Support Provided by Caregivers for Community-Dwelling Obesity Individuals: Focus on Elderly and Hispanics
Abstract
:1. Introduction
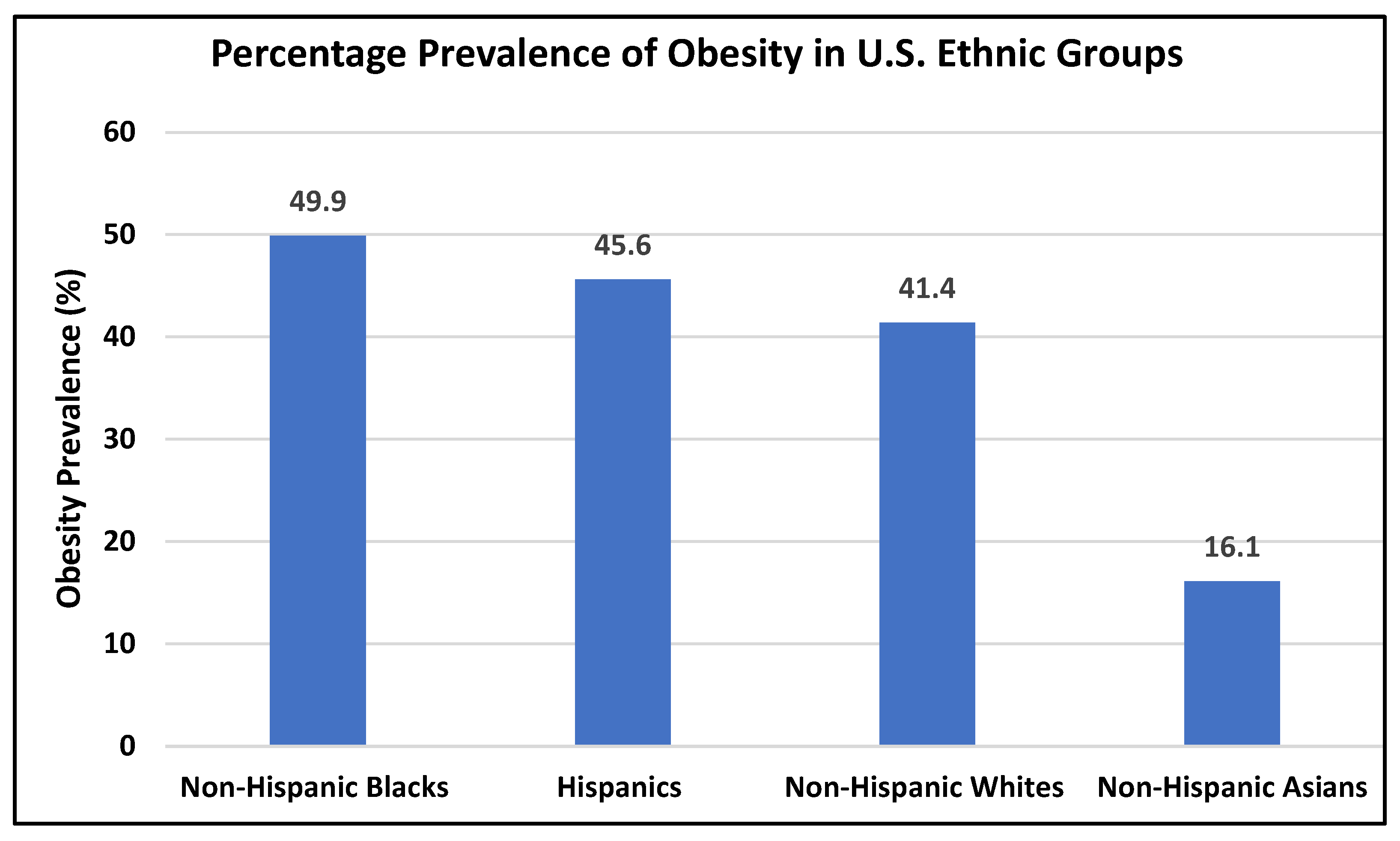
2. Obesity Rates According to Age, Sex, and Ethnic Groups: Focus on Hispanics
3. Factors That Contribute to Obesity
3.1. Genetic, Epigenetic and Biological Factors of Obesity
Focus on Hispanics
3.2. Medication and Disease Factors
Focus on Hispanics
3.3. Environmental and Socio-Demographic Factors
Focus on Hispanics
3.4. Diet and Exercise Factors
Focus on Hispanics
4. Obesity Management Strategies
4.1. Lifestyle Interventions
4.2. Dietary Calorie Restriction
4.3. Physical Activity
4.4. Weight Management and Lifestyle Intervention for the Elderly
4.5. Bariatric Surgery
4.6. Bariatric Equipment
- Bariatric mattresses,
- Hoists,
- Slings,
- Bed transfer boards,
- Bariatric wheelchairs,
- Bariatric rollators.
5. Caregivers for Individuals with Obesity
5.1. Challenges Encountered by Family Caregivers
5.1.1. A. Increasing Caregiver Age
5.1.2. B. Risk of Caregiver Injury
5.2. Caregiver Management Tools
- Availability of appropriate bariatric equipment and supplies,
- Can the home or patient care location incorporate and fit this equipment?
- Adequate walking space in hallways and doorways,
- Adequate number of caregivers or nursing staff.
6. Conclusions and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Ad-36 | Adenovirus-36 |
| AgRP | Agoutirelated protein |
| BAT | Brown adipose tissue |
| BMI | Body mass index |
| CDC | Centers for Disease Control |
| CNS | Central nervous system |
| CR | Calorie restriction |
| CER | Continuous energy restriction |
| DNA | Deoxyribonucleic acid |
| CVD | Cardiovascular disease |
| GDP | Gross domestic product |
| NCD | Non-communicable diseases |
| NHANES | National Health and Nutrition Examination Survey |
| NPY | Neuropeptide-y |
| OAO | Overweight and obesity |
| POMC | Proopiomelanocortin |
| RMR | Resting metabolic rate |
| SES | Socio-economic status |
| U.S. | United States |
| WAT | White adipose tissue |
References
- Basu, T.; Selman, A.; Reddy, A.P.; Reddy, P.H. Current Status of Obesity: Protective Role of Catechins. Antioxid 2023, 12, 474. [Google Scholar] [CrossRef] [PubMed]
- Selman, A.; Burns, S.; Reddy, A.P.; Culberson, J.; Reddy, P.H. The Role of Obesity and Diabetes in Dementia. Int. J. Mol. Sci. 2022, 23, 9267. [Google Scholar] [CrossRef] [PubMed]
- Dhurandhar, N.V.; Petersen, K.S.; Webster, C. Key Causes and Contributors of Obesity: A Perspective. Nurs. Clin. N. Am. 2021, 56, 449–464. [Google Scholar] [CrossRef] [PubMed]
- Apovian, C.M. Obesity: Definition, comorbidities, causes, and burden. Am. J. Manag. Care 2016, 22, s176–s185. [Google Scholar] [PubMed]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 10 March 2023).
- Ogden, C.L.; Fakhouri, T.H.; Carroll, M.D.; Hales, C.M.; Fryar, C.D.; Li, X.; Freedman, D.S. Prevalence of Obesity Among Adults, by Household Income and Education—United States, 2011–2014. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1369–1373. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, H.; Roser, M. Obesity. Our World Data 2017. Available online: https://ourworldindata.org/obesity?country (accessed on 14 March 2023).
- Chooi, Y.C.; Ding, C.; Magkos, F. The epidemiology of obesity. Metabolism 2019, 92, 6–10. [Google Scholar] [CrossRef]
- World Obesity Federation. World Obesity Atlas 2023. Available online: https://www.worldobesity.org/resources/resource-library/world-obesity-atlas-2023 (accessed on 14 March 2023).
- Okunogbe, A.; Nugent, R.; Spencer, G.; Powis, J.; Ralston, J.; Wilding, J. Economic impacts of overweight and obesity: Current and future estimates for 161 countries. BMJ Glob. Health 2022, 7, e009773. [Google Scholar] [CrossRef]
- CDC. Defining Adult Overweight and Obesity; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/obesity/basics/adult-defining.html (accessed on 2 January 2023).
- CDC. Obesity, Race/Ethnicity, and COVID-19; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/obesity/data/HavingobesityincreasesriskofsevereillnessfromCOVID-19 (accessed on 13 December 2022).
- Petersen, R. Racial and Ethnic Disparities in Adult Obesity in the United States: CDC’s Tracking to Inform State and Local Action. Prev. Chronic. Dis. 2019, 16, E46. [Google Scholar] [CrossRef]
- Volaco, A.; Cavalcanti, A.M.; Filho, R.P.; Précoma, D.B. Socioeconomic Status: The Missing Link Between Obesity and Diabetes Mellitus? Curr. Diabetes Rev. 2018, 14, 321–326. [Google Scholar] [CrossRef]
- An, R. Educational disparity in obesity among U.S. adults, 1984–2013. Ann. Epidemiol. 2015, 25, 637–642.e5. [Google Scholar] [CrossRef]
- CDC. Hispanic/Latino Americans and Type 2 Diabetes; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2022. Available online: https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html (accessed on 13 December 2022).
- Gomez, S.; Blumer, V.; Rodriguez, F. Unique Cardiovascular Disease Risk Factors in Hispanic Individuals. Curr. Cardiovasc. Risk Rep. 2022, 16, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Balfour, P.C.; Ruiz, J.M.; Talavera, G.A.; Allison, M.A.; Rodriguez, C.J. Cardiovascular Disease in Hispanics/Latinos in the United States. J. Lat. Psychol. 2016, 4, 98–113. [Google Scholar] [CrossRef] [PubMed]
- de Cosio, F.G.; Diaz-Apodaca, B.; Baker, A.; Cifuentes, M.P.; Ojeda-Casares, H.; Constandce, D.; Becerra, F. US Obesity Mortality Trends and Associated Noncommunicable Diseases Contributing Conditions Among White, Black, and Hispanic Individuals by Age from 1999 to 2017. SN Compr. Clin. Med. 2021, 3, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Mehta, T.; McCubrey, R.; Pajewski, N.M.; Keith, S.W.; Allison, D.B.; Crespo, C.J.; Fontaine, K.R. Does obesity associate with mortality among Hispanic persons? Results from the National Health Interview Survey. Obesisty 2013, 21, 1474–1477. [Google Scholar] [CrossRef]
- Nimptsch, K.; Konigorski, S.; Pischon, T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism 2019, 92, 61–70. [Google Scholar] [CrossRef]
- Ling, C.; Rönn, T. Epigenetics in Human Obesity and Type 2 Diabetes. Cell Metab. 2019, 29, 1028–1044. [Google Scholar] [CrossRef]
- Balistreri, C.R.; Caruso, C.; Candore, G. The Role of Adipose Tissue and Adipokines in Obesity-Related Inflammatory Diseases. Mediat. Inflamm. 2010, 2010, 802078. [Google Scholar] [CrossRef]
- Stanirowski, P.J.; Szukiewicz, D.; Pyzlak, M.; Abdalla, N.; Sawicki, W.; Cendrowski, K. Impact of pre-gestational and gestational diabetes mellitus on the expression of glucose transporters GLUT-1, GLUT-4 and GLUT-9 in human term placenta. Endocrine 2017, 55, 799–808. [Google Scholar] [CrossRef]
- Xu, X.; Su, S.; Barnes, V.A.; De Miguel, C.; Pollock, J.; Ownby, D.; Shi, H.; Zhu, H.; Snieder, H.; Wang, X. A genome-wide methylation study on obesity: Differential variability and differential methylation. Epigenetics 2013, 8, 522–533. [Google Scholar] [CrossRef]
- King, S.E.; Skinner, M.K. Epigenetic Transgenerational Inheritance of Obesity Susceptibility. Trends Endocrinol. Metab. TEM 2020, 31, 478–494. [Google Scholar] [CrossRef]
- Singh, R.K.; Kumar, P.; Mahalingam, K. Molecular genetics of human obesity: A comprehensive review. Comptes. Rendus. Biol. 2017, 340, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Oelsner, K.T.; Guo, Y.; To, S.B.-C.; Non, A.L.; Barkin, S.L. Maternal BMI as a predictor of methylation of obesity-related genes in saliva samples from preschool-age Hispanic children at-risk for obesity. BMC Genom. 2017, 18, 57. [Google Scholar] [CrossRef] [PubMed]
- Rushing, A.; Sommer, E.C.; Zhao, S.; Po’e, E.K.; Barkin, S.L. Salivary epigenetic biomarkers as predictors of emerging childhood obesity. BMC Med. Genet. 2020, 21, 34. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, H.E.; Escaname, E.N.; Alana, N.B.; Lavender, E.; Gelfond, J.; Fernandez, R.; Hibbs, M.A.; King, J.M.; Carr, N.R.; Blanco, C.L. Maternal diabetes and obesity influence the fetal epigenome in a largely Hispanic population. Clin. Epigenetics 2020, 12, 34. [Google Scholar] [CrossRef]
- Voruganti, V.S.; Kent, J.W.; Debnath, S.; Cole, S.A.; Haack, K.; Göring, H.H.H.; Carless, M.A.; Curran, J.E.; Johnson, M.P.; Almasy, L.; et al. Genome-wide association analysis confirms and extends the association of SLC2A9 with serum uric acid levels to Mexican Americans. Front. Genet. 2013, 4, 279. [Google Scholar] [CrossRef]
- Stanirowski, P.J.; Szukiewicz, D.; Pyzlak, M.; Abdalla, N.; Sawicki, W.; Cendrowski, K. Analysis of correlations between the placental expression of glucose transporters GLUT-1, GLUT-4 and GLUT-9 and selected maternal and fetal parameters in pregnancies complicated by diabetes mellitus. J. Matern. -Fetal Neonatal Med. 2019, 32, 650–659. [Google Scholar] [CrossRef]
- Szebenyi, G.; Wigley, W.C.; Hall, B.; Didier, A.; Yu, M.; Thomas, P.; Krämer, H. Hook2 contributes to aggresome formation. BMC Cell Biol. 2007, 8, 19. [Google Scholar] [CrossRef]
- Huang, Y.; Mahley, R.W. Apolipoprotein E: Structure and function in lipid metabolism, neurobiology, and Alzheimer’s diseases. Neurobiol. Dis. 2014, 72 (Pt A), 3–12. [Google Scholar] [CrossRef]
- Anwar, M.Y.; Baldassari, A.R.; Polikowsky, H.G.; Sitlani, C.M.; Highland, H.M.; Chami, N.; Chen, H.-H.; Graff, M.; Howard, A.G.; Jung, S.Y.; et al. Genetic pleiotropy underpinning adiposity and inflammation in self-identified Hispanic/Latino populations. BMC Med. Genom. 2022, 15, 192. [Google Scholar] [CrossRef]
- Wright, S.M.; Aronne, L.J. Causes of obesity. Abdom. Radiol. 2012, 37, 730–732. [Google Scholar] [CrossRef]
- Dhurandhar, N.V.; Israel, B.A.; Kolesar, J.M.; Mayhew, G.F.; Cook, M.E.; Atkinson, R.L. Increased adiposity in animals due to a human virus. Int. J. Obes. 2000, 24, 989–996. [Google Scholar] [CrossRef] [PubMed]
- Pasarica, M.; Shin, A.C.; Yu, M.; Ou Yang, H.-M.; Rathod, M.; Jen, K.-L.C.; MohanKumar, S.; Mohankumar, P.S.; Markward, N.; Dhurandhar, N.V. Human adenovirus 36 induces adiposity, increases insulin sensitivity, and alters hypothalamic monoamines in rats. Obesity 2006, 14, 1905–1913. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, R.L.; Dhurandhar, N.V.; Allison, D.B.; Bowen, R.L.; Israel, B.A.; Albu, J.B.; Augustus, A.S. Human adenovirus-36 is associated with increased body weight and paradoxical reduction of serum lipids. Int. J. Obes. 2005, 29, 281–286. [Google Scholar] [CrossRef]
- Cheng, L.; Wang, J.; Dai, H.; Duan, Y.; An, Y.; Shi, L.; Lv, Y.; Li, H.; Wang, C.; Ma, Q.; et al. Brown and beige adipose tissue: A novel therapeutic strategy for obesity and type 2 diabetes mellitus. Adipocyte 2021, 10, 48–65. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.L. Lifestyle Factors and Genetic Variants Associated to Health Disparities in the Hispanic Population. Nutrients 2021, 13, 2189. [Google Scholar] [CrossRef]
- D’Alonzo, K.T.; Johnson, S.; Fanfan, D. A Biobehavioral Approach to Understanding Obesity and the Development of Obesogenic Illnesses Among Latino Immigrants in the United States. Biol. Res. Nurs. 2012, 14, 364–374. [Google Scholar] [CrossRef]
- Nicolaidis, S. Environment and obesity. Metabolism 2019, 100, 153942. [Google Scholar] [CrossRef]
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Pavela, G.; Lewis, D.W.; Locher, J.; Allison, D.B. Socioeconomic Status, Risk of Obesity, and the Importance of Albert J. Stunkard. Curr. Obes. Rep. 2016, 5, 132–139. [Google Scholar] [CrossRef]
- Anekwe, C.V.; Jarrell, A.R.; Townsend, M.J.; Gaudier, G.I.; Hiserodt, J.M.; Stanford, F.C. Socioeconomics of Obesity. Curr. Obes. Rep. 2020, 9, 272–279. [Google Scholar] [CrossRef]
- Gordon-Larsen, P. Food Availability/Convenience and Obesity. Adv. Nutr. 2014, 5, 809–817. [Google Scholar] [CrossRef]
- Isasi, C.R.; Rastogi, D.; Molina, K. Health Issues in Hispanic/Latino Youth. J. Lat. Psychol. 2016, 4, 67–82. [Google Scholar] [CrossRef]
- Escarce, J.J.; Kapur, K. Access to and Quality of Health Care; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Sehar, U.; Rawat, P.; Choudhury, M.; Boles, A.; Culberson, J.; Khan, H.; Malhotra, K.; Basu, T.; Reddy, P.H. Comprehensive Understanding of Hispanic Caregivers: Focus on Innovative Methods and Validations. J. Alzheimers Dis. Rep. 2022, 1–18, Preprint. [Google Scholar] [CrossRef]
- Overcash, F.; Reicks, M. Diet Quality and Eating Practices among Hispanic/Latino Men and Women: NHANES 2011–2016. Int. J. Environ. Res. Public Health 2021, 18, 1302. [Google Scholar] [CrossRef]
- Bray, G.A.; Nielsen, S.J.; Popkin, B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004, 79, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Johnsen, L.; Craven, M.; Nava, M.; Alonso, A.; Dykema-Engblade, A.; Rademaker, A.; Xie, H. Cultural Variables Underlying Obesity in Latino Men: Design, Rationale and Participant Characteristics from the Latino Men’s Health Initiative. J. Community Health 2017, 42, 826–838. [Google Scholar] [CrossRef] [PubMed]
- Fontana, L.; Partridge, L.; Longo, V.D. Extending healthy life span—From yeast to humans. Science 2010, 328, 321–326. [Google Scholar] [CrossRef]
- Zubrzycki, A.; Cierpka-Kmiec, K.; Kmiec, Z.; Wronska, A. The role of low-calorie diets and intermittent fasting in the treatment of obesity and type-2 diabetes. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2018, 69, 663–683. [Google Scholar] [CrossRef]
- Kim, J.Y. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J. Obes. Metab. Syndr. 2021, 30, 20–31. [Google Scholar] [CrossRef]
- Volek, J.S.; Vanheest, J.L.; Forsythe, C.E. Diet and exercise for weight loss: A review of current issues. Sport. Med. 2005, 35, 1–9. [Google Scholar] [CrossRef]
- Batsis, J.A.; Gill, L.E.; Masutani, R.K.; Adachi-Mejia, A.M.; Blunt, H.B.; Bagley, P.J.; Lopez-Jimenez, F.; Bartels, S.J. Weight loss interventions in older adults with obesity: A systematic review of randomized controlled trials since 2005. J. Am. Geriatr. Soc. 2017, 65, 257–268. [Google Scholar] [CrossRef]
- Mirza, N.M.; Palmer, M.G.; Sinclair, K.B.; McCarter, R.; He, J.; Ebbeling, C.B.; Ludwig, D.S.; Yanovski, J.A. Effects of a low glycemic load or a low-fat dietary intervention on body weight in obese Hispanic American children and adolescents: A randomized controlled trial. Am. J. Clin. Nutr. 2013, 97, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Diaz: Are Ethnic Differences in Insulin Sensitivity. Available online: https://scholar.google.com/scholar_lookup?title=Are%20ethnic%20differences%20in%20insulin%20sensitivity%20explained%20by%20variation%20in%20carbohydrate%20intake%3F&journal=Diabetologia&doi=10.1007%2Fs00125-005-1745-z&volume=48&pages=1264-1268&publication_year=2005&author=Diaz%2CVA&author=Mainous%2CAG&author=Koopman%2CR&author=Geesey%2CME (accessed on 4 May 2023).
- Cuy Castellanos, D. Dietary Acculturation in Latinos/Hispanics in the United States. Am. J. Lifestyle Med. 2015, 9, 31–36. [Google Scholar] [CrossRef]
- CDC. Healthy Eating for a Healthy Weight; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2023. Available online: https://www.cdc.gov/healthyweight/healthy_eating/index.html (accessed on 9 May 2023).
- Manore, M.M. Exercise and the Institute of Medicine recommendations for nutrition. Curr. Sports Med. Rep. 2005, 4, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Oppert, J.-M.; Bellicha, A.; Ciangura, C. Physical activity in management of persons with obesity. Eur. J. Intern. Med. 2021, 93, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Jakicic, J.M.; Davis, K.K. Obesity and physical activity. Psychiatr. Clin. N. Am. 2011, 34, 829–840. [Google Scholar] [CrossRef]
- Rippe, J.M.; Hess, S. The Role of Physical Activity in the Prevention and Management of Obesity. J. Am. Diet. Assoc. 1998, 98, S31–S38. [Google Scholar] [CrossRef]
- CDC. Physical Activity for a Healthy Weight; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2023. Available online: https://www.cdc.gov/healthyweight/physical_activity/index.html (accessed on 4 May 2023).
- Hannan, J.; Brooten, D.; Youngblut, J.M.; Hildago, I.; Roche, R.; Seagrave, L. Physical activity and stress in adult Hispanics. J. Am. Assoc. Nurse. Pract. 2015, 27, 79. [Google Scholar] [CrossRef]
- Afable-Munsuz, A.; Ponce, N.A.; Rodriguez, M.; Perez-Stable, E.J. Immigrant generation and physical activity among Mexican, Chinese & Filipino adults in the U.S. Soc. Sci. Med. 2010, 70, 1997–2005. [Google Scholar] [CrossRef]
- Perez, L.G.; Arredondo, E.M.; Elder, J.P.; Barquera, S.; Nagle, B.; Holub, C.K. Evidence-Based Obesity Treatment Interventions for Latino Adults in the U.S. Am. J. Prev. Med. 2013, 44, 550–560. [Google Scholar] [CrossRef]
- Oh, S.S.; Galanter, J.; Thakur, N.; Pino-Yanes, M.; Barcelo, N.E.; White, M.J.; de Bruin, D.M.; Greenblatt, R.M.; Bibbins-Domingo, K.; Wu, A.H.B.; et al. Diversity in Clinical and Biomedical Research: A Promise Yet to Be Fulfilled. PLoS Med. 2015, 12, e1001918. [Google Scholar] [CrossRef]
- Holub, C.K.; Elder, J.P.; Arredondo, E.M.; Barquera, S.; Eisenberg, C.M.; Sánchez Romero, L.M.; Rivera, J.; Lobelo, F.; Simoes, E. Obesity Control in Latin American and U.S. Latinos: A Systematic Review. Am. J. Prev. Med. 2013, 44, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Living A for C. 2020 Profile of Hispanic Americans Age 65 and Older 2020. Available online: https://acl.gov/sites/default/files/Profile%20of%20OA/HispanicProfileReport2021.pdf (accessed on 13 March 2023).
- Flegal, K.M.; Graubard, B.I.; Williamson, D.F.; Gail, M.H. Excess deaths associated with underweight, overweight, and obesity: An evaluation of potential bias. Vital. Health Stat. 2018, 42, 1–12. [Google Scholar]
- Yang, Z.; Hall, A.G. The Financial Burden of Overweight and Obesity among Elderly Americans: The Dynamics of Weight, Longevity, and Health Care Cost. Health Serv. Res. 2008, 43, 849–868. [Google Scholar] [CrossRef] [PubMed]
- Mullin, G.E.; Cheskin, L.J.; Matarese, L.E. Introduction to Integrative Weight Management. Integr. Weight Manag. Guide Clin. 2014, 1–8. [Google Scholar] [CrossRef]
- Batsis, J.A.; Zagaria, A.B. Addressing Obesity in Aging Patients. Med. Clin. N. Am. 2018, 102, 65–85. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.; Cai, J.; Pamuk, E.R.; Williamson, D.F.; Thun, M.J.; Wood, J.L. The effect of age on the association between body-mass index and mortality. N. Engl. J. Med. 1998, 338, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Locher, J.L.; Goldsby, T.U.; Goss, A.M.; Kilgore, M.L.; Gower, B.; Ard, J.D. Calorie restriction in overweight older adults: Do benefits exceed potential risks? Exp. Gerontol. 2016, 86, 4–13. [Google Scholar] [CrossRef]
- Halter, J.B.; Musi, N.; McFarland Horne, F.; Crandall, J.P.; Goldberg, A.; Harkless, L.; Hazzard, W.R.; Huang, E.S.; Kirkman, M.S.; Plutzky, J.; et al. Diabetes and Cardiovascular Disease in Older Adults: Current Status and Future Directions. Diabetes 2014, 63, 2578–2589. [Google Scholar] [CrossRef]
- Colleluori, G.; Aguirre, L.; Phadnis, U.; Fowler, K.; Armamento-Villareal, R.; Sun, Z.; Brunetti, L.; Park, J.H.; Kaipparettu, B.A.; Putluri, N.; et al. Aerobic plus resistance exercise in obese older adults improves muscle protein synthesis and preserves myocellular quality despite weight loss. Cell Metab. 2019, 30, 261–273. [Google Scholar] [CrossRef]
- Gloy, V.L.; Briel, M.; Bhatt, D.L.; Kashyap, S.R.; Schauer, P.R.; Mingrone, G.; Bucher, H.C.; Nordmann, A.J. Bariatric surgery versus non-surgical treatment for obesity: A systematic review and meta-analysis of randomised controlled trials. BMJ 2013, 347, f5934. [Google Scholar] [CrossRef]
- Huang, T.-S.; Hu, F.-C.; Fan, C.-W.; Lee, C.-H.; Jwo, S.-C.; Chen, H.-Y. A simple novel model to predict hospital mortality, surgical site infection, and pneumonia in elderly patients undergoing operation. Dig. Surg. 2010, 27, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Iranmanesh, P.; Boudreau, V.; Ramji, K.; Barlow, K.; Lovrics, O.; Anvari, M. Outcomes of bariatric surgery in elderly patients: A registry-based cohort study with 3-year follow-up. Int. J. Obes. 2022, 46, 574–580. [Google Scholar] [CrossRef] [PubMed]
- Staff, C. Challenges of Bariatric Caregiving. CareLink 2018. Available online: https://www.carelink.org/challenges-of-bariatric-caregiving/ (accessed on 13 March 2023).
- For Caregivers, Family and Friends 2022. Available online: https://www.cdc.gov/aging/caregiving/index.htm (accessed on 4 November 2022).
- Ankuda, C.K.; Harris, J.; Ornstein, K.; Levine, D.A.; Langa, K.M.; Kelley, A.S. Caregiving for Older Adults with Obesity in the United States. J. Am. Geriatr. Soc. 2017, 65, 1939–1945. [Google Scholar] [CrossRef] [PubMed]
- Jura, M.; Kozak Leslie, P. Obesity and related consequences to ageing. Age 2016, 38, 23. [Google Scholar] [CrossRef]
- Robstad, N.; Söderhamn, U.; Fegran, L. Intensive care nurses’ experiences of caring for obese intensive care patients: A hermeneutic study. J. Clin. Nurs. 2018, 27, 386–395. [Google Scholar] [CrossRef]
- Kalish, V.B. Obesity in Older Adults. Prim. Care 2016, 43, 137–144, ix. [Google Scholar] [CrossRef]
- McClean, K.; Cross, M.; Reed, S. Risks to Healthcare Organizations and Staff Who Manage Obese (Bariatric) Patients and Use of Obesity Data to Mitigate Risks: A Literature Review. J. Multidiscip. Healthc. 2021, 14, 577–588. [Google Scholar] [CrossRef]
- Galinsky, T.; Deter, L.; Krieg, E.; Feng, H.A.; Battaglia, C.; Bell, R.; Haddock, K.S.; Hilton, T.; Lynch, C.; Matz, M.; et al. Safe patient handling and mobility (SPHM) for increasingly bariatric patient populations: Factors related to caregivers’ self-reported pain and injury. Appl. Ergon. 2021, 91, 103300. [Google Scholar] [CrossRef]
- Levine, J.A. Poverty and Obesity in the U.S. Diabetes 2011, 60, 2667–2668. [Google Scholar] [CrossRef]
- Fruh, S.M.; Nadglowski, J.; Hall, H.R.; Davis, S.L.; Crook, E.D.; Zlomke, K. Obesity Stigma and Bias. J. Nurse. Pract. JNP 2016, 12, 425–432. [Google Scholar] [CrossRef]
- Riffin, C.; Van Ness, P.H.; Wolff, J.L.; Fried, T. Family and Other Unpaid Caregivers and Older Adults with and without Dementia and Disability. J. Am. Geriatr. Soc. 2017, 65, 1821–1828. [Google Scholar] [CrossRef] [PubMed]



| BMI Range | Weight Classification |
|---|---|
| <18.5 | Underweight |
| 18.5–24.9 | Healthy Weight |
| 25.0–29.9 | Overweight |
| 30.0–34.9 | Class I Obesity |
| 35.0–39.9 | Class II Obesity |
| >40.0 | Class III Obesity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basu, T.; Sehar, U.; Selman, A.; Reddy, A.P.; Reddy, P.H. Support Provided by Caregivers for Community-Dwelling Obesity Individuals: Focus on Elderly and Hispanics. Healthcare 2023, 11, 1442. https://doi.org/10.3390/healthcare11101442
Basu T, Sehar U, Selman A, Reddy AP, Reddy PH. Support Provided by Caregivers for Community-Dwelling Obesity Individuals: Focus on Elderly and Hispanics. Healthcare. 2023; 11(10):1442. https://doi.org/10.3390/healthcare11101442
Chicago/Turabian StyleBasu, Tanisha, Ujala Sehar, Ashley Selman, Arubala P. Reddy, and P. Hemachandra Reddy. 2023. "Support Provided by Caregivers for Community-Dwelling Obesity Individuals: Focus on Elderly and Hispanics" Healthcare 11, no. 10: 1442. https://doi.org/10.3390/healthcare11101442





