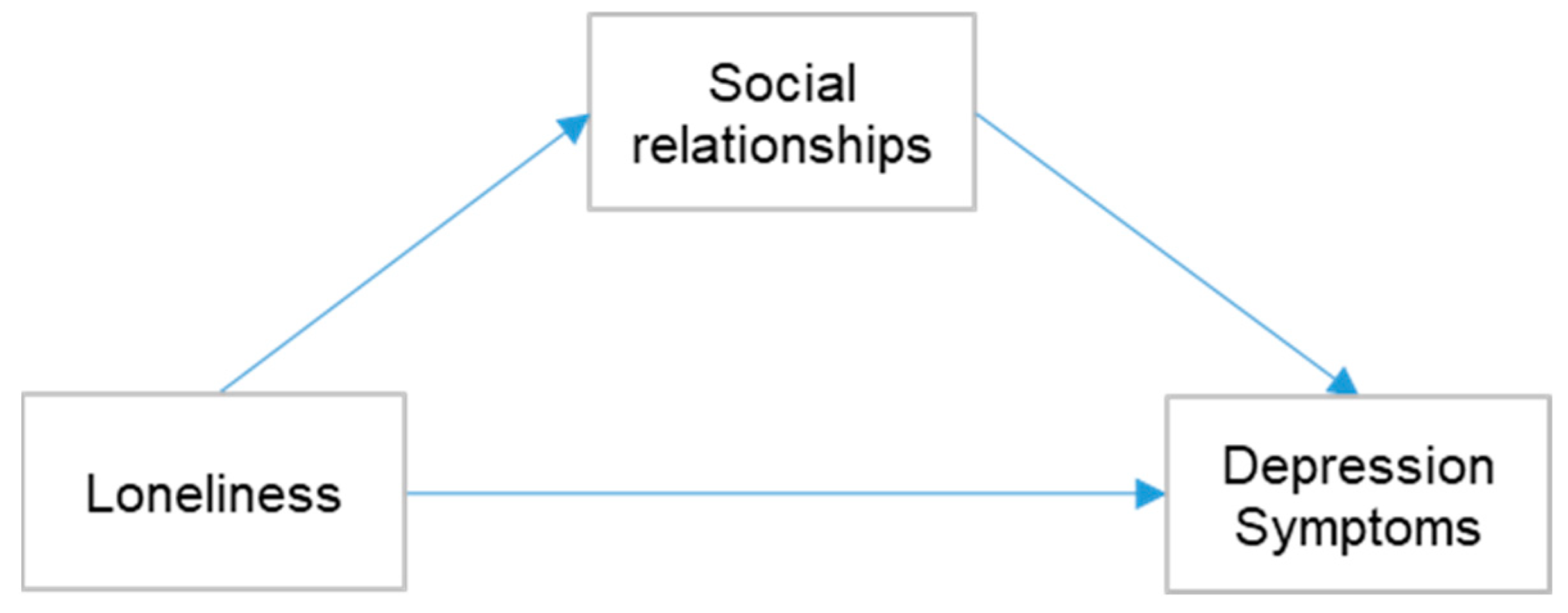
Role of Multifaceted Social Relationships on the Association of Loneliness with Depression Symptoms: A Moderated Mediation Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Measures
2.3.1. Loneliness
2.3.2. Depression Symptoms
2.3.3. Social Relationships
2.3.4. Covariables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Partridge, L.; Deelen, J.; Slagboom, P.E. Facing up to the Global Challenges of Ageing. Nature 2018, 561, 45–56. [Google Scholar] [CrossRef] [Green Version]
- Cosco, T.D.; Howse, K.; Brayne, C. Healthy Ageing, Resilience and Wellbeing. Epidemiol. Psychiatr. Sci. 2017, 26, 579–583. [Google Scholar] [CrossRef]
- Akiyama, H. Aging Well: An Update. Nutr. Rev. 2020, 78, 3–9. [Google Scholar] [CrossRef]
- Ageing. Available online: https://www.who.int/health-topics/ageing (accessed on 2 December 2022).
- Forman, D.E.; Maurer, M.S.; Boyd, C.; Brindis, R.; Salive, M.E.; Horne, F.M.; Bell, S.P.; Fulmer, T.; Reuben, D.B.; Zieman, S.; et al. Multimorbidity in Older Adults with Cardiovascular Disease. J. Am. Coll. Cardiol. 2018, 71, 2149–2161. [Google Scholar] [CrossRef]
- McGilton, K.S.; Vellani, S.; Yeung, L.; Chishtie, J.; Commisso, E.; Ploeg, J.; Andrew, M.K.; Ayala, A.P.; Gray, M.; Morgan, D.; et al. Identifying and Understanding the Health and Social Care Needs of Older Adults with Multiple Chronic Conditions and Their Caregivers: A Scoping Review. BMC Geriatr. 2018, 18, 231. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-W.; Chippendale, T. Factors Associated with IADL Independence: Implications for OT Practice. Scand. J. Occup. Ther. 2017, 24, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Kiyoshige, E.; Kabayama, M.; Gondo, Y.; Masui, Y.; Inagaki, H.; Ogawa, M.; Nakagawa, T.; Yasumoto, S.; Akasaka, H.; Sugimoto, K.; et al. Age Group Differences in Association between IADL Decline and Depressive Symptoms in Community-Dwelling Elderly. BMC Geriatr. 2019, 19, 309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alexopoulos, G.S. Depression in the Elderly. Lancet 2005, 365, 1961–1970. [Google Scholar] [CrossRef]
- Ezeokonkwo, F.C.; Sekula, K.L.; Theeke, L.A. Loneliness in Homebound Older Adults: Integrative Literature Review. J. Gerontol. Nurs. 2021, 47, 13–20. [Google Scholar] [CrossRef]
- Depression. Available online: https://www.nimh.nih.gov/health/topics/depression (accessed on 2 December 2022).
- Blazer, D.G. Depression in Late Life: Review and Commentary. J. Gerontol. A Biol. Sci. Med. Sci. 2003, 58, M249–M265. [Google Scholar] [CrossRef]
- Smith, K. Mental Health: A World of Depression. Nature 2014, 515, 180–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faravelli, C.; Alessandra Scarpato, M.; Castellini, G.; Lo Sauro, C. Gender Differences in Depression and Anxiety: The Role of Age. Psychiatry Res. 2013, 210, 1301–1303. [Google Scholar] [CrossRef] [PubMed]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef] [PubMed]
- Ströhle, A. Physical Activity, Exercise, Depression and Anxiety Disorders. J. Neural Transm. 2009, 116, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Esposito, L.; Villaseñor, A. Depression and Economic Status: Evidence for Non-Linear Patterns in Women from Mexico. J. Ment. Health 2018, 27, 529–551. [Google Scholar] [CrossRef]
- Sbolli, M.; Fiuzat, M.; Cani, D.; O’Connor, C.M. Depression and Heart Failure: The Lonely Comorbidity. Eur. J. Heart Fail. 2020, 22, 2007–2017. [Google Scholar] [CrossRef]
- Wu, Y.; Zhu, B.; Chen, Z.; Duan, J.; Luo, A.; Yang, L.; Yang, C. New Insights into the Comorbidity of Coronary Heart Disease and Depression. Curr. Probl. Cardiol. 2021, 46, 100413. [Google Scholar] [CrossRef]
- Aldabayan, Y.S.; Alqahtani, J.S.; Al Rajeh, A.M.; Abdelhafez, A.I.; Siraj, R.A.; Thirunavukkarasu, V.; Aldhahir, A.M. Prevalence and Predictors of Sleep Disturbance, Anxiety and Depression among Patients with Chronic Respiratory Diseases. Int. J. Environ. Res. Public Health 2022, 19, 12819. [Google Scholar] [CrossRef]
- Palmer, S.; Vecchio, M.; Craig, J.C.; Tonelli, M.; Johnson, D.W.; Nicolucci, A.; Pellegrini, F.; Saglimbene, V.; Logroscino, G.; Fishbane, S.; et al. Prevalence of Depression in Chronic Kidney Disease: Systematic Review and Meta-Analysis of Observational Studies. Kidney Int. 2013, 84, 179–191. [Google Scholar] [CrossRef] [Green Version]
- Linden, W.; Vodermaier, A.; Mackenzie, R.; Greig, D. Anxiety and Depression after Cancer Diagnosis: Prevalence Rates by Cancer Type, Gender, and Age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef]
- Wang, Y.-H.; Li, J.-Q.; Shi, J.-F.; Que, J.-Y.; Liu, J.-J.; Lappin, J.M.; Leung, J.; Ravindran, A.V.; Chen, W.-Q.; Qiao, Y.-L.; et al. Depression and Anxiety in Relation to Cancer Incidence and Mortality: A Systematic Review and Meta-Analysis of Cohort Studies. Mol. Psychiatry 2020, 25, 1487–1499. [Google Scholar] [CrossRef]
- Jonas, J.B.; Wei, W.B.; Xu, L.; Rietschel, M.; Streit, F.; Wang, Y.X. Self-Rated Depression and Eye Diseases: The Beijing Eye Study. PLoS ONE 2018, 13, e0202132. [Google Scholar] [CrossRef] [PubMed]
- Vieira, G.C.F.; Rodrigues, B.R.d.O.; da Cunha, C.E.X.; de Morais, G.B.; Ferreira, L.H.R. de M.; Ribeiro, M.V.M.R. Depression and Dry Eye: A Narrative Review. Rev. Assoc. Med. Bras. 2021, 67, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Cosh, S.; Helmer, C.; Delcourt, C.; Robins, T.G.; Tully, P.J. Depression in Elderly Patients with Hearing Loss: Current Perspectives. Clin. Interv. Aging 2019, 14, 1471–1480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutherford, B.R.; Brewster, K.; Golub, J.S.; Kim, A.H.; Roose, S.P. Sensation and Psychiatry: Linking Age-Related Hearing Loss to Late-Life Depression and Cognitive Decline. Am. J. Psychiatry 2018, 175, 215–224. [Google Scholar] [CrossRef] [Green Version]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a Specific Risk Factor for Depressive Symptoms: Cross-Sectional and Longitudinal Analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, Depression, Loneliness and Social Network in the Elderly: Longitudinal Associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2019, 246, 82–88. [Google Scholar] [CrossRef] [Green Version]
- Erzen, E.; Çikrikci, Ö. The Effect of Loneliness on Depression: A Meta-Analysis. Int. J. Soc. Psychiatry 2018, 64, 427–435. [Google Scholar] [CrossRef]
- Lee, S.L.; Pearce, E.; Ajnakina, O.; Johnson, S.; Lewis, G.; Mann, F.; Pitman, A.; Solmi, F.; Sommerlad, A.; Steptoe, A.; et al. The Association between Loneliness and Depressive Symptoms among Adults Aged 50 Years and Older: A 12-Year Population-Based Cohort Study. Lancet Psychiatry 2021, 8, 48–57. [Google Scholar] [CrossRef]
- Anme, T.; Shimada, C. Social interaction and mortality in a five year longitudinal study of the elderly. Nihon Koshu Eisei Zasshi 2000, 47, 127–133. [Google Scholar]
- Cacioppo, J.T.; Hawkley, L.C. Perceived Social Isolation and Cognition. Trends Cogn. Sci. 2009, 13, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.J.; Harwood, R.H.; Blizard, R.A.; Thomas, A.; Mann, A.H. Social Support Deficits, Loneliness and Life Events as Risk Factors for Depression in Old Age. The Gospel Oak Project VI. Psychol. Med. 1997, 27, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-Y.S.; Goldstein, S.E.; Dik, B.J.; Rodas, J.M. Sources of Social Support and Gender in Perceived Stress and Individual Adjustment among Latina/o College-Attending Emerging Adults. Cultur. Divers. Ethnic Minor. Psychol. 2020, 26, 134–147. [Google Scholar] [CrossRef] [PubMed]
- Arslantaş, H.; Adana, F.; Abacigil Ergin, F.; Kayar, D.; Acar, G. Loneliness in Elderly People, Associated Factors and Its Correlation with Quality of Life: A Field Study from Western Turkey. Iran. J. Public Health 2015, 44, 43–50. [Google Scholar] [PubMed]
- Seabrook, E.M.; Kern, M.L.; Rickard, N.S. Social Networking Sites, Depression, and Anxiety: A Systematic Review. JMIR Ment. Health 2016, 3, e50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, X.; Yip, B.H.K.; Mak, A.D.P.; Zhang, D.; Lee, E.K.P.; Wong, S.Y.S. The Differential Effects of Social Media on Depressive Symptoms and Suicidal Ideation among the Younger and Older Adult Population in Hong Kong during the COVID-19 Pandemic: Population-Based Cross-Sectional Survey Study. JMIR Public Health Surveill. 2021, 7, e24623. [Google Scholar] [CrossRef] [PubMed]
- Park, N.S.; Lee, B.S.; Chiriboga, D.A.; Chung, S. Loneliness as a Mediator in the Relationship between Social Engagement and Depressive Symptoms: Age Differences among Community-Dwelling Korean Adults. Health Soc. Care Community 2019, 27, 706–716. [Google Scholar] [CrossRef]
- Burholt, V.; Scharf, T. Poor Health and Loneliness in Later Life: The Role of Depressive Symptoms, Social Resources, and Rural Environments. J. Gerontol. B Psychol. Sci. Soc. Sci. 2014, 69, 311–324. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Gou, Z.; Zuo, J. Social Support Mediates Loneliness and Depression in Elderly People. J. Health Psychol. 2016, 21, 750–758. [Google Scholar] [CrossRef]
- Zhao, X.; Zhang, D.; Wu, M.; Yang, Y.; Xie, H.; Li, Y.; Jia, J.; Su, Y. Loneliness and Depression Symptoms among the Elderly in Nursing Homes: A Moderated Mediation Model of Resilience and Social Support. Psychiatry Res. 2018, 268, 143–151. [Google Scholar] [CrossRef]
- Gray, T.F.; Azizoddin, D.R.; Nersesian, P.V. Loneliness among Cancer Caregivers: A Narrative Review. Palliat. Support. Care 2020, 18, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Nersesian, P.V.; Han, H.-R.; Yenokyan, G.; Blumenthal, R.S.; Nolan, M.T.; Hladek, M.D.; Szanton, S.L. Loneliness in Middle Age and Biomarkers of Systemic Inflammation: Findings from Midlife in the United States. Soc. Sci. Med. 2018, 209, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Vingeliene, S.; Hiyoshi, A.; Lentjes, M.; Fall, K.; Montgomery, S. Longitudinal Analysis of Loneliness and Inflammation at Older Ages: English Longitudinal Study of Ageing. Psychoneuroendocrinology 2019, 110, 104421. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Sakata, R.; Murayama, C.; Yamaguchi, M.; Matsuoka, Y.; Kondo, N. Changes in Work and Life Patterns Associated with Depressive Symptoms during the COVID-19 Pandemic: An Observational Study of Health App (CALO Mama) Users. Occup. Environ. Med. 2021, 78, 632–637. [Google Scholar] [CrossRef] [PubMed]
- Tsoi, K.K.F.; Chan, J.Y.C.; Hirai, H.W.; Wong, S.Y.S. Comparison of Diagnostic Performance of Two-Question Screen and 15 Depression Screening Instruments for Older Adults: Systematic Review and Meta-Analysis. Br. J. Psychiatry 2017, 210, 255–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noguchi, T.; Hayashi, T.; Kubo, Y.; Tomiyama, N.; Ochi, A.; Hayashi, H. Association between Family Caregivers and Depressive Symptoms among Community-Dwelling Older Adults in Japan: A Cross-Sectional Study during the COVID-19 Pandemic. Arch. Gerontol. Geriatr. 2021, 96, 104468. [Google Scholar] [CrossRef]
- Anme, T.; Shinohara, R.; Sugisawa, Y.; Itoh, S. Social interaction and mortality: A seven-year longitudinal study of elderly people. Nihon Koshu Eisei Zasshi 2006, 53, 681–687. [Google Scholar]
- Jiao, D.; Watanabe, K.; Sawada, Y.; Tanaka, E.; Watanabe, T.; Tomisaki, E.; Ito, S.; Okumura, R.; Kawasaki, Y.; Anme, T. Multimorbidity and Functional Limitation: The Role of Social Relationships. Arch. Gerontol. Geriatr. 2021, 92, 104249. [Google Scholar] [CrossRef]
- Jiao, D.; Watanabe Miura, K.; Sawada, Y.; Tanaka, E.; Watanabe, T.; Tomisaki, E.; Ito, S.; Okumura, R.; Kawasaki, Y.; Anme, T. Changes in Social Relationships and Physical Functions in Community-Dwelling Older Adults. J. Nurs. Res. 2022, 30, e228. [Google Scholar] [CrossRef]
- Watanabe, K.; Tanaka, E.; Watanabe, T.; Chen, W.; Wu, B.; Ito, S.; Okumura, R.; Anme, T. Association between the Older Adults’ Social Relationships and Functional Status in Japan. Geriatr. Gerontol. Int. 2017, 17, 1522–1526. [Google Scholar] [CrossRef]
- Ge, L.; Yap, C.W.; Ong, R.; Heng, B.H. Social Isolation, Loneliness and Their Relationships with Depressive Symptoms: A Population-Based Study. PLoS ONE 2017, 12, e0182145. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, L.M.; Gullone, E. The Clinical Significance of Loneliness: A Literature Review. Clin. Psychol. Rev. 2006, 26, 695–718. [Google Scholar] [CrossRef]
- Losecaat Vermeer, A.B.; Muth, A.; Terenzi, D.; Park, S.Q. Curiosity for Information Predicts Wellbeing Mediated by Loneliness during COVID-19 Pandemic. Sci. Rep. 2022, 12, 7771. [Google Scholar] [CrossRef]
- O’Day, E.B.; Heimberg, R.G. Social Media Use, Social Anxiety, and Loneliness: A Systematic Review. Comput. Hum. Behav. Rep. 2021, 3, 100070. [Google Scholar] [CrossRef]
- Nikoui, V.; Ostadhadi, S.; Azhand, P.; Zolfaghari, S.; Amiri, S.; Foroohandeh, M.; Motevalian, M.; Sharifi, A.M.; Bakhtiarian, A. The Effect of Nitrazepam on Depression and Curiosity in Behavioral Tests in Mice: The Role of Potassium Channels. Eur. J. Pharmacol. 2016, 791, 369–376. [Google Scholar] [CrossRef]

| Item | Category | n | % | Depression Symptom | p | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Yes | % | No | % | |||||||
| Age | 65–74 | 343 | 61.8 | 113 | 32.9 | 230 | 67.1 | 0.657 | ||
| ≥75 | 212 | 38.2 | 66 | 31.1 | 146 | 68.9 | ||||
| Sex | Men | 271 | 48.8 | 86 | 31.7 | 185 | 68.3 | 0.799 | ||
| Women | 284 | 51.2 | 93 | 32.7 | 191 | 67.3 | ||||
| Exercise | Yes | 325 | 58.6 | 95 | 29.2 | 230 | 70.8 | 0.070 | ||
| No | 230 | 41.4 | 84 | 36.5 | 146 | 63.5 | ||||
| Alcohol consumption | Daily | 120 | 21.6 | 32 | 26.7 | 88 | 71.3 | 0.139 | ||
| Non-daily | 435 | 78.4 | 147 | 33.8 | 288 | 66.2 | ||||
| Smoking | Daily | 67 | 12.1 | 17 | 25.4 | 50 | 74.6 | 0.199 | ||
| Non-daily | 488 | 87.9 | 162 | 33.2 | 326 | 66.8 | ||||
| Economic | Not good | 129 | 23.2 | 57 | 44.2 | 72 | 55.8 | 0.004 | ||
| Normal | 382 | 68.8 | 109 | 28.5 | 273 | 71.5 | ||||
| Good | 44 | 7.9 | 13 | 18.5 | 31 | 81.5 | ||||
| Hypertension | Yes | 247 | 44.5 | 75 | 30.4 | 172 | 69.6 | 0.394 | ||
| No | 308 | 55.5 | 104 | 33.8 | 204 | 66.2 | ||||
| Stroke | Yes | 29 | 5.2 | 9 | 31.0 | 20 | 69.0 | 0.885 | ||
| No | 526 | 94.8 | 170 | 32.3 | 356 | 67.7 | ||||
| Heart Disease | Yes | 46 | 8.3 | 21 | 45.7 | 25 | 54.3 | 0.042 | ||
| No | 509 | 91.7 | 158 | 31.0 | 351 | 69.0 | ||||
| Diabetes | Yes | 86 | 15.5 | 28 | 32.6 | 58 | 67.4 | 0.947 | ||
| No | 469 | 84.5 | 151 | 32.2 | 318 | 67.8 | ||||
| Hyperlipidemia | Yes | 65 | 11.7 | 23 | 35.4 | 42 | 64.6 | 0.565 | ||
| No | 490 | 88.3 | 156 | 31.8 | 334 | 68.2 | ||||
| Respiratory disease | Yes | 27 | 49 | 14 | 51.9 | 13 | 48.1 | 0.026 | ||
| No | 528 | 95.1 | 165 | 31.3 | 363 | 68.7 | ||||
| Stomach disease | Yes | 19 | 3.4 | 10 | 52.6 | 9 | 47.4 | 0.053 | ||
| No | 536 | 96.6 | 169 | 31.5 | 367 | 68.5 | ||||
| Kidney disease | Yes | 40 | 7.2 | 22 | 55.0 | 18 | 45.0 | 0.001 | ||
| No | 515 | 92.8 | 157 | 30.5 | 358 | 69.5 | ||||
| Muscle disease | Yes | 58 | 10.5 | 24 | 41.4 | 34 | 58.6 | 0.116 | ||
| No | 497 | 89.5 | 155 | 31.2 | 342 | 68.8 | ||||
| Cancers | Yes | 21 | 3.8 | 11 | 52.4 | 10 | 47.6 | 0.044 | ||
| No | 534 | 96.2 | 169 | 31.6 | 366 | 68.4 | ||||
| Immune diseases | Yes | 9 | 1.6 | 2 | 22.2 | 7 | 77.8 | 0.516 | ||
| No | 546 | 98.4 | 177 | 32.4 | 369 | 67.6 | ||||
| Dementia | Yes | 11 | 2 | 6 | 51.5 | 5 | 48.5 | 0.110 | ||
| No | 544 | 98 | 173 | 31.8 | 371 | 68.2 | ||||
| Parkinson’s disease | Yes | 4 | 0.7 | 3 | 75.0 | 1 | 25.0 | 0.066 | ||
| No | 511 | 99.3 | 176 | 34.4 | 375 | 65.6 | ||||
| Eye diseases | Yes | 126 | 22.7 | 55 | 43.7 | 71 | 56.3 | 0.002 | ||
| No | 429 | 77.3 | 124 | 28.9 | 305 | 71.1 | ||||
| Ear diseases | Yes | 35 | 6.3 | 22 | 62.9 | 13 | 37.1 | <0.001 | ||
| No | 520 | 93.7 | 157 | 30.2 | 363 | 69.8 | ||||
| a | b | c | d | e | f | |
|---|---|---|---|---|---|---|
| Loneliness | 1 | |||||
| Depression symptoms | 0.296 ** | 1 | ||||
| Social curiosity | 0.244 ** | 0.195 ** | 1 | |||
| Independence | 0.138 ** | 0.121 ** | 0.556 ** | 1 | ||
| Interaction | 0.104 * | 0.130 ** | 0.360 ** | 0.329 ** | 1 | |
| Participation | 0.179 ** | 0.177 ** | 0.469 ** | 0.434 ** | 0.406 ** | 1 |
| Feeling safe | 0.062 | 0.111 ** | 0.110 ** | 0.153 ** | 0.311 ** | 0.197 ** |
| Outcome | Variable | B | SE |
|---|---|---|---|
| Social curiosity | Loneliness | 0.280 ** | 0.101 |
| Depression symptom | Social curiosity | 0.317 ** | 0.093 |
| Depression symptom | Loneliness | 1.235 ** | 0.218 |
| R2 | 0.303 | ||
| F | 10.504 | ||
| Independence | Loneliness | 0.080 | 0.045 |
| Depression symptom | Independence | 0.414 * | 0.200 |
| Depression symptom | Loneliness | 1.268 ** | 0.216 |
| R2 | 0.145 | ||
| F | 4.107 | ||
| Interaction | Loneliness | 0.055 | 0.043 |
| Depression symptom | Interaction | 0.439 * | 0.212 |
| Depression symptom | Loneliness | 1.285 ** | 0.217 |
| R2 | 0.059 | ||
| F | 1.526 | ||
| Participation | Loneliness | 0.195 ** | 0.070 |
| Depression symptom | Participation | 0.367 ** | 0.134 |
| Depression symptom | Loneliness | 1.242 ** | 0.218 |
| R2 | 0.153 | ||
| F | 4.382 | ||
| Feeling safe | Loneliness | 0.063 | 0.037 |
| Depression symptom | Feeling safe | 0.396 | 0.245 |
| Depression symptom | Loneliness | 1.273 | 0.216 |
| R2 | 0.063 | ||
| F | 1.624 |
| Outcome | Variable | B | SE | t/z | LLCI | ULCI |
|---|---|---|---|---|---|---|
| Social curiosity | Loneliness | 0.191 * | 0.088 | 2.170 | 0.018 | 0.363 |
| Independence | 1.235 ** | 0.103 | 11.959 | 1.033 | 1.438 | |
| Loneliness × Independence | −0.375 * | 0.167 | −2.243 | −0.703 | −0.047 | |
| Depression symptom | Loneliness | 1.239 ** | 0.220 | 5.616 | 0.807 | 1.672 |
| Social curiosity | 0.287 ** | 0.109 | 2.647 | 0.075 | 0.450 | |
| Independence | 0.008 | 0.610 | 0.013 | −1.187 | 1.203 | |
| Loneliness × Independence | −0.680 | 0.497 | −1.369 | −1.654 | 0.294 | |
| Social curiosity × Independence | −1.114 | 0.187 | −0.609 | −0.479 | 0.252 | |
| Social curiosity | Loneliness | 0.237 * | 0.095 | 2.487 | 0.050 | 0.424 |
| Interaction | 0.674 ** | 0.138 | 4.897 | 0.404 | 0.945 | |
| Loneliness × Interaction | 0.233 | 0.193 | 1.207 | −0.146 | 0.612 | |
| Depression symptom | Loneliness | 1.242 ** | 0.221 | 5.607 | 0.808 | 1.676 |
| Social curiosity | 0.306 ** | 0.104 | 2.933 | 0.101 | 0.511 | |
| Interaction | 0.770 * | 0.381 | 2.020 | 0.023 | 1.516 | |
| Loneliness × Interaction | −1.161 * | 0.502 | −2.314 | −2.144 | −0.176 | |
| Social curiosity × Interaction | −0.050 | 0.148 | −0.336 | −0.341 | 0.241 | |
| Social curiosity | Loneliness | 0.165 | 0.093 | 1.770 | −0.018 | 0.348 |
| Participation | 0.680 ** | 0.077 | 8.781 | 0.528 | 0.832 | |
| Loneliness × Participation | −0.241 * | 0.110 | −2.187 | −0.458 | −0.025 | |
| Depression symptom | Loneliness | 1.204 ** | 0.220 | 5.466 | 0.772 | 1.635 |
| Social curiosity | 0.254 * | 0.107 | 2.374 | 0.044 | 0.463 | |
| Participation | 0.363 | 0.218 | 1.665 | −0.064 | 0.791 | |
| Loneliness × Participation | −0.290 | 0.272 | −1.067 | −0.823 | 0.243 | |
| Social curiosity × Participation | 0.006 | 0.080 | 0.071 | −0.150 | 0.161 | |
| Social curiosity | Loneliness | 0.259 ** | 0.100 | 2.587 | 0.062 | 0.456 |
| Feeling safe | 0.150 | 0.166 | 0.904 | −0.176 | 0.472 | |
| Loneliness × Feeling safe | 0.420 | 0.231 | 1.819 | −0.334 | 0.873 | |
| Depression symptom | Loneliness | 1.194 ** | 0.220 | 5.437 | 0.764 | 1.625 |
| Social curiosity | 0.323 ** | 0.096 | 3.372 | 0.135 | 0.511 | |
| Feeling safe | 0.478 | 0.361 | 1.327 | −0.228 | 1.185 | |
| Loneliness × Feeling safe | −0.201 | 0.496 | −0.405 | −1.174 | 0.772 | |
| Social curiosity × Feeling safe | 0.231 | 0.181 | 1.278 | −0.123 | 0.586 |
| Outcome | Variable | B | SE | t/z | LLCI | ULCI |
|---|---|---|---|---|---|---|
| Participation | Loneliness | 0.117 | 0.065 | 1.800 | −0.011 | 0.245 |
| Social curiosity | 0.300 ** | 0.035 | 8.641 | 0.232 | 0.368 | |
| Loneliness × Social curiosity | −0.064 | 0.050 | −1.282 | −0.162 | 0.034 | |
| Depression symptom | Loneliness | 1.208 ** | 0.220 | 5.484 | 0.776 | 1.640 |
| Participation | 0.224 | 0.165 | 1.355 | −0.100 | 0.548 | |
| Social curiosity | 0.313 * | 0.130 | 2.409 | 0.058 | 0.568 | |
| Loneliness × Social curiosity | −0.145 | 0.174 | 0.834 | −0.486 | 0.196 | |
| Participation × Social curiosity | 0.001 | 0.079 | 0.013 | −0.154 | 0.156 | |
| Participation | Loneliness | 0.151 * | 0.066 | 2.292 | 0.022 | 0.280 |
| Independence | 0.643 ** | 0.077 | 8.329 | 0.492 | 0.795 | |
| Loneliness × Independence | −0.256 * | 0.125 | −2.049 | −0.501 | −0.011 | |
| Depression symptom | Loneliness | 1.245 ** | 0.221 | 5.648 | 0.813 | 1.677 |
| Participation | 0.297 * | 0.146 | 2.031 | 0.010 | 0.584 | |
| Independence | 0.484 | 0.368 | 1.316 | −0.237 | 1.204 | |
| Loneliness × Independence | −0.808 | 0.477 | −1.695 | −1.743 | 0.127 | |
| Participation × Independence | −0.029 | 0.197 | −0.146 | −0.415 | 0.358 | |
| Participation | Loneliness | 0.161 * | 0.065 | 2.466 | 0.033 | 0.289 |
| Interaction | 0.652 ** | 0.094 | 6.926 | 0.467 | 0.836 | |
| Loneliness × Interaction | −0.053 | 0.132 | −0.402 | −0.312 | 0.206 | |
| Depression symptom | Loneliness | 1.238 ** | 0.220 | 5.631 | 0.807 | 1.670 |
| Participation | 0.323 * | 0.153 | 2.115 | 0.024 | 0.623 | |
| Interaction | 0.798 * | 0.385 | 2.073 | 0.044 | 1.553 | |
| Loneliness × Interaction | −0.949 * | 0.479 | −1.981 | −1.888 | −0.010 | |
| Participation × Interaction | 0.055 | 0.188 | 0.291 | −0.314 | 0.423 | |
| Participation | Loneliness | 0.173 * | 0.069 | 2.515 | 0.038 | 0.309 |
| Feeling safe | 0.238 | 0.114 | 2.081 | 0.013 | 0.462 | |
| Loneliness × Feeling safe | 0.265 | 0.159 | 1.666 | −0.047 | 0.577 | |
| Depression symptom | Loneliness | 1.193 ** | 0.219 | 5.436 | 0.763 | 1.623 |
| Participation | 0.405 ** | 0.142 | 2.854 | 0.127 | 0.684 | |
| Feeling safe | 0.570 | 0.377 | 1.513 | −0.168 | 1.308 | |
| Loneliness × Feeling safe | −0.095 | 0.510 | −0.185 | −1.094 | 0.905 | |
| Participation × Feeling safe | 0.515 * | 0.248 | 2.074 | 0.028 | 1.001 |
| Mediator | Moderator | B | SE | LLCI | ULCI |
|---|---|---|---|---|---|
| Social curiosity | −1 SD independence | 0.122 | 0.067 | 0.015 | 0.274 |
| Mean independence | 0.060 | 0.036 | 0.003 | 0.145 | |
| 1 SD independence | 0.043 | 0.034 | −0.015 | 0.121 | |
| Social curiosity | −1 SD participation | 0.114 | 0.064 | 0.015 | 0.260 |
| Mean participation | 0.052 | 0.036 | −0.007 | 0.133 | |
| 1 SD participation | 0.005 | 0.038 | −0.075 | 0.076 | |
| Participation | −1 SD independence | 0.104 | 0.068 | 0.006 | 0.266 |
| Mean independence | 0.055 | 0.036 | 0.003 | 0.140 | |
| 1 SD independence | 0.042 | 0.032 | −0.008 | 0.118 | |
| Participation | −1 SD feeling safe | 0.038 | 0.043 | −0.037 | 0.136 |
| Mean feeling safe | 0.079 | 0.045 | 0.012 | 0.185 | |
| 1 SD feeling safe | 0.09 | 0.049 | 0.017 | 0.204 | |
| No mediator | −1 SD interaction | 1.738 | 0.314 | 1.112 | 2.354 |
| Mean interaction | 1.283 | 0.218 | 0.856 | 1.710 | |
| 1 SD interaction | 1.122 | 0.229 | 0.673 | 1.571 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Jiao, D.; Yang, M.; Cui, M.; Li, X.; Zhu, Z.; Sawada, Y.; Watanabe Miura, K.; Watanabe, T.; Tanaka, E.; et al. Role of Multifaceted Social Relationships on the Association of Loneliness with Depression Symptoms: A Moderated Mediation Analysis. Healthcare 2023, 11, 124. https://doi.org/10.3390/healthcare11010124
Liu Y, Jiao D, Yang M, Cui M, Li X, Zhu Z, Sawada Y, Watanabe Miura K, Watanabe T, Tanaka E, et al. Role of Multifaceted Social Relationships on the Association of Loneliness with Depression Symptoms: A Moderated Mediation Analysis. Healthcare. 2023; 11(1):124. https://doi.org/10.3390/healthcare11010124
Chicago/Turabian StyleLiu, Yang, Dandan Jiao, Mengjiao Yang, Mingyu Cui, Xiang Li, Zhu Zhu, Yuko Sawada, Kumi Watanabe Miura, Taeko Watanabe, Emiko Tanaka, and et al. 2023. "Role of Multifaceted Social Relationships on the Association of Loneliness with Depression Symptoms: A Moderated Mediation Analysis" Healthcare 11, no. 1: 124. https://doi.org/10.3390/healthcare11010124
APA StyleLiu, Y., Jiao, D., Yang, M., Cui, M., Li, X., Zhu, Z., Sawada, Y., Watanabe Miura, K., Watanabe, T., Tanaka, E., & Anme, T. (2023). Role of Multifaceted Social Relationships on the Association of Loneliness with Depression Symptoms: A Moderated Mediation Analysis. Healthcare, 11(1), 124. https://doi.org/10.3390/healthcare11010124







