Why Does It Hurt So Much? Emotion Regulation Mediates the Association between Fibromyalgia Symptoms and Psychological Distress
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Associations between Study Variables
3.2. ER According to Major Depression and Perceived Stress Levels
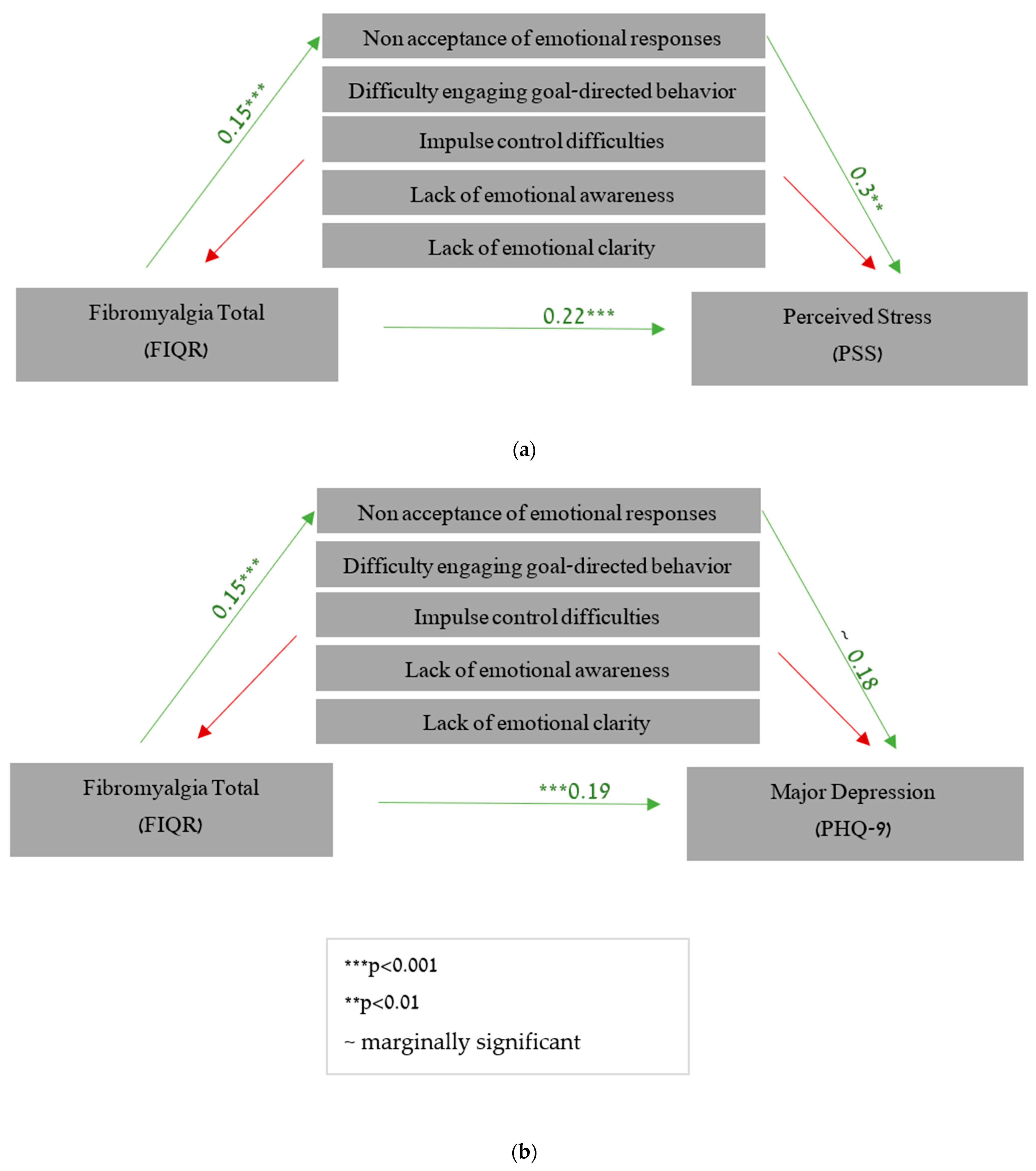
3.3. The Mediating Role of Emotion Regulation
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, P.J.; Rice, F.L. Fibromyalgia syndrome pathology and environmental influences on afflictions with medically unexplained symptoms. Rev. Environ. Health 2016, 31, 281–294. [Google Scholar] [CrossRef]
- Wolfe, F.; Clauw, D.J.; Fitzcharles, M.A.; Goldenberg, D.L.; Häuser, W.; Katz, R.S.; Mease, P.; Russell, A.S.; Russell, I.J.; Winfield, J.B. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: A modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J. Rheumatol. 2011, 38, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Kleykamp, B.A.; Ferguson, M.C.; McNicol, E.; Bixho, I.; Arnold, L.M.; Edwards, R.R.; Fillingim, R.; Grol-Prokopczyk, H.; Turk, D.C.; Dworkin, R.H. The prevalence of psychiatric and chronic pain comorbidities in fibromyalgia: An ACTTION systematic review. In Seminars in Arthritis and Rheumatism; WB Saunders: Philadelphia, PA, USA, 2021; Volume 51, pp. 166–174. [Google Scholar]
- Thieme, K.; Turk, D.C.; Flor, H. Comorbid depression and anxiety in fibromyalgia syndrome: Relationship to somatic and psychosocial variables. Psychosom. Med. 2004, 66, 837–844. [Google Scholar] [CrossRef]
- Arnold, L.M.; Crofford, L.J.; Mease, P.J.; Burgess, S.M.; Palmer, S.C.; Abetz, L.; Martin, S.A. Patient perspectives on the impact of fibromyalgia. Patient Educ. Couns. 2008, 73, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Pinto, A.M.; Geenen, R.; Wager, T.D.; Lumley, M.A.; Häuser, W.; Kosek, E.; Ablin, J.N.; Amris, K.; Branco, J.; Buskila, D.; et al. Emotion regulation and the salience network: A hypothetical integrative model of fibromyalgia. Nat. Rev. Rheumatol. 2022, 19, 44–60. [Google Scholar] [CrossRef]
- Kaleycheva, N.; Cullen, A.E.; Evans, R.; Harris, T.; Nicholson, T.; Chalder, T. The role of lifetime stressors in adult fibromyalgia: Systematic review and meta-analysis of case-control studies. Psychol. Med. 2021, 51, 177–193. [Google Scholar] [CrossRef]
- Kopp, C.B. Regulation of distress and negative emotions: A developmental view. Dev. Psychol. 1989, 25, 343. [Google Scholar] [CrossRef]
- Gross, J.J. Emotion regulation in adulthood: Timing is everything. Curr. Dir. Psychol. Sci. 2001, 10, 214–219. [Google Scholar] [CrossRef]
- Hayes, S.C.; Wilson, K.G.; Gifford, E.V.; Follette, V.M.; Strosahl, K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. J. Consult. Clin. Psychol. 1996, 64, 1152. [Google Scholar] [CrossRef]
- Lumley, M.A.; Cohen, J.L.; Borszcz, G.S.; Cano, A.; Radcliffe, A.M.; Porter, L.S.; Schubiner, H.; Keefe, F.J. Pain and emotion: A biopsychosocial review of recent research. J. Clin. Psychol. 2011, 67, 942–968. [Google Scholar] [CrossRef] [PubMed]
- Town, J.M.; Lomax, V.; Abbass, A.A.; Hardy, G. The role of emotion in psychotherapeutic change for medically unexplained symptoms. Psychother. Res. 2019, 29, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Zautra, A.J.; Fasman, R.; Reich, J.W.; Harakas, P.; Johnson, L.M.; Olmsted, M.E.; Davis, M.C. Fibromyalgia: Evidence for deficits in positive affect regulation. Psychosom. Med. 2005, 67, 147. [Google Scholar] [CrossRef] [PubMed]
- Rost, S.; Crombez, G.; Sütterlin, S.; Vögele, C.; Veirman, E.; Van Ryckeghem, D.M. Altered regulation of negative affect in patients with fibromyalgia: A diary study. Eur. J. Pain 2021, 25, 714–724. [Google Scholar] [CrossRef]
- Trucharte, A.; Leon, L.; Castillo-Parra, G.; Magán, I.; Freites, D.; Redondo, M. Emotional regulation processes: Influence on pain and disability in Fibromyalgia patients. Clin. Exp. Rheumatol. 2020, 38 (Suppl. S123), 40–46. [Google Scholar]
- Geenen, R.; van Ooijen-van der Linden, L.; Lumley, M.A.; Bijlsma, J.W.; van Middendorp, H. The match–mismatch model of emotion processing styles and emotion regulation strategies in fibromyalgia. J. Psychosom. Res. 2012, 72, 45–50. [Google Scholar] [CrossRef]
- Sayar, K.; Gulec, H.; Topbas, M. Alexithymia and anger in patients with fibromyalgia. Clin. Rheumatol. 2004, 23, 441–448. [Google Scholar] [CrossRef]
- van Middendorp, H.; Lumley, M.A.; Jacobs, J.W.; van Doornen, L.J.; Bijlsma, J.W.; Geenen, R. Emotions and emotional approach and avoidance strategies in fibromyalgia. J. Psychosom. Res. 2008, 64, 159–167. [Google Scholar] [CrossRef]
- Bennett, R.M.; Friend, R.; Jones, K.D.; Ward, R.; Han, B.K.; Ross, R.L. The revised Fibromyalgia impact questionnaire (FIQR): Validation and psychometric properties. Arthritis Res. Ther. 2009, 11, R120. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Swaminathan, A.; Viswanathan, S.; Gnanadurai, T.; Ayyavoo, S.; Manickam, T. Perceived stress and sources of stress among first-year medical undergraduate students in a private medical college—Tamil Nadu. Natl. J. Physiol. Pharm. Pharmacol. 2015, 6, 9–14. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Gratz, K.L.; Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess. 2004, 26, 41–54. [Google Scholar] [CrossRef]
- Rockwood, N.J.; Hayes, A.F. MLmed: An SPSS macro for multilevel mediation and conditional process analysis. In Proceedings of the Poster Presented at the Annual Meeting of the Association of Psychological Science (APS), Boston, MA, USA, 25 May 2017. [Google Scholar]
- Holm, S. A simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Arnold, L.M.; Hudson, J.I.; Keck, P.E.; Auchenbach, M.B.; Javaras, K.N.; Hess, E.V. Comorbidity of Fibromyalgia and psychiatric disorders. J. Clin. Psychiatry 2006, 67, 1219–1225. [Google Scholar] [CrossRef]
- Bondesson, E.; Larrosa Pardo, F.; Stigmar, K.; Ringqvist, Å.; Petersson, I.F.; Jöud, A.; Schelin, M.E.C. Comorbidity between pain and mental illness–evidence of a bidirectional relationship. Eur. J. Pain 2018, 22, 1304–1311. [Google Scholar] [CrossRef]
- Åsbring, P.; Närvänen, A.L. Women’s experiences of stigma in relation to chronic fatigue syndrome and fibromyalgia. Qual. Health Res. 2002, 12, 148–160. [Google Scholar]
- Aldao, A.; Nolen-Hoeksema, S.; Schweizer, S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin. Psychol. Rev. 2010, 30, 217–237. [Google Scholar] [CrossRef]
- Haugmark, T.; Hagen, K.B.; Smedslund, G.; Zangi, H.A. Mindfulness-and acceptance-based interventions for patients with fibromyalgia–A systematic review and meta-analyses. PLoS ONE 2019, 14, e0221897. [Google Scholar] [CrossRef]
| Major Depression (PHQ-9) | Perceived Stress (PSS) | FM (FIQR) | Difficulties in Emotion Regulation (DERS) | Nonacceptance of Emotional Responses (DERS) | Difficulty Engaging in Goal-Directed Behavior (DERS) | Impulse Control Difficulties (DERS) | Lack of Emotional Awareness (DERS) | Limited Access to ER Strategies (DERS) | Lack of Emotional Clarity (DERS) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Major depression (PHQ-9) | 0.752 *** | 0.719 *** | 0.373 *** | 0.507 *** | 0.287 ** | 0.367 *** | −0.139 | 0.325 *** | 0.280 ** | |
| Perceived stress (PSS) | 0.698 *** | 0.480 *** | 0.618 *** | 0.316 ** | 0.516 *** | −0.172 | 0.452 *** | 0.246 * | ||
| FM impact (FIQR) | 0.351 *** | 0.436 *** | 0.279 ** | 0.322 ** | −0.035 | 0.230 * | 0.353 ** | |||
| Difficulties in emotion regulation (DERS) | 0.798 *** | 0.691 *** | 0.804 *** | 0.406 *** | 0.851 *** | 0.490 *** | ||||
| Nonacceptance of emotional responses (DERS) | 0.527 *** | 0.684 *** | 0.005 | 0.721 *** | 0.333 ** | |||||
| Difficulty engaging in goal-directed behavior (DERS) | 0.492 *** | 0.070 | 0.703 *** | 0.182 | ||||||
| Impulse control difficulties (DERS) | 0.021 | 0.762 *** | 0.417 *** | |||||||
| Lack of emotional awareness (DERS) | 0.065 | 0.232 * | ||||||||
| Limited access to ER strategies (DERS) | 0.246 * | |||||||||
| Lack of emotional clarity (DERS) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frumer, L.; Marom Harel, H.; Horesh, D. Why Does It Hurt So Much? Emotion Regulation Mediates the Association between Fibromyalgia Symptoms and Psychological Distress. Healthcare 2023, 11, 1368. https://doi.org/10.3390/healthcare11101368
Frumer L, Marom Harel H, Horesh D. Why Does It Hurt So Much? Emotion Regulation Mediates the Association between Fibromyalgia Symptoms and Psychological Distress. Healthcare. 2023; 11(10):1368. https://doi.org/10.3390/healthcare11101368
Chicago/Turabian StyleFrumer, Lee, Hadar Marom Harel, and Danny Horesh. 2023. "Why Does It Hurt So Much? Emotion Regulation Mediates the Association between Fibromyalgia Symptoms and Psychological Distress" Healthcare 11, no. 10: 1368. https://doi.org/10.3390/healthcare11101368
APA StyleFrumer, L., Marom Harel, H., & Horesh, D. (2023). Why Does It Hurt So Much? Emotion Regulation Mediates the Association between Fibromyalgia Symptoms and Psychological Distress. Healthcare, 11(10), 1368. https://doi.org/10.3390/healthcare11101368





