Trend of Admissions Due to Chronic Lower Respiratory Diseases: An Ecological Study
Abstract
:1. Introduction
2. Methods
2.1. Study Sources and the Population
2.2. Statistical Analysis
3. Results
3.1. Chronic Lower Respiratory Disease Admission Rate by Gender
3.2. Chronic Lower Respiratory Diseases Admission Rate by Age Group
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Cancer Institute. NCI Dictionary of Cancer Terms. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/respiratory-disease (accessed on 5 November 2022).
- British Lung Foundation. The Battle for Breath: The Impact of Lung Disease in the UK. Available online: https://www.blf.org.uk/policy/the-battle-for-breath-2016 (accessed on 5 November 2022).
- World Health Organization. ICD-10 Version: 2019. Available online: https://icd.who.int/browse10/2019/en#/J40-J47 (accessed on 5 November 2022).
- World Health Organization. Global Surveillance, Prevention and Control of CHRONIC Respiratory Diseases. Available online: https://www.who.int/publications/i/item/global-surveillance-prevention-and-control-of-chronic-respiratory-diseases (accessed on 5 November 2022).
- Pesce, G. Mortality rates for chronic lower respiratory diseases in Italy from 1979 to 2010: An age-period-cohort analysis. ERJ Open Res. 2016, 2, 00093-02015. [Google Scholar] [CrossRef] [Green Version]
- Townsend, C.M. Sabiston Textbook of Surgery E-Book: The Biological Basis of Modern Surgical Practice; Elsevier Health Sciences: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Office for National Statistics. Deaths Registered in England and Wales. Available online: https://www.ons.gov.uk/file?uri=/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathsregisteredinenglandandwalesseriesdrreferencetables/2019/finalreftables2019.xlsx (accessed on 5 November 2022).
- Wedzicha, J.A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet 2007, 370, 786–796. [Google Scholar] [CrossRef]
- Criner, G.J.; Bourbeau, J.; Diekemper, R.L.; Ouellette, D.R.; Goodridge, D.; Hernandez, P.; Curren, K.; Balter, M.S.; Bhutani, M.; Camp, P.G.; et al. Executive summary: Prevention of acute exacerbation of COPD: American college of chest physicians and canadian thoracic society guideline. Chest 2015, 147, 883–893. [Google Scholar] [CrossRef]
- Naser, A.Y.; Mansour, M.M.; Alanazi, A.F.R.; Sabha, O.; Alwafi, H.; Jalal, Z.; Paudyal, V.; Dairi, M.S.; Salawati, E.M.; Alqahtan, J.S.; et al. Hospital admission trends due to respiratory diseases in England and Wales between 1999 and 2019: An ecologic study. BMC Pulm. Med. 2021, 21, 356. [Google Scholar] [CrossRef]
- Naser, A.Y.; Alrawashdeh, H.M.; Alwafi, H.; AbuAlhommos, A.K.; Jalal, Z.; Paudyal, V.; Alsairafi, Z.K.; Salawati, E.M.; Samannodi, M.; Sweiss, K.; et al. Hospital admission trends due to viral infections characterised by skin and mucous membrane lesions in the past two decades in england and wales: An ecological study. Int. J. Environ. Res. Public Health 2021, 18, 1649. [Google Scholar] [CrossRef]
- Naser, A.Y.; Alwafi, H.; Hemmo, S.I.; Alrawashdeh, H.M.; Alqahtani, J.S.; Alghamdi, S.M.; Mustafa Ali, M.K. Trends in hospital admissions due to neoplasms in england and wales between 1999 and 2019: An ecological study. Int. J. Environ. Res. Public Health 2022, 19, 8054. [Google Scholar] [CrossRef]
- Naser, A.Y.; Dahmash, E.Z.; Al-Daghastani, T.; Alwafi, H.; Abu Hamdah, S.; Alsairafi, Z.K.; Alsaleh, F.M. An ecological analysis of hospitalization patterns for diseases of the nervous system in england and wales over the last 20 years. Healthcare 2022, 10, 1670. [Google Scholar] [CrossRef]
- Naser, A.Y.; Dahmash, E.Z.; Alqahtani, J.S.; Alsairafi, Z.K.; Alsaleh, F.M.; Alwafi, H. Trends in hospital admissions for mental, behavioural and neurodevelopmental disorders in england and wales between 1999 and 2019: An ecological study. Healthcare 2022, 10, 2191. [Google Scholar] [CrossRef]
- Naser, A.Y.; Wang, Q.; Wong, L.Y.L.; Ilomaki, J.; Bell, J.S.; Fang, G.; Wong, I.C.K.; Wei, L. Hospital admissions due to dysglycaemia and prescriptions of antidiabetic medications in england and wales: An ecological study. Diabetes Ther. 2018, 9, 153–163. [Google Scholar] [CrossRef] [Green Version]
- Alanazi, A.F.R.; Naser, A.Y.; Pakan, P.; Alanazi, A.F.; Alanazi, A.A.A.; Alsairafi, Z.K.; Alsaleh, F.M. Trends of hospital admissions due to congenital anomalies in england and wales between 1999 and 2019: An ecological study. Int. J. Environ. Res. Public Health 2021, 18, 11808. [Google Scholar] [CrossRef]
- Al-Daghastani, T.; Naser, A.Y. Hospital admission profile related to poisoning by, adverse effect of and underdosing of psychotropic drugs in England and Wales: An ecological study. Saudi Pharm. J. 2022, 30, 1262–1272. [Google Scholar] [CrossRef] [PubMed]
- Alrawashdeh, H.M.; Naser, A.Y.; Alwafi, H.; AbuAlhommos, A.K.; Jalal, Z.; Paudyal, V.; Abdulmannan, D.M.; Hassanin, F.F.; Hemmo, S.I.; Al Sarireh, F. Trends in hospital admission due to diseases of the eye and adnexa in the past two decades in england and wales: An ecological study. Int. J. Gen. Med. 2022, 15, 1097–1110. [Google Scholar] [CrossRef]
- Al-shehri, H.; Dahmash, D.T.; Rochow, N.; Alturki, B.; Alrajhi, D.; Alayed, F.; Alhazani, F.; Alsuhibany, H.; Naser, A.Y. Hospital admission profile of neonates for conditions originating in the perinatal period in england and wales between 1999–2020: An ecological study. Int. J. Gen. Med. 2022, 15, 1973–1984. [Google Scholar] [CrossRef]
- Hemmo, S.I.; Naser, A.Y.; Alwafi, H.; Mansour, M.M.; Alanazi, A.F.R.; Jalal, Z.; Alsairafi, Z.K.; Paudyal, V.; Alomari, E.; Al-Momani, H.; et al. Hospital admissions due to ischemic heart diseases and prescriptions of cardiovascular diseases medications in england and wales in the past two decades. Int. J. Environ. Res. Public Health 2021, 18, 7041. [Google Scholar] [CrossRef] [PubMed]
- Sweiss, K.; Naser, A.Y.; Alrawashdeh, H.M.; Alharazneh, A. Hospital admissions due to vasomotor and allergic rhinitis in England and Wales between 1999 and 2019: An ecological study. Ir. J. Med. Sci. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Sweiss, K.; Naser, A.Y.; Samannodi, M.; Alwafi, H. Hospital admissions due to infectious and parasitic diseases in England and Wales between 1999 and 2019: An ecological study. BMC Infect. Dis. 2022, 22, 398. [Google Scholar] [CrossRef] [PubMed]
- Mustafa Ali, M.; Naser, A.; AbuAlhommos, A.K.; Al-Daghastani, T.; Alrawashdeh, H.M.; Mustafa Ali, S.; Alwafi, H.; Alqurashi, M.; Basha Ahmed, A.; Albarqi, H. Hospital admissions secondary to diseases of the blood, blood-forming organs, and immune system in england and wales. Cureus 2022, 14, 30179. [Google Scholar] [CrossRef]
- Mustafa Ali, S.; Naser, A.Y.; Alghanemi, A.G.; AbuAlhommos, A.K.; Sabha, M.; Mustafa Ali, M.K.; Hemmo, S.I.; Alrajeh, A.M.; Alqahtani, J.S.; Aldhahir, A.M.; et al. Musculoskeletal system and connective tissue related hospital admission in england and wales between 1999 and 2019: An ecologic study. Cureus 2022, 14, 32453. [Google Scholar] [CrossRef]
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 14 September 2022).
- Office for National Statistics. Leading Causes of Death, UK: 2001 to 2018. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/articles/leadingcausesofdeathuk/2001to2018 (accessed on 14 September 2022).
- Trueman, D.W.F.; Hancock, E. Estimating the Economic Burden of Respiratory Illness in the UK. 28/10. Available online: https://www.blf.org.uk/policy/economic-burden (accessed on 14 September 2022).
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease; GOLD Report; Global Initiative for Chronic Obstructive Lung Disease: Deer Park, IL, USA, 2022. [Google Scholar]
- Al Rajeh, A.; Hurst, J. Monitoring of physiological parameters to predict exacerbations of chronic obstructive pulmonary disease (copd): A systematic review. J. Clin. Med. 2016, 5, 108. [Google Scholar] [CrossRef]
- Al Rajeh, A.M.; Aldabayan, Y.S.; Aldhahir, A.; Pickett, E.; Quaderi, S.; Alqahtani, J.S.; Mandal, S.; Lipman, M.C.I.; Hurst, J.R. Once daily versus overnight and symptom versus physiological monitoring to detect exacerbations of chronic obstructive pulmonary disease: Pilot randomized controlled trial. JMIR Mhealth Uhealth 2020, 8, e17597. [Google Scholar] [CrossRef]
- Office for National Statistics. Overview of the UK Population. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021 (accessed on 14 September 2022).
- Bartynski, W.S.; Heller, M.T.; Grahovac, S.Z.; Rothfus, W.E.; Kurs-Lasky, M. Severe thoracic kyphosis in the older patient in the absence of vertebral fracture: Association of extreme curve with age. AJNR Am. J. Neuroradiol. 2005, 26, 2077–2085. [Google Scholar] [PubMed]
- Sharma, G.; Goodwin, J. Effect of aging on respiratory system physiology and immunology. Clin. Interv. Aging 2006, 1, 253. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, E.; Lowery, E.; Kuhlmann, E.; Brubaker, A. The aging lung. Clin. Interv. Aging 2013, 8, 1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Freitas, F.S.; Ibiapina, C.C.; Alvim, C.G.; Britto, R.R.; Parreira, V.F. Relationship between cough strength and functional level in elderly. Braz. J. Phys. Ther. 2010, 14, 470–476. [Google Scholar] [CrossRef] [Green Version]
- Burgel, P.-R.; Nesme-Meyer, P.; Chanez, P.; Caillaud, D.; Carré, P.; Perez, T.; Roche, N. Cough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjects. Chest 2009, 135, 975–982. [Google Scholar] [CrossRef]
- Brandstetter, R.D.; Kazemi, H. Aging and the respiratory system. Med. Clin. N. Am. 1983, 67, 419–431. [Google Scholar] [CrossRef]
- Hurst, J.R.; Vestbo, J.; Anzueto, A.; Locantore, N.; Müllerova, H.; Tal-Singer, R.; Miller, B.; Lomas, D.A.; Agusti, A.; MacNee, W.; et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N. Engl. J. Med. 2010, 363, 1128–1138. [Google Scholar] [CrossRef] [Green Version]
- Bhowmik, A.; Seemungal, T.A.; Sapsford, R.J.; Wedzicha, J.A. Relation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbations. Thorax 2000, 55, 114–120. [Google Scholar] [CrossRef] [Green Version]
- Seemungal, T.A.; Donaldson, G.C.; Paul, E.A.; Bestall, J.C.; Jeffries, D.J.; Wedzicha, J.A. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1998, 157, 1418–1422. [Google Scholar] [CrossRef]
- Miravitlles, M.; Guerrero, T.; Mayordomo, C.; Sánchez-Agudo, L.; Nicolau, F.; Segú, J.L. Factors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory copd patients: A multiple logistic regression analysis. Respiration 2000, 67, 495–501. [Google Scholar] [CrossRef]
- Foreman, M.G.; DeMeo, D.L.; Hersh, C.P.; Reilly, J.J.; Silverman, E.K. Clinical determinants of exacerbations in severe, early-onset COPD. Eur. Respir. J. 2007, 30, 1124–1130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huisman, M.; Kunst, A.E.; Bopp, M.; Borgan, J.K.; Borrell, C.; Costa, G.; Deboosere, P.; Gadeyne, S.; Glickman, M.; Marinacci, C.; et al. Educational inequalities in cause-specific mortality in middle-aged and older men and women in eight western European populations. Lancet 2005, 365, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Pleasants, R.A.; Riley, I.L.; Mannino, D.M. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 2475–2496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prescott, E.; Godtfredsen, N.; Vestbo, J.; Osler, M. Social position and mortality from respiratory diseases in males and females. Eur. Respir. J. 2003, 21, 821–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montserrat-Capdevila, J.; Marsal, J.R.; Ortega, M.; Castañ-Abad, M.T.; Alsedà, M.; Barbé, F.; Godoy, P. Clinico-epidemiological characteristics of men and women with a new diagnosis of chronic obstructive pulmonary disease: A database (SIDIAP) study. BMC Pulm. Med. 2021, 21, 44. [Google Scholar] [CrossRef]


| ICD Code | Description | Percentage from Total Number of Admissions |
|---|---|---|
| J40 | “Bronchitis, not specified as acute or chronic” | 1.0% |
| J41 | “Simple and mucopurulent chronic bronchitis” | <0.1% |
| J42 | “Unspecified chronic bronchitis” | 0.2% |
| J43 | “Emphysema” | 2.0% |
| J44 | “Other chronic obstructive pulmonary diseases (chronic obstructive pulmonary disease with (acute) lower respiratory infection and chronic obstructive pulmonary disease with (acute) exacerbation)” | 62.3% |
| J45 | “Asthma” | 26.7% |
| J46 | “Status asthmaticus” | 3.0% |
| J47 | “Bronchiectasis” | 4.8% |
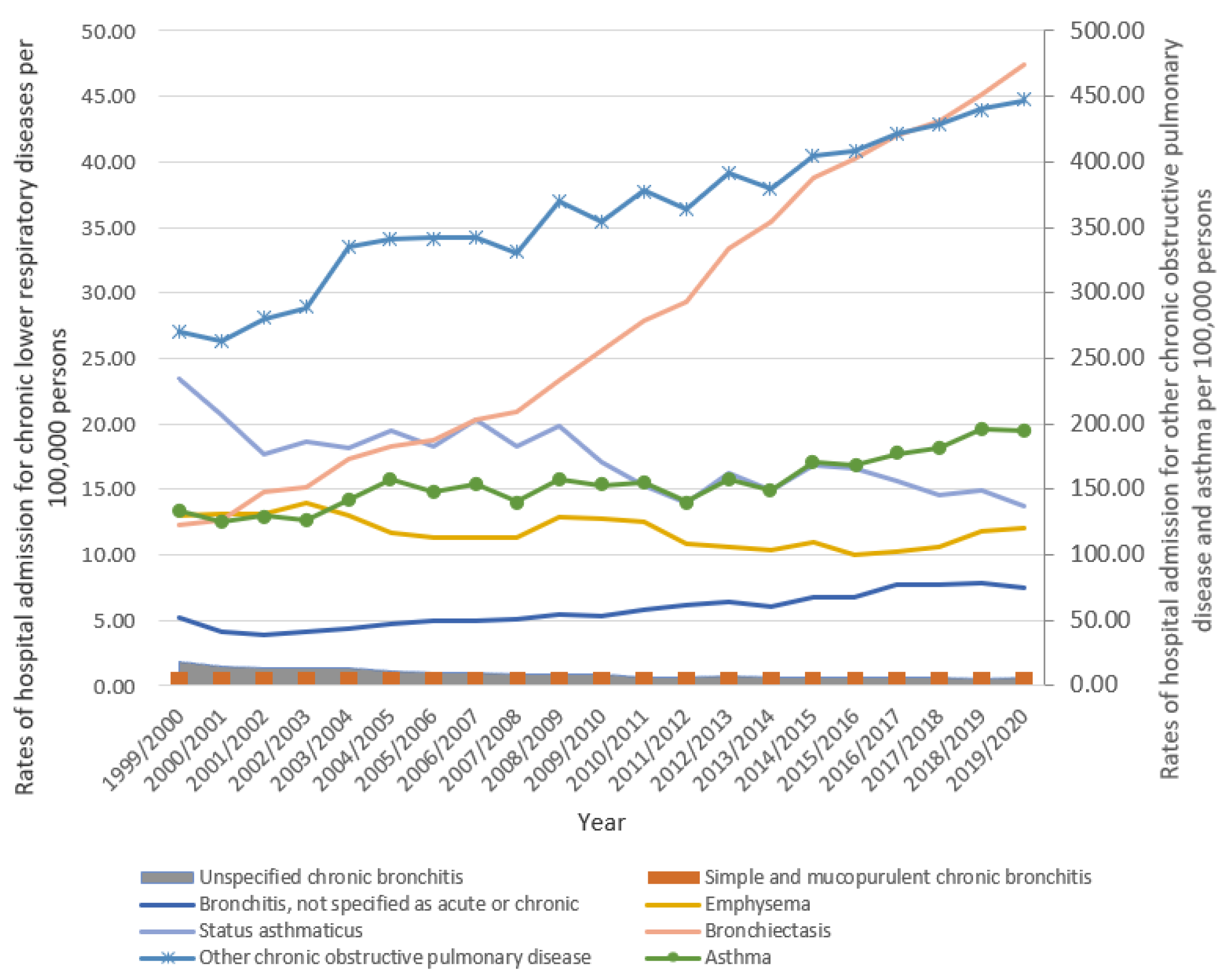
| Diseases | Rate of Diseases in 1999 Per 100,000 Persons (95% CI) | Rate of Diseases in 2020 Per 100,000 Persons (95% CI) | Percentage Change from 1999 to 2020 | p-Value |
|---|---|---|---|---|
| “Bronchitis, not specified as acute or chronic” | 5.14 (4.94–5.33) | 7.46 (7.24–7.68) | 45.2% | ≤0.01 |
| “Simple and mucopurulent chronic bronchitis” | 0.11 (0.08–0.14) | 0.06 (0.04–0.08) | −41.8% | ≤0.01 |
| “Unspecified chronic bronchitis” | 1.82 (1.71–1.94) | 0.58 (0.52–0.64) | −68.2% | ≤0.01 |
| “Emphysema” | 12.99 (12.68–13.30) | 11.98 (11.71–12.26) | −7.8% | ≥0.05 |
| “Other chronic obstructive pulmonary diseases” | 270.18 (268.77–271.59) | 447.18 (445.49–448.88) | 65.5% | ≤0.01 |
| “Asthma” | 133.59 (132.60–134.58) | 195.24 (194.12–196.36) | 46.1% | ≤0.01 |
| “Status asthmaticus” | 23.45 (23.04–23.87) | 13.77 (13.47–14.06) | −41.3% | ≤0.01 |
| “Bronchiectasis” | 12.26 (11.96–12.56) | 47.43 (46.88–47.98) | 287.0% | ≤0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Rajeh, A.M. Trend of Admissions Due to Chronic Lower Respiratory Diseases: An Ecological Study. Healthcare 2023, 11, 65. https://doi.org/10.3390/healthcare11010065
Al Rajeh AM. Trend of Admissions Due to Chronic Lower Respiratory Diseases: An Ecological Study. Healthcare. 2023; 11(1):65. https://doi.org/10.3390/healthcare11010065
Chicago/Turabian StyleAl Rajeh, Ahmed M. 2023. "Trend of Admissions Due to Chronic Lower Respiratory Diseases: An Ecological Study" Healthcare 11, no. 1: 65. https://doi.org/10.3390/healthcare11010065




