Pilates to Improve Core Muscle Activation in Chronic Low Back Pain: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
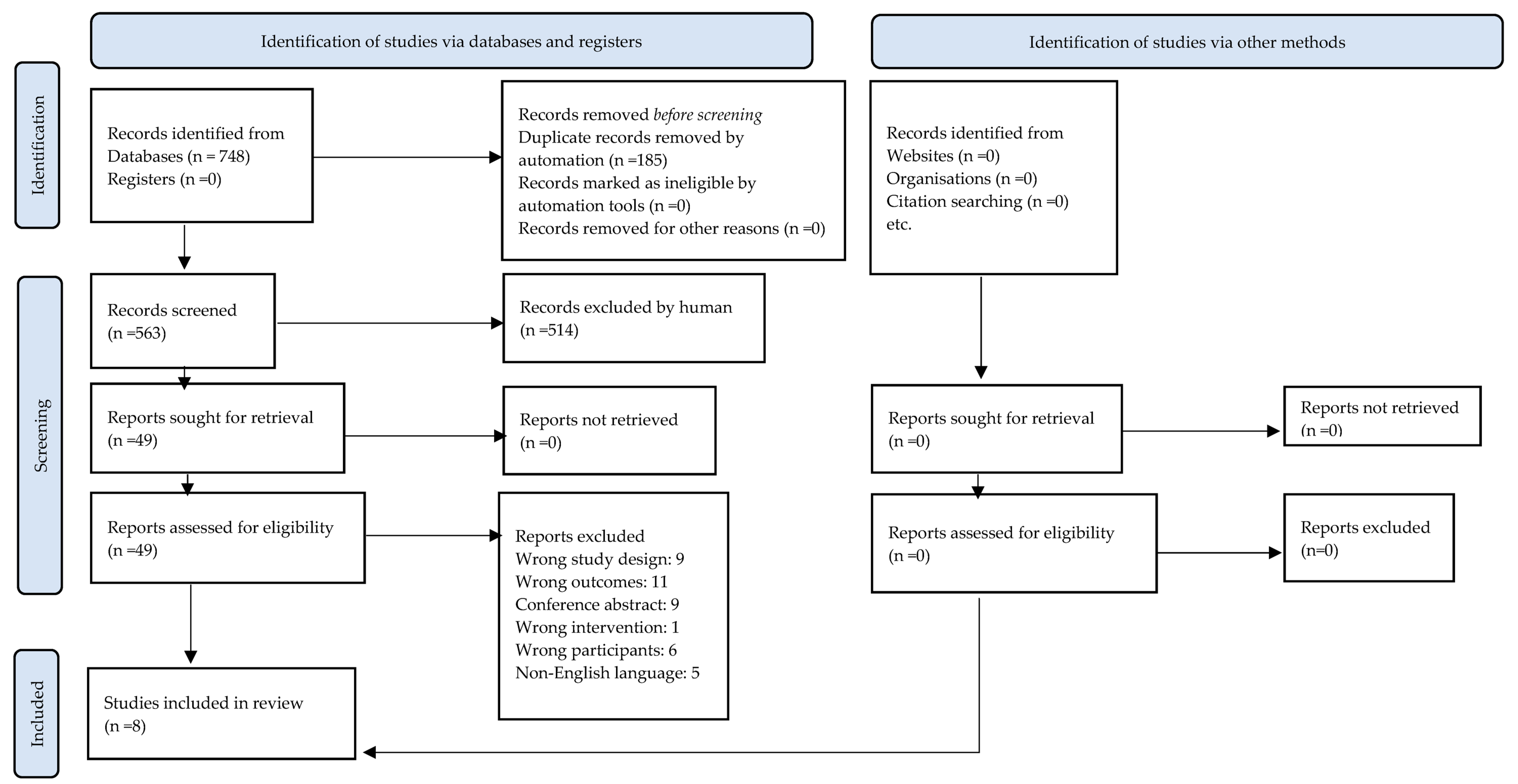
3.1. Search Results
3.2. Methodological Quality
3.3. Study Characteristics
3.4. Participant Characteristics
3.5. Interventions
3.6. Muscle Thickness and Muscle Activation
3.7. Pain, Disability, and Quality of Life
3.8. Certainty of Findings
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alves, M.C.; de Souza Neto, R.J.; Barbosa, R.I.; Marcolino, A.M.; Kuriki, H.U. Effects of a Pilates protocol in individuals with non-specific low back pain compared with healthy individuals: Clinical and electromyographic analysis. Clin. Biomech. 2020, 72, 172–178. [Google Scholar] [CrossRef]
- Schimidt, A.C.; Herzinger, P.D.O.; Matias, D.P.; Welling, L.C. Influence of Pilates Method on Nonspecific Lumbar Pain. Braz. Neurosurg. 2020, 39, 300–305. [Google Scholar] [CrossRef]
- Gholamalishahi, S.; Backhaus, I.; Cilindro, C.; Masala, D.; La Torre, G. Pilates-based exercise in the reduction of the low back pain: An overview of reviews. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 4557–4563. [Google Scholar] [PubMed]
- Latey, P. The Pilates method: History and philosophy. J. Bodyw. Mov. Ther. 2001, 5, 275–282. [Google Scholar] [CrossRef]
- Owsley, A. An introduction to clinical Pilates. Athl. Ther. Today 2005, 10, 19–68. [Google Scholar] [CrossRef]
- Wells, C.; Kolt, G.S.; Bialocerkowski, A. Defining Pilates exercise: A systematic review. Complement. Ther. Med. 2012, 20, 253–262. [Google Scholar] [CrossRef]
- Cordeiro, A.L.L.; Oliveira, A.P.S.; Cerqueira, N.S.; Santos, F.A.F.; Oliveira, A.M.S. Pilates method on pain in patients with low back pain: Systematic review. BrJP 2022, 5, 265–271. [Google Scholar]
- Yu, Z.; Yin, Y.; Wang, J.; Zhang, X.; Cai, H.; Peng, F. Efficacy of Pilates on Pain, Functional Disorders and Quality of Life in Patients with Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 2850. [Google Scholar] [CrossRef]
- Pereira, M.J.; Mendes, R.; Mendes, R.S.; Martins, F.; Gomes, R.; Gama, J.; Dias, G.; Castro, M.A. Benefits of Pilates in the Elderly Population: A Systematic Review and Meta-Analysis. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 236–268. [Google Scholar] [CrossRef]
- Cronin, E.; Broderick, P.; Clarke, H.; Monaghan, K. What are the effects of pilates in the post stroke population? A systematic literature review & meta-analysis of randomised controlled trials. J. Bodyw. Mov. Ther. 2023, 33, 223–232. [Google Scholar]
- Beyera, G.K.; O’Brien, J.; Campbell, S. Health-care utilisation for low back pain: A systematic review and meta-analysis of population-based observational studies. Rheumatol. Int. 2019, 39, 1663–1679. [Google Scholar] [CrossRef] [PubMed]
- Mattiuzzi, C.; Lippi, G.; Bovo, C. Current epidemiology of low back pain. J. Hosp. Manag. Health Policy 2020, 4, 15. [Google Scholar] [CrossRef]
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study 2017. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ye, H.; Li, Z.; Lu, C.; Ye, J.; Liao, M.; Chen, X. Epidemiological trends of low back pain at the global, regional, and national levels. Eur. Spine J. 2022, 31, 953–962. [Google Scholar] [CrossRef]
- Bento, T.P.F.; dos Santos Genebra, C.V.; Maciel, N.M.; Cornelio, G.P.; Simeão, S.F.A.P.; de Vitta, A. Low back pain and some associated factors: Is there any difference between genders? Braz. J. Phys. Ther. 2020, 24, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M.X. Prevalence of chronic low back pain: Systematic review. Rev. Saúde Pública 2015, 49, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W. Core stability exercise in chronic low back pain. Orthop. Clin. N. Am. 2003, 34, 245–254. [Google Scholar] [CrossRef]
- Hides, J.A.; Richardson, C.A.; Jull, G.A. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine (Phila Pa 1976) 1996, 21, 2763–2769. [Google Scholar] [CrossRef]
- Hodges, P.W.; Richardson, C.A. Inefficient muscular stabilization of the lumbar spine associated with low back pain: A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976) 1996, 21, 2640–2650. [Google Scholar] [CrossRef]
- Newcomer, K.L.; Jacobson, T.D.; Gabriel, D.A.; Larson, D.R.; Brey, R.H.; An, K.-N. Muscle activation patterns in subjects with and without low back pain. Arch. Phys. Med. Rehabil. 2002, 83, 816–821. [Google Scholar] [CrossRef]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core Stability Exercise Principles. Curr. Sport. Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Mazloum, V.; Sahebozamani, M.; Barati, A.; Nakhaee, N.; Rabiei, P. The effects of selective Pilates versus extension-based exercises on rehabilitation of low back pain. J. Bodyw. Mov. Ther. 2018, 22, 999–1003. [Google Scholar] [CrossRef]
- He, B.; Jiang, P.; Zhang, X. Meta-Analysis of the Efficacy of Pilates Exercises in the Treatment of Non-specific Low Back Pain. Soc. Med. Health Manag. 2022, 3, 36–48. [Google Scholar]
- Romao, C.I.G.; Mercê, C.I.A.; Cordeiro, J.F.C.; de Brito, A.M.V.V.; Branco, M.A.C. The Effect of Pilates Exercises on Muscle Electrical Activation in Adults with Chronic Low Back Pain: A Systematic Review. Coluna/Columna 2022, 21. [Google Scholar] [CrossRef]
- Barbosa, A.W.C.; Guedes, C.A.; Bonifácio, D.N.; Silva, A.D.F.; Martins, F.L.M.; Barbosa, M.C.S.A. The Pilates breathing technique increases the electromyographic amplitude level of the deep abdominal muscles in untrained people. J. Bodyw. Mov. Ther. 2015, 19, 57–61. [Google Scholar] [CrossRef]
- MacHado, P.M.; Alves, M.C.; Hendler, K.G.; Benetti, V.B.; Souza, R.J.D.; Barbosa, R.I.; Kuriki, H.U. Effectiveness of the Pilates method for individuals with nonspecific low back pain: Clinical and electromyographic aspects. Mot. Rev. De Educ. Fis. 2018, 23. [Google Scholar] [CrossRef]
- Panhan, A.C.; Gonçalves, M.; Eltz, G.D.; Villalba, M.M.; Cardozo, A.C.; Bérzin, F. Co-contraction of the core muscles during Pilates exercise on the Wunda Chair. J. Back Musculoskelet. Rehabil. 2020, 33, 719–725. [Google Scholar] [CrossRef]
- Yamato, T.P.; Maher, C.G.; Saragiotto, B.T.; Hancock, M.J.; Ostelo, R.W.; Cabral, C.M.; Costa, L.O. Pilates for low back pain. Cochrane Database Syst. Rev. 2015, CD12004. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, G.C.; Costa, L.O.P.; Cabral, C.M.N. Efficacy of the Pilates method for pain and disability in patients with chronic nonspecific low back pain: A systematic review with meta-analysis. Braz. J. Phys. Ther. 2013, 17, 517–532. [Google Scholar] [CrossRef] [PubMed]
- Domingues de Freitas, C.; Costa, D.A.; Junior, N.C.; Civile, V.T. Effects of the pilates method on kinesiophobia associated with chronic non-specific low back pain: Systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2020, 24, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Br. Med. J. 2021, 372, n71. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Covidence Systematic Review Software. 2022. Available online: www.covidence.org (accessed on 19 December 2022).
- Valentine, J.C.; Thompson, S.G. Issues relating to confounding and meta-analysis when including non-randomized studies in systematic reviews on the effects of interventions. Res. Synth. Methods 2013, 4, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Coleman, K.; Norris, S.; Weston, A.; Grimmer-Somers, K.; Hillier, S.; Merlin, T.; Tooher, R. NHMRC Additional Levels of Evidence and Grades for Recommendations for Developers of Guidelines; NHMRC: Canberra, Australia, 2005. [Google Scholar]
- Hebert, J.J.; Koppenhaver, S.L.; Parent, E.C.; Fritz, J.M. A Systematic Review of the Reliability of Rehabilitative Ultrasound Imaging for the Quantitative Assessment of the Abdominal and Lumbar Trunk Muscles. Spine 2009, 34, E848–E856. [Google Scholar] [CrossRef]
- Yoo, S.; Lee, N.G.; Park, C.; You, J.S.H. Concurrent Validity and Test-retest Reliability of the Core Stability Test Using Ultrasound Imaging and Electromyography Measurements. Phys. Ther. Korea 2021, 28, 186–193. [Google Scholar] [CrossRef]
- Grooms, D.R.; Grindstaff, T.L.; Croy, T.; Hart, J.M.; Saliba, S.A. Clinimetric Analysis of Pressure Biofeedback and Transversus Abdominis Function in Individuals With Stabilization Classification Low Back Pain. J. Orthop. Sport. Phys. Ther. 2013, 43, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Alkhathami, K.; Alshehre, Y.; Wang-Price, S.; Brizzolara, K. Reliability and Validity of the Functional Movement Screen™ with a Modified Scoring System for Young Adults with Low Back Pain. Int. J. Sports Phys. Ther. 2021, 16, 620–627. [Google Scholar] [CrossRef]
- Hodges, P.W.; Pengel, L.; Herbert, R.; Gandevia, S. Measurement of muscle contraction with ultrasound imaging. Muscle Nerve 2003, 27, 682–692. [Google Scholar] [CrossRef]
- Lima, P.O.d.P.; de Oliveira, R.R.; Costa, L.O.P.; Laurentino, G.E.C. Measurement properties of the pressure biofeedback unit in the evaluation of transversus abdominis muscle activity: A systematic review. Physiotherapy 2011, 97, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Marshall, P.; Murphy, B. The validity and reliability of surface EMG to assess the neuromuscular response of the abdominal muscles to rapid limb movement. J. Electromyogr. Kinesiol. 2003, 13, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Dawson, A.P.; Steele, E.J.; Hodges, P.W.; Stewart, S. Utility of the Oswestry Disability Index for studies of back pain related disability in nurses: Evaluation of psychometric and measurement properties. Int. J. Nurs. Stud. 2010, 47, 604–607. [Google Scholar] [CrossRef]
- Johnsen, L.G.; Hellum, C.; Nygaard, P.; Storheim, K.; Brox, J.I.; Rossvoll, I.; Leivseth, G.; Grotle, M. Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet. Disord. 2013, 14, 148. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Preuper, H.R.S.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef]
- Lurie, J. A review of generic health status measures in patients with low back pain. Spine (Phila Pa 1976) 2000, 25, 3125–3129. [Google Scholar] [CrossRef]
- Gibbs, M.T.; Morrison, N.M.; Raftry, S.; Jones, M.D.; Marshall, P.W. Does a powerlifting inspired exercise programme better compliment pain education compared to bodyweight exercise for people with chronic low back pain? A multicentre, single-blind, randomised controlled trial. Clin. Rehabil. 2022, 36, 1199–1213. [Google Scholar] [CrossRef]
- McKenzie, J.E.; Brennan, S.E. Chapter 12: Synthesizing and presenting findings using other methods. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.3; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, United Kingdom, 2023. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. Bmj 2019, 366, l4898. [Google Scholar] [CrossRef]
- GRADEpro. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. 2023. Available online: gradepro.org (accessed on 19 December 2022).
- Silveira, A.P.d.B.; Nagel, L.Z.; Pereira, D.D.; Morita, Â.K.; Spinoso, D.H.; Navega, M.T.; Marques, N.R. Immediate effect of a Pilates method exercise session on the co-contraction pattern of the trunk stabilizing muscles in individuals with and without nonspecific chronic low back pain. Fisioterapia e Pesquisa 2018, 25, 173–181. [Google Scholar] [CrossRef]
- Sharma, S.; Sarin, A. To Compare the Effect of Mat Pilates Core Muscle Strengthening Exercises with and without EMG Biofeedback on Pain, Strength and Disability with Chronic Low Back Pain. Indian J. Physiother. Occup. Ther.-Int. J. 2017, 11, 98–104. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Bhadauria, E.A.; Gurudut, P. Comparative effectiveness of lumbar stabilization, dynamic strengthening, and Pilates on chronic low back pain: Randomized clinical trial. J. Exerc. Rehabil. 2017, 13, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Brooks, C.; Kennedy, S.; Marshall, P.W. Specific trunk and general exercise elicit similar changes in anticipatory postural adjustments in patients with chronic low back pain: A randomized controlled trial. Spine (Phila Pa 1976) 2012, 37, E1543–E1550. [Google Scholar] [CrossRef]
- Ashtiani, A.; Askari, A. Effects of Modified Pilates Exercises on Pain, Disability, and Lumbopelvic Motor Control in Patients With Chronic Low Back Pain. Phys. Treat. Specif. Phys. Ther. J. 2020, 10, 195–204. [Google Scholar] [CrossRef]
- Batibay, S.; Külcü, D.G.; Kaleoğlu; Mesci, N. Effect of Pilates mat exercise and home exercise programs on pain, functional level, and core muscle thickness in women with chronic low back pain. J. Orthop. Sci. 2021, 26, 979–985. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Bergamin, M.; Gobbo, S.; Martínez-Amat, A.; Hita-Contreras, F. Comparative effects of 12 weeks of equipment based and mat Pilates in patients with Chronic Low Back Pain on pain, function and transversus abdominis activation. A randomized controlled trial. Complement. Ther. Med. 2017, 33, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Mendes Tozim, B.; Nava, G.; Marques, A.; Navega, M. Efficacy of the Pilates versus general exercises versus educational workshops on neuromuscular parameters: A randomized controlled trial. J. Bodyw. Mov. Ther. 2021, 26, 420–427. [Google Scholar] [CrossRef]
- Nabavi, N.; Bandpei, M.A.M.; Mosallanezhad, Z.; Rahgozar, M.; Jaberzadeh, S. The Effect of 2 Different Exercise Programs on Pain Intensity and Muscle Dimensions in Patients With Chronic Low Back Pain: A Randomized Controlled Trial. J. Manip. Physiol. Ther. 2018, 41, 102–110. [Google Scholar] [CrossRef]
- Sonmezer, E.; Özköslü, M.A.; Yosmaoğlu, H.B. The effects of clinical pilates exercises on functional disability, pain, quality of life and lumbopelvic stabilization in pregnant women with low back pain: A randomized controlled study. J. Back Musculoskelet. Rehabil. 2021, 34, 69–76. [Google Scholar] [CrossRef]
- The Physiotherapy Evidence Database (PEDro). 2010. Available online: www.pedro.org.au (accessed on 19 December 2022).
- WHO. Physical Status: The Use of and Interpretation of Anthropometry; Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Ostelo, R.W.J.G.; de Vet, H.C.W. Clinically important outcomes in low back pain. Best Pract. Res. Clin. Rheumatol. 2005, 19, 593–607. [Google Scholar] [CrossRef]
- Monticone, M.; Baiardi, P.; Vanti, C.; Ferrari, S.; Pillastrini, P.; Mugnai, R.; Foti, C. Responsiveness of the Oswestry Disability Index and the Roland Morris Disability Questionnaire in Italian subjects with sub-acute and chronic low back pain. Eur. Spine J. 2012, 21, 122–129. [Google Scholar] [CrossRef]
- Copay, A.G.; Glassman, S.D.; Subach, B.R.; Berven, S.; Schuler, T.C.; Carreon, L.Y. Minimum clinically important difference in lumbar spine surgery patients: A choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and Pain Scales. Spine J. 2008, 8, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Rugg, B.; Geere, J.-A. The effects of Pilates exercise in comparison to other forms of exercise on pain and disability in individuals with chronic non-specific low back pain: A systematic review with meta-analysis. Musculoskelet. Care 2023, 21, 78–96. [Google Scholar] [CrossRef] [PubMed]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.; Tagliaferri, S.D.; Brisby, H.; Belavy, D.L. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. Sport. Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef]
- Hayden, J.A.; Ellis, J.; Ogilvie, R.; Stewart, S.A.; Bagg, M.K.; Stanojevic, S.; Yamato, T.P.; Saragiotto, B.T. Some types of exercise are more effective than others in people with chronic low back pain: A network meta-analysis. J. Physiother. 2021, 67, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Gladwell, V.; Head, S.; Haggar, M.; Beneke, R. Does a program of Pilates improve chronic non-specific low back pain? J. Sport Rehabil. 2006, 15, 338–350. [Google Scholar] [CrossRef]
- Rackwitz, B.; de Bie, R.; Limm, H.; von Garnier, K.; Ewert, T.; Stucki, G. Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials. Clin. Rehabil. 2006, 20, 553–567. [Google Scholar] [CrossRef]


| Study | Eligibility Specified | Random Allocation | Concealed Allocation | Groups Similar at Baseline | Participant Blinding | Therapist Blinding | Assessor Blinding | <15% Dropouts | Intention-to-Treat Analysis | Between-Group Difference | Point Estimate and Variability | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ashtiani [58] | Y | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Batibay [59] | Y | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Bhadauria [56] | Y | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
| Brooks [57] | Y | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 8 |
| Cruz-Diaz [60] | Y | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 7 |
| Mendes Tozim [61] | Y | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| Nabavi [62] | Y | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| Sonmezer [63] | Y | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 7 |
| Author Country Sample Size (Dropouts) | Age (Range)/Body Mass Index Gender | Intervention; Dosage; Setting; Practitioner | Relevant Outcome Domains | Assessment Method/ Muscles Assessed | Outcome Assessment Time Points |
|---|---|---|---|---|---|
| Pilates vs. equivalent exercise intervention | |||||
| Ashtiani (2020) [58] Iran 30 (0) | 18–50 MP: 34.5 (6.4)/25.1 (3.9) GE: 35.5 (5.9)/26.5 (4.3) F: 30 | MP: modified exercises; 3 times/week for 6 weeks (session length NR); University clinic (practitioner NR) GE: cycling, stretching, and strengthening; 3 times/week for 6 weeks (session length NR); University clinic (practitioner NR) | Muscle activation Pain Disability | Pressure biofeedback/ NR | NR |
| Bhadauria (2017) [56] India 44 (8) | 20–60 MP: 35.3 (12.9)/26.0 (6.2) LS: 32.7 (11.7)/21.8 (2.9) DS: 36.7 (10.7)/24.7 (4.6) ‡ M: 24, ‡ F: 12 | MP: 10 exercises; 60 min, 10 sessions over 3 weeks; Outpatient clinic, group of 12; Physiotherapist LS *: 16 exercises 10 s × 10 reps; 60 min, 10 sessions over 3 weeks; Outpatient clinic, group of 12; Physiotherapist DS: 14 exercises activating LES and RA 10 s × 10 reps; 60 min, 10 sessions over 3 weeks; Outpatient clinic, group of 12; Physiotherapist | Muscle activation Pain Disability | Pressure biofeedback/ NR | Baseline, 3 weeks |
| Mendes Tozim (2021) [61] Brazil 46 (5) | 60–75 MP: 66.7 (3.6)/31.1 (8.0) GE: 68.5 (4.9)/26.2 (3.5) EG: 68.0 (4.7)/29.1 (5.3) F: 46 | MP: 3–10 exercise variations increasing in number; fortnightly, 2 sets; 60 min, 2 times/week for 8 weeks; setting NR, group of 5; Physiotherapist Pilates instructor GE: walking, resistance training, stretching and balance exercises, fortnightly variations; 60 min, 2 times/week for 8 weeks; setting NR, group of 5; Physiotherapist EG *: 4 workshops; 30 min, fortnightly for 8 weeks; setting NR, group of 15; Physiotherapist | Muscle activation Pain | sEMG and lumbar dynamometer/ LM, IL | Baseline, 8 weeks |
| Nabavi (2018) [62] Iran 41 (0) | 18–55 SE: 40.8(8.2)/24.9 (4.4) GE: 34.1 (10.8)/26.4 (3.2) NR | SE: 16 exercises 10 reps × 10 s; 3 times/week for 4 weeks (session length NR); University clinic, group size NR; Physiotherapist GE: 16 routine exercises 10 reps × 10 s; 3 times/week for 4 weeks (session length NR); University clinic, group size NR; Physiotherapist | Muscle thickness Pain | Real-time ultrasound/ TrA, LM | Baseline, 4 weeks |
| Pilates vs. non-equivalent exercise intervention | |||||
| Batibay (2021) [59] Turkey 60 (7) | 18–60 MP: 49.3 (10.4)/25.0 (2.6) GE: 48.4 (9.3)/26.3 (2.7) F: 60 | MP: basic/intermediate exercises 3 × 10 reps; 60 min 3 times/week for 8 weeks; Outpatient clinic, group of 8; Physiotherapist GE: general stretching and strengthening exercises 3 × 10 reps; 60 min; 3 times/week for 8 weeks; Home, individual; nil supervision | Muscle thickness Muscle activation Pain Disability Quality of life | Real-time ultrasound/ Right LM, TrA IO, EO, RA | Baseline, 8 weeks |
| Brooks (2012) [57] Australia 64 (12) | 18–50 AP/MP: 36.2 (8.2)/NR GE: 36.3 (6.3)/NR M: 24, F: 40 | AP/MP: combination of mat and reformer Pilates exercises; 50–60 min, 3 times/week for 8 weeks; setting NR, group of 10; supervisor with >5 years’ experience GE: indoor stationary cycling training; 50–60 min, 3 times/week over 8 weeks; setting NR, group of 10; supervisor with >5 years’ experience | Muscle activation Pain Disability | sEMG/TrA, IO, LES, RA | Baseline, 8 weeks |
| Pilates vs. non-exercise intervention | |||||
| Cruz-Diaz (2017) [60] Spain 102 (4) | 18–50 MP: 36.9 (12.5)/NR AP: 35.5 (12.0)/NR Con: 36.3 (10.7)/NR ‡ M: 35, ‡ F: 63 | MP †: 21 exercises; 50 min 2 times/week for 12 weeks; setting NR, group of 4; Physiotherapist Pilates instructor AP †: 14 reformer exercises; 50 min 2 times/week for 12 weeks; setting NR, group of 4; Physiotherapist Pilates instructor CG: no intervention | Muscle thickness Pain Disability | Real-time ultrasound/TrA | Baseline, 6 weeks, 12 weeks |
| Sonmezer (2021) [63] Turkey 50 (10) | 20–35 MP: 29.0 (2.8)/23.8 (3.2) Con: 28.0 (2.1)/23.3 (2.6) F: 50 | MP: 18 exercises, 2–3 sets of 3–12 reps progressed fortnightly; 60–70 min, 2 times/week for 8 weeks; setting NR, individual; Physiotherapist Pilates instructor CG: no exercise prescription. Usual prenatal care. | Muscle activation Pain Disability Quality of life | Pressure biofeedback/ TrA | Baseline, 8 weeks |
| Study | Primary Outcomes | Secondary Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Muscle Thickness (Real-time Ultrasound) | Muscle Activation | Pain (Visual Analogue Scale) | Disability (Questionnaires) | Quality of Life (Questionnaires) | ||||||
| within Group | between Groups | within Group | between Groups | within Group | between Groups | within Group | between Groups | within Group | between Groups | |
| Pilates vs. exercise intervention | ||||||||||
| Ashtiani (2020) [58] | Biofeedback Bent knee fall out, Biering-Sorenson test ↑*+ Knee lift abdominal test ↑+ | No difference | ↓*+ | ↓*+ | Oswestry ↓*+ | Oswestry ND | ||||
| Bhadauria † (2017) [56] | Biofeedback ↑*+ | Biofeedback ↑+ | ↓*+ | ↓+ | Oswestry ↓*+ | Oswestry ↓+ | ||||
| Mendes-Tozim † (2021) [61] | Electromyography RMU ↑*+ LMU ↑+ | Electromyography RMU ↑*+ LMU no difference | Not reported | Not reported | ||||||
| Nabavi (2018) [62] | LLM, RLM, LTrA, RTrA ↑*+ | LLM, RLM, LTrA, RTrA ↑+ | ↓*+ | ↓+ | ||||||
| Pilates vs. non-equivalent exercise intervention | ||||||||||
| Batibay (2020) [59] | LM, TrA, IO ↑*+ | LM, TrA, IO ↑*+ | Sit-up test ↑*+ | Sit-up test ↑+ | ↓*+ | ↓*+ | BDI, QUB ↓*+ | BDI, QUB ↓*+ | SF-36 ↑*+ | SF-36 ↑*+ |
| Brooks (2012) [57] | Electromyography LTrA, IO ↓*+ RTrA, IO no difference | Electromyography Not reported | ↓*+ | ↓*+ | Oswestry ↓*+ | Oswestry ↓*+ | ||||
| Pilates vs. non exercise intervention | ||||||||||
| Cruz-Diaz ‡ (2017) [60] | TrA ↑*+ | TrA ↑*+ | ↓*+ | ↓+ | RMDQ, TSK ↓*+ | RMDQ, TSK ↓*+ | ||||
| Sonmezer (2021) [63] | Biofeedback ↑*+ | Biofeedback ↑*+ | ↓*+ | ↓*+ | Oswestry ↓*+ | Oswestry ↓*+ | NHP ↑− | NHP ↓+ | ||
| Certainty Assessment | No. of Participants | Impact | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | No. of Studies | Quality | Inconsistency | Indirectness | Imprecision | Other Considerations | Pilates | Control | Significance Reported | Certainty |
| Muscle activation (PBU) | 2 | fair * | serious † | serious ‡ | very serious § | none | 32 | 32 | significant impact reported in one study | ⨁◯◯◯ Very low |
| Muscle activation (sEMG) | 2 | good ** | serious †† | low concern | very serious § | none | 46 | 45 | significant impact reported in one study | ⨁◯◯◯ Very low |
| Muscle thickness (RTUS) | 3 | good ** | serious ††† | serious ‡ | very serious § | none | 118 | 81 | significant impact reported in two studies | ⨁◯◯◯ Very low |
| Pain (VAS) | 8 | fair * | serious †††† | serious ‡ | very serious § | none | 211 | 173 | significant impact reported in four studies | ⨁◯◯◯ Very low |
| Disability (ODI) | 4 | fair * | serious ††† | serious ‡ | very serious § | none | 61 | 60 | significant impact reported in two studies | ⨁◯◯◯ Very low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franks, J.; Thwaites, C.; Morris, M.E. Pilates to Improve Core Muscle Activation in Chronic Low Back Pain: A Systematic Review. Healthcare 2023, 11, 1404. https://doi.org/10.3390/healthcare11101404
Franks J, Thwaites C, Morris ME. Pilates to Improve Core Muscle Activation in Chronic Low Back Pain: A Systematic Review. Healthcare. 2023; 11(10):1404. https://doi.org/10.3390/healthcare11101404
Chicago/Turabian StyleFranks, Jennifer, Claire Thwaites, and Meg E. Morris. 2023. "Pilates to Improve Core Muscle Activation in Chronic Low Back Pain: A Systematic Review" Healthcare 11, no. 10: 1404. https://doi.org/10.3390/healthcare11101404
APA StyleFranks, J., Thwaites, C., & Morris, M. E. (2023). Pilates to Improve Core Muscle Activation in Chronic Low Back Pain: A Systematic Review. Healthcare, 11(10), 1404. https://doi.org/10.3390/healthcare11101404






