Abstract
College students, particularly female students, often suffer from severe stress and poor sleep. Aromatherapy yoga has become a popular exercise in recent years and may help reduce stress and improve sleep quality, although empirical evidence is limited. We investigated the effectiveness of aromatherapy yoga intervention in reducing stress and improving sleep quality among Chinese female college students. A total of 89 participants—44 in the experimental group (aromatherapy yoga) and 45 in the control group (yoga)—with an average age of 19.88 ± 1.13 years, were enrolled in this quasi-experimental study. Interventions were performed in the respective groups once a week for 12 weeks, for 90 min each time. The Wilcoxon signed-rank test and Mann–Whitney U test (including effect size) were used to test the differences in stress reduction and sleep quality before and after the intervention. From the findings of the current research, both therapies did not help female students’ stress levels or sleep hygiene significantly. However, aromatherapy yoga has the potential to improve sleep disturbances experienced by female college students. Additionally, there was no difference in the amount of stress or the quality of sleep between the aromatherapy yoga groups and the regular yoga groups before and after therapy.
1. Introduction
College years are considered to be one of the most stressful periods of a person’s life [1]. College students must adjust to a new social environment, a change in lifestyle, increased academic load and must modify their interpersonal relationships [2]. Excessive stress may have negative psychological (e.g., depression, melancholy) and physical (fatigue, muscle tightness) effects [3,4] and may weaken university students’ self-worth, which may affect their studies and even pose a risk of dropping out of college [5,6]. Reportedly, female college students were more likely to be stressed than male college students [7]. Physiological differences between men and women (e.g., gene vulnerability, cortisol levels, and other hormone levels) may manifest via emotions and behaviors [8]. Females and males respond to stress differently because of their differential sensitivity to events [9]. Female university students were found to be more sensitive to pressure than men; hence, they may experience more sadness and anxiety [10]. When stress is not reduced effectively, bad habits [11], such as alcohol consumption [11], smoking [12], and even suicide ideation [13], become common. Additionally, the relationship between stress and sleep quality may be reciprocal. Stress influences sleep quality if it is not dealt with effectively [14,15].
It has been reported that the percentage of Chinese university students with a sleep duration shorter than 7 h per day was 43.9% [16]. The sleep quality of female college students is worse than that of male college students [17]. A study utilizing the Pittsburgh Sleep Quality Index (PSQI) showed that the sleep quality of female participants aged 20–29 years was worse than that of males [18]. Women aged 17–30 years were more likely to have nightmares, delayed sleep onset, and frequent night awakenings [19]. The decrease in sleep quality was probably caused by the hormone cycles of women [20,21]. Female college students with poor sleep quality were more likely to indulge in excessive drinking [22] and self-mutilation [23], which were often accompanied by unhealthy sleep habits such as using mobile phones before sleep [24]. Good sleep quality is a predictor of physical and mental health as well as overall viability [25]. Good sleep quality may contribute to the academic performance of female college students [26] and may help to avoid problems such as adult obesity [27] and drug abuse [28].
Aromatherapy has been demonstrated to be effective in reducing pressure and improving sleep quality [29,30]. Aromatherapy is a complementary and alternative treatment/medicine (CAM), wherein oils extracted from natural sources such as flowers, petals, and bark of plants are used [31] and absorbed via the respiratory system or skin. This is achieved by massage, bathing, and inhalation to improve the physical and psychological conditions of stressed individuals [29,30]. Volatile compounds can be absorbed most rapidly via inhalation, whereby they act through the limbic system, particularly the amygdala and hippocampus [32]. Aromatherapy can reduce sympathetic nerve activity, increase parasympathetic nerve activity, loosen muscles, and adjust the circadian clock, thereby improving sleep quality and relieving a stressed mood [33,34,35]. Compared with drug treatment, aromatherapy is milder and has fewer side effects.
Additionally, yoga is a physical activity preferred by many female college students [36]. Yoga acts as a nonpharmacological, self-empowering CAM that has the potential to enhance stress management [37] and sleep quality in college students [38]. Yoga enhances general health via pranayamas (respiration-control practice), asanas (yoga poses), and chanda (meditative methods), which collectively aim to achieve mental serenity and foster concentration. Asanas and pranayamas can enhance muscular strength and body flexibility and promote blood circulation and hormone function [39]. Meditation is effective in stabilizing the autonomic nervous system, with emphasis on parasympathetic innervation [40] and an effective reduction in arousal [41].
Since aromatherapy has been shown to have psychological effects on mood improvement, using it to help healthy exercisers avoid feeling awful during a workout can be a viable option [42]. If aromatherapy and yoga are combined, their combined positive effects on health care may be enhanced. Therefore, this study aimed to explore the efficacy of aromatherapy yoga in reducing stress and improving sleep quality among Chinese female college students, with a combination of complementary and alternative therapies designed to alleviate female college students’ negative emotions and improve their overall academic performance and mental health.
2. Materials and Methods
2.1. Study Design and Participants
This study is a quasi-experimental design that lasted from 1 March 2021 to 1 June 2021. Participants were chosen from a specific university in Wuhan, Hubei Province, and only the female students were included. The purpose of this study was explained to the participants by the research assistant, and the students volunteered to participate in the aromatherapy yoga arm (experimental group) or yoga arm (control group) after providing their consent for the study. Both groups attended a 90 min aromatherapy yoga or yoga course once a week for 12 weeks. A questionnaire was administered 1 day before the interventions and included basic information, the Perceived Stress Scale 14 (PSS-14), and PSQI. We included female college students aged > 18 years who were able to understand the questionnaire. We excluded male students, those with a history of respiratory disease, asthma, or allergy to flowers, plants, or essential oils, those who worked at night, and those with a history of mental diseases. The study was approved by the Ethics Committee of Huazhong Agriculture University (HZAUHU-2021-0001) and registered in the ClinicalTrials.gov Protocol Registration and Results System (NCT05459025). All the participants signed an informed consent form.
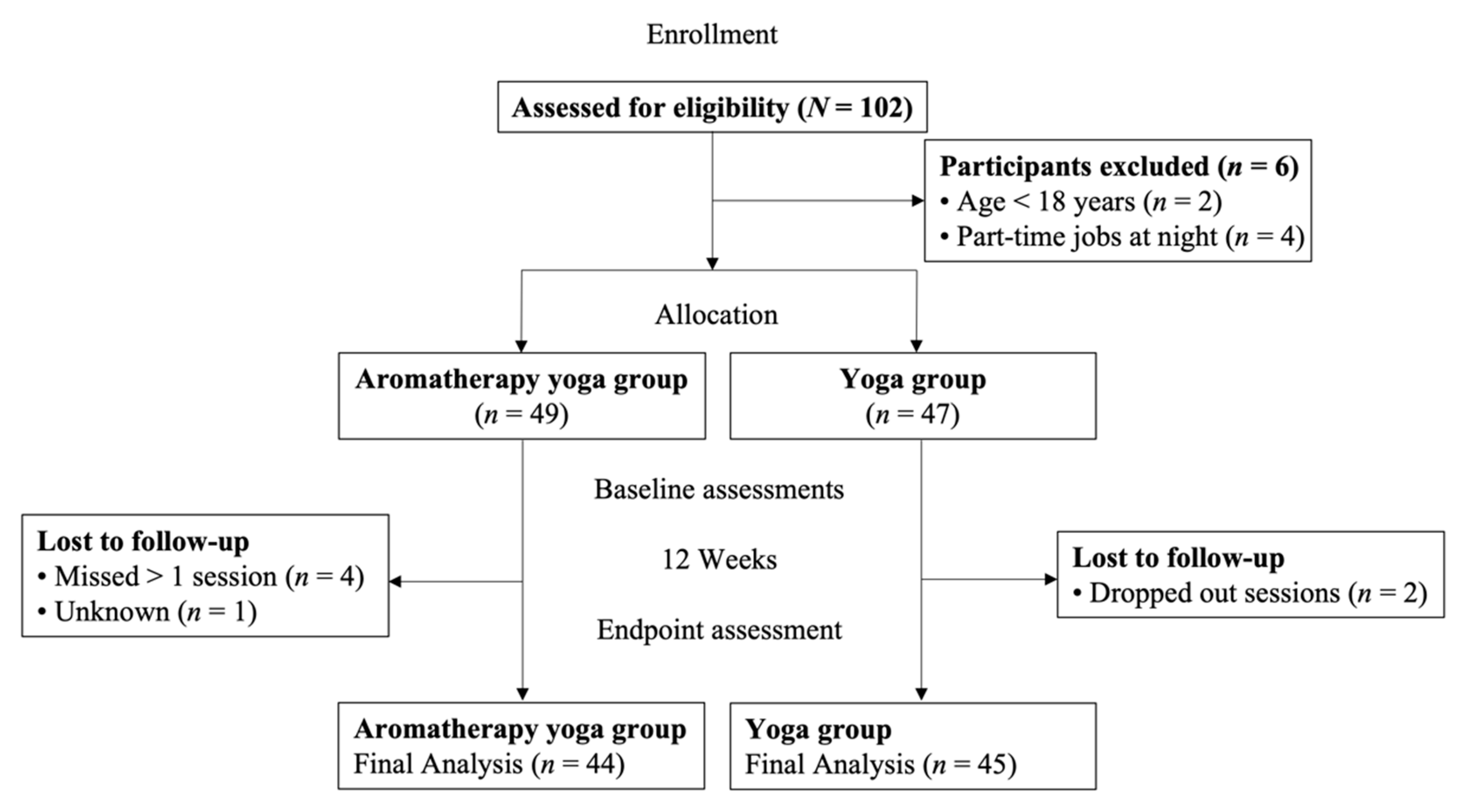
G*Power 3.1. software (Aichach, Germany) was used to calculate the sample size. We used the study by Huang et al. as a reference [43], which had an effect size of 0.74, an alpha level of 0.05, a power of 0.90, and an estimated number of samples of 84. Thus, a total of 102 participants were recruited, and 89 of them completed the study (experimental group, n = 44; control group, n = 45). Four female college students had part-time jobs in the evening and could not participate in the whole intervention; therefore, they were excluded. A flowchart of this study is shown in Figure 1.
Figure 1.
Research flow diagram.
2.2. Questionnaire
The first section of the questionnaire included items on basic personal information, such as age, body mass index (BMI), smoking habit (defined as smoking at least one cigarette once a week in the past 6 months), drinking habit (defined as at least three drinks containing alcohol per week in the past 6 months), tea-/coffee-drinking habit (defined as drinking at least three cups of tea/coffee per week in the past 6 months), mobile phone-use habit before sleep (defined as using a mobile phone within half an hour before sleep in the past 1 month).
The second section was the PSS-14 developed by Cohen et al. [44]. PSS-14 is the questionnaire that is most widely used for measuring the degree to which situations in one’s life are appraised as being stressful. The PSS-14 is a 14-item questionnaire, with each item scored on a 5-point Likert scale, ranging from 0 (“never”) to 4 (“very often”). Seven positive and seven negative items were included in the analysis. The total score ranged from 0 to 56 points, with a higher score representing a higher level of perceived stress. The Chinese version of the PSS-14 has good reliability and validity [45]. The Cronbach’s α values for the PSS-14 before and after the study were 0.82 and 0.85, respectively.
The third section was the PSQI developed by Buysse et al. [46], which evaluates the sleep quality of the participants in the past month. This scale is seven subscales (18 items) self-report questionnaire, which includes: (1) Subjective sleep quality (1 item): degree of self-satisfaction in the past month. A higher score represents a more unsatisfactory result; (2) Sleep latency (2 items): the amount of time it took to fall asleep in the past month. A higher score represents more time needed to fall asleep; (3) Sleep duration (1 item): the average sleep time every night in the past month. A higher score represents a shorter sleep time; (4) Habitual sleep efficiency (2 items): higher scores represent lower efficiency of sleep; (5) Sleep disturbances (9 items): higher scores represent more severe sleep disturbances; (6) Use of sleeping medication (1 item): a higher score indicates more frequent use of sleep medication; (7) Daytime dysfunction (2 items): a higher score represents more problems encountered with daily life activities. The score ranges from 0 to 3. The total score ranges from 0 to 21, with higher scores representing worse sleep quality [46]. The Chinese version of the PSQI has good reliability and validity [47]. The Cronbach’s α values before and after the study for the PSQI (including subscales) were above 0.71.
2.3. Intervention
2.3.1. Aromatherapy
Lavender (Lavandula angustifolia, of the family Lamiaceae) essential oil is a commonly used essential oil that is mild and safe for oral administration [48]. It is not only beneficial for reducing stress and nervousness but also for ameliorating sleep disorders [49]. Therefore, 100% pure Lavandula angustifolia essential oil (Erbamea, Italy) was selected, and aromatherapy was implemented by aroma diffusers (W701, fog output volume: 10 ± 4 mL/h, Media).
2.3.2. Yoga
The design of the yoga lessons was based on a past study [43] and a professional yoga instruction book [50]. Yoga lessons were led by certified yoga tutors, with the curriculum contents stated as follows: First, the participant holds her breath and adjusts respiration for approximately 15 min. Subsequently, the participants switched from diaphragmatic respiration to abdominal respiration. Breathing duration was extended progressively to promote both mental and physical serenity, after which the next phase was initiated. The overall duration of the asana exercise was approximately 1 h. It began with a sun-salutation posture as a warm-up, before various asanas, such as the cobra posture, downward facing dog, warrior posture, triangle posture, boat posture, cow-face posture, hero posture 1, hero posture 2, twisted triangle posture, spinal twist posture, seated angle posture, child’s posture, fish posture, wheel posture, locust posture, camel posture, shoulder stand, plow posture, and, lastly, the corpse posture were performed. Eventually, participants spent 15 min in meditation and adjusted their respiration.
2.3.3. Aromatherapy Yoga
The research assistant diluted the Lavandula angustifolia essential oil with distilled water (1:75) 10 min before the yoga session started. The solution was then atomized by three aroma diffusers, placed in the front, middle, and back of the classroom. The distance from each participant was less than 10 m to ensure that the aroma was absorbed completely. The yoga course for the aromatherapy yoga group was the same as that of the yoga-only group. The yoga-only group only took a yoga course without aromatherapy.
Each intervention session in both the study and control groups lasted 90 min, between 6 p.m. and 7:30 p.m. The course was held in a yoga classroom once a week, in an area of 30 m × 35 m. Furthermore, the total intervention period lasted for 12 weeks. The sessions for both groups were scheduled (spread out) to avoid the influence of aromatherapy on the control group. The windows of the classroom were closed during each session. The temperature was maintained between 25 °C and 26 °C, and the average humidity was controlled at 55 ± 5%. The participants were allowed to withdraw if they were uncomfortable. The aromatherapy yoga course was designed by a yoga teacher and a certified aroma therapist. The two groups shared the same yoga teacher.
2.4. Statistical Analysis
First, descriptive, statistical demographic data included age, BMI, grade, smoking habit, drinking habit, mobile phone-use habit before sleep, PSS-14 baseline, PSQI total score, and seven subscale scores at baseline. The Wilcoxon rank-sum test and chi-square tests were used to evaluate the differences in demographic data between groups. Second, the Wilcoxon signed-rank test was used to evaluate the within-group difference in the total score of the PSS-14 and the scores of the seven PSQI subscales before and after the study. This method was used because the data were not normally distributed (based on the Shapiro–Wilk test, skewness values for the PSS-14 score, and PSQI subscales ranged from 2.17 to 3.68, whereas kurtosis ones ranged from 2.29 to 11.16). Finally, the Mann–Whitney U test was used to compare the changes (i.e., the difference between the end of the study and the baseline values) of the total PSS-14 score and the scores of the seven PSQI subscales of the two groups to evaluate the efficacy of aromatherapy yoga. The effect size was presented to reflect the difference between the two groups. Effect sizes were calculated using the Mann–Whitney U test (Effect Size r), which captures the standardized median difference between the two groups. Cohen’s classification of effect sizes was used: 0.1 (small effect), 0.3 (moderate effect), and 0.5 and above (large effect) [51]. All calculations were performed using SPSS 25 for Mac (IBM Corp., Armonk, NY, USA). Statistical significance was set at p < 0.05.
3. Results
Table 1 shows basic demographic information and a comparison of baseline values (PSS-14, PSQI total score with seven scales). There were 89 participants (44 in the aromatherapy yoga group and 45 in the yoga-only group) with an average age of 19.88 ± 1.13 and an average BMI of 20.50 ± 3.38 kg/m2. Most participants were freshmen (51.7%), 95.5% of them had no alcohol-drinking habits, and 66.3% had no tea-/coffee-drinking habits. None of the participants had smoking habits, but all had the habit of using cell phones half an hour before bedtime, and all lived in on-campus dormitories. There were no significant differences between the two groups in terms of BMI, alcohol-drinking habits, tea-/coffee-drinking habits, and baseline PSS-14 (p > 0.05); however, there were significant differences in age (p < 0.001).

Table 1.
Basic demographic information and comparison of baseline values (PSS-14 and PSQI total score with seven subscales, N = 89).
Table 2 shows the differences in the PSS-14 and PSQI scores measured before and after the test in the aromatherapy yoga group and the yoga-only group. There was no significant difference within the aromatherapy yoga group in terms of the PSS-14; however, there was a significant difference (p < 0.05) in the PSQI subscale of sleep disturbance. This implies that there was a significant improvement in sleep disturbance with the aromatherapy yoga intervention. However, there was no significant difference in the PSS-14, PSQI total score, and seven PSQI subscales in the yoga-only group.

Table 2.
Intragroup differences in the PSS-14 and PSQI scores in the aromatherapy yoga group and the yoga-only group.
Table 3 displays the differences in PSS-14 and PSQI scores between the aromatherapy yoga and yoga-only group. The PSS-14 and PSQI scores between the two groups were not significantly different. In addition, the effect sizes of sleep length (r = 0.12) and sleep disturbance (r = 0.17) revealed a slight difference between the two groups.

Table 3.
Intergroup differences in the PSS-14 and PSQI scores in the aromatherapy yoga group and the yoga-only group.
4. Discussion
Few studies have examined the combination of aromatherapy and yoga [42] to determine its effectiveness on stress reduction and sleep quality among Chinese female college students. The results of the present study showed that aromatherapy yoga could effectively reduce sleep disturbance in female college students. In aromatherapy yoga and yoga-only groups, there were no differences in stress levels or sleep quality between before and after therapy (except on one PSQI subscale of sleep disturbance in the aromatherapy yoga group).
4.1. Stress
As shown in Table 2, there was no significant difference between the aromatherapy yoga and yoga-only groups in terms of stress. Although there have been very few studies on the effects of aromatherapy yoga on an individual’s stress, recent studies have reported the use of lavender essential oil in inhalation aromatherapy to reduce stress levels in female college students, particularly among those who prefer a lavender aroma [52]. Its positive effect on stress levels in different groups, such as women with postpartum stress [53], individuals with academic stress [54], and nurses’ work stress [55], has been demonstrated. Furthermore, it has been reported that performing yoga exercises (lasting 60 min) twice weekly for 7 months rendered a positive influence on female students’ psychoemotional state (i.e., stress), general physical self-feeling, and physical condition [56]. Yoga has also been shown as effective for stress management among healthcare workers [57] and for stress reduction in employees [58]. However, the present study observed a statistically insignificant decrease in PSS-14 scores in both groups after the intervention, but this might have been a result of the study limitations, such as a low intensity of the intervention. Moreover, the baseline score of PSS-14 in this study is lower than those of other college students [58], and thus, there may be less room for change. These could be the reasons the decrease in PSS-14 scores did not reach statistical significance.
In addition, there was no significant difference in the reduction in stress between the aromatherapy yoga and yoga-only groups (Table 3). Both aromatherapy yoga and yoga showed a decreasing trend in PSS-14 scores after the intervention. In other words, both interventions provided some degree of improvement for the participants. This may be one of the reasons for the lack of a significant difference. Further studies should be conducted in this regard in the future.
4.2. Sleep Quality
Different groups of people can benefit from the favorable benefits of yoga [59] and aromatherapy [33,60] on their quality of sleep. In this study, the lavender essential oil was used as an intervention. Linalool and linalyl acetate, the two main constituents of lavender oil, have a notable hypnotic effect that promotes sleep by inhibiting the production of acetylcholine and creating a hypnotic effect [61,62,63]. For instance, Gürler et al. [64] discovered that a steam inhalation intervention with a lavender aroma for menopausal women experiencing sleep deficit helped to improve their sleep quality. Additionally, participants saw improvements in subjective sleep quality, sleep latency, sleep length, use of sleep medicines, and particularly sleep disturbance following seven interventions of weekly yoga [65]. The aforementioned factors may help to explain why this study combined yoga and aromatherapy to treat sleep disruption (Table 2). Only the PSQI item measuring sleep disruption showed a significant improvement in the current trial. The usefulness of aromatherapy yoga in enhancing sleep quality has to be further investigated.
There was no significant improvement in sleep quality in the yoga-only group (Table 2), which was inconsistent with previous studies [66,67] related to the effectiveness of yoga in improving sleep quality. Previous studies have noted that low levels of physical activity (e.g., yoga) had no significant effect on improving sleep quality [68,69]. Furthermore, one study noted that general exercise (e.g., yoga) had no significant effect on sleep quality across genders, which could be attributed to relevant demographic variables that were not investigated [70]. Therefore, the lack of a significant effect of the yoga intervention on sleep quality in this study may be due to the low level of physical activity, as well as the uninvestigated demographic variables (e.g., work status and family type), which may have led to the lack of significant difference in the study results. Moreover, the baseline score of PSQI in this study is lower than those of other college students [58], and thus, there may be less room for change.
In Table 3, the differences between baseline and endpoint scores of the aromatherapy yoga group and yoga-only group show that the scores of four components (sleep duration, habitual sleep efficiency, use of sleep medication, and daytime dysfunction) in the aromatherapy yoga group increased, while those of six components of yoga-only group increased, suggesting that most of the PSQI scores were slightly but not significantly increased from the baseline to endpoint. According to the university calendar, the midterm exams were held in the week of the study endpoint. Thus, exam preparation could be a reason students had reduced sleep quality.
In addition, the results in Table 3 show no significant difference in sleep quality improvement between the aromatherapy yoga and yoga-only groups. Considering the relatively small sample size of this study, the statistical test may not have been able to detect significant differences between the two groups because of insufficient test power. The differences in each variable between the two groups are presented in terms of the effect size. Sleep duration and sleep disturbance showed small effect sizes, which suggests a potential better effect of aromatherapy yoga intervention. A previous study showed that the sleep quality of those who were admitted to the intensive care units for percutaneous coronary interventions and underwent aromatherapy was significantly improved compared with those who underwent conventional nursing intervention [71]. Another study showed that a yoga-only group reported significantly lower sleep disturbance scores than the control group, indicating that such a program significantly improves sleep-related outcomes [65]. Therefore, the combination of these two interventions in this study may have reduced sleep disturbance through synergistic effects. The results support the hypothesis that the combination of aromatherapy and yoga may be an effective intervention for reducing sleep disturbance among Chinese female college students. Nonetheless, further studies are required to provide more evidence.
4.3. Limitations
This study had some limitations. First, there were significant differences in age between the two study groups at baseline, probably due to nonrandomized allocation into the aromatherapy yoga group since the participants were assigned according to their preference. A randomized study is recommended in the future to reduce bias and extend the sample size to explain causation. Second, response bias could have been induced by the sleep quality scales, although they are extensively used and have good reliability. Therefore, the experimental method may need to consider an objective index to monitor sleep, such as sleep time, sleep cycles, and heart rate variability, in order to reduce the influence of subjective factors. Third, although we utilized G*Power 3.1. software (Aichach, Germany) to calculate the sample size in the initial study stage, more samples are recommended to investigate the efficacy of these two therapies. Finally, sleep disorders are influenced by a variety of other factors, such as the learning pressure in different phases, learning pressure with different majors, and the influence of other factors prior to sleeping. Therefore, future research is needed to consider more compounding factors. In order to control the stability of the intervention effects, it is also advised that future research adopt a nonintervention/aromatherapy-only group as a control group and use three-time measurements: before (Time 1), after therapy (Time 2), and one month/few weeks after therapy (Time 3). Despite these limitations, the findings of this study provide important clues for exploring the efficacy of aromatherapy yoga in improving individual stress and sleep quality.
5. Conclusions
Our study suggests that aromatherapy yoga interventions might improve sleep disturbance in female college students. However, the efficacy of improving sleep quality was small compared with that of yoga alone. In general, the therapies did not help female students’ stress levels or sleep hygiene. Therefore, more empirical studies that investigate the effect of aromatherapy yoga intervention on stress and sleep quality in female college students are needed.
Author Contributions
Conceptualization, Y.G., C.L. and S.-Y.Y.; methodology, C.L. and S.-Y.Y.; formal analysis, J.-Y.W.; investigation, F.K.; resources, Y.G. and F.K.; data curation, J.-Y.W.; writing—original draft preparation, Y.G., F.K. and C.L.; writing—review and editing, J.-Y.W., S.-Y.Y., C.L. and R.T.; funding acquisition, S.-Y.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a research grant from the Asia University, Taiwan (ASIA-109-CMUH-08; ASIA-110-CMUH-23).
Institutional Review Board Statement
The institutional review boards of Huazhong Agriculture University (HZAUHU-2021-0001) approved this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Acknowledgments
The authors wholeheartedly thank Hui-Wen Kang (certified aroma therapist, Taiwan), Ling Qiu (yoga teacher, China), and all participants who helped make this research possible.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eisenbarth, C.A. Coping with stress: Gender differences among college students. Coll. Stud. J. 2019, 53, 151–162. [Google Scholar]
- Ross, S.E.; Niebling, B.C.; Heckert, T.M. Sources of stress among college students. Coll. Stud. J. 1999, 33, 312–317. [Google Scholar]
- Contrada, R.; Baum, A. The Handbook of Stress Science: Biology, Psychology, and Health; Springer Publishing Company: New York, NY, USA, 2010. [Google Scholar]
- Misra, R.; McKean, M.; West, S.; Russo, T. Academic stress of college students: Comparison of student and faculty perceptions. Coll. Stud. J. 2000, 34. [Google Scholar]
- Muller, K.; Feuer, E.; Nyman, M.; Sokolowski, K.; Rotella, L. Examining predictors of first year college student retention. N. Y. J. Stud. Aff. 2017, 17, 2. [Google Scholar]
- Silver, H.K.; Glicken, A.D. Medical student abuse: Incidence, severity, and significance. JAMA 1990, 263, 527–532. [Google Scholar] [CrossRef]
- Anastasiades, M.H.; Kapoor, S.; Wootten, J.; Lamis, D.A. Perceived stress, depressive symptoms, and suicidal ideation in undergraduate women with varying levels of mindfulness. Arch. Women’s Ment. Health 2017, 20, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L.; Abramson, L.Y. Development of gender differences in depression: Description and possible explanations. Ann. Med. 1999, 31, 372–379. [Google Scholar] [CrossRef]
- Afifi, M. Gender differences in mental health. Singap. Med. J. 2007, 48, 385. [Google Scholar]
- Chaplin, T.M.; Hong, K.; Bergquist, K.; Sinha, R. Gender Differences in Response to Emotional Stress: An Assessment Across Subjective, Behavioral, and Physiological Domains and Relations to Alcohol Craving. Alcohol. Clin. Exp. Res. 2008, 32, 1242–1250. [Google Scholar] [CrossRef]
- Morgan, S. Cheap drinks, heavy costs students and alcohol. Youth Policy 1997, 56, 42–54. [Google Scholar]
- Liu, X. Cigarette smoking, life stress, and behavioral problems in Chinese adolescents. J. Adolesc. Health 2003, 33, 189–192. [Google Scholar] [CrossRef]
- Hirsch, J.K.; Ellis, J.B. Differences in life stress and reasons for living among college suicide ideators and non-ideators. Coll. Stud. J. 1996, 30, 377–386. [Google Scholar]
- Alsaggaf, M.A.; Wali, S.O.; Merdad, R.A.; Merdad, L.A. Sleep quantity, quality, and insomnia symptoms of medical students during clinical years: Relationship with stress and academic performance. Saudi Med. J. 2016, 37, 173. [Google Scholar] [CrossRef] [PubMed]
- Doolin, J.; Vilches, J.E.; Cooper, C.; Gipson, C.; Sorensen, W. Perceived stress and worldview influence sleep quality in Bolivian and United States university students. Sleep Health 2018, 4, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, Y.-Y.; Wang, S.-B.; Li, L.; Lu, L.; Ng, C.; Ungvari, G.S.; Chiu, H.F.; Hou, C.-L.; Jia, F.-J.; et al. Sleep Duration and Sleep Patterns in Chinese University Students: A Comprehensive Meta-Analysis. J. Clin. Sleep Med. 2017, 13, 1153–1162. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Wuertz, C.; Rogers, R.; Chen, Y.-P. Stress and Sleep Disturbances in Female College Students. Am. J. Health Behav. 2013, 37, 851–858. [Google Scholar] [CrossRef]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M. Subjective sleep quality and sleep problems in the general Japanese adult population. Psychiatry Clin. Neurosci. 2001, 55, 213–215. [Google Scholar] [CrossRef]
- Coren, S. The prevalence of self-reported sleep disturbances in young adults. Int. J. Neurosci. 1994, 79, 67–73. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Vasireddi, M.; Chen, Y.P.; Wang, Y.T.; Hilliard, J. PNI Biomarkers and Health Outcomes in College Women. Healthcare 2014, 2, 207–219. [Google Scholar] [CrossRef]
- Xing, X.; Xue, P.; Li, S.X.; Zhou, J.; Tang, X. Sleep disturbance is associated with an increased risk of menstrual problems in female Chinese university students. Sleep Breath. 2020, 24, 1719–1727. [Google Scholar] [CrossRef]
- Liu, X.; Chen, H.; Bo, Q.-G.; Fan, F.; Jia, C.-X. Poor sleep quality and nightmares are associated with non-suicidal self-injury in adolescents. Eur. Child Adolesc. Psychiatry 2017, 26, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.; Lee, H.; Hong, J.P.; Cho, M.J.; Fava, M.; Mischoulon, D.; Kim, D.J.; Jeon, H.J. Poor sleep quality and suicide attempt among adults with internet addiction: A nationwide community sample of Korea. PLoS ONE 2017, 12, e0174619. [Google Scholar] [CrossRef] [PubMed]
- Chahine, R.; Farah, R.; Chahoud, M.; Harb, A.; Tarabay, R.; Sauleau, E.; Godbout, R. Assessing sleep quality of Lebanese high school students in relation to lifestyle: Pilot study in Beirut. East. Mediterr. Health J. 2018, 24, 722–728. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J. Clin. Sleep Med. 2015, 11, 931–952. [Google Scholar] [CrossRef] [PubMed]
- Gaultney, J.F. The Prevalence of Sleep Disorders in College Students: Impact on Academic Performance. J. Am. Coll. Health. 2010, 59, 91–97. [Google Scholar] [CrossRef]
- Chen, T.Y.; Chou, Y.C.; Tzeng, N.S.; Chang, H.A.; Kuo, S.C.; Pan, P.Y.; Yeh, Y.W.; Yeh, C.B.; Mao, W.C. Effects of a selective educational system on fatigue, sleep problems, daytime sleepiness, and depression among senior high school adolescents in Taiwan. Neuropsychiatr. Dis. Treat. 2015, 11, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Britton, W.B.; Bootzin, R.R.; Cousins, J.C.; Hasler, B.P.; Peck, T.; Shapiro, S.L. The Contribution of Mindfulness Practice to a Multicomponent Behavioral Sleep Intervention Following Substance Abuse Treatment in Adolescents: A Treatment-Development Study. Subst. Abus. 2010, 31, 86–97. [Google Scholar] [CrossRef]
- Posadzki, P.; Watson, L.K.; Alotaibi, A.; Ernst, E. Prevalence of use of complementary and alternative medicine (CAM) by patients/consumers in the UK: Systematic review of surveys. Clin. Med. (Lond.) 2013, 13, 126–131. [Google Scholar] [CrossRef]
- Lee, M.-K.; Lim, S.; Song, J.-A.; Kim, M.-E.; Hur, M.-H. The effects of aromatherapy essential oil inhalation on stress, sleep quality and immunity in healthy adults: Randomized controlled trial. Eur. J. Integr. Med. 2017, 12, 79–86. [Google Scholar] [CrossRef]
- Ahmad, R.; Naqvi, A.A.; Ahmad, N.; Baraka, M.; Mastour, M.; Al Sharedah, S.; Al Ghamdi, S.; Al Rabae, G.; Al Ghamdi, M.S. Awareness, perception, attitude, and knowledge regarding complementary and alternative medicines (cams) among the pharmacy and medical students of a public university in Saudi Arabia. Arch. Pharm. Pract. 2017, 8, 51–63. [Google Scholar] [CrossRef]
- Cavanagh, H.M.A.; Wilkinson, J.M. Biological activities of Lavender essential oil. Phytother. Res. 2002, 16, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.-C.; Lee, P.-H.; Tseng, S.-J.; Lin, Y.-M.; Chen, S.-R.; Hou, W.-H. Effects of aromatherapy on sleep quality: A systematic review and meta-analysis. Complement. Ther. Med. 2019, 45, 156–166. [Google Scholar] [CrossRef] [PubMed]
- López, V.; Nielsen, B.; Solas, M.; Ramírez, M.J.; Jäger, A.K. Exploring Pharmacological Mechanisms of Lavender (Lavandula angustifolia) Essential Oil on Central Nervous System Targets. Front. Pharmacol. 2017, 8, 280. [Google Scholar] [CrossRef] [PubMed]
- Hwang, E.; Shin, S. The Effects of Aromatherapy on Sleep Improvement: A Systematic Literature Review and Meta-Analysis. J. Altern. Complement. Med. 2015, 21, 61–68. [Google Scholar] [CrossRef]
- Cruz, S.Y.; Fabián, C.; Pagán, I.; Ríos, J.L.; González, A.M.; Betancourt, J.; González, M.J.; Rivera-Soto, W.T.; Palacios, C. Physical activity and its associations with sociodemographic characteristics, dietary patterns, and perceived academic stress in students attending college in Puerto Rico. Puerto Rico Health Sci. J. 2013, 32, 44–50. [Google Scholar]
- Tripathi, M.N.; Kumari, S.; Ganpat, T.S. Psychophysiological effects of yoga on stress in college students. J. Educ. Health Promot. 2018, 7, 43. [Google Scholar] [CrossRef]
- Elstad, T.; Ulleberg, P.; Klonteig, S.; Hisdal, J.; Dyrdal, G.M.; Bjorndal, A. The effects of yoga on student mental health: A randomised controlled trial. Health Psychol. Behav. Med. 2020, 8, 573–586. [Google Scholar] [CrossRef]
- Woodyard, C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int. J. Yoga 2011, 4, 49–54. [Google Scholar] [CrossRef]
- Parshad, O. Role of yoga in stress management. West Indian Med. J. 2004, 53, 191–194. [Google Scholar]
- Khalsa, S.B.S. Treatment of chronic insomnia with yoga: A preliminary study with sleep–wake diaries. Appl. Psychophysiol. Biofeedback 2004, 29, 269–278. [Google Scholar] [CrossRef]
- Kwon, S.; Ahn, J.; Jeon, H. Can Aromatherapy Make People Feel Better Throughout Exercise? Int. J. Environ. Res. Public Health 2020, 17, 4559. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.-J.; Chien, D.-K.; Chung, U.-L. Effects of Hatha Yoga on Stress in Middle-Aged Women. J. Nurs. Res. 2013, 21, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Chu, L.C.; Kao, H.S. The moderation of meditation experience and emotional intelligence on the relationship between perceived stress and negative mental health. Chin. J. Physiol. 2005, 47, 157. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Zheng, B.; Li, M.; Wang, K.L.; Lv, J. Analysis of the reliability and validity of the Chinese version of Pittsburgh sleep quality index among medical college students. Beijing Da Xue Xue Bao Yi Xue Ban 2016, 48, 424–428. [Google Scholar]
- Ali, B.; Al-Wabel, N.A.; Shams, S.; Ahamad, A.; Khan, S.A.; Anwar, F. Essential oils used in aromatherapy: A systemic review. Asian Pac. J. Trop. Biomed. 2015, 5, 601–611. [Google Scholar] [CrossRef]
- Setzer, W.N. Essential Oils and Anxiolytic Aromatherapy. Nat. Prod. Commun. 2009, 4, 1934578X0900400928. [Google Scholar] [CrossRef]
- Farhi, D. Yoga Mind, Body & Spirit: A Return to Wholeness; Holt Paperbacks; Macmillan: New York, NY, USA, 2011. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155. [Google Scholar] [CrossRef]
- Toda, M.; Matsuse, R. Endocrinological effect of lavender aromatherapy on stressful visual stimuli. Contemp. Clin. Trials Commun. 2020, 17, 100547. [Google Scholar] [CrossRef] [PubMed]
- Kianpour, M.; Mansouri, A.; Mehrabi, T.; Asghari, G. Effect of lavender scent inhalation on prevention of stress, anxiety and depression in the postpartum period. Iran. J. Nurs. Midwifery Res. 2016, 21, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Naqvi, A.A.; Al-Bukhaytan, H.M.; Al-Nasser, A.H.; Al-Ebrahim, A.H.B. Evaluation of aromatherapy with lavender oil on academic stress: A randomized placebo controlled clinical trial. Contemp. Clin. Trials Commun. 2019, 14, 100346. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-C.; Fang, S.-H.; Fang, L. The effects of aromatherapy in relieving symptoms related to job stress among nurses. Int. J. Nurs. Pract. 2013, 21, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Skurikhina, N.; Kudryavtsev, M.D.; Kuzmin, V.A.; Iermakov, S.S. Fitness yoga as modern technology of special health groups’ girl students’ psycho-physical condition and psycho-social health strengthening. Phys. Educ. Stud. 2016, 20, 24–31. [Google Scholar] [CrossRef]
- Cocchiara, R.A.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; La Torre, G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef]
- Maddux, R.E.; Daukantaité, D.; Tellhed, U. The effects of yoga on stress and psychological health among employees: An 8- and 16-week intervention study. Anxiety Stress Coping 2017, 31, 121–134. [Google Scholar] [CrossRef]
- Wang, W.-L.; Chen, K.-H.; Pan, Y.-C.; Yang, S.-N.; Chan, Y.-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry 2020, 20, 195. [Google Scholar] [CrossRef]
- Her, J.; Cho, M.-K. Effect of aromatherapy on sleep quality of adults and elderly people: A systematic literature review and meta-analysis. Complement. Ther. Med. 2021, 60, 102739. [Google Scholar] [CrossRef]
- Karadag, E.; Samancioglu, S.; Ozden, D.; Bakir, E. Effects of aromatherapy on sleep quality and anxiety of patients. Nurs. Crit. Care 2015, 22, 105–112. [Google Scholar] [CrossRef]
- Najafi, Z.; Tagharrobi, Z.; Shahriyari-Kale-Masihi, M. Effect of aromatherapy with Lavender on sleep quality among patients undergoing hemodialysis. KAUMS J. 2014, 18, 145–150. [Google Scholar]
- Nasiri Lari, Z.; Hajimonfarednejad, M.; Riasatian, M.; Abolhassanzadeh, Z.; Iraji, A.; Vojoud, M.; Heydari, M.; Shams, M. Efficacy of inhaled Lavandula angustifolia Mill. Essential oil on sleep quality, quality of life and metabolic control in patients with diabetes mellitus type II and insomnia. J. Ethnopharmacol. 2020, 251, 112560. [Google Scholar] [CrossRef] [PubMed]
- Gürler, M.; Kızılırmak, A.; Baser, M. The Effect of Aromatherapy on Sleep and Quality of Life in Menopausal Women with Sleeping Problems: A Non-Randomized, Placebo-Controlled Trial. Complement. Med. Res. 2020, 27, 421–430. [Google Scholar] [CrossRef]
- Cohen, L.; Warneke, C.; Fouladi, R.T.; Rodriguez, M.A.; Chaoul-Reich, A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer 2004, 100, 2253–2260. [Google Scholar] [CrossRef]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, B.; Parajuli, N.; Jat, M. Effect of four weeks of integrated yoga intervention on perceived stress and sleep quality among female nursing professionals working at a tertiary care hospital: A pilot study. Ind. Psychiatry J. 2021, 30, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Avis, N.E.; Legault, C.; Russell, G.; Weaver, K.; Danhauer, S.C. Pilot study of integral yoga for menopausal hot flashes. Menopause 2014, 21, 846–854. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Arias, J.Á.; Marín-Cascales, E.; Ramos-Campo, D.J.; Hernandez, A.V.; Pérez-López, F.R. Effect of exercise on sleep quality and insomnia in middle-aged women: A systematic review and meta-analysis of randomized controlled trials. Maturitas 2017, 100, 49–56. [Google Scholar] [CrossRef]
- Soltani Shal, R.; Aghamohammadian Sharbaf, H. Effect of exercise on general health, quality of sleep and quality of life in Ferdowsi University of Mashhad students. J. Inflam. Dis. 2013, 17, 39–46. [Google Scholar]
- Cho, M.-Y.; Min, E.S.; Hur, M.-H.; Lee, M.S. Effects of Aromatherapy on the Anxiety, Vital Signs, and Sleep Quality of Percutaneous Coronary Intervention Patients in Intensive Care Units. Evid.-Based Complement. Altern. Med. 2013, 2013, 381381. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).