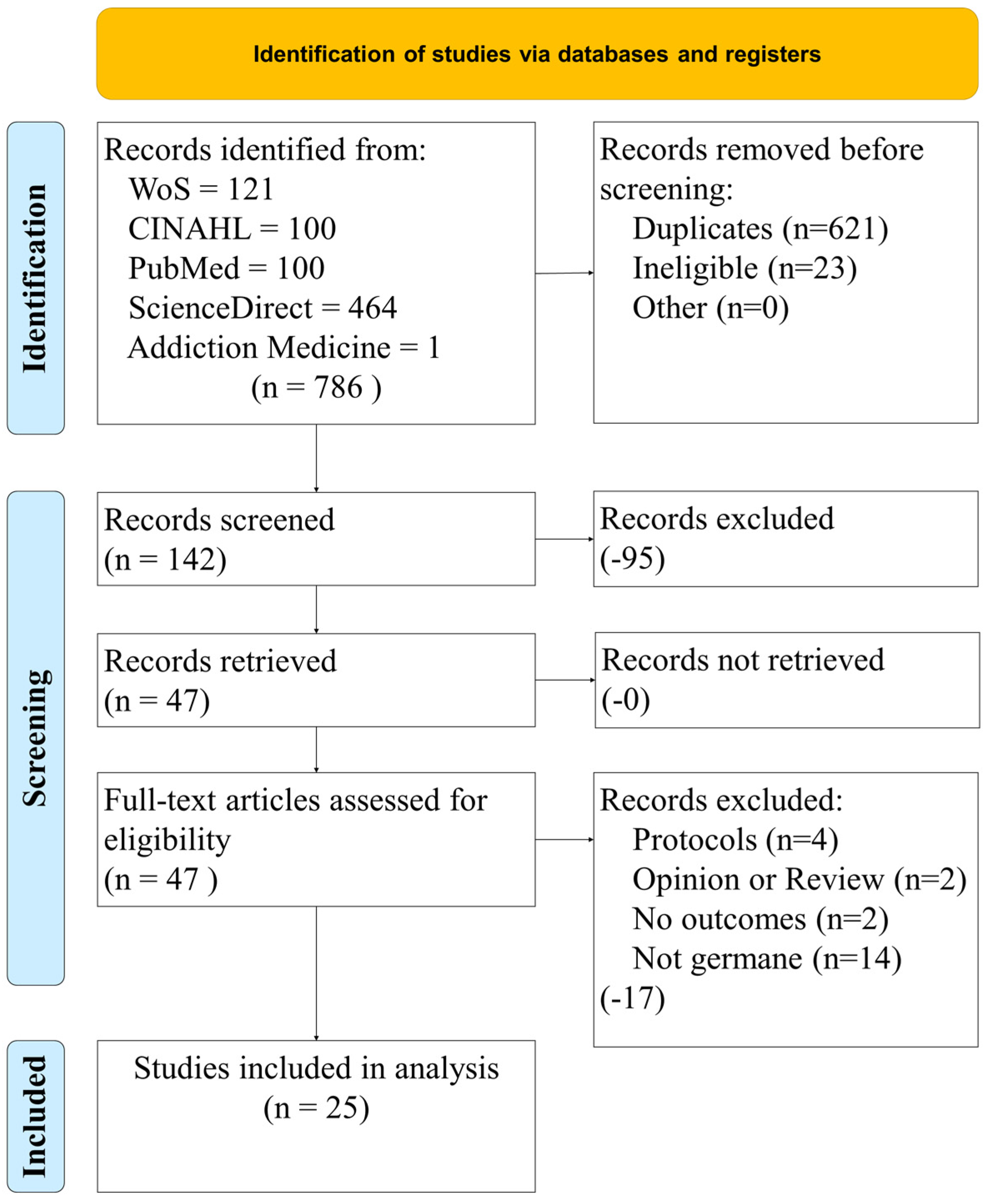
4.1. Study Selection
4.2. Study Characteristics
4.3. Risk of Bias within and across Studies
4.4. Results of Individual Studies
4.5. Results of Syntheses
4.6. Additional Analysis and Certainty of Evidence
4.6.1. Patient Satisfaction
4.6.2. Results of Studies
Medical Outcome Commensurate with the Use of mHealth
Effectiveness Themes and Observations
Barriers to the Adoption of mHealth and Wearable Sensors to Manage AUD
Interactions between Observations
5. Discussion
5.1. Summary of Evidence
5.2. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Authors | Experimental Intervention | Intervention Theme | Results | Results Themes | Medical Outcomes Reported | Medical Outcomes Themes |
|---|---|---|---|---|---|---|
| McTavish et al. [17] | mHealth app to control SUD and AUD | mHealth app | 94% used the app 1st week, and 80% used continued to use at week 16 | Good retention | Participants with AUD will use an app to manage their condition, App decreased cravings | Reduction in cravings |
| Murray et al. [18] | mHealth app Down Your Drink (DYD) | mHealth app | No control group. Of those still using the app at 12 months, the reduction in drinking was 35 units | Reduction in consumption | Reduction in consumption, reduction in AUD identification test, reduction in Leeds Dependence Questionnaire (LDQ, dependence), no significant change in Clinical Outcomes in Routine Evaluation (CORE-10, mental health) or EQ-5D (quality of life). | Reduction in consumption |
| Improvement in dependence | ||||||
| No significant difference in treatment outcomes | ||||||
| Morgan et al. [19] | mHealth Internet-based app | mHealth app | Internet-based recruitment to mental health interventions is feasible | High rates of acceptance | Improved rates of depression using intervention | Improved rates of depression |
| Chih et al. [20] | mHealth (A-CHESS) and BN | mHealth app | No control group. Responses to weekly check in on A-CHESS can be a predictor of relapse | Computer models can predict relapse | The prediction of lapse in sobriety gives counselors the chance to intervene through text, email, or phone call | With prediction of relapse, providers can intervene |
| Kalapatapu et al. [21] | telephone | Telephone/Interactive voice response | Face-to-face cognitive based therapy (CBT) and T-CBT groups were similar on all treatment adherence outcomes and depression outcomes at all time points | No significant difference in treatment outcomes | telehealth means of treating is equally as effective as traditional therapy | No significatn difference in treatment outcomes |
| Stoner et al. [22] | mHealth SMS | mHealth SMS | Adequate adherence ≥80% at week 8, not statistically significant between groups | No significant difference in treatment outcomes | SMS messages do not improve medication adherence, but equally as effective as traditional treatment to reduce consumption | No significant difference in treatment outcomes |
| Bock et al. [23] | mHealth SMS, text-message alcohol program (TMAP) | mHealth SMS | At week 6–12, TMAP participants less likely to report heavy drinking and negative alcohol consequences. Increased self-efficacy to resist drinking. | Reduction in consumption | SMS effective at reducing consumption and increasing self-efficacy | Reduction in consumption |
| Increased self-efficacy | Increased self-efficacy | |||||
| Freyer-Adam et al. [24] | mHealth Internet-based app | mHealth app | reached individuals and helped retain them in AUD programs | Good retention | Not reported | Not reported |
| Gamito et al. [25] | mHealth cognitive stimulation program (CSP) serious games | mHealth serious games/cognitive training | Cognitive ability between groups not statistically significant, but frontal-lobe function (Frontal Lobe Assessment, FAB) was significantly improved in the intervention group | Positive frontal lobe function (FAB) | Improvement in FAB with mHealth intervention | Increased frontal lobe function |
| Barrio et al. [26] | mHealth app, SIDEAL | mHealth app | Reduced binge drinking and mean daily consumption, participants achieved their self-imposed objectives | Decreased binge drinking | Significant reduction in alcohol consumption` | Reduction in consumption |
| Reduction in consumption | ||||||
| Gajecki et al. [27] | mHealth app (skills training) | mHealth serious games/cognitive training | Reduced binge drinking and mean daily consumption, participants achieved their self-imposed objectives | Decreased binge drinking | Reduced alcohol consumption | Reduction in consumption |
| Reduction in consumption | ||||||
| Glass et al. [28] | mHealth app (A-CHESS) | mHealth app | Intervention showed increased odds of outpatient addiction treatment across follow-ups, but not mutual help | Good retention | Reduced alcohol consumption, increased treatment | Reduction in consumption |
| Increased motivation to change | ||||||
| Rose et al. [29] | interactive voice response (IVR) brief intervention (BI) | Telephone/Interactive voice response | Reduced alcohol consumption, but not statistically different than control | No significant difference in treatment outcomes | Reduced alcohol consumption | Reduction in consumption |
| Jo et al. [30] | mHealth (online-based brief empowerment for alcohol-use monitor, on-BEAM) | mHealth app | intervention group reported consuming less alcohol during the past week and lower AUDIT score | Reduction in consumption | Reduced alcohol consumption | Reduction in consumption |
| Increased self-efficacy | Increased self-efficacy | |||||
| Mellentin et al. [31] | mHealth (cue exposure) | mHealth serious games/cognitive training | No differences were detected between the two experimental CET groups on any outcomes | No significant difference in treatment outcomes | Reduced alcohol consumption | Reduction in consumption |
| Harder et al. [32] | mHealth (motivational interviewing) | Telephone/Interactive voice response | Average AUDIT scores were lower for the intervention group | Reduction in consumption | Reduced alcohol consumption, increased self-efficacy | Reduction in consumption |
| Increased self-efficacy | Increased self-efficacy | |||||
| Hendershot et al. [33] | mHealth feedback, opiod receptor gene (OPRM1) | mHealth app | OPRM1 genotype moderated the association of daily adherence with reduced same-day consumption (p = 0.007) and craving (p = 0.06), with these associations being stronger for participants with the 118 G variant. OPRM1 genotype did not moderate changes in craving and consumption over time. | Reduction in consumption | high-density assessments and person-centered analytic approaches, including modeling within-person variation in medication adherence, could be advantageous for pharmacogenetic studies. | Reduction in consumption |
| No significant difference in treatment outcomes | Increased medication compliance | |||||
| Constant et al. [34] | telephone | Telephone/Interactive voice response | Study group had better alcohol abstinence rates than control | Reduction in consumption | Intervention improves patient coping skills and motivation to modify alcohol use behaviors | Reduction in consumption |
| Increased motivation to change | ||||||
| Graser et al. [35] | telephone and smartphone-based intervention | mHealth + telephone | Telephone-based intervention was more effective than text-based intervention | Reduction in consumption | Sustained abstinence from excessive drinking occurred in telephone intervention group | Reduction in consumption |
| Hammond et al. [36] | mHealth app | mHealth app | Intervention group utilized mobile app more effectively than control group | Reduction in consumption | Complemented community substance use intervention programs | Reduction in consumption |
| Manning et al. [37] | mHealth app | mHealth app | No control group. Participants reduced alcohol consumption rates | Reduction in consumption | Improved alcohol consumption rates | Reduction in consumption |
| Howe et al. [38] | mHealth app | mHealth app | No control group. Use of mobile app improved decision making of study group participants | Reduction in consumption | Mobile data collection can positively influence drinking decisions | Reduction in consumption |
| Increased motivation to change | ||||||
| Leightley et al. [39] | mHealth app | mHealth app | Use of mobile app reduced rate of alcohol consumption among Veterans in study group | Reduction in consumption | Reduced rates of alcohol consumption | Reduction in consumption |
| McKay et al. [40] | telephone and smartphone-based intervention | mHealth + telephone | Use of telephone or smartphone was effective in treating AUD | Reduction in consumption | Improved rates of alcohol dependent persons | Reduction in consumption |
| O’Grady et al. [41] | mHealth app | mHealth app | Provider-facing technology is effective alcohol intervention services and increase access to care in low- and middle-income countries. | Reduction in consumption | Improved rates in alcohol dependent persons | Reduction in consumption |
Appendix B
| Authors | Measures of Effectiveness | Effectiveness Themes | Barriers to Adoption | Barrier Themes |
|---|---|---|---|---|
| McTavish et al. [17] | Low cost intervention, good acceptance, decreased cravings, increased autonomy and self-determination | Low cost | Must train users | Must train users |
| Good acceptance | ||||
| Decreased consumption/cravings | ||||
| Increased self-efficacy/self-determination | ||||
| Murray et al. [18] | Low operation cost (120/mo), effective at reducing consumption | Low cost | High setup cost (3200), must train users | Cost |
| Decreased consumption/cravings | Must train users | |||
| Equally as effective as traditional care (preference) | ||||
| Good acceptance | ||||
| Morgan et al. [19] | Improved rates of depression | Decreased depression symptoms | Must have access to internet, average cost of AUD $12 per participant | Computer literacy/access to Internet |
| Cost | ||||
| Chih et al. [20] | Effective at predicting relapse | Can predict relapse and enable intervention | Must train users | Must train users |
| Kalapatapu et al. [21] | Effective at treating | Decreased consumption/cravings | none | Equally as effective, so change may not be necessary |
| Equally as effective as traditional care (preference) | ||||
| Stoner et al. [22] | Equally as effective at reducing consumption | Decreased consumption/cravings | Equally as effective, but expensive (unnecessarily) | Equally as effective, so change may not be necessary |
| Equally as effective as traditional care (preference) | Cost | |||
| Bock et al. [23] | SMS effective at reducing consumption and increasing self-efficacy | Decreased consumption/cravings | Must train users | Must train users |
| Increased self-efficacy/self-determination | ||||
| Freyer-Adam et al. [24] | Educates participants and increases retention in programs | Educates | Must train users, computer literacy | Must train users |
| Increased retention in treatment program | ||||
| Gamito et al. [25] | Improved FAB indicates greater frontal-lobe activity, which could decrease alcohol addiction | Increased frontal lobe function | Must train users | Must train users |
| Barrio et al. [26] | Effective at reducing consumption | Decreased consumption/cravings | Must train users | Must train users |
| Increased self-efficacy/self-determination | ||||
| Gajecki et al. [27] | Effective at reducing consumption | Decreased consumption/cravings | Must train users | Must train users |
| Increased self-efficacy/self-determination | ||||
| Glass et al. [28] | Effective at reducing consumption, effective at increasing treatment participation | Decreased consumption/cravings | Must train users | Must train users |
| Increased retention in treatment program | ||||
| Rose et al. [29] | Equally as effective at reducing consumption | Decreased consumption/cravings | Equally as effective, but expensive (unnecessarily), must train users | Cost |
| Equally as effective, so change may not be necessary | ||||
| Must train users | ||||
| Jo et al. [30] | Reduced alcohol consumption, improved self-efficacy | Decreased consumption/cravings | Must train users | Must train users |
| Increased self-efficacy/self-determination | ||||
| Mellentin et al. [31] | Equally as effective at reducing consumption | Decreased consumption/cravings | Equally as effective, but expensive (unnecessarily), must train users | Equally as effective, so change may not be necessary |
| Must train users | ||||
| Harder et al. [32] | Reduced alcohol consumption, increased self-efficacy | Decreased consumption/cravings | Must train users | Must train users |
| Increased self-efficacy/self-determination | ||||
| Hendershot et al. [33] | increased medication adherence, decreased consumption, decreased cravings | Increased medication compliance | Must train users | Must train users |
| Equally as effective as traditional care (preference) | ||||
| Decreased consumption/cravings | ||||
| Constant et al. [34] | Sustained abstinence from excessive drinking | Decreased consumption/cravings | Must train users Must sustain intervention repeated for best results | Must train users |
| Increased self-efficacy/self-determination | Must sustain intervention for long-term results | |||
| Sustained abstinence from drinking | ||||
| Graser et al. [35] | Sustained abstinence from excessive drinking | Decreased consumption/cravings | Must train users | Must train users |
| Sustained abstinence from drinking | ||||
| Hammond et al. [36] | Reinforced positive behaviors | Increased self-efficacy/self-determination | Must train users | Must train users |
| Manning et al. [37] | Reduced alcohol consumption | Decreased consumption/cravings | Must train users | Must train users |
| Howe et al. [38] | Improved decision making of alcohol users | Increased self-efficacy/self-determination | Must train users Must possess smartphone | Must train users |
| Decreased consumption/cravings | ||||
| Leightley et al. [39] | Reduced alcohol consumption rates | Decreased consumption/cravings | Must train users | Must train users |
| McKay et al. [40] | Improved rates of alcohol dependent persons | Increased self-efficacy/self-determination | Must train users | Must train users |
| Decreased consumption/cravings | ||||
| O’Grady et al. [41] | Improved rates of alcohol dependent persons, increased access | Increased self-efficacy/self-determination | Must have access to internet; time constraints on provider workload | Computer literacy/access to Internet |
| Decreased consumption/cravings | Impacts provider workload | |||
| Increased access to care | Must train users |
Appendix C
| Authors | Sample Size (#s Only) | Bias within Study (See Article) Selection Bias, Sample Bias, etc. | Effect Size (Small, Medium, or Large with Cohen’s d Statistic) Sensitivity, Specificity, F1 | Country of Origin (Where Was the Study Conducted?) | Statistics Used | Strength of Evidence | Quality of Evidence |
|---|---|---|---|---|---|---|---|
| McTavish et al. [17] | 349 | One region of one country (selection bias), mostly Caucasian males (sample bias) | not reported | USA | Measures of central tendency, Descriptive Statistics | I | A |
| Murray et al. [18] | 19 | One region of one country (selection bias) | not reprted | UK | Measures of central tendency, Descriptive Statistics | III | B |
| Morgan et al. [19] | 1326 | One region of one country (selection bias) | small effect size | Australia | Descriptive statistics | I | A |
| Chih et al. [20] | 152 | One region of one country (selection bias), 81% Caucasian (sample bias) | sensitivity (prediction of true lapse) at >4–6% 75% (21/28), specificity (prediction of non-lapse) at >4–6% 88% (234/266) | USA | Bayesian Network Model | III | A |
| Kalapatapu et al. [21] | 103 | One region of one country (selection bias), 87% female (sample bias) | not reported | USA | Kolmogorov–Smirnov and Shapiro–Wilk tests (normality), Levene’s test (homogeneity of variance), non-parametric tests (continuous variables), chi-square and Fisher’s exact tests (categorical variables), Wilcoxon signed-rank test (change in AUDIT) score from baseline to end of treatment. | I | A |
| Stoner et al. [22] | 76 | One region of one country (selection bias), mostly male (sample bias) | w = 0.32 | USA | t-test, chi-square test, and ANCOVA | I | A |
| Bock et al. [23] | 60 | One region of one country (selection bias), mostly female (sample bias) | Magnitude of effect ranged from small to large (d+ = 0.46–0.62; 12-week follow-up: d+ = 0.13–0.35). | USA | chi-square test and ANOVA | I | A |
| Freyer-Adam et al. [24] | 961 | One region of one country (selection bias) | not reported | Germany | Descriptive statistics, measures of central tendency, multivariate logistic regression analysis, t-test | I | A |
| Gamito et al. [25] | 42 | One region of one country (selection bias), mostly male (sample bias) | medium effect (0.30) | Portugal | ANCOVA, t-tests | I | A |
| Barrio et al. [26] | 24 | One region of one country (selection bias) | not reported | Spain | Measures of central tendency, Descriptive Statistics, paired t-tests and chi-square tests | III | B |
| Gajecki et al. [27] | 144 | One region of one country (selection bias), mostly female (sample bias) | not reported | Sweden | ANOVA | I | A |
| Glass et al. [28] | 349 | One region of one country (selection bias) | not reported | USA | Measures of central tendency, descriptive statistics, logistic models, mixed effects models, chi-square | I | A |
| Rose et al. [29] | 1855 | One region of one country (selection bias) | not reported | USA | chi square, t-tests and Wilcoxon Rank Sum tests | I | A |
| Jo et al. [30] | 1496 | One region of one country (selection bias) | alcohol consumption (d = 0.24), binge drinking (d = 0.29), total AUDIT-K score (d = 0.34) | Korea | t-test or chi-square test | I | A |
| Mellentin et al. [31] | 164 | One region of one country (selection bias) | not reported | Denmark | Generalized mixed models | I | A |
| Harder et al. [32] | 230 | One region of one country (selection bias) | sensitivity = 0.86; specificity = 0.72 | Kenya | Multiple linear regression | I | A |
| Hendershot et al. [33] | 76 | One region of one country (selection bias) | not reported | USA | Multi-level modeling and multi-level structural equation modeling | III | A |
| Constant et al. [34] | 799 | Multiple regions of one country (selection bias) | not reported | Brazil | logistic regression and chi-square | I | A |
| Graser et al. [35] | 240 | One region of one country (selection bias) | not reported | USA | Descriptive statistics | I | A |
| Hammond et al. [36] | 61 | One region of one country (selection bias) | d = 0.26 (small) | USA | Descriptive statistics, t-test | I | A |
| Manning et al. [37] | 1309 | One region of one country (selection bias) | not reported | Australia | Descriptive statistics | I | A |
| Howe et al. [38] | 104 | One region of one country (selection bias), mostly young adults median age 20 yrs old (sample bias) | not reported | USA | Descriptive statistics | I | A |
| Leightley et al. [39] | 123 | One region of one country (selection bias), mostly Veteran males (sample bias) | Cohen d = 0.5 (medium effect) | UK | Descriptive statistics | I | A |
| McKay et al. [40] | 262 | One region of one country (selection bias), mostly African American males (sample bias) | PDHD lower in TMC (d = 0.35, medium), A-CHESS (d = 0.31, medium), TMC + A-CHESS (d = 0.36, medium), differences between groups small (d ≤ 0.06, small) | USA | Descriptive statistics | I | A |
| O’Grady et al. [41] | 60 | Selection bias | not reported | USA | Descriptive statistics | I | A |
References
- National Institute on Alcohol Abuse and Alcoholisma. Understanding Alcohol Abuse Disorder. Available online: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder (accessed on 1 August 2022).
- Manthey, J.; Gual, A.; Jakubczyk, A.; Pieper, L.; Probst, C.; Struzzo, P.; Trapencieris, M.; Wojnar, M.; Rehm, J. Alcohol use disorders in Europe: A comparison of general population and primary health care prevalence rates. J. Subst. Use 2016, 21, 478–484. [Google Scholar] [CrossRef]
- World Health Organization. Status Report on Alcohol Consumption, Harm and Policy Responses in 30 European Countries 2019; World Health Organization Regional Office for Europe: København, Denmark, 2019. [Google Scholar]
- Buono, F.D.; Gleed, C.; Boldin, M.; Aviles, A.; Wheeler, N. Preliminary Effectiveness of a Remotely Monitored Blood Alcohol Concentration Device as Treatment Modality: Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2022, 11, e30186. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Telemedicine: Opportunities and Developments in Member States. Report on the Second Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2010.
- Davis-Martin, R.E.; Alessi, S.M.; Boudreaux, E.D. Alcohol use disorder in the age of technology: A review of wearable biosensors in alcohol use disorder treatment. Front. Psychiatry 2021, 12, 642813. [Google Scholar] [CrossRef] [PubMed]
- Lansdorp, B.; Ramsay, W.; Hamid, R.; Strenk, E. Wearable enzymatic alcohol biosensor. Sensors 2019, 19, 2380. [Google Scholar] [CrossRef]
- Goldfine, C.; Lai, J.T.; Lucey, E.; Newcomb, M.; Carreiro, S. Wearable and wireless mHealth technologies for substance use disorder. Curr. Addict. Rep. 2020, 7, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Carreiro, S.; Newcomb, M.; Leach, R.; Ostrowski, S.; Boudreaux, E.D.; Amante, D. Current reporting of usability and impact of mHealth interventions for substance use disorder: A systematic review. Drug Alcohol Depend. 2020, 215, 108201. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Lee, K.; Watson, J.B.; Lobo, L.G.; Stoppelmoor, A.G.; Oyibo, S.E. Measures of effectiveness, efficiency, and quality of telemedicine in the management of alcohol abuse, addiction, and rehabilitation: Systematic review. J. Med. Internet Res. 2020, 22, e13252. [Google Scholar] [CrossRef]
- Kruse, C.S. Writing a Systematic Review for Publication in a Health-Related Degree Program. JMIR Res. Protoc. 2019, 8, e15490. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Newhouse, R.; Dearholt, S.; Poe, S.; Pugh, L.; White, K. The Johns Hopkins Nursing Evidence-Based Practice Rating Scale; The Johns Hopkins Hospital: Baltimore, MD, USA, 2005. [Google Scholar]
- Pannucci, C.J.; Wilkins, E.G. Identifying and avoiding bias in research. Plast. Reconstr. Surg. 2010, 126, 619. [Google Scholar] [CrossRef]
- Light, R.J. Measures of response agreement for qualitative data: Some generalizations and alternatives. Psychol. Bull. 1971, 76, 365. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- McTavish, F.M.; Chih, M.-Y.; Shah, D.; Gustafson, D.H. How Patients Recovering From Alcoholism Use a Smartphone Intervention. J. Dual Diagn. 2012, 8, 294–304. [Google Scholar] [CrossRef]
- Murray, E.; Linke, S.; Harwood, E.; Conroy, S.; Stevenson, F.; Godfrey, C. Widening Access to Treatment for Alcohol Misuse: Description and Formative Evaluation of an Innovative Web-Based Service in One Primary Care Trust. Alcohol Alcohol. 2012, 47, 697–701. [Google Scholar] [CrossRef] [PubMed]
- Morgan, A.J.; Jorm, A.F.; Mackinnon, A.J. Internet-based recruitment to a depression prevention intervention: Lessons from the Mood Memos study. J. Med. Internet Res. 2013, 15, e2262. [Google Scholar] [CrossRef]
- Chih, M.-Y.; Patton, T.; McTavish, F.M.; Isham, A.J.; Judkins-Fisher, C.L.; Atwood, A.K.; Gustafson, D.H. Predictive modeling of addiction lapses in a mobile health application. J. Subst. Abus. Treat. 2014, 46, 29–35. [Google Scholar] [CrossRef]
- Kalapatapu, R.K.; Ho, J.; Cai, X.; Vinogradov, S.; Batki, S.L.; Mohr, D.C. Cognitive-behavioral therapy in depressed primary care patients with co-occurring problematic alcohol use: Effect of telephone-administered vs. Face-to-face treatment—A secondary analysis. J. Psychoact. Drugs 2014, 46, 85–92. [Google Scholar] [CrossRef]
- Stoner, S.A.; Arenella, P.B.; Hendershot, C.S. Randomized controlled trial of a mobile phone intervention for improving adherence to naltrexone for alcohol use disorders. PLoS ONE 2015, 10, e0124613. [Google Scholar] [CrossRef]
- Bock, B.C.; Barnett, N.P.; Thind, H.; Rosen, R.; Walaska, K.; Traficante, R.; Foster, R.; Deutsch, C.; Fava, J.L.; Scott-Sheldon, L.A. A text message intervention for alcohol risk reduction among community college students: TMAP. Addict. Behav. 2016, 63, 107–113. [Google Scholar] [CrossRef]
- Freyer-Adam, J.; Baumann, S.; Haberecht, K.; Tobschall, S.; Schnuerer, I.; Bruss, K.; Bandelin, E.; John, U.; Gaertner, B. In-person and computer-based alcohol interventions at general hospitals: Reach and retention. Eur. J. Public Health 2016, 26, 844–849. [Google Scholar] [CrossRef] [Green Version]
- Gamito, P.; Oliveira, J.; Lopes, P.; Brito, R.; Morais, D.; Rebelo, S.; Silva, D.; Caçôete, C.; Deus, A. Cognitive stimulation through mHealth-based program for patients with alcohol dependence syndrome: A randomized controlled study. J. Pain Manag. 2016, 9, 235–241. [Google Scholar]
- Barrio, P.; Ortega, L.; López, H.; Gual, A. Self-management and Shared Decision-Making in Alcohol Dependence via a Mobile App: A Pilot Study. Int. J. Behav. Med. 2017, 24, 722–727. [Google Scholar] [CrossRef]
- Gajecki, M.; Andersson, C.; Rosendahl, I.; Sinadinovic, K.; Fredriksson, M.; Berman, A.H. Skills training via smartphone app for university students with excessive alcohol consumption: A randomized controlled trial. Int. J. Behav. Med. 2017, 24, 778–788. [Google Scholar] [CrossRef]
- Glass, J.E.; McKay, J.R.; Gustafson, D.H.; Kornfield, R.; Rathouz, P.J.; McTavish, F.M.; Atwood, A.K.; Isham, A.; Quanbeck, A.; Shah, D. Treatment seeking as a mechanism of change in a randomized controlled trial of a mobile health intervention to support recovery from alcohol use disorders. J. Subst. Abus. Treat. 2017, 77, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Rose, G.L.; Badger, G.J.; Skelly, J.M.; MacLean, C.D.; Ferraro, T.A.; Helzer, J.E. A randomized controlled trial of brief intervention by interactive voice response. Alcohol Alcohol. 2017, 52, 335–343. [Google Scholar] [CrossRef]
- Jo, S.J.; Lee, H.K.; Kang, K.; Joe, K.H.; Lee, S.B. Efficacy of a Web-Based Screening and Brief Intervention to Prevent Problematic Alcohol Use in Korea: Results of a Randomized Controlled Trial. Alcohol. Clin. Exp. Res. 2019, 43, 2196–2202. [Google Scholar] [CrossRef]
- Mellentin, A.I.; Nielsen, B.; Nielsen, A.S.; Yu, F.; Mejldal, A.; Nielsen, D.G.; Stenager, E. A Mobile Phone App Featuring Cue Exposure Therapy As Aftercare for Alcohol Use Disorders: An Investigator-Blinded Randomized Controlled Trial. JMIR Mhealth Uhealth 2019, 7, e13793. [Google Scholar] [CrossRef]
- Harder, V.S.; Musau, A.M.; Musyimi, C.W.; Ndetei, D.M.; Mutiso, V.N. A randomized clinical trial of mobile phone motivational interviewing for alcohol use problems in Kenya. Addiction 2020, 115, 1050–1060. [Google Scholar] [CrossRef]
- Hendershot, C.S.; Dermody, S.S.; Wardell, J.D.; Zaso, M.J.; Kennedy, J.L.; Stoner, S.A. OPRM1 Moderates Daily Associations of Naltrexone Adherence With Alcohol Consumption: Preliminary Evidence From a Mobile Health Trial. Alcohol. Clin. Exp. Res. 2020, 44, 983–991. [Google Scholar] [CrossRef]
- Constant, H.M.R.M.; Ferigolo, M.; Barros, H.M.T.; Moret-Tatay, C. A clinical trial on a brief motivational intervention in reducing alcohol consumption under a telehealth supportive counseling. Psychiatry Res. 2021, 303, 114068. [Google Scholar] [CrossRef]
- Graser, Y.; Stutz, S.; Rösner, S.; Moggi, F.; Soravia, L.M. Telephone-and Text Message–Based Continuing Care After Residential Treatment for Alcohol Use Disorder: A Randomized Clinical Multicenter Study. Alcohol. Clin. Exp. Res. 2021, 45, 224–233. [Google Scholar] [CrossRef]
- Hammond, A.S.; Sweeney, M.M.; Chikosi, T.U.; Stitzer, M.L. Digital delivery of a contingency management intervention for substance use disorder: A feasibility study with DynamiCare Health. J. Subst. Abuse Treat. 2021, 126, 108425. [Google Scholar] [CrossRef]
- Manning, V.; Piercy, H.; Garfield, J.B.B.; Clark, S.G.; Andrabi, M.N.; Lubman, D.I. A Personalized Approach Bias Modification Smartphone App (“SWiPE”) to Reduce Alcohol Use: Open-Label Feasibility, Acceptability, and Preliminary Effectiveness Study. JMIR Mhealth Uhealth 2021, 9, e31353. [Google Scholar] [CrossRef]
- Howe, L.K.; Copeland, S.; Fisher, L.; Farmer, E.; Nemes, L.; Finn, P.R. Mobile assessment of decisions to drink in young adults: Examining the role of incentives and disincentives. Alcohol. Clin. Exp. Res. 2022, 46, 152–165. [Google Scholar] [CrossRef]
- Leightley, D.; Williamson, C.; Rona, R.J.; Carr, E.; Shearer, J.; Davis, J.P.; Simms, A.; Fear, N.T.; Goodwin, L.; Murphy, D. Evaluating the Efficacy of the Drinks: Ration Mobile App to Reduce Alcohol Consumption in a Help-Seeking Military Veteran Population: Randomized Controlled Trial. JMIR Mhealth Uhealth 2022, 10, e38991. [Google Scholar] [CrossRef]
- McKay, J.R.; Gustafson, D.H.; Ivey, M.; Pe-Romashko, K.; Curtis, B.; Thomas, T.; Oslin, D.W.; Polsky, D.; Quanbeck, A.; Lynch, K.G. Efficacy and comparative effectiveness of telephone and smartphone remote continuing care interventions for alcohol use disorder: A randomized controlled trial. Addiction 2022, 117, 1326–1337. [Google Scholar] [CrossRef]
- O’Grady, M.A.; Mootz, J.; Suleman, A.; Sweetland, A.; Teodoro, E.; Anube, A.; Feliciano, P.; Bezuidenhout, C.; Dos Santos, P.F.; Fumo, W. Mobile technology and task shifting to improve access to alcohol treatment services in Mozambique. J. Subst. Abus. Treat. 2022, 134, 108549. [Google Scholar] [CrossRef]

| Authors | Participants | Experimental Intervention | Results | Medical Outcomes Reported | Study Design (See the List Below) |
|---|---|---|---|---|---|
| McTavish et al. [17] | Adults, average age 38.3, 60.6% male, 82.9% Caucasian | mHealth app to control SUD and AUD | 94% used the app 1st week, and 80% used continued to use at week 16 | Participants with AUD will use an app to manage their condition, App decreased cravings | True experiment |
| Murray et al. [18] | Adults ≥ 18, affluent area outside of London | mHealth app Down Your Drink (DYD) | No control group. Of those still using the app at 12 month, the reduction in drinking was 35 units | Reduction in consumption, reduction in AUD identification test, reduction in Leeds Dependence Questionnaire (LDQ, dependence), no significant change in Clinical Outcomes in Routine Evaluation (CORE-10, mental health) or EQ-5D (quality of life). | Mixed-Methods |
| Morgan et al. [19] | Adults ≥ 18 | mHealth Internet-based app | Internet-based recruitment to mental health interventions is feasible | Improved rates of depression using intervention | RCT |
| Chih et al. [20] | Adults ≥ 18, average age 38, 62% male, 83% Caucasian | mHealth (A-CHESS) and BN | No control group. Responses to weekly check-in on A-CHESS can be a predictor of relapse | The prediction of lapse in sobriety gives counselors the chance to intervene through text, email, or phone call | Qualitative |
| Kalapatapu et al. [21] | Adults ≥ 18, average age 43.7, 87% female | telephone | Face-to-face cognitive based therapy (CBT) and T-CBT groups were similar on all treatment adherence outcomes and depression outcomes at all time points | telehealth means of treating is equally as effective as traditional therapy | True experiment |
| Stoner et al. [22] | Adults ≥ 18 (22–55), average age 37.5, 34.5% female | mHealth SMS | Adequate adherence ≥80% at week 8, not statistically significant between groups | SMS messages do not improve medication adherence, but equally as effective as traditional treatment to reduce consumption | RCT |
| Bock et al. [23] | Adults ≥ 18, average age 22, 61.3% female | mHealth SMS, text-message alcohol program (TMAP) | At week 6–12, TMAP participants less likely to report heavy drinking and negative alcohol consequences. Increased self-efficacy to resist drinking. | SMS effective at reducing consumption and increasing self-efficacy | True experiment |
| Freyer-Adam et al. [24] | Adults ≥ 18 (18–64) | mHealth Internet-based app | reached individuals and helped retain them in AUD programs | Not reported | RCT |
| Gamito et al. [25] | Adults ≥ 18, average age 45.45, 90% male | mHealth cognitive stimulation program (CSP) serious games | Cognitive ability between groups not statistically significant, but frontal-lobe function (Frontal Lobe Assessment, FAB) was significantly improved in the intervention group | Improvement in FAB with mHealth intervention | RCT |
| Barrio et al. [26] | Adults ≥ 18, average age 48, 50% female | mHealth app, SIDEAL | Reduced binge drinking and mean daily consumption, participants achieved their self-imposed objectives | Significant reduction in alcohol consumption | Non-experimental (no randomization, no control) |
| Gajecki et al. [27] | Adults ≥ 18, students, 66.7% female | mHealth app (skills training) | Reduced binge drinking and mean daily consumption, participants achieved their self-imposed objectives | Reduced alcohol consumption | RCT |
| Glass et al. [28] | Adults ≥ 18 | mHealth app (A-CHESS) | Intervention showed increased odds of outpatient addiction treatment across follow-ups, but not mutual help | Reduced alcohol consumption, increased treatment | RCT |
| Rose et al. [29] | Adults ≥ 18 | interactive voice response (IVR) brief intervention (BI) | Reduced alcohol consumption, but not statistically different than control | Reduced alcohol consumption | RCT |
| Jo et al. [30] | Adults ≥ 18 | mHealth (online-based brief empowerment for alcohol-use monitor, on-BEAM) | Intervention group reported consuming less alcohol during the past week and lower AUDIT score | Reduced alcohol consumption | RCT |
| Mellentin et al. [31] | Adults ≥ 18 | mHealth (cue exposure) | No differences were detected between the two experimental CET groups on any outcomes | Reduced alcohol consumption | RCT |
| Harder et al. [32] | Adults ≥ 18 | mHealth (motivational interviewing) | Average AUDIT scores were lower for the intervention group | Reduced alcohol consumption, increased self-efficacy | RCT |
| Hendershot et al. [33] | Adults ≥ 18 (21–55) | mHealth feedback, opioid receptor gene (OPRM1) | OPRM1 genotype moderated the association of daily adherence with reduced same-day consumption (p = 0.007) and craving (p = 0.06), with these associations being stronger for participants with the 118 G variant. OPRM1 genotype did not moderate changes in craving and consumption over time | high-density assessments and person-centered analytic approaches, including modeling within-person variation in medication adherence, could be advantageous for pharmacogenetic studies | Non-experimental (no randomization, no control) |
| Constant et al. [34] | Adults ≥ 18 | telephone | Study group had better alcohol abstinence rates than control | Intervention improves patient coping skills and motivation to modify alcohol use behaviors | RCT |
| Graser et al. [35] | Adults ≥ 18 (69% male) | telephone and smartphone-based intervention | Telephone-based intervention was more effective than text-based intervention | Sustained abstinence from excessive drinking occurred in telephone intervention group | RCT |
| Hammond et al. [36] | Adults ≥ 18 (61% male) | mHealth app | Intervention group utilized mobile app more effectively than control group | Complemented community substance use intervention programs | True Experiment |
| Manning et al. [37] | Adults ≥ 18 (58% female) | mHealth app | Intervention group reduced alcohol consumption rates | Improved alcohol consumption rates | Observational |
| Howe et al. [38] | Adults ≥ 18 (85% female; 62% Caucasian) | mHealth app | Use of mobile app improved decision making of study group participants | Mobile data collection can positively influence drinking decisions | Observational |
| Leightley et al. [39] | Adults > 18 (95% male; 100% Veterans) | mHealth app | Use of mobile app reduced rate of alcohol consumption among Veterans in study group | Reduced rates of alcohol consumption | RCT |
| McKay et al. [40] | Adults ≥ 18 (71% male; 82% African American) | telephone and smartphone-based intervention | Use of telephone or smartphone was effective in treating AUD | Improved rates of alcohol dependent persons | RCT |
| O’Grady et al. [41] | Adults ≥ 18 (Quant = 87% male/13% female; Qual = 43% male/57% female) | mHealth app | Provider-facing technology is effective alcohol intervention services and increased access to care in low- and middle-income countries. | Improved rates in alcohol dependent persons | Mixed Methods |
| Authors | Intervention Theme | Results Themes | Medical Outcomes Themes | Effectiveness Themes | Barrier Themes |
|---|---|---|---|---|---|
| McTavish et al. [17] | mHealth app | Good retention | Reduction in cravings | Low cost | Must train users |
| Good acceptance | |||||
| Decreased consumption/cravings | |||||
| Increased self-efficacy/self-determination | |||||
| Murray et al. [18] | mHealth app | Reduction in consumption | Reduction in consumption | Low cost | Cost |
| Improvement in dependence | Decreased consumption/cravings | Must train users | |||
| No significant difference in treatment outcomes | Equally as effective as traditional care (preference) | ||||
| Good acceptance | |||||
| Morgan et al. [19] | mHealth app | High rates of acceptance | Improved rates of depression | Decreased depression symptoms | Computer literacy/access to Internet |
| Cost | |||||
| Chih et al. [20] | mHealth app | Computer models can predict relapse | With prediction of relapse, providers can intervene | Can predict relapse and enable intervention | Must train users |
| Kalapatapu et al. [21] | Telephone/Interactive voice response | No significant difference in treatment outcomes | No significant difference in treatment outcomes | Decreased consumption/cravings | Equally as effective, so change may not be necessary |
| Equally as effective as traditional care (preference) | |||||
| Stoner et al. [22] | mHealth SMS | No significant difference in treatment outcomes | No significant difference in treatment outcomes | Decreased consumption/cravings | Equally as effective, so change may not be necessary |
| Equally as effective as traditional care (preference) | Cost | ||||
| Bock et al. [23] | mHealth SMS | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Increased self-efficacy | Increased self-efficacy | Increased self-efficacy/self-determination | |||
| Freyer-Adam et al. [24] | mHealth app | Good retention | Not reported | Educates | Must train users |
| Increased retention in treatment program | |||||
| Gamito et al. [25] | mHealth serious games/cognitive training | Positive frontal lobe function (FAB) | Increased frontal lobe function | Increased frontal lobe function | Must train users |
| Barrio et al. [26] | mHealth app | Decreased binge drinking | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Reduction in consumption | Increased self-efficacy/self-determination | ||||
| Gajecki et al. [27] | mHealth serious games/cognitive training | Decreased binge drinking | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Reduction in consumption | Increased self-efficacy/self-determination | ||||
| Glass et al. [28] | mHealth app | Good retention | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Increased motivation to change | Increased retention in treatment program | ||||
| Rose et al. [29] | Telephone/Interactive voice response | No significant difference in treatment outcomes | Reduction in consumption | Decreased consumption/cravings | Cost |
| Equally as effective, so change may not be necessary | |||||
| Must train users | |||||
| Jo et al. [30] | mHealth app | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Increased self-efficacy | Increased self-efficacy | Increased self-efficacy/self-determination | |||
| Mellentin et al. [31] | mHealth serious games/cognitive training | No significant difference in treatment outcomes | Reduction in consumption | Decreased consumption/cravings | Equally as effective, so change may not be necessary |
| Must train users | |||||
| Harder et al. [32] | Telephone/Interactive voice response | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Increased self-efficacy | Increased self-efficacy | Increased self-efficacy/self-determination | |||
| Hendershot et al. [33] | mHealth app | Reduction in consumption | Reduction in consumption | Increased medication compliance | Must train users |
| No significant difference in treatment outcomes | Increased medication compliance | Equally as effective as traditional care (preference) | |||
| Decreased consumption/cravings | |||||
| Constant et al. [34] | Telephone/Interactive voice response | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Increased motivation to change | Increased self-efficacy/self-determination | Must sustain intervention for long-term results | |||
| Sustained abstinence from drinking | |||||
| Graser et al. [35] | mHealth + telephone | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Sustained abstinence from drinking | |||||
| Hammond et al. [36] | mHealth app | Reduction in consumption | Reduction in consumption | Increased self-efficacy/self-determination | Must train users |
| Manning et al. [37] | mHealth app | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| Howe et al. [38] | mHealth app | Reduction in consumption | Reduction in consumption | Increased self-efficacy/self-determination | Must train users |
| Increased motivation to change | Decreased consumption/cravings | ||||
| Leightley et al. [39] | mHealth app | Reduction in consumption | Reduction in consumption | Decreased consumption/cravings | Must train users |
| McKay et al. [40] | mHealth + telephone | Reduction in consumption | Reduction in consumption | Increased self-efficacy/self-determination | Must train users |
| Decreased consumption/cravings | |||||
| O’Grady et al. [41] | mHealth app | Reduction in consumption | Reduction in consumption | Increased self-efficacy/self-determination | Computer literacy/access to Internet |
| Decreased consumption/cravings | Impacts provider workload | ||||
| Increased access to care | Must train users |
| Results Themes and Observations | Frequency |
|---|---|
| Reduction in consumption [18,23,26,27,30,32,33,34,35,36,37,38,39,40,41] | 15 |
| No significant difference in treatment outcomes [21,22,29,31,33] | 5 |
| Good retention in treatment [17,24,28] | 3 |
| Increased self-efficacy [23,30,32] | 3 |
| Decreased binge drinking [26,27] | 2 |
| Computer models can predict relapse [20] | 1 |
| High rates of acceptance [19] | 1 |
| Positive frontal lobe function (FAB) [25] | 1 |
| 31 |
| Medical Outcomes Themes and Observations | Frequency |
|---|---|
| Reduction in consumption [18,23,26,27,28,29,30,31,32,33,34,35,36,38,39,40,41] | 18 |
| Increased self-efficacy [23,30,32] | 3 |
| Increased motivation to change [28,34,38] | 3 |
| No significant difference in treatment outcomes [18,21,22] | 3 |
| Reduction in cravings [17] | 1 |
| With prediction of relapse, providers can intervene | 1 |
| Improved rates of depression [19] | 1 |
| Improvement in dependence [18] | 1 |
| Increased frontal lobe function [25] | 1 |
| Increased medication compliance [33] | 1 |
| Not reported [24] | 1 |
| 34 |
| Effectiveness Themes and Observations. | Frequency |
|---|---|
| Decreased consumption/cravings [17,18,21,22,23,26,27,28,29,30,31,32,33,34,35,37,38,39,40,41] | 20 |
| Increased self-efficacy/self-determination [17,23,26,27,30,32,34,36,38,40,41] | 11 |
| Equally as effective as traditional care (preference) [18,21,22,33] | 4 |
| Increased retention in treatment program [17,24,28] | 3 |
| Low cost [17,18] | 2 |
| Good acceptance [17,18] | 2 |
| Sustained abstinence from drinking [34,35] | 2 |
| Increased frontal lobe function [25] | 1 |
| Increased access to care [41] | 1 |
| Decreased depression symptoms [19] | 1 |
| Increased medication compliance [33] | 1 |
| Educates [24] | 1 |
| Can predict relapse and enable intervention [20] | 1 |
| 50 |
| Barriers Themes and Observations | Frequency |
|---|---|
| Must train users [17,18,20,23,24,25,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41] | 22 |
| Equally as effective, so change may not be necessary [21,22,29,31] | 4 |
| Cost [22,29] | 4 |
| Computer literacy/access to Internet [19,41] | 2 |
| Must sustain intervention for long-term results [34] | 1 |
| Impacts provider workload [41] | 1 |
| Not reported | 0 |
| 34 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kruse, C.S.; Betancourt, J.A.; Madrid, S.; Lindsey, C.W.; Wall, V. Leveraging mHealth and Wearable Sensors to Manage Alcohol Use Disorders: A Systematic Literature Review. Healthcare 2022, 10, 1672. https://doi.org/10.3390/healthcare10091672
Kruse CS, Betancourt JA, Madrid S, Lindsey CW, Wall V. Leveraging mHealth and Wearable Sensors to Manage Alcohol Use Disorders: A Systematic Literature Review. Healthcare. 2022; 10(9):1672. https://doi.org/10.3390/healthcare10091672
Chicago/Turabian StyleKruse, Clemens Scott, Jose A. Betancourt, Stephanie Madrid, Christopher William Lindsey, and Vanessa Wall. 2022. "Leveraging mHealth and Wearable Sensors to Manage Alcohol Use Disorders: A Systematic Literature Review" Healthcare 10, no. 9: 1672. https://doi.org/10.3390/healthcare10091672







