The Effects of Abdominal Hollowing and Bracing Maneuvers on Trunk Muscle Activity and Pelvic Rotation Angle during Leg Pull Front Pilates Exercise
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Surface Electromyography and Data Processing
2.3. Smart Phone-Based Measurement Tool
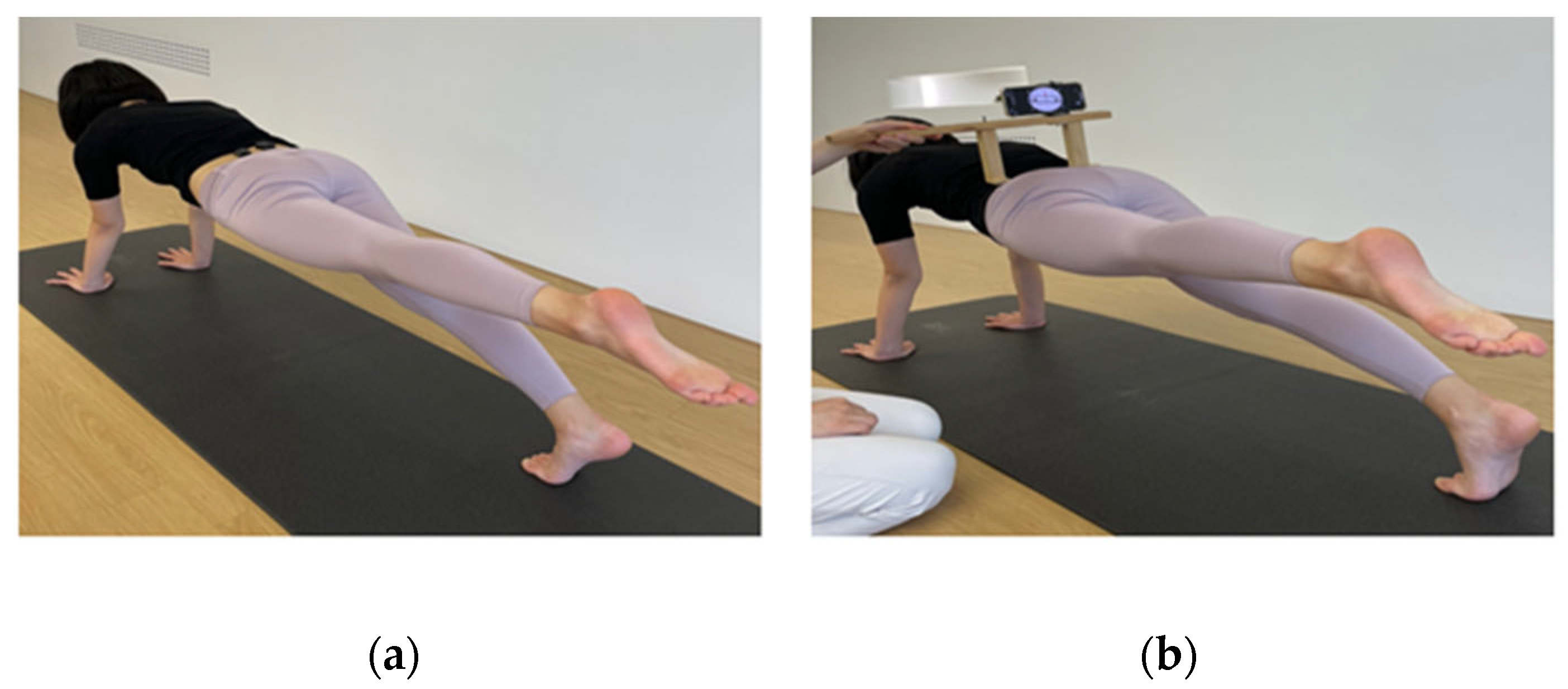
2.4. Pilates Exercises
2.5. Experimental Procedures
2.6. Statistical Analysis
3. Results
3.1. Electromyographic Activity of the Trunk Muscles
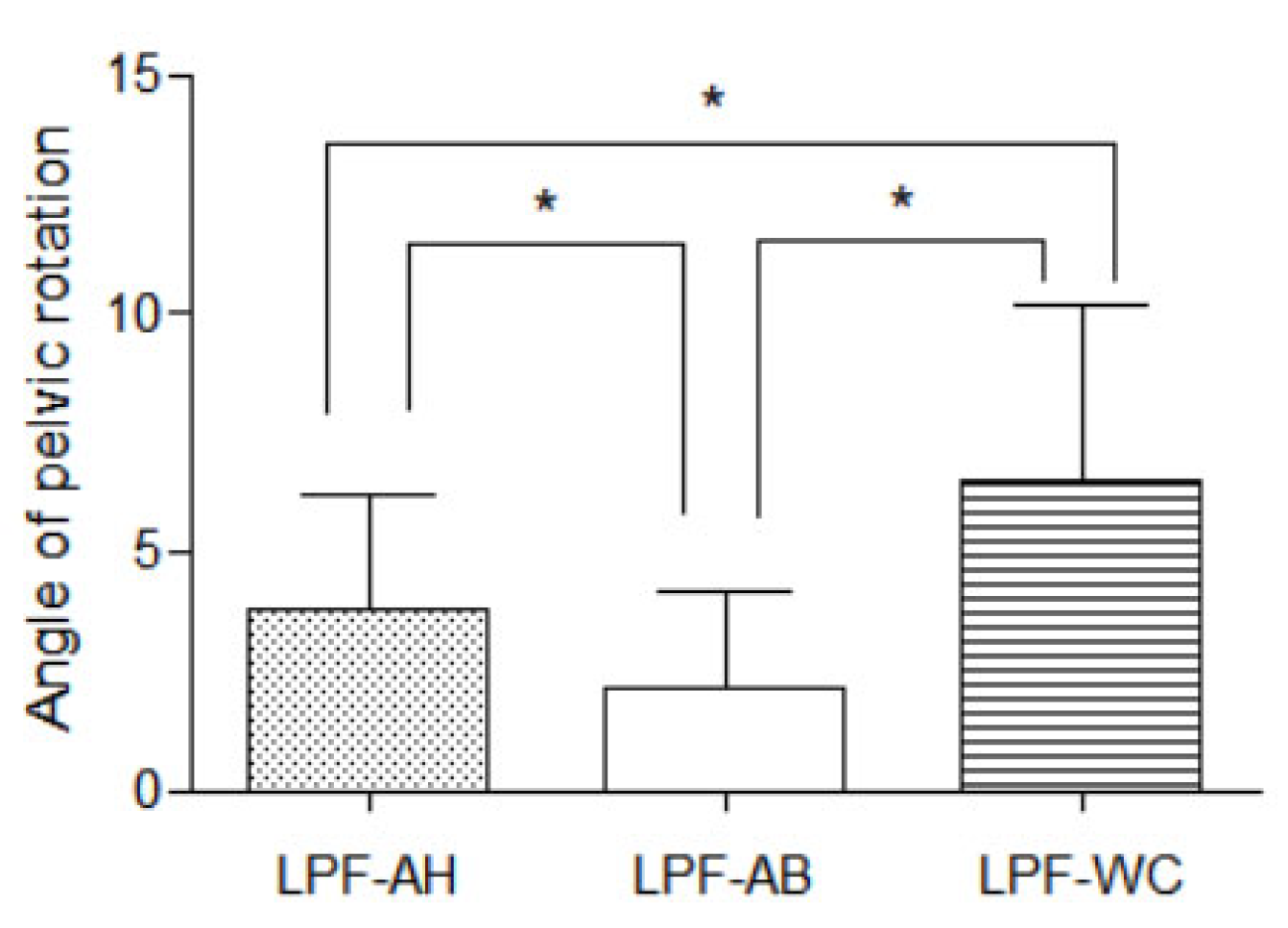
3.2. Angle of Pelvic Rotation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Richardson, C.A.; Hodges, P.W.; Hides, A.P. Therapeutic Exercise for Lumbopelvic Stabilization: A Motor Control Approach for the Treatment and Prevention of Low Back Pain, 2nd ed.; Churchill Livingstone: Edinburgh, UK, 2004; pp. 111–114. [Google Scholar]
- Rydeard, R.; Leger, A.; Smith, D. Pilates-based therapeutic exercise: Effect on subjects with nonspecific chronic low back pain and functional disability: A randomized controlled trial. J. Orthop. Sports Phys. Ther. 2006, 36, 472–484. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Ferreira, A.; Fernandes, J.; Laranjo, L.; Bernardo, L.M.; Silva, A. A systematic review of the effects of pilates method of exercise in healthy people. Arch. Phys. Med. Rehabil. 2011, 92, 2071–2081. [Google Scholar] [CrossRef] [PubMed]
- Phrompaet, S.; Paungmali, A.; Pirunsan, U.; Sitilertpisan, P. Effects of pilates training on lumbo-pelvic stability and flexibility. Asian J. Sports Med. 2011, 2, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Snarr, R.L.; Esco, M.R. Electromyographical comparison of plank variations performed with and without instability devices. J. Strength Cond. Res. 2014, 28, 3298–3305. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.K.; Kang, M.H.; Kim, J.W.; Kim, Y.G.; Park, J.H.; Oh, J.S. Effects of non-paretic arm exercises using a tubing band on abdominal muscle activity in stroke patients. NeuroRehabilitation 2013, 33, 605–610. [Google Scholar] [CrossRef]
- Hodges, P.; Cresswell, A.; Thorstensson, A. Preparatory trunk motion accompanies rapid upper limb movement. Exp. Brain Res. 1999, 124, 69–79. [Google Scholar] [CrossRef]
- Aruin, A.S.; Latash, M.L. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary arm movements. Exp. Brain Res. 1995, 103, 323–332. [Google Scholar] [CrossRef]
- Comerford, M.; Mottram, S. Kinetic Control: The Management of Uncontrolled Movement, 1st ed.; Churchill Livingstone: Edinburgh, UK, 2012; pp. 152–153. [Google Scholar]
- Hoffman, S.L.; Johnson, M.B.; Zou, D.; Harris-Hayes, M.; Van Dillen, L.R. Effect of classification-specific treatment on lumbopelvic motion during hip rotation in people with low back pain. Man. Ther. 2011, 16, 344–350. [Google Scholar] [CrossRef]
- Hoffman, S.L.; Johnson, M.B.; Zou, D.; Van Dillen, L.R. Sex differences in lumbopelvic movements during hip medial rotation in people with chronic low back pain. Arch. Phys. Med. Rehabil. 2011, 92, 1053–1059. [Google Scholar] [CrossRef]
- Roussel, N.A.; Nijs, J.; Mottram, S.; Van Moorsel, A.; Truijen, S.; Stassijns, G. Altered lumbopelvic movement control but not generalized hypermobility is associated with increased injury in dancers. A prospective study. Man. Ther. 2009, 14, 630–635. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine 1996, 21, 2640–2650. [Google Scholar] [CrossRef] [PubMed]
- Kisner, C.; Colby, L.A.; Borstad, J. Therapeutic Exercise: Foundations and Techniques; Fa Davis: Philadelphia, PA, USA, 2017; pp. 517–518. [Google Scholar]
- McGill, S.M.; Grenier, S.; Kavcic, N.; Cholewicki, J. Coordination of muscle activity to assure stability of the lumbar spine. J. Electromyogr. Kinesiol. 2003, 13, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Vera-Garcia, F.J.; Elvira, J.L.; Brown, S.H.; McGill, S.M. Effects of abdominal stabilization maneuvers on the control of spine motion and stability against sudden trunk perturbations. J. Electromyogr. Kinesiol. 2007, 17, 556–567. [Google Scholar] [CrossRef] [PubMed]
- Cynn, H.S.; Oh, J.S.; Kwon, O.Y.; Yi, C.H. Effects of lumbar stabilization using a pressure biofeedback unit on muscle activity and lateral pelvic tilt during hip abduction in sidelying. Arch. Phys. Med. Rehabil. 2006, 87, 1454–1458. [Google Scholar] [CrossRef] [PubMed]
- Ko, M.J.; Oh, J.S.; An, D.H.; Yoo, W.G.; Noh, K.H.; Kang, M.H. Effects of the abdominal drawing-in maneuver on hamstring rotational activity and pelvic stability in females. J. Back Musculoskelet. Rehabil. 2022, 35, 413–419. [Google Scholar] [CrossRef]
- Liebenson, C.; Karpowicz, A.M.; Brown, S.H.; Howarth, S.J.; McGill, S.M. The active straight leg raise test and lumbar spine stability. PM R 2009, 1, 530–535. [Google Scholar] [CrossRef]
- Oh, J.S.; Cynn, H.S.; Won, J.H.; Kwon, O.Y.; Yi, C.H. Effects of performing an abdominal drawing-in maneuver during prone hip extension exercises on hip and back extensor muscle activity and amount of anterior pelvic tilt. J. Orthop. Sports Phys. Ther. 2007, 37, 320–324. [Google Scholar] [CrossRef]
- Park, K.N.; Cynn, H.S.; Kwon, O.Y.; Lee, W.H.; Ha, S.M.; Kim, S.J.; Weon, J.H. Effects of the abdominal drawing-in maneuver on muscle activity, pelvic motions, and knee flexion during active prone knee flexion in patients with lumbar extension rotation syndrome. Arch. Phys. Med. Rehabil. 2011, 92, 1477–1483. [Google Scholar] [CrossRef]
- Jung, E.J.; Sung, J.W.; Uh, I.J.; Oh, J.S. The effects of abdominal hollowing and bracing on abdominal muscle thicknesses and pelvic rotation during active straight leg raise. Isokinet. Exerc. Sci. 2022, 30, 1–6. [Google Scholar] [CrossRef]
- Stanton, T.; Kawchuk, G. The effect of abdominal stabilization contractions on posteroanterior spinal stiffness. Spine 2008, 33, 694–701. [Google Scholar] [CrossRef]
- McGalliard, M.K.; Dedrick, G.S.; Brismée, J.M.; Cook, C.E.; Apte, G.G.; Sizer, P.S., Jr. Changes in transversus abdominis thickness with use of the abdominal drawing-in maneuver during a functional task. PM R 2010, 2, 187–194. [Google Scholar] [CrossRef]
- Park, K.H.; Ha, S.M.; Kim, S.J.; Park, K.N.; Kwon, O.Y.; Oh, J.S. Effects of the pelvic rotatory control method on abdominal muscle activity and the pelvic rotation during active straight leg raising. Man. Ther. 2013, 18, 220–224. [Google Scholar] [CrossRef]
- Marshall, P.; Murphy, B. The validity and reliability of surface EMG to assess the neuromuscular response of the abdominal muscles to rapid limb movement. J. Electromyogr. Kinesiol. 2003, 13, 477–489. [Google Scholar] [CrossRef]
- Suehiro, T.; Mizutani, M.; Watanabe, S.; Ishida, H.; Kobara, K.; Osaka, H. Comparison of spine motion and trunk muscle activity between abdominal hollowing and abdominal bracing maneuvers during prone hip extension. J. Bodyw. Mov. Ther. 2014, 18, 482–488. [Google Scholar] [CrossRef]
- Arokoski, J.P.; Kankaanpää, M.; Valta, T.; Juvonen, I.; Partanen, J.; Taimela, S.; Lindgren, K.A.; Airaksinen, O. Back and hip extensor muscle function during therapeutic exercises. Arch. Phys. Med. Rehabil. 1999, 80, 842–850. [Google Scholar] [CrossRef]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles: Testing and Function, with Posture and Pain; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1993; pp. 131–176. [Google Scholar]
- Jung, S.H.; Kwon, O.Y.; Jeon, I.C.; Hwang, U.J.; Weon, J.H. Reliability and criterion validity of measurements using a smart phone-based measurement tool for the transverse rotation angle of the pelvis during single-leg lifting. Physiother. Theory Pract. 2018, 34, 58–65. [Google Scholar] [CrossRef]
- Sykes, K.; Wong, Y.M. Electrical activity of vastus medialis oblique muscle in straight leg raise exercise with different angles of hip rotation. Physiotherapy 2003, 89, 423–430. [Google Scholar] [CrossRef]
- van Deun, S.; Staes, F.F.; Stappaerts, K.H.; Janssens, L.; Levin, O.; Peers, K.K. Relationship of chronic ankle instability to muscle activation patterns during the transition from double-leg to single-leg stance. Am. J. Sports Med. 2007, 35, 274–281. [Google Scholar] [CrossRef]
- Allison, G.T.; Godfrey, P.; Robinson, G. EMG signal amplitude assessment during abdominal bracing and hollowing. J. Electromyogr. Kinesiol. 1998, 8, 51–57. [Google Scholar] [CrossRef]
- Matthijs, O.C.; Dedrick, G.S.; James, C.R.; Brismée, J.M.; Hooper, T.L.; McGalliard, M.K.; Sizer Jr, P.S. Co-contractive activation of the superficial multifidus during volitional preemptive abdominal contraction. PM R 2014, 6, 13–21. [Google Scholar] [CrossRef]
- Grenier, S.G.; McGill, S.M. Quantification of lumbar stability by using 2 different abdominal activation strategies. Arch. Phys. Med. Rehabil. 2007, 88, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Juker, D.; McGill, S.; Kropf, P. Quantitative intramuscular myoelectric activity of lumbar portions of psoas and the abdominal wall during cycling. J. Appl. Biomech. 1998, 14, 428–438. [Google Scholar] [CrossRef][Green Version]
- Hides, J.; Stanton, W.; Mendis, M.D.; Sexton, M. The relationship of transversus abdominis and lumbar multifidus clinical muscle tests in patients with chronic low back pain. Man. Ther. 2011, 16, 573–577. [Google Scholar] [CrossRef] [PubMed]
- Henry, S.M.; Westervelt, K.C. The use of real-time ultra-sound feedback in teaching abdominal hollowing exercises to healthy subjects. J. Orthop. Sports Phys. Ther. 2005, 35, pp. 338–345. Available online: https://www.jospt.org/doi/10.2519/jospt.2005.35.6.338 (accessed on 1 June 2005).
- García-Jaén, M.; Cortell-Tormo, J.M.; Hernández-Sánchez, S.; Tortosa-Martínez, J. Influence of Abdominal Hollowing Maneuver on the Core Musculature Activation during the Prone Plank Exercise. Int. J. Environ. Res. Public Health 2020, 17, 7410. [Google Scholar] [CrossRef] [PubMed]
- Mew, R. Comparison of changes in abdominal muscle thickness between standing and crook lying during active abdominal hollowing using ultrasound imaging. Man. Ther. 2009, 14, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.; Fede, C.; Gaudreault, N.; Porzionato, A.; Macchi, V.; de Caro, R.; Stecco, C. Anatomical and functional relationships between external abdominal oblique muscle and posterior layer of thoracolumbar fascia. Clin. Anat. 2018, 31, 1092–1098. [Google Scholar] [CrossRef]
- Panjabi, M.M. The Stabilizing System of the Spine. Part I. Function, Dysfunction, Adaptation, and Enhancement. J. Spinal Disord. 1992, 5, 383–389. [Google Scholar] [CrossRef]
- Chanthapetch, P.; Kanlayanaphotporn, R.; Gaogasigam, C.; Chiradejnant, A. Abdominal muscle activity during abdominal hollowing in four starting positions. Man. Ther. 2009, 14, 642–646. [Google Scholar] [CrossRef]
- Beith, I.D.; Synnott, R.E.; Newman, S.A. Abdominal muscle activity during the abdominal hollowing manoeuvre in the four-point kneeling and prone positions. Man. Ther. 2001, 6, 82–87. [Google Scholar] [CrossRef]
- Urquhart, D.M.; Hodges, P.W.; Allen, T.J.; Story, I.H. Abdominal muscle recruitment during a range of voluntary exercises. Man. Ther. 2005, 10, 144–153. [Google Scholar] [CrossRef]
- Ekstrom, R.A.; Donatelli, R.A.; Carp, K.C. Electromyographic analysis of core trunk, hip, and thigh muscles during 9 rehabilitation exercises. J. Orthop. Sports Phys. Ther. 2007, 37, 754–762. [Google Scholar] [CrossRef]
- Imai, A.; Kaneoka, K.; Okubo, Y.; Shiina, I.; Tatsumura, M.; Izumi, S.; Shiraki, H. Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. J. Orthop. Sports Phys. Ther. 2010, 40, 369–375. [Google Scholar] [CrossRef]
- Okubo, Y.; Kaneoka, K.; Imai, A.; Shiina, I.; Tatsumura, M.; Izumi, S.; Miyakawa, S. Electromyographic Analysis of Transversus Abdominis and Lumbar Multifidus Using Wire Electrodes During Lumbar Stabilization Exercises. J. Orthop. Sports Phys. Ther. 2010, 40, 743–750. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Contreras, B.; Tiryaki-Sonmez, G.; Willardson, J.M.; Fontana, F. An electromyographic comparison of a modified version of the plank with a long lever and posterior tilt versus the traditional plank exercise. Sports Biomech. 2014, 13, 296–306. [Google Scholar] [CrossRef]

| Muscle Activity (%MVIC) | LPF-AH | LPF-AB | LPF-WC | f | p |
|---|---|---|---|---|---|
| Rt. TrA/IO | 58.46 ± 26.70 a,c | 42.80 ± 20.39 b | 27.23 ± 14.05 | 20.787 | <0.001 ** |
| Lt. TrA/IO | 52.90 ± 24.47 a,c | 45.88 ± 19.15 b | 34.56 ± 18.86 | 11.949 | <0.001 ** |
| Rt. EO | 42.57 ± 15.88 c | 39.89 ± 14.66 | 37.29 ± 14.27 | 5.068 | 0.018 * |
| Lt. EO | 41.00 ± 17.52 | 40.76 ± 19.42 | 37.32 ± 16.73 | 1.615 | 0.226 |
| Rt. MF | 40.48 ± 21.03 c | 42.47 ± 17.78 b | 31.29 ± 13.06 | 18.302 | <0.001 ** |
| Lt. MF | 23.00 ± 7.51 c | 28.55 ± 12.20 b | 15.93 ± 4.45 | 23.181 | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, E.-J.; Oh, J.-S. The Effects of Abdominal Hollowing and Bracing Maneuvers on Trunk Muscle Activity and Pelvic Rotation Angle during Leg Pull Front Pilates Exercise. Healthcare 2023, 11, 60. https://doi.org/10.3390/healthcare11010060
Jung E-J, Oh J-S. The Effects of Abdominal Hollowing and Bracing Maneuvers on Trunk Muscle Activity and Pelvic Rotation Angle during Leg Pull Front Pilates Exercise. Healthcare. 2023; 11(1):60. https://doi.org/10.3390/healthcare11010060
Chicago/Turabian StyleJung, Eun-Joo, and Jae-Seop Oh. 2023. "The Effects of Abdominal Hollowing and Bracing Maneuvers on Trunk Muscle Activity and Pelvic Rotation Angle during Leg Pull Front Pilates Exercise" Healthcare 11, no. 1: 60. https://doi.org/10.3390/healthcare11010060
APA StyleJung, E.-J., & Oh, J.-S. (2023). The Effects of Abdominal Hollowing and Bracing Maneuvers on Trunk Muscle Activity and Pelvic Rotation Angle during Leg Pull Front Pilates Exercise. Healthcare, 11(1), 60. https://doi.org/10.3390/healthcare11010060







