The Search for an Outcome Variable That Measures Both Quality and Processes in Cardiac Surgery: Comparing the Quality Process Index and Mortality
Abstract
:1. Introduction
- How do the Quality Process Index and mortality rates compare as indicators of quality and process in healthcare in the Amsterdam Cardiosurgical Database?
- How was the evolution of quality and processes over ten years in the Amsterdam Cardiosurgical Database?
2. Materials and Methods
2.1. Data Collection
2.2. Metrics
2.3. Calculation of Quality Process Index (QPI)
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Quality Process Index Total
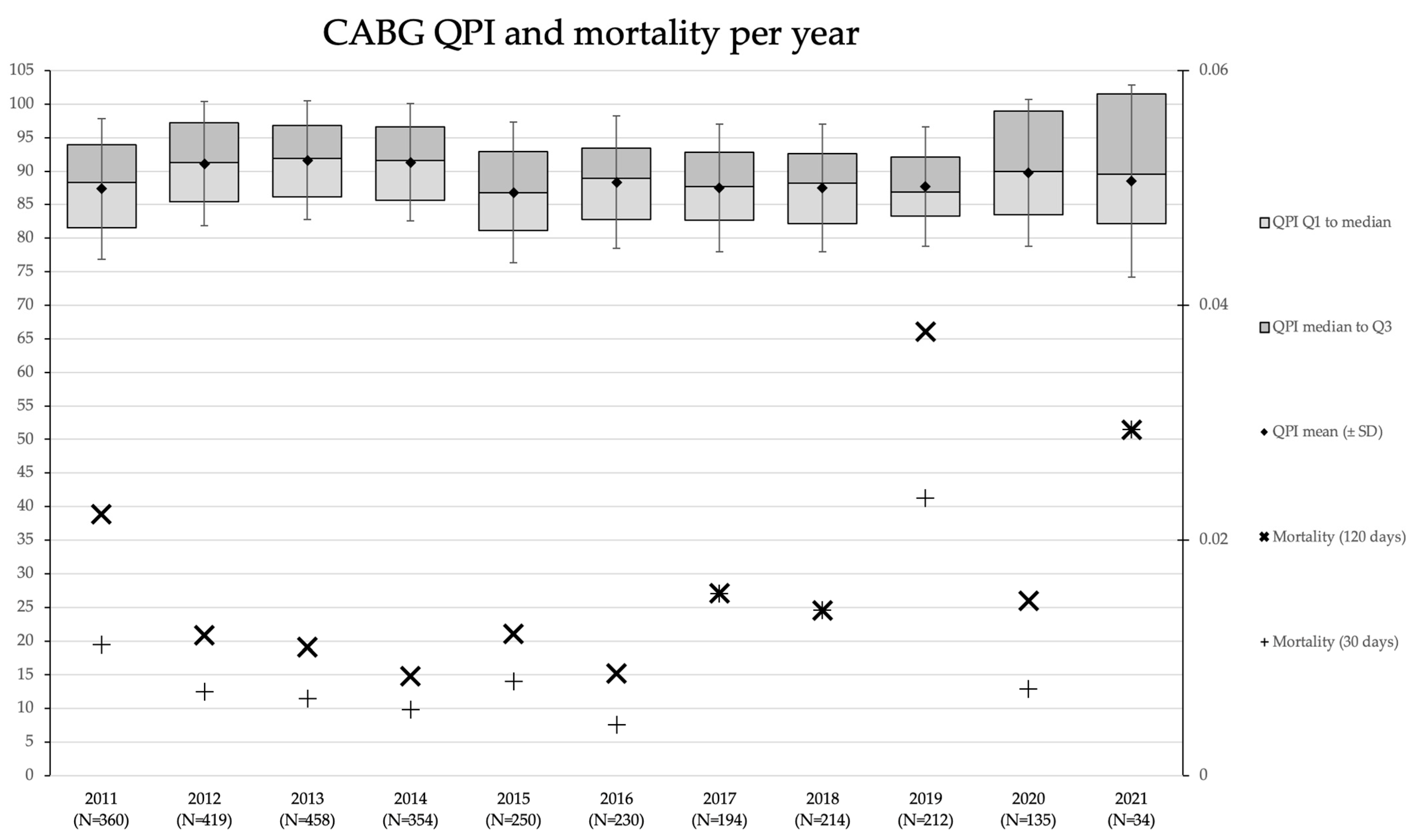
3.3. QPI CABG and Mortality Rates
4. Conclusions
5. Discussion
5.1. How Do the Quality Process Index and Mortality Rates Compare as Indicators of Quality and Processes in the Amsterdam Cardiosurgical Database?
5.2. How Was the Evolution of Quality and Processes over Ten Years in the Amsterdam Cardiosurgical Database?
5.3. Reflection on Method
5.4. In Perspective: QPI versus EQI
5.5. Generalizability, Limitations, and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
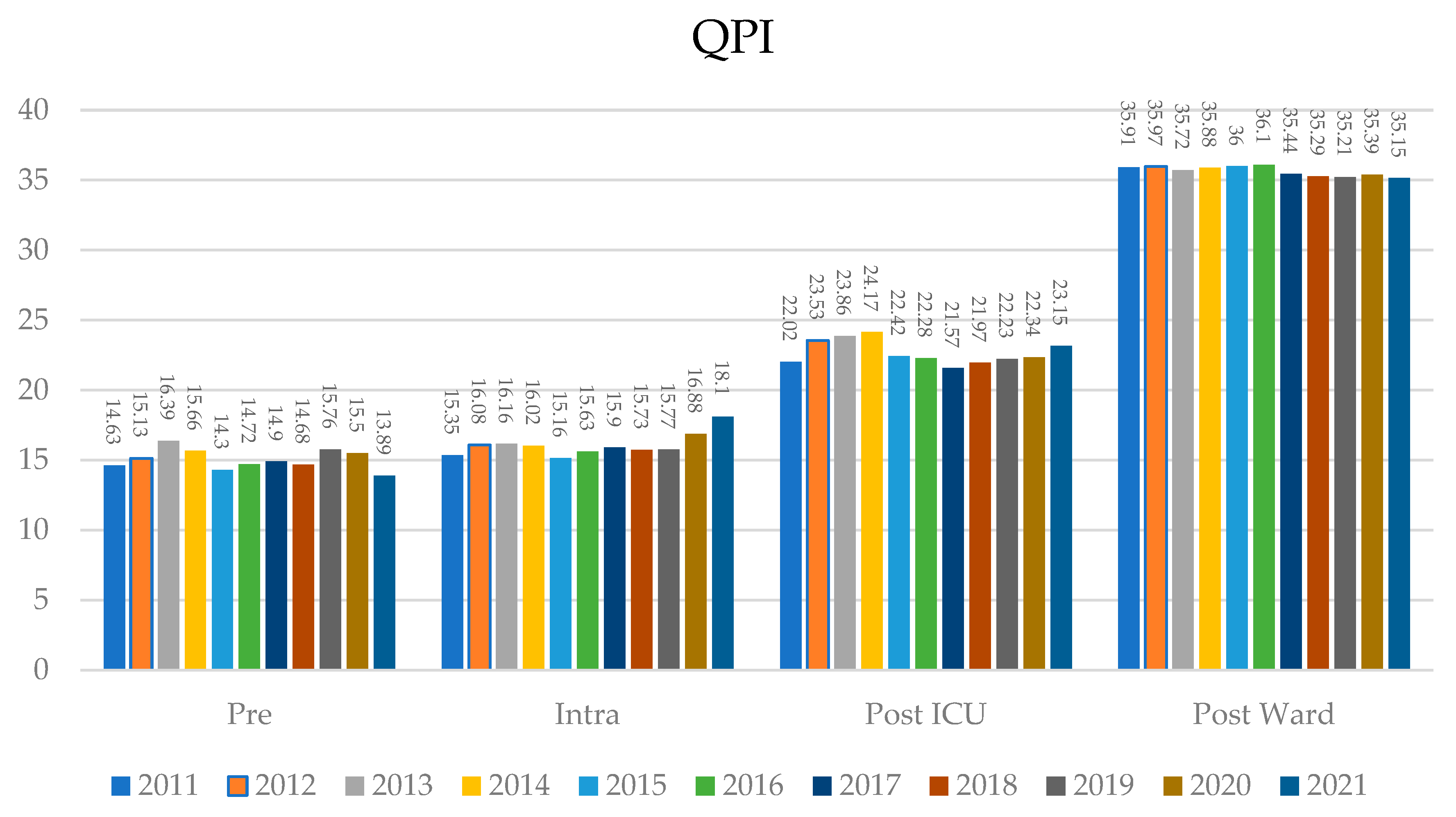
Appendix A. Quality Process Index per Type of Surgery
- Table A1: QPI total and per phase per year (means).
- Table A2: Descriptive characteristics total and per type of procedure (means).
- Table A3: Correlation matrix of metrics.
- Figure A1: QPI total and mortality per type of surgery.
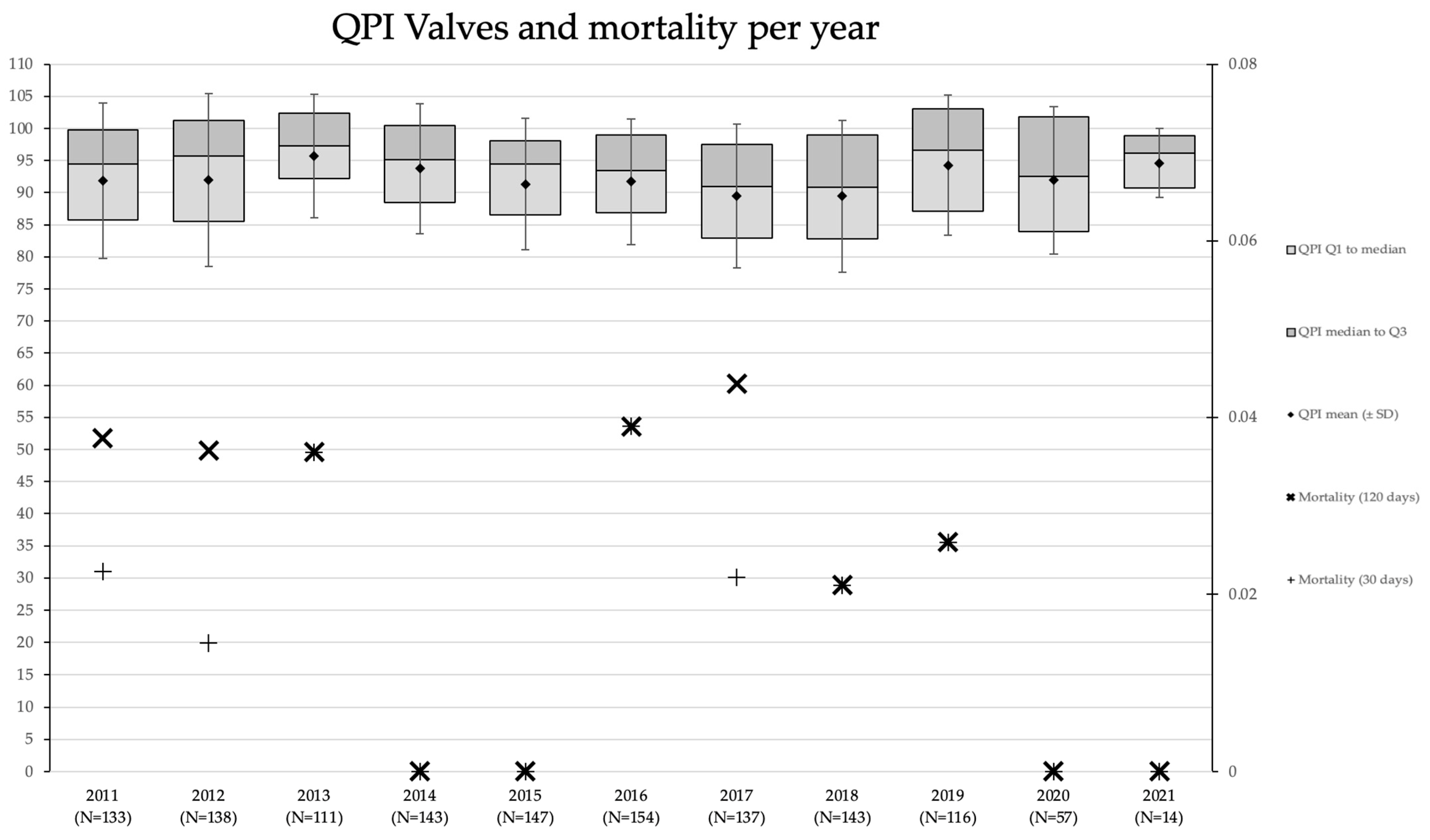
- Figure A2: QPI valves and mortality per year.
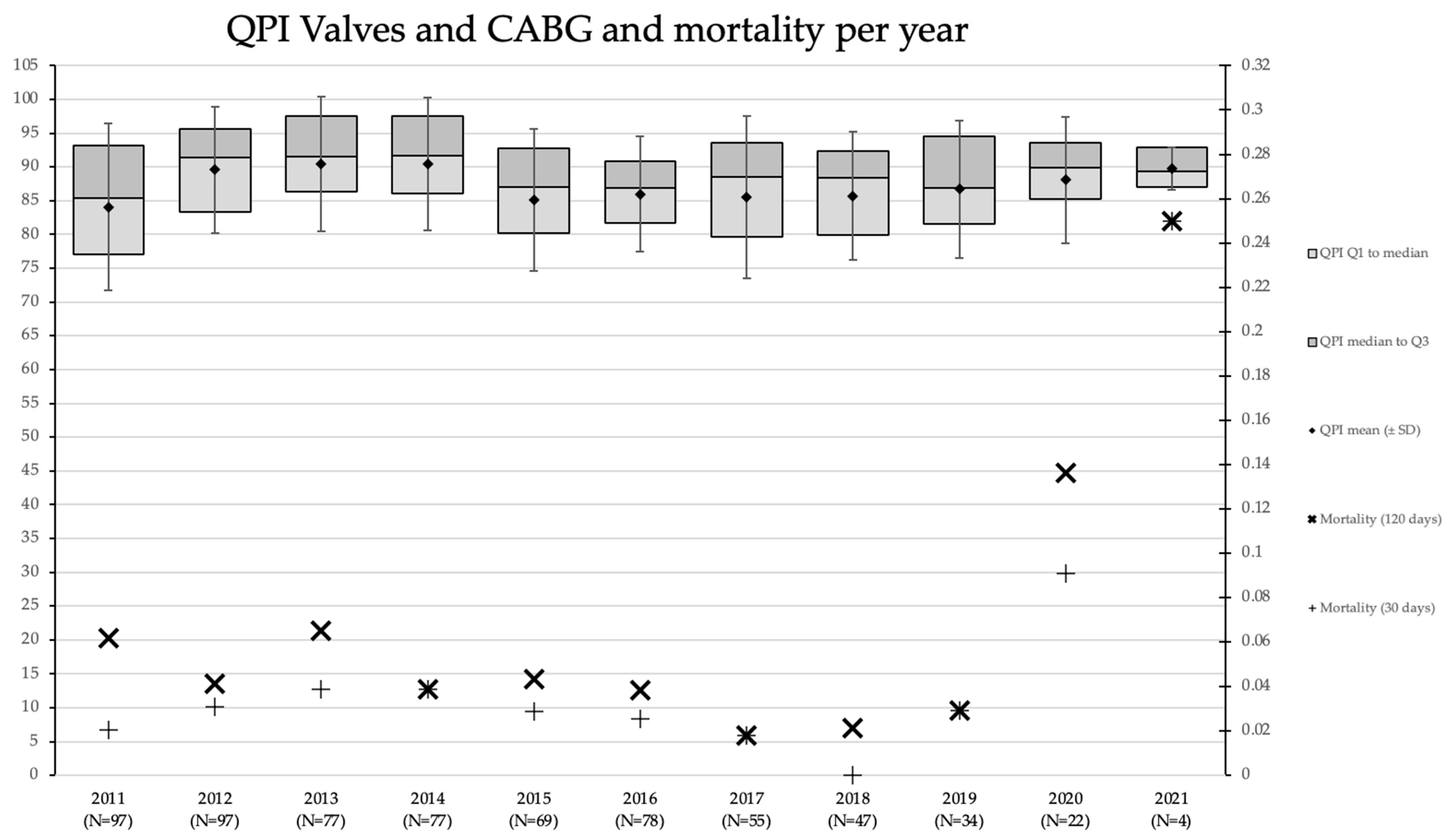
- Figure A3: QPI Valves and CABG and mortality per year.
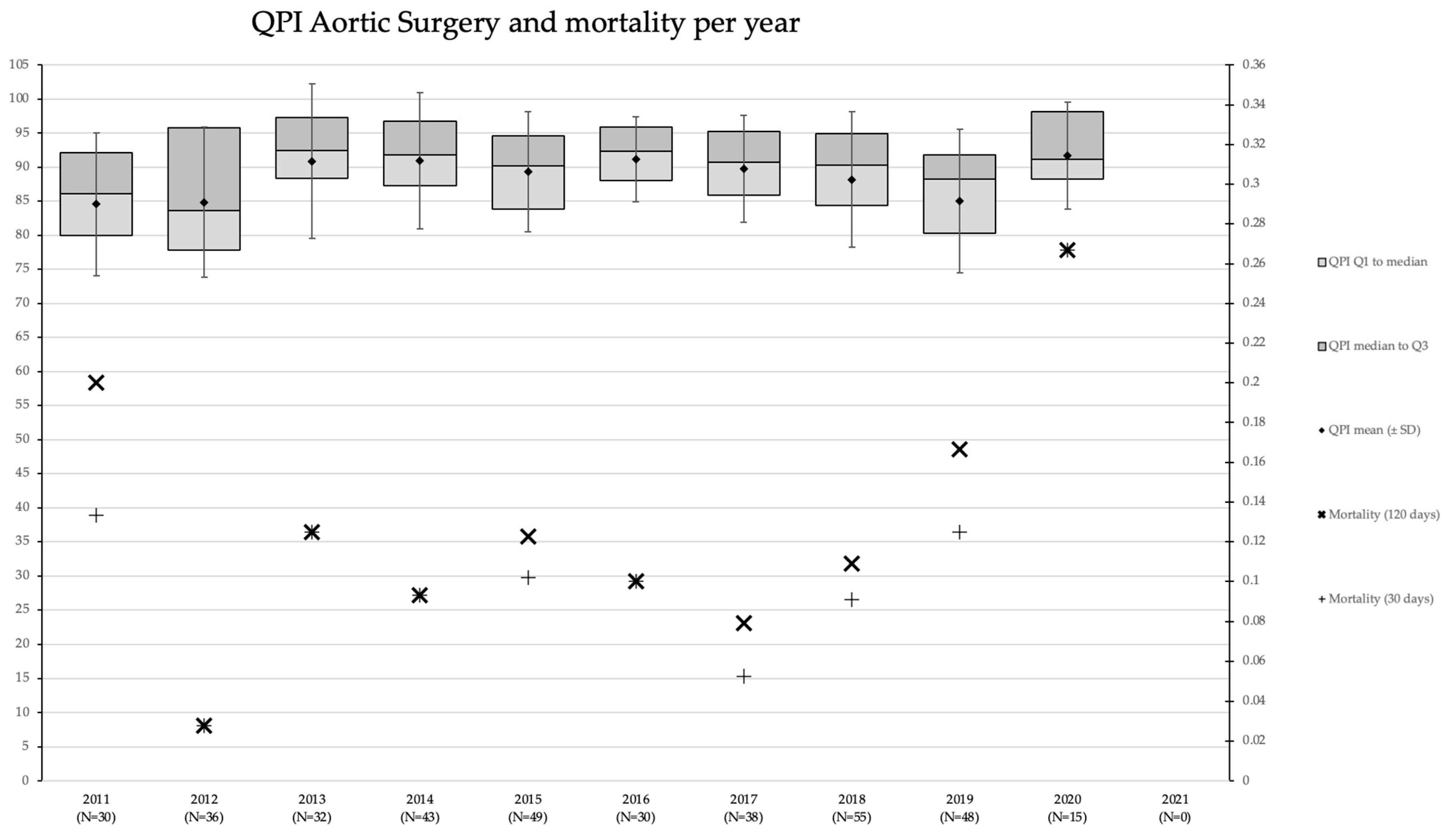
- Figure A4: QPI Aortic surgery and mortality per year.
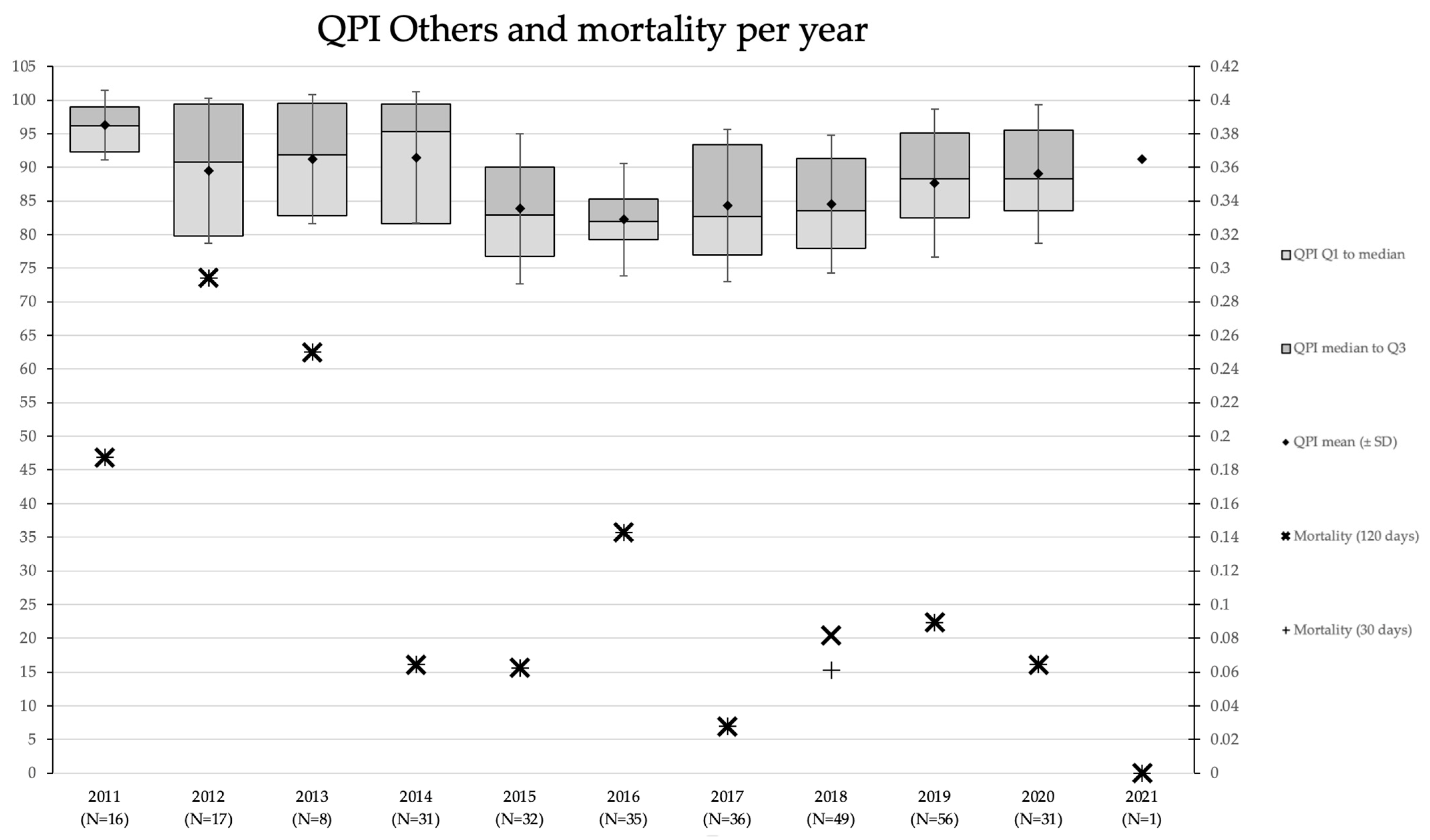
- Figure A5: QPI Others and mortality per year.
| Total | Pre | Intra | Post ic | Post Ward | |
|---|---|---|---|---|---|
| 2011 | 87.91 (SD 11.37) | 14.63 (SD 4.71) | 15.35 (SD 5.36) | 22.02 (SD 5.71) | 35.91 (SD 2.96) |
| 2012 | 90.70 (SD 10.44) | 15.13 (SD 4.55) | 16.08 (SD 5.28) | 23.53 (SD 5.16) | 35.97 (SD 2.78) |
| 2013 | 92.12 (SD 9.36) | 16.39 (SD 3.93) | 16.16 (SD 5.12) | 23.86 (SD 5.03) | 35.72 (SD 2.89) |
| 2014 | 91.73 (SD 9.36) | 15.66 (SD 4.26) | 16.02 (SD 4.98) | 24.17 (SD 4.34) | 35.88 (SD 2.89) |
| 2015 | 87.88 (SD 10.57) | 14.30 (SD 4.68) | 15.16 (SD 5.29) | 22.42 (SD 5.46) | 36.00 (SD 3.16) |
| 2016 | 88.73 (SD 9.72) | 14,72 (SD 4.60) | 15.63 (SD 4.94) | 22.28 (SD 4.48) | 36.10 (SD 3.15) |
| 2017 | 87.77 (SD 10.48) | 14.90 (SD 4.72) | 15.90 (SD 5.69) | 21.57 (SD 4.51) | 35.44 (SD 3.94) |
| 2018 | 87.67 (SD 10.39) | 14.68 (SD 4.76) | 15.73 (SD 5.68) | 21.97 (SD 4.24) | 35.29 (SD 3.36) |
| 2019 | 88.98 (SD 10.42) | 15.76 (SD 3.97) | 15.77 (SD 5.92) | 22.23 (SD 3.95) | 35.21 (SD 3.63) |
| 2020 | 90.10 (SD 10.72) | 15.50 (SD 4.24) | 16.88 (SD 6.14) | 22.34 (SD 3.86) | 35.39 (SD 3.20) |
| 2021 | 90.30 (SD 12.04) | 13.89 (SD 5.61) | 18.10 (SD 6.28) | 23.15 (SD 3.20) | 35.15 (SD 3.61) |
| Total | 89.51 (SD 10.40) | 15.17 (SD 4.51) | 15.85 (SD 5.40) | 22.76 (SD 4.87) | 35.73 (SD 3.18) |
| Procedures | Age (Years) | Weight (kg) | Height (cm) | Gender | Euroscore II | |
|---|---|---|---|---|---|---|
| Total | 5498 | 67.4 (SD 10.3) | 83.0 (SD 15.3) | 174.0 (SD 9.4) | Male 4083 Female 1415 | 3.6 (SD 6.8) |
| CABG | 2860 | 67.3 (SD 9.33) | 84.2 (SD 14.7) | 174.6 (SD 8.9) | Male 2386 Female 474 | 2.6 (SD 3.8) |
| Valve | 1293 | 68.3 (SD 10.6) | 81.2 (SD 15.5) | 172.7 (SD 9.9) | Male 782 Female 511 | 2.8 (SD 5.7) |
| Aortic surgery | 376 | 63.1 (SD 11.2) | 84.2 (SD 16.3) | 176.9 (SD 10.3) | Male 261 Female 115 | 11.2 (SD 12.5) |
| CABG + valve | 657 | 68.4 (SD 10.6) | 81.8 (SD 14.5) | 172.2 (SD 8.9) | Male 473 Female 184 | 4.4 (SD 6.5) |
| Others | 311 | 60.5 (SD 14.7) | 81.1 (SD 18.4) | 173.7 (SD 10) | Male 181 Female 131 | 8.2 (SD 13.1) |
| Correlations | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Readmissions | Referral to Treatment Times (Days) | Length of Stay in Intensive Care Unit (Days) | Cardiopulmonary Bypass Time (Minutes) | X(clamp)time | Bloodloss 24 h | Bloodloss 6 h | Re-thoracotomy | Cardiac tamponade | Mediastinitis | Referral to Decision Time (Days) | Length of Stay in Surgical Ward | Mortality 30 Days | Mortality 120 Days | ||
| Readmissions | Pearson Correlation | 1 | −0.064 ** | 0.052 ** | −0.049 ** | −0.061 ** | 0.018 | 0.024 | −0.016 | −0.013 | −0.005 | −0.017 | 0.069 ** | 0.018 | 0.013 |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.300 | 0.164 | 0.228 | 0.352 | 0.719 | 0.197 | 0.000 | 0.182 | 0.351 | ||
| N | 5498 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5498 | 5498 | 5498 | 5493 | 5398 | 5497 | 5497 | |
| Referral to treatment times (days) | Pearson Correlation | −0.064 ** | 1 | −0.049 ** | 0.117 ** | 0.143 ** | −0.038 * | −0.044 * | 0.000 | 0.016 | 0.023 | 0.129 ** | −0.017 | −0.074 ** | −0.081 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.029 | 0.012 | 0.977 | 0.241 | 0.088 | 0.000 | 0.213 | 0.000 | 0.000 | ||
| N | 5493 | 5493 | 5434 | 5476 | 5476 | 3244 | 3244 | 5493 | 5493 | 5493 | 5493 | 5394 | 5493 | 5493 | |
| Length of stay in intensive care unit (days) | Pearson Correlation | 0.052 ** | −0.049 ** | 1 | 0.147 ** | 0.079 ** | 0.154 ** | 0.136 ** | 0.114 ** | 0.099 ** | 0.005 | −0.008 | 0.201 ** | 0.109 ** | 0.250 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.705 | 0.533 | 0.000 | 0.000 | 0.000 | ||
| N | 5438 | 5434 | 5438 | 5427 | 5426 | 3243 | 3243 | 5438 | 5438 | 5438 | 5434 | 5398 | 5438 | 5438 | |
| Cardiopulmonary bypass time (minutes) | Pearson Correlation | −0.049 ** | 0.117 ** | 0.147 ** | 1 | 0.893 ** | 0.214 ** | 0.170 ** | 0.078 ** | 0.082 ** | 0.002 | 0.021 | 0.203 ** | 0.138 ** | 0.135 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.886 | 0.125 | 0.000 | 0.000 | 0.000 | ||
| N | 5480 | 5476 | 5427 | 5480 | 5479 | 3244 | 3244 | 5480 | 5480 | 5480 | 5476 | 5388 | 5480 | 5480 | |
| X(clamp)time | Pearson Correlation | −0.061 ** | 0.143 ** | 0.079 ** | 0.893 ** | 1 | 0.211 ** | 0.174 ** | 0.074 ** | 0.089 ** | 0.011 | 0.044 ** | 0.183 ** | 0.074 ** | 0.077 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.430 | 0.001 | 0.000 | 0.000 | 0.000 | ||
| N | 5480 | 5476 | 5426 | 5479 | 5480 | 3244 | 3244 | 5480 | 5480 | 5480 | 5476 | 5387 | 5480 | 5480 | |
| Bloodloss 24 h | Pearson Correlation | 0.018 | −0.038 * | 0.154 ** | 0.214 ** | 0.211 ** | 1 | 0.864 ** | 0.372 ** | 0.100 ** | −0.001 | 0.033 | 0.139 ** | 0.065 ** | 0.069 ** |
| Sig. (2-tailed) | 0.300 | 0.029 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.950 | 0.062 | 0.000 | 0.000 | 0.000 | ||
| N | 3244 | 3244 | 3243 | 3244 | 3244 | 3244 | 3239 | 3244 | 3244 | 3244 | 3244 | 3229 | 3244 | 3244 | |
| Bloodloss 6 h | Pearson Correlation | 0.024 | −0.044 * | 0.136 ** | 0.170 ** | 0.174 ** | 0.864 ** | 1 | 0.360 ** | 0.074 ** | 0.002 | 0.054 ** | 0.097 ** | 0.057 ** | 0.061 ** |
| Sig. (2-tailed) | 0.164 | 0.012 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.912 | 0.002 | 0.000 | 0.001 | 0.000 | ||
| N | 3244 | 3244 | 3243 | 3244 | 3244 | 3239 | 3244 | 3244 | 3244 | 3244 | 3244 | 3229 | 3244 | 3244 | |
| Re-thoracotomy | Pearson Correlation | −0.016 | 0.000 | 0.114 ** | 0.078 ** | 0.074 ** | 0.372 ** | 0.360 ** | 1 | 0.323 ** | 0.142 ** | 0.019 | 0.110 ** | 0.085 ** | 0.101 ** |
| Sig. (2-tailed) | 0.228 | 0.977 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.153 | 0.000 | 0.000 | 0.000 | ||
| N | 5498 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5498 | 5498 | 5498 | 5493 | 5398 | 5497 | 5497 | |
| Cardiac tamponade | Pearson Correlation | −0.013 | 0.016 | 0.099 ** | 0.082 ** | 0.089 ** | 0.100 ** | 0.074 ** | 0.323 ** | 1 | 0.062 ** | 0.017 | 0.124 ** | 0.046 ** | 0.072 ** |
| Sig. (2-tailed) | 0.352 | 0.241 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.211 | 0.000 | 0.001 | 0.000 | ||
| N | 5498 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5498 | 5498 | 5498 | 5493 | 5398 | 5497 | 5497 | |
| Mediastinitis | Pearson Correlation | −0.005 | 0.023 | 0.005 | 0.002 | 0.011 | −0.001 | 0.002 | 0.142 ** | 0.062 ** | 1 | 0.011 | 0.066 ** | 0.045 ** | 0.069 ** |
| Sig. (2-tailed) | 0.719 | 0.088 | 0.705 | 0.886 | 0.430 | 0.950 | 0.912 | 0.000 | 0.000 | 0.407 | 0.000 | 0.001 | 0.000 | ||
| N | 5498 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5498 | 5498 | 5498 | 5493 | 5398 | 5497 | 5497 | |
| Referral to decision time (days) | Pearson Correlation | −0.017 | 0.129 ** | −0.008 | 0.021 | 0.044 ** | 0.033 | 0.054 ** | 0.019 | 0.017 | 0.011 | 1 | 0.020 | −0.004 | 0.008 |
| Sig. (2-tailed) | 0.197 | 0.000 | 0.533 | 0.125 | 0.001 | 0.062 | 0.002 | 0.153 | 0.211 | 0.407 | 0.139 | 0.753 | 0.547 | ||
| N | 5493 | 5493 | 5434 | 5476 | 5476 | 3244 | 3244 | 5493 | 5493 | 5493 | 5493 | 5394 | 5493 | 5493 | |
| Length of stay in surgical ward (days) | Pearson Correlation | 0.069 ** | −0.017 | 0.201 ** | 0.203 ** | 0.183 ** | 0.139 ** | 0.097 ** | 0.110 ** | 0.124 ** | 0.066 ** | 0.020 | 1 | −0.059 ** | 0.002 |
| Sig. (2-tailed) | 0.000 | 0.213 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.139 | 0.000 | 0.895 | ||
| N | 5398 | 5394 | 5398 | 5388 | 5387 | 3229 | 3229 | 5398 | 5398 | 5398 | 5394 | 5398 | 5398 | 5398 | |
| Mortality 30 days | Pearson Correlation | 0.018 | −0.074 ** | 0.109 ** | 0.138 ** | 0.074 ** | 0.065 ** | 0.057 ** | 0.085 ** | 0.046 ** | 0.045 ** | −0.004 | −0.059 ** | 1 | 0.874 ** |
| Sig. (2-tailed) | 0.182 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.001 | 0.000 | 0.001 | 0.001 | 0.753 | 0.000 | 0.000 | ||
| N | 5497 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5497 | 5497 | 5497 | 5493 | 5398 | 5497 | 5497 | |
| Mortality 120 days | Pearson Correlation | 0.013 | −0.081 ** | 0.250 ** | 0.135 ** | 0.077 ** | 0.069 ** | 0.061 ** | 0.101 ** | 0.072 ** | 0.069 ** | 0.008 | 0.002 | 0.874 ** | 1 |
| Sig. (2-tailed) | 0.351 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.547 | 0.895 | 0.000 | ||
| N | 5497 | 5493 | 5438 | 5480 | 5480 | 3244 | 3244 | 5497 | 5497 | 5497 | 5493 | 5398 | 5497 | 5497 | |

References
- Sharma, V.; Glotzbach, J.P.; Ryan, J.; Selzman, C.H. Evaluating Quality in Adult Cardiac Surgery. Tex. Heart Inst. J. 2021, 48, e197136. [Google Scholar] [CrossRef] [PubMed]
- Grover, F.L.; Cleveland, J.C.; Shroyer, A.L. Quality Improvement in Cardiac Care. Arch. Surg. 2002, 137, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Grover, F.L.; Johnson, R.R.; Laurie, A.; Shroyer, W.; Marshall, G.; Hammermeister, K.E. The veterans affairs continuous improvement in cardiac surgery study. Ann. Thorac. Surg. 1994, 58, 1845–1851. [Google Scholar] [CrossRef] [PubMed]
- Grover, F.L.; Shahian, D.M.; Clark, R.E.; Edwards, F.H. The STS national database. Ann. Thorac. Surg. 2014, 97, S48–S54. [Google Scholar] [CrossRef] [PubMed]
- Head, S.J.; Howell, N.J.; Osnabrugge, R.L.; Bridgewater, B.; Keogh, B.E.; Kinsman, R.; Walton, P.; Gummert, J.F.; Pagano, D.; Kappetein, A.P. The European Association for Cardio-Thoracic Surgery (EACTS) database: An introduction. Eur. J. Cardio-Thoracic. Surg. 2013, 44, e175–e180. [Google Scholar] [CrossRef] [PubMed]
- Netherlands Heart Registration. Annual Report 2021. Available online: https://nhr.nl/wp-content/uploads/2021/09/NHR-Rapportage-2021-090921.pdf (accessed on 12 January 2023).
- Cerfolio, R.J.; Chang, S.H. Efficiency Quality Index (EQI)—Implementing a Novel Metric That Delivers Overall Institutional Excellence and Value for Patients. Front. Surg. 2020, 7, 604916. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, G.T.; Plume, S.K.; Olmstead, E.M.; Morton, J.R.; Maloney, C.T.; Nugent, W.C.; Hernandez, F.; Clough, R.; Leavitt, B.J.; Coffin, L.H.; et al. A regional intervention to improve the hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. JAMA 1996, 275, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, H.; Miyata, H.; Tanemoto, K.; Saiki, Y.; Yokoyama, H.; Fukuchi, E.; Motomura, N.; Ueda, Y.; Takamoto, S. Quality improvement in cardiovascular surgery: Results of a surgical quality improvement programme using a nationwide clinical database and database-driven site visits in Japan. BMJ Qual. Saf. 2020, 29, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Shojania, K.G.; Forster, A.J. Hospital mortality: When failure is not a good measure of success. Can. Med. Assoc. J. 2008, 179, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Craig, K.J.T.; McKillop, M.M.; Huang, H.T.; George, J.; Punwani, E.S.; Rhee, K.B.U.S. hospital performance methodologies: A scoping review to identify opportunities for crossing the quality chasm. BMC Health Serv. Res. 2020, 20, 640. [Google Scholar] [CrossRef]
- Kotz, S.; Johnson, N.L. Process Capability Indices; Chapman & Hall: Boca Raton, FL, USA, 1993. [Google Scholar]
- Jaworeck, S. A New Approach for Constructing a Health Care Index including the Subjective Level. Int. J. Environ. Res. Public Health 2022, 19, 9686. [Google Scholar] [CrossRef] [PubMed]
- Björnberg, A.; Phang, A.Y. Euro Health Consumer Index Health Consumer Powerhouse. 2019. Available online: https://healthpowerhouse.com/media/EHCI-2018/EHCI-2018-report.pdf (accessed on 6 April 2023).
- Bloomberg’s Global Health Index for 2020. Available online: https://worldhealth.net/news/bloombergs-global-health-index-2020/ (accessed on 6 April 2023).
- Economist Impact. Global Health Index Methodology. 2021. Available online: https://www.ghsindex.org/wp-content/uploads/2021/11/2021_GHSindex_Methodology_FINAL.pdf (accessed on 6 April 2023).
- Office for National Statistics. Health Index Methods and Development: 2015 to 2020. 2022. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/methodologies/healthindexmethodsanddevelopment2015to2019 (accessed on 6 April 2023).
- De Mast, J.; Does, R.J.M.M.; De Koning, H.; Lameijer, B.A.; Lokkerbol, J. Operational Excellence with Lean Six Sigma; Van Haren Publishing: Hertogenbosch, The Netherlands, 2022. [Google Scholar]
- Steiner, S.; Abraham, B.; MacKay, J. Understanding Process Capability Indices; Institute for Improvement of Quality and Productivity, Department of Statistics and Actuarial Science, University of Waterloo: Waterloo, ON, Canada, 1997. [Google Scholar]
- Schretlen, S.; Hoefsmit, P.; Kats, S.; van Merode, G.; Maessen, J.; Zandbergen, R. Reducing surgical cancellations: A successful application of Lean Six Sigma in healthcare. BMJ Open Qual. 2021, 10, e001342. [Google Scholar] [CrossRef] [PubMed]
- Yates, M.T.; Balmforth, D.; Kirmani, B.H.; Acharya, M.; Jeganathan, R.; Ngaage, D.; Kanani, M.; Deglurkar, I.; Lopez-Marco, A.; Sanders, J.; et al. A multi-centre prospective cohort study of patients on the elective waiting list for cardiac surgery during the COVID-19 pandemic. J. R. Soc. Med. 2022, 115, 348–353. [Google Scholar] [CrossRef] [PubMed]
- Bickel, P.J.; Doksum, K.A. Mathematical Statistics: Basic Ideas and Selected Topics, 2nd ed.; Prentice-Hall: Upper Saddle River, NJ, USA, 2001. [Google Scholar]
- Hazra, A.; Gogtay, N. Biostatistics series module 6: Correlation and linear regression. Indian J. Dermatol. 2016, 61, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Coulson, T.G.; Mullany, D.V.; Reid, C.M.; Bailey, M.; Pilcher, D. Measuring the quality of perioperative care in cardiac surgery. Eur. Hearth J.—Qual. Care Clin. Outcomes 2016, 3, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Quentin, W.; Partanen, V.M.; Browwood, I.; Klazinga, N. Measuring Healthcare Quality. Improving Healthcare Quality in Europe: Characteristics, Effectiveness and Implementation of Different Strategies; European Observatory on Health Systems: Copenhagen, Denmark, 2019. [Google Scholar]
- Panesar, A. Machine Learning and AI for Healthcare; Apress: Berkeley, CA, USA, 2021. [Google Scholar]

| Phase | Metric | |
|---|---|---|
| Preoperative | Referral to decision time (days) | 10 |
| Referral to treatment time (days) | 10 | |
| Intraoperative | Cardiopulmonary bypass time (minutes) | 15 |
| Rethoracotomy (binary: yes/no) | 10 | |
| Postoperative ICU | Length of stay in intensive care unit (days) | 15 |
| Blood loss after 24 h (milliliters) | 15 | |
| Postoperative ward | Length of stay in surgical ward (days) | 15 |
| Cardiac tamponade (binary: yes/no) | 10 | |
| Mediastinitis (binary: yes/no) | 10 | |
| Readmissions (binary: yes/no) | 10 | |
| Total (maximum) | 120 |
| Procedures | Age (Years) | Weight (kg) | Gender | Height (cm) | Euroscore II | Mortality 30 Days | Mortality 120 Days | |
|---|---|---|---|---|---|---|---|---|
| 2011 | 636 | 67.70 (SD 10.38) | 82.52 (SD 13.855) | 0.24 (SD 0.43) | 173.42 (SD 8.89) | 3.108 (SD 4.5839) | 0.025 | 0.044 |
| 2012 | 707 | 67.26 (SD 10.17) | 82.88 (SD 14.66) | 0.26 (SD 0.44) | 173.74 (SD 9.60) | 3.51 (SD 5.72) | 0.024 | 0.028 |
| 2013 | 686 | 67.94 (SD 10.0) | 82.59 (SD 15.52) | 0.24 (SD 0.43) | 173.50 (SD 8.74) | 3.50 (SD 6.65) | 0.023 | 0.029 |
| 2014 | 648 | 66.76 (SD 10.75) | 83.48 (15.24) | 0.24 (SD 0.43) | 173.97 (SD 9.60) | 3.50 (SD 6.57) | 0.017 | 0.019 |
| 2015 | 547 | 67.82 (SD 10.20) | 83.24 (SD 15.51) | 0.26 (SD 0.44) | 173.23 (SD 9.46) | 3.48 (SD 6.03) | 0.020 | 0.026 |
| 2016 | 527 | 67.99 (SD 9.59) | 82.92 (SD 15.80) | 0.29 (SD 0.45) | 173.18 (SD 9.82) | 3.56 (SD 6.90) | 0.032 | 0.036 |
| 2017 | 460 | 67.34 (SD 10.67) | 83.84 (SD 15.31) | 0.27 (SD 0.45) | 174.94 (SD 9.06) | 3.93 (SD 7.66) | 0.022 | 0.030 |
| 2018 | 508 | 67.70 (SD 10.31) | 82.16 (15.04) | .25 (SD 0.436) | 174.92 (9.05) | 4.22 (SD 8.69) | 0.028 | 0.033 |
| 2019 | 466 | 66.81 (SD 10.53) | 82.20 (SD 16.27) | 0.29 (SD 0.45) | 174.39 (SD 9.82) | 4.71 (SD 9.39) | 0.043 | 0.054 |
| 2020 | 260 | 66.12 (SD 11.08) | 85.28 (SD 16.26) | 0.24 (SD 0.43) | 175.56 (9.95) | 3.01 (SD 6.13) | 0.035 | 0.042 |
| 2021 | 53 | 68.46 (SD 10.42) | 85.23 (SD 15.15) | 0.17 (SD 0.379) | 175.83 (SD 9.05) | 1.76 (SD 1.67) | 0.038 | 0.038 |
| Total | 5498 | 67.4 (10.33) | 83.01 (SD 15.26) | 0.26 (SD 0.44) | 173.96 (SD 9.38) | 3.62 (SD 6.84) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoefsmit, P.C.; Jansen, E.K.; Does, R.J.M.M.; Zandbergen, H.R. The Search for an Outcome Variable That Measures Both Quality and Processes in Cardiac Surgery: Comparing the Quality Process Index and Mortality. Healthcare 2023, 11, 1419. https://doi.org/10.3390/healthcare11101419
Hoefsmit PC, Jansen EK, Does RJMM, Zandbergen HR. The Search for an Outcome Variable That Measures Both Quality and Processes in Cardiac Surgery: Comparing the Quality Process Index and Mortality. Healthcare. 2023; 11(10):1419. https://doi.org/10.3390/healthcare11101419
Chicago/Turabian StyleHoefsmit, Paulien C., Evert K. Jansen, Ronald J. M. M. Does, and H. Reinier Zandbergen. 2023. "The Search for an Outcome Variable That Measures Both Quality and Processes in Cardiac Surgery: Comparing the Quality Process Index and Mortality" Healthcare 11, no. 10: 1419. https://doi.org/10.3390/healthcare11101419






